Abstract
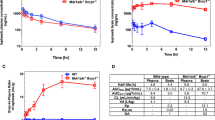
In malignant glioma, cytotoxic drugs are often inhibited from accessing the tumor site due to the blood-tumor barrier (BTB). Ibrutinib, FDA-approved lymphoma agent, inhibits Bruton tyrosine kinase (BTK) and has previously been shown to independently impair aortic endothelial adhesion and increase rodent glioma model survival in combination with cytotoxic therapy. Yet additional research is required to understand ibrutinib’s effect on BTB function. In this study, we detail baseline BTK expression in glioma cells and its surrounding vasculature, then measure endothelial junctional expression/function changes with varied ibrutinib doses in vitro. Rat glioma cells and rodent glioma models were treated with ibrutinib alone (1–10 µM and 25 mg/kg) and in combination with doxil (10–100 µM and 3 mg/kg) to assess additive effects on viability, drug concentrations, tumor volume, endothelial junctional expression and survival. We found that ibrutinib, in a dose-dependent manner, decreased brain endothelial cell–cell adhesion over 24 h, without affecting endothelial cell viability (p < 0.005). Expression of tight junction gene and protein expression was decreased maximally 4 h after administration, along with inhibition of efflux transporter, ABCB1, activity. We demonstrated an additive effect of ibrutinib with doxil on rat glioma cells, as seen by a significant reduction in cell viability (p < 0.001) and increased CNS doxil concentration in the brain (56 ng/mL doxil alone vs. 74.6 ng/mL combination, p < 0.05). Finally, Ibrutinib, combined with doxil, prolonged median survival in rodent glioma models (27 vs. 16 days, p < 0.0001) with brain imaging showing a − 53% versus − 75% volume change with doxil alone versus combination therapy (p < 0.05). These findings indicate ibrutinib’s ability to increase brain endothelial permeability via junctional disruption and efflux inhibition, to increase BTB drug entry and prolong rodent glioma model survival. Our results motivate the need to identify other BTB modifiers, all with the intent of improving survival and reducing systemic toxicities.
Similar content being viewed by others
Introduction
One of the crucial treatment challenges of glioblastoma is the restrictiveness of the blood–brain barrier/blood-tumor barrier (BBB/BTB). Glioma progression has been linked to BTB (blood- disruption, causing increased permeability due to structural changes from angiogenesis, astrocytic end feet displacement, and neuronal death [1]. Specifically in high-grade gliomas, structural abnormalities across the BTB can lead to extravasation of blood contents, including solutes, antibodies, fluorescent markers, and immune cells [2]. However, the BTB demonstrates heterogeneous permeability. Specifically, high-grade gliomas have certain intact sections of BTB, which aid in continued tumor growth, invasion, and limitation of therapeutic drug penetration, leading to disease progression and treatment resistance [3]. To overcome these challenges, it is essential to identify BTB modulators that can transiently increase permeability and help the entry of chemotherapy or directed cytotoxic agents in such restricted areas.
The BBB is one of the main components of the neurovascular unit which includes endothelial cells, pericytes, and astrocytic end feet working harmoniously. In a healthy person, the BBB maintains the central nervous system (CNS) homeostasis by regulating the entry and exit of drugs, molecules, and toxins [4]. The key player of the BBB is endothelial cells, mesodermally derived, modified simple squamous epithelial cells that comprise blood vessel walls and are in the most direct contact with blood that circulates throughout the brain [5]. Mechanisms of BBB permeability are mostly centered around the expression and function of endothelial tight junctions along with membrane transport proteins, such as ATP binding cassette (ABC) transporters. These endothelial cells are held together by bicellular and tricellular junction proteins that aid in communication for paracellular transport of drugs, cells and immunologics. Bicellular junctions include the claudin proteins (claudin-1, claudin-3, claudin-5), zonula occluden (ZO-1, ZO-2) and tricellular junctions include (angulin-1/LSR, tricellulin/MarvelD2). Brain endothelial cells also express exceptionally high levels of nutrient transport proteins such as ABC transporters, mainly localized on the luminal side of the vasculature, to assist with pum** specific cytotoxic chemotherapies out of the cell [6, 7]. Both endothelial cells and malignant glioma cells have been reported to express high levels of ABC transporters, specifically P-glycoprotein (P-gp) (encoded by the—ABCB1 gene), ABCG2 and ABCC4 [8, 9]. Overall, these mechanisms are regulated through various modalities, including direct communication with the CNS and neuroimmune modulators released by nearby cells. The dynamic nature of the BBB allows for permeability adjustment in response to changes in the microenvironment, especially in the presence of malignant glioma cells [10, 11].
