Abstract
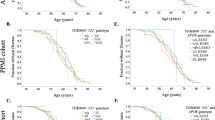
Mitochondrial health is important in ageing and dysfunctional oxidative phosphorylation (OXPHOS) accelerates ageing and influences neurodegeneration. Mitochondrial DNA (mtDNA) codes for vital OXPHOS subunits and mtDNA background has been associated with neurodegeneration; however, no study has characterised mtDNA variation in Progressive supranuclear palsy (PSP) or Corticobasal degeneration (CBD) risk or pathogenesis. In this case–control study, 910 (42.6% male) neurologically-healthy controls, 1042 (54.1% male) pathologically-confirmed PSP cases, and 171 (52.0% male) pathologically-confirmed CBD cases were assessed to determine how stable mtDNA polymorphisms, in the form of mtDNA haplogroups, were associated with risk of PSP, risk of CBD, age of PSP onset, PSP disease duration, and neuropathological tau pathology measures for neurofibrillary tangles (NFT), neuropil threads (NT), tufted astrocytes (TA), astrocytic plaques (AP), and oligodendroglial coiled bodies (CB). 764 PSP cases and 150 CBD cases had quantitative tau pathology scores. mtDNA was genotyped for 39 unique SNPs using Agena Bioscience iPlex technologies and mitochondrial haplogroups were defined to mitochondrial phylogeny. After adjustment for multiple testing, we observed an association with risk of CBD for mtDNA sub-haplogroup H4 (OR = 4.51, P = 0.001) and the HV/HV0a haplogroup was associated with a decreased severity of NT tau pathology in PSP cases (P = 0.0023). Our study reports that mitochondrial genomic background may be associated with risk of CBD and may be influencing tau pathology measures in PSP. Replication of these findings will be important.
Similar content being viewed by others
Introduction
Progressive supranuclear palsy (PSP) and Corticobasal degeneration (CBD) are rare progressive neurodegenerative movement disorders [1, 2]. PSP typically presents clinically with early falls, supranuclear vertical gaze palsy, parkinsonism, and dementia at about 65 years of age [3]. Individuals with CBD often present with progressive asymmetric rigidity and apraxia, loss of coordination, tremor, bradykinesia, akinesia, and occasionally alien limb syndrome [4, 5]. Both diseases have overlap** clinical symptoms with each other and other neurodegenerative diseases, such as Parkinson’s disease (PD) and Alzheimer’s disease (AD) [3, 6,7,8]. This can result in an inaccurate clinical diagnosis; definitive diagnosis is only achieved post-mortem using specific neuropathological diagnostic criteria [9, 10].
Neuropathologically, PSP and CBD are characterised as primary four-repeat (4R) tauopathies, with tau-positive aggregates in the form of neurofibrillary tangles (NFT), tufted astrocytes (TA), astrocytic plaques (AP), neuropil threads (NT), and oligodendroglia coiled bodies (CB), evident in the basal ganglia, diencephalon, and brainstem in PSP [11, 12], and in the substantia nigra and locus coeruleus in CBD [10]. Although generally considered sporadic disorders, MAPT, which encodes microtubule associated protein tau, is consistently documented as a strong genetic risk factor for both PSP and CBD [13, 14], and genetic variation in MAPT influences tau pathology severity in PSP [15]. Other genetic factors have also been identified however they do not explain complete disease aetiology [11, 13, 14, 16].
Age is the major risk factor for PSP and CBD, and mitochondrial health is well-established to contribute significantly to healthy ageing [17]. Mitochondrial dysfunction is also recognised in PSP pathogenesis as well as other clinically