Ibrutinib is an FDA-approved B-cell lymphoma/lymphocytic leukemia agent that inhibits BTK (Bruton tyrosine kinase) activation, leading to decreased B-cell receptor signaling and decreased proliferative potential. In cardiac endothelium, ibrutinib inhibits vascular cell adhesion, platelet aggregation, and the associated inflammatory responses that occur during endothelial cell activation [https://boevalab.inf.ethz.ch/FREEC/) was applied to the local realigned and refined alignments over a range of ploidy (ploidy = 2, 3, 4, 5, 6, 7, 8). Based on the ploidy esitmate returned from this tool (output_ploidy = 7), variants were filtered to keep those observed to have a freqeuncy ≥ 14% and indicated by functional annotation to be non-synonomous. Surviving variants were then summarized in table form by variant type stratified by chromosome. Variants prior to filtering were also summarized in table form for select genes (Atrx, Egfr, H3f3a, H3f3b, Idh1, Idh2, Tert, Tp53).
Statistical analyses
Data are presented as mean ± standard error of the mean, unless otherwise noted. The Student t-test (2-tailed), and 1-way analysis of variance with Tukey’s test evaluated statistical significance with GraphPad Prism 9.3 software (GraphPad Software, Inc).
Results
High bruton tyrosine kinase (BTK) expression in grade IV human gliomas
Previous studies have demonstrated the high expression of BTK/BMX in glioblastoma [28, 28, 29]. While our brain endothelial cell viability studies exhibit no effects from ibrutinib, cell–cell interaction is reduced after 2 h, with notable recovery over the next 24 h. However, it was not a complete recovery, which could be due to a lack of systemic washout in this in vitro brain endothelial cell only assay. Specifically, junctional protein expression and down-stream ERK pathway proteins were found to be reduced following ibrutinib therapy, which agrees with previous studies showcasing BTK/BMX inhibition causing disruption of epithelial cell tightness [46, 47, 49]. A reduction of pERK has been shown to lead to reduced expression of tight junction proteins in the epididymis of mice, within the blood-testis barrier as reported by Kim et al. [50] Unfortunately, there is no one method to state whether the BBB is intact or not within these glioma models, thus evaluations of drug permeability and immunohistochemical staining of junctional markers is the best surrogate of such determinations. Combined, this data showcases ibrutinib’s ability to reduce expression of ZO-1 and other tight junctions resulting in associated attenuation of p-ERK pathway activation and ABCB1 inhibition. Previous studies have shown high BTK expression on glioma cells and ibrutinib’s efficacy to hinder lymphoma and other solid tumors progression through inhibition of the BTK/BMX pathway. Yet, no studies of ibrutinib’s effect on brain endothelium have been published, which could demonstrate a more complete picture of this drugs effects on the tumor microenvironment [12]. As such, these findings showcasing ibrutinib’s influence of brain endothelial cell–cell integrity and ABCB1 transporter function have larger implications for various neurologic, vascular and oncologic diseases. In our studies, we chose to explore the ABCB1 substrate doxil, and Zhou et al. found that ibrutinib’s use in human-derived glioma rodent models demonstrated additive cytotoxicity with etoposide (ABCB1 and ABCC1 substrate), which suggests that ibrutinib may target more than just one ABC transporter [16].
Some limitations of our studies include investigations of ibrutinib’s effects on the 1) tumor immune microenvironment, 2) long-term disease course with combination chemotherapy and 3) varied in vivo models. Our initial studies detailed the effect of ibrutinib on brain endothelium and tumor cells, as the former studies were novel and have the potential to positively benefit field knowledge related to CNS drug entry and impaired disease progression. While our studies did not explore effects of ibrutinib on the immune cells within the tumor microenvironment, previous studies have demonstrated ibrutinib’s ability to decrease glioma derived pericyte expression, which are cells known to create a formidable BBB but also demonstrate scavenger like functions when necessary [14]. In complement, Li et al., found that ibrutinib reduced CD8 + T cell exhaustion both in the in vitro setting and in BTK deficient mice, specifically by downregulating inhibitory receptors and increasing cytokine production [51]. The presence of T cell inhibitory signaling has been implicated in assistance with disease progression in glioblastomas thus further studies are warranted to further delineate the influence of BTK/BMX inhibition on T-cell infiltration, microglial behaviors and cytokine production within immunocompetent models [52].
Additionally, because S635 glioma cells orthotopically injected in immunocompetent hosts resulted in approximately 20–30 + days of survival with ibrutinib alone vs combination therapy, we were unable to assess long-term effects of ibrutinib therapy on disease course. Using another rat glioma model with less invasive quality and pronged survival without therapy could provide additional studies that help to explore systemic and neurologic sequelae from repeat ibrutinib therapy additive and/or synergistic with varied cytotoxic chemotherapy agents. These studies would assist in understanding more about the long-term effects of transient BBB disruption from ibrutinib as related to survival outcomes and tumor biology.
Other than S635, there only exists 9L, C6 and F98 rat derived glioma cells. We chose not to use 9L as it has previously been shown to be more akin histologically to gliosarcoma. C6 and F98 rat glioma lines, while most closely resemble (histologically and molecularly) glioblastoma, its growth patterns evoke alloimmunity or weak immunogenicity, respectively [53,54,55]. As such, its use has been cautioned for use with any evaluations that could aim to evaluate immunotherapeutics or agents that may influence the immune microenvironment [54]. As such, we opted to use a model with no limitations for evaluation. While the use of rodent models are highly necessary to advance to the neurooncologic field, there still exist restrictions within the suitability of models for translational applications.
Shi et al. reported that high BMX expression in glioma stem cells could be inhibited by ibrutinib resulting in decreased cell proliferation alone or with etoposide chemotherapeutic agent [14]. Comparatively, in this study, we found that ibrutinib has no significant effect on S635 rat glioma cell viability, yet it influenced endothelial junction proteins, inhibited efflux of ABCB1 and impaired migration. Classically, it is a known challenge to extrapolate in vitro dosing to rodent models due to the lack of dynamic fluidity as seen in a living system, thus we relied on published data from varied endothelial and cancer lines for treatment of our endothelial and glioma cells [12, 56, 57]. For additional clinical relevance, we investigated the additive effect of ibrutinib with and without doxil or doxorubicin treatment. Doxorubicin is a well-known substrate of both ABCB1 and ABCG2 and an effective chemotherapy drug that has been shown to hinder cancer proliferation of multiple solid tumors [58, 59]. However, doxorubicin cannot penetrate through the BBB easily and even with the assistance of ibrutinib we found no enhancement in survival or tumor volume with combined therapy (Additional file 2: Fig. 2). Doxil is the pegylated liposomal form of doxorubicin which confers a higher likelihood to cross the BBB, therefore these findings further point to the need to strategically select agents that can be paired with ibrutinib which are ABCB1 or potentially ABCC1 substrates and can impair glioma viability, migration and growth [60]. We evaluated free doxorubicin released from doxil within plasma and brain approximately 2 h after administration and found higher concentrations post ibrutinib. Yet, additional evaluations from 6 to 24 h after administration may aid determing differences in the brain and brain tumor settings regarding drug clearance with ibrutinib [24].
In our current study, we have provided evidence that ibrutinib influences brain endothelial integrity, efflux transport, and tumor progression. Our animal studies provide additional data in support of ibrutinib use to provide sustainable effects on BBB/BTB permeability and glioma cell propagation. Current clinical trials are ongoing to explore the use of ibrutinib with chemoradiation against glioblastoma which will provide further data on the use of this agent for varied treatment types (NCT03535350 and NCT05106296). Continued and novel research is needed to investigate ibrutinib’s efficacy with tumor directed agents, changes to the immune microenvironment and prolonged use for malignant gliomas; all with the aim of increasing CNS drug entry and improving disease survival.
References
Arvanitis CD, Ferraro GB, Jain RK (2020) The blood-brain barrier and blood-tumour barrier in brain tumours and metastases. Nat Rev Cancer 20(1):26–41
Belykh E, Shaffer KV, Lin C, Byvaltsev VA, Preul MC, Chen L (2020) Blood-brain barrier, blood-brain tumor barrier, and fluorescence-guided neurosurgical oncology: delivering optical labels to brain tumors. Front Oncol 10:739
van Tellingen O, Yetkin-Arik B, de Gooijer MC, Wesseling P, Wurdinger T, de Vries HE (2015) Overcoming the blood-brain tumor barrier for effective glioblastoma treatment. Drug Resist Updates Rev Comment Antimicrob Anticancer Chemotherapy 19:1–12
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ (2010) Structure and function of the blood-brain barrier. Neurobiol Dis 37(1):13–25
Daneman R, Agalliu D, Zhou L, Kuhnert F, Kuo CJ, Barres BA (2009) Wnt/beta-catenin signaling is required for CNS, but not non-CNS, angiogenesis. Proc Natl Acad Sci U S A 106(2):641–646
Saunders NR, Habgood MD, Mollgard K, Dziegielewska KM (2016) The biological significance of brain barrier mechanisms: Help or hindrance in drug delivery to the central nervous system? F1000Res 5:313
Shen S, Zhang W (2010) ABC transporters and drug efflux at the blood-brain barrier. Rev Neurosci 21(1):29–53
Zhang W, Mojsilovic-Petrovic J, Andrade MF, Zhang H, Ball M, Stanimirovic DB (2003) The expression and functional characterization of ABCG2 in brain endothelial cells and vessels. FASEB J 17(14):2085–2087
de Gooijer MC, Kemper EM, Buil LCM, Citirikkaya CH, Buckle T, Beijnen JH, van Tellingen O (2021) ATP-binding cassette transporters restrict drug delivery and efficacy against brain tumors even when blood-brain barrier integrity is lost. Cell Rep Med 2(1):100184
Banks WA (2009) Characteristics of compounds that cross the blood-brain barrier. BMC Neurol 9(Suppl 1):S3
Gu JJ, Zhang JH, Chen HJ, Wang SS (2016) TPX2 promotes glioma cell proliferation and invasion via activation of the AKT signaling pathway. Oncol Lett 12(6):5015–5022
Kohs TCL, Olson SR, Pang J, Jordan KR, Zheng TJ, **e A, Hodovan J, Muller M, McArthur C, Johnson J, Sousa BB, Wallisch M, Kievit P, Aslan JE, Seixas JD, Bernardes GJL, Hinds MT, Lindner JR, McCarty OJT, Puy C, Shatzel JJ (2022) Ibrutinib inhibits BMX-dependent endothelial VCAM-1 expression in vitro and pro-atherosclerotic endothelial activation and platelet adhesion in vivo. Cell Mol Bioeng 15(3):231–243
Grommes C, Pastore A, Palaskas N, Tang SS, Campos C, Schartz D, Codega P, Nichol D, Clark O, Hsieh WY, Rohle D, Rosenblum M, Viale A, Tabar VS, Brennan CW, Gavrilovic IT, Kaley TJ, Nolan CP, Omuro A, Pentsova E, Thomas AA, Tsyvkin E, Noy A, Palomba ML, Hamlin P, Sauter CS, Moskowitz CH, Wolfe J, Dogan A, Won M, Glass J, Peak S, Lallana EC, Hatzoglou V, Reiner AS, Gutin PH, Huse JT, Panageas KS, Graeber TG, Schultz N, DeAngelis LM, Mellinghoff IK (2017) Ibrutinib unmasks critical role of bruton tyrosine kinase in primary CNS lymphoma. Cancer Discov 7(9):1018–1029
Shi Y, Guryanova OA, Zhou W, Liu C, Huang Z, Fang X, Wang X, Chen C, Wu Q, He Z, Wang W, Zhang W, Jiang T, Liu Q, Chen Y, Wang W, Wu J, Kim L, Gimple RC, Feng H, Kung HF, Yu JS, Rich JN, ** YF, Bian XW, Bao S (2018) Ibrutinib inactivates BMX-STAT3 in glioma stem cells to impair malignant growth and radioresistance. Sci Transl Med 10(443):eaah6816
Guerra DAP, Paiva AE, Sena IFG, Azevedo PO, Silva WN, Mintz A, Birbrair A (2018) Targeting glioblastoma-derived pericytes improves chemotherapeutic outcome. Angiogenesis 21(4):667–675
Zhou W, Chen C, Shi Y, Wu Q, Gimple RC, Fang X, Huang Z, Zhai K, Ke SQ, ** YF, Feng H, Rich JN, Yu JS, Bao S, Bian XW (2017) Targeting glioma stem cell-derived pericytes disrupts the blood-tumor barrier and improves chemotherapeutic efficacy. Cell Stem Cell 21(5):591–603
Zhang H, Patel A, Wang YJ, Zhang YK, Kathawala RJ, Qiu LH, Patel BA, Huang LH, Shukla S, Yang DH, Ambudkar SV, Fu LW, Chen ZS (2017) The BTK inhibitor ibrutinib (PCI-32765) overcomes paclitaxel resistance in ABCB1- and ABCC10-overexpressing cells and tumors. Mol Cancer Ther 16(6):1021–1030
Lee YS, Bigner SH, Eng LF, Molnar P, Kuruvilla A, Groothuis DR, Bigner DD (1986) A glial fibrillary acidic protein-expressing and tumorigenic cell line derived from an avian sarcoma virus-induced rat astrocytoma. J Neuropathol Exp Neurol 45(6):704–720
Robey RW, Shukla S, Finley EM, Oldham RK, Barnett D, Ambudkar SV, Fojo T, Bates SE (2008) Inhibition of P-glycoprotein (ABCB1)- and multidrug resistance-associated protein 1 (ABCC1)-mediated transport by the orally administered inhibitor, CBT-1((R)). Biochem Pharmacol 75(6):1302–1312
Vézina A, Manglani M, Morris D, Foster B, McCord M, Song H, Zhang M, Davis D, Zhang W, Bills J, Nagashima K, Shankarappa P, Kindrick J, Walbridge S, Peer CJ, Figg WD, Gilbert MR, McGavern DB, Muldoon LL, Jackson S (2021) Adenosine A2A receptor activation enhances blood-tumor barrier permeability in a rodent glioma model. Mol Cancer Res MCR 19(12):2081–2095
Nie W, Zan X, Yu T, Ran M, Hong Z, He Y, Yang T, Ju Y, Gao X (2020) Synergetic therapy of glioma mediated by a dual delivery system loading α-mangostin and doxorubicin through cell cycle arrest and apoptotic pathways. Cell Death Dis 11(10):928
Watanabe A, Murayama S, Karasawa K, Yamamoto E, Morikawa S, Takita R, Murata S, Kato M (2019) A simple and easy method of monitoring doxorubicin release from a liposomal drug formulation in the serum using fluorescence spectroscopy. Chem Pharm Bull 67(4):367–371
Itoh N, Kimoto A, Yamamoto E, Higashi T, Santa T, Funatsu T, Kato M (2017) High performance liquid chromatography analysis of 100-nm liposomal nanoparticles using polymer-coated, silica monolithic columns with aqueous mobile phase. J Chromatogr A 1484:34–40
Yamamoto E, Hyodo K, Suzuki T, Ishihara H, Kikuchi H, Kato M (2018) Simulation of stimuli-responsive and stoichiometrically controlled release rate of doxorubicin from liposomes in tumor interstitial fluid. Pharm Res 35(5):103
Mauda-Havakuk M, Mikhail AS, Starost MF, Jones EC, Karim B, Kleiner DE, Partanen A, Esparza-Trujillo JA, Bakhutashvili I, Wakim PG, Kassin MT, Lewis AL, Karanian JW, Wood BJ, Pritchard WF (2021) Imaging pathology, and immune correlates in the woodchuck hepatic tumor model. J Hepatocell Carcinoma 8:71–83
Ames HM, Rooper LM, Laterra JJ, Eberhart CG, Rodriguez FJ (2018) INSM1 expression is frequent in primary central nervous system neoplasms but not in the adult brain parenchyma. J Neuropathol Exp Neurol 77(5):374–382
Fedor HL, De Marzo AM (2005) Practical methods for tissue microarray construction. Methods Mol Med 103:89–101
Wei L, Su YK, Lin CM, Chao TY, Huang SP, Huynh TT, Jan HJ, Whang-Peng J, Chiou JF, Wu AT, Hsiao M (2016) Preclinical investigation of ibrutinib, a Bruton’s kinase tyrosine (Btk) inhibitor, in suppressing glioma tumorigenesis and stem cell phenotypes. Oncotarget 7(43):69961–69975
Yue C, Niu M, Shan QQ, Zhou T, Tu Y, **e P, Hua L, Yu R, Liu X (2017) High expression of Bruton’s tyrosine kinase (BTK) is required for EGFR-induced NF-kappaB activation and predicts poor prognosis in human glioma. J Exp Clin Cancer Res CR 36(1):132
Zhao Z, Meng F, Wang W, Wang Z, Zhang C, Jiang T (2017) Comprehensive RNA-seq transcriptomic profiling in the malignant progression of gliomas. Sci Data 4:170024
Zhang Q, Zheng M, Betancourt CE, Liu L, Sitikov A, Sladojevic N, Zhao Q, Zhang JH, Liao JK, Wu R (2021) Increase in blood-brain barrier (BBB) permeability is regulated by MMP3 via the ERK signaling pathway. Oxid Med Cell Longev 2021:6655122
Ryu WI, Lee H, Bae HC, Jeon J, Ryu HJ, Kim J, Kim JH, Son JW, Kim J, Imai Y, Yamanishi K, Jeong SH, Son SW (2018) IL-33 down-regulates CLDN1 expression through the ERK/STAT3 pathway in keratinocytes. J Dermatol Sci 90(3):313–322
Chu H, Yang X, Huang C, Gao Z, Tang Y, Dong Q (2017) Apelin-13 protects against ischemic blood-brain barrier damage through the effects of aquaporin-4. Cerebrovasc Dis 44(1–2):10–25
Shi Y, Guryanova OA, Zhou W, Liu C, Huang Z, Fang X, Wang X, Chen C, Wu Q, He Z, Wang W, Zhang W, Jiang T, Liu Q, Chen Y, Wang W, Wu J, Kim L, Gimple RC, Feng H, Kung HF, Yu JS, Rich JN, ** YF, Bian XW, Bao S (2018) Ibrutinib inactivates BMX-STAT3 in glioma stem cells to impair malignant growth and radioresistance. Sci Transl Med 10(443):eaah6816
Hatoum A, Mohammed R, Zakieh O (2019) The unique invasiveness of glioblastoma and possible drug targets on extracellular matrix. Cancer Manag Res 11:1843–1855
Davis ME (2016) Glioblastoma: overview of disease and treatment. Clin J Oncol Nurs 20(5 Suppl):S2–S8
Fernandes C, Costa A, Osorio L, Lago RC, Linhares P, Carvalho B, Caeiro C (2017) Current standards of care in glioblastoma therapy. In: De Vleeschouwer S (ed) Glioblastoma. Codon Publications, Brisbane (AU)
Minniti G, Niyazi M, Alongi F, Navarria P, Belka C (2021) Current status and recent advances in reirradiation of glioblastoma. Radiat Oncol 16(1):36
Wang Z, Sun H, Yakisich JS (2014) Overcoming the blood-brain barrier for chemotherapy: limitations, challenges and rising problems. Anticancer Agents Med Chem 14(8):1085–1093
Portnow J, Badie B, Chen M, Liu A, Blanchard S, Synold TW (2009) The neuropharmacokinetics of temozolomide in patients with resectable brain tumors: potential implications for the current approach to chemoradiation. Clin Cancer Res 15(22):7092–7098
Jackson S, Weingart J, Nduom EK, Harfi TT, George RT, McAreavey D, Ye X, Anders NM, Peer C, Figg WD, Gilbert M, Rudek MA, Grossman SA (2018) The effect of an adenosine A(2A) agonist on intra-tumoral concentrations of temozolomide in patients with recurrent glioblastoma. Fluids Barriers CNS 15(1):2
Proescholdt MA, Merrill MJ, Ikejiri B, Walbridge S, Akbasak A, Jacobson S, Oldfield EH (2001) Site-specific immune response to implanted gliomas. J Neurosurg 95(6):1012–1019
Falter J, Lohmeier A, Eberl P, Stoerr EM, Koskimäki J, Falter L, Rossmann J, Mederer T, Schmidt NO, Proescholdt M (2023) CXCR2-blocking has context-sensitive effects on rat glioblastoma cell line outgrowth (S635) in an organotypic rat brain slice culture depending on microglia-depletion (PLX5622) and dexamethasone treatment. Int J Mol Sci 24(23):16803
Fu Y, Huang R, Zheng Y, Zhang Z, Liang A (2011) Glioma-derived mutations in isocitrate dehydrogenase 2 beneficial to traditional chemotherapy. Biochem Biophys Res Commun 410(2):218–223
He Y, Luo Y, Tang S, Rajantie I, Salven P, Heil M, Zhang R, Luo D, Li X, Chi H, Yu J, Carmeliet P, Schaper W, Sinusas AJ, Sessa WC, Alitalo K, Min W (2006) Critical function of Bmx/Etk in ischemia-mediated arteriogenesis and angiogenesis. J Clin Investig 116(9):2344–2355
Holopainen T, Rasanen M, Anisimov A, Tuomainen T, Zheng W, Tvorogov D, Hulmi JJ, Andersson LC, Cenni B, Tavi P, Mervaala E, Kivela R, Alitalo K (2015) Endothelial Bmx tyrosine kinase activity is essential for myocardial hypertrophy and remodeling. Proc Natl Acad Sci U S A 112(42):13063–13068
Dai B, Kim O, **e Y, Guo Z, Xu K, Wang B, Kong X, Melamed J, Chen H, Bieberich CJ, Borowsky AD, Kung HJ, Wei G, Ostrowski MC, Brodie A, Qiu Y (2006) Tyrosine kinase Etk/BMX is up-regulated in human prostate cancer and its overexpression induces prostate intraepithelial neoplasia in mouse. Cancer Res 66(16):8058–8064
Abassi YA, Rehn M, Ekman N, Alitalo K, Vuori K (2003) p130Cas Couples the tyrosine kinase Bmx/Etk with regulation of the actin cytoskeleton and cell migration. J Biol Chem 278(37):35636–35643
Chau CH, Clavijo CA, Deng HT, Zhang Q, Kim KJ, Qiu Y, Le AD, Ann DK (2005) Etk/Bmx mediates expression of stress-induced adaptive genes VEGF, PAI-1, and iNOS via multiple signaling cascades in different cell systems. Am J Physiol Cell Physiol 289(2):C444–C454
Kim B, Breton S (2016) The MAPK/ERK-signaling pathway regulates the expression and distribution of tight junction proteins in the mouse proximal epididymis. Biol Reprod 94(1):22
Li L, Zhao M, Kiernan CH, Castro Eiro MD, van Meurs M, Brouwers-Haspels I, Wilmsen MEP, Grashof DGB, van de Werken HJG, Hendriks RW, Mueller YM, Katsikis PD (2023) Ibrutinib directly reduces CD8+T cell exhaustion independent of BTK. Front Immunol 14:1201415
Lee J, Nicosia M, Hong ES, Silver DJ, Li C, Bayik D, Watson DC, Lauko A, Kay KE, Wang SZ, Johnson S, McGraw M, Grabowski MM, Kish DD, Desai AB, Goodman WA, Cameron SJ, Okada H, Valujskikh A, Fairchild RL, Ahluwalia MS, Lathia JD (2023) Sex-biased T-cell exhaustion drives differential immune responses in glioblastoma. Cancer Discov 13(9):2090–2105
Giakoumettis D, Kritis A, Foroglou N (2018) C6 cell line: the gold standard in glioma research. Hippokratia 22(3):105–112
Parsa AT, Chakrabarti I, Hurley PT, Chi JH, Hall JS, Kaiser MG, Bruce JN (2000) Limitations of the C6/Wistar rat intracerebral glioma model: implications for evaluating immunotherapy. Neurosurgery 47(4):993–9
Sahu U, Barth RF, Otani Y, McCormack R, Kaur B (2022) Rat and mouse brain tumor models for experimental neuro-oncology research. J Neuropathol Exp Neurol 81(5):312–329
Liu J, Liu Z, Zhang J, Chen X, Chen J, Sui L, Yu J (2022) Ibrutinib inhibits angiogenesis and tumorigenesis in a BTK-independent manner. Pharmaceutics 14(9):1876
Segura-Collar B, Garranzo-Asensio M, Herranz B, Hernández-SanMiguel E, Cejalvo T, Casas BS, Matheu A, Pérez-Núñez Á, Sepúlveda-Sánchez JM, Hernández-Laín A, Palma V, Gargini R, Sánchez-Gómez P (2021) Tumor-derived pericytes driven by EGFR mutations govern the vascular and immune microenvironment of gliomas. Cancer Res 81(8):2142–2156
Meredith AM, Dass CR (2016) Increasing role of the cancer chemotherapeutic doxorubicin in cellular metabolism. J Pharm Pharmacol 68(6):729–741
Rivankar S (2014) An overview of doxorubicin formulations in cancer therapy. J Cancer Res Ther 10(4):853–858
Gaillard PJ, Appeldoorn CC, Dorland R, van Kregten J, Manca F, Vugts DJ, Windhorst B, van Dongen GA, de Vries HE, Maussang D, van Tellingen O (2014) Pharmacokinetics, brain delivery, and efficacy in brain tumor-bearing mice of glutathione pegylated liposomal doxorubicin (2B3-101). PLoS ONE 9(1):e82331
Acknowledgements
This work was supported by the NINDS Intramural Research Program. The authors thank Yosuke Mukouyama for advice on experimental designs.
Author information
Authors and Affiliations
Contributions
SL, MK, JK, BF, MC, RR, WJF, MD, BK, DB, KT, NN, PJC and SJ contributed to the experimental design. JK, KT, MC, BF, MD, RR, SL, MK, BK, DB, ML, PJC, and SJ analyzed the imaging of samples and interpreted the findings. All authors have contributed to the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
High BTK expression seen in lymph node TMA tissue (positive control) compared with kidney, liver, colon, lung and soft tissue BTK staining (a). Decreased phospho-ERK expression seen after ibrutinib treatment of rat brain endothelium from 0.5-8 hours after treatment, **p<001 (b). Decreased ZO-1 tight junction expression on human brain endothelial cells seen with higher ibrutinib dosing (c). Ibrutinib significantly decreased rat brain endothelial cell-cell interaction after 4 hours treatment via electron microscopy imaging. 1. Mitochondria, 2. lysosome, 3. cell-cell junction, 4. herolysosome, 5. ribosome, 6. lamellar bodies (d). HEK overexpressing ABCB1/PGP transporter exhibited ibrutinib dose-dependently increased rhodamine accumulation, similar to valspodar (e).
Additional file 2.
Treatment schema for animal model with ibrutinib and doxorubicin therapy (a). No statistical difference seen in model survival with doxorubicin alone or combination therapy (b). Alternative treatment schedules also provided no statistical difference in survival benefit with combination therapy, yet doxil alone provided a trend towards improved survival (c). Magnetic resonance imaging of control (left panel), doxil (left middle panel), ibrutinib (right middle panel) and combination (right panel) demonstrated no statistically significant difference in tumor volumes (d).
Additional file 3.
qPCR Primers.
Additional file 4.
Antibodies for Western blots and IF.
Additional file 5.
Description of S635 glioma cell whole genome sequencing. Variant calls are described for select genes. For H3f3a, H3f3b, Idh1, Idh2, and Tert genes, variants called included only those that render a coding change but no amino acid change. Given this, the S635 glioma cell line can be characterized as IDH wild type. For Atrx, Egfr, and Tp53 genes, variants called included those that render both a coding change and a non-synonymous amino acid change. For Atrx, four single nucleotide variants were called (X:c.70901795:G>T:5.71%; X:c.70930985:G>T,7.41%; X:c.70931078:T>C,20.83%; X:c.70931082:G>C,10.53%) resulting in a non-synonymous impact for multiple transcripts (ENSRNOP00000070457:p.Ser1573Ile, ENSRNOP00000087612:p.Ser1584Ile, ENSRNOP00000087702:p.Ser1546Ile; ENSRNOP00000070457:p.Gly873Cys, ENSRNOP00000087612:p.Gly884Cys, ENSRNOP00000087702:p.Gly846Cys; ENSRNOP00000070457:p.Ser842Pro, ENSRNOP00000087612:p.Ser853Pro, ENSRNOP00000087702:p.Ser815Pro; ENSRNOP00000070457:p.Arg840Ser, ENSRNOP00000087612:p.Arg851Ser, ENSRNOP00000087702:p.Arg813Ser). For Egfr, two single nucleotide variants were called (14:c.91288218:A>G:15.38%; c.14:91341469:A>C) resulting in a non-synonymous impact for multiple transcripts (ENSRNOP00000006087:p.Arg132Gly, ENSRNOP00000078445:p.Arg106Gly, ENSRNOP00000080460:p.Arg106Gly; ENSRNOP00000080460:p.Lys940Thr) along with one insertion (14:91287423^91287424:->T:100%) that possibly impacts splicing for multiple transcripts (ENSRNOT00000006087:c.234+1dupT, ENSRNOT00000097681:c.159+28dupT, ENSRNOT00000111139:c.159+28dupT). For Tp53, two single nucleotide variants were called (10:c.54309391:C>A:6.90%, 10:c.54309411:C>A:8%) resulting in a non-synonymous impact for multiple transcripts (ENSRNOP00000047840:p.Ser313Tyr, ENSRNOP00000074031:p.Ser307Tyr, ENSRNOP00000075724:p.Ser313Tyr, ENSRNOP00000080907:p.Ser286Tyr, ENSRNOP00000089020:p.Ser321Tyr, ENSRNOP00000092831:p.Ser328Tyr; ENSRNOP00000047840:p.Pro320Thr, ENSRNOP00000074031:p.Pro314Thr, ENSRNOP00000075724:p.Pro320Thr, ENSRNOP00000080907:p.Pro293Thr, ENSRNOP00000089020:p.Pro328Thr, ENSRNOP00000092831:p.Pro335Thr).
Additional file 6.
S635 glioma cell whole genome sequencing table.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lim, S., Kwak, M., Kang, J. et al. Ibrutinib disrupts blood-tumor barrier integrity and prolongs survival in rodent glioma model. acta neuropathol commun 12, 56 (2024). https://doi.org/10.1186/s40478-024-01763-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-024-01763-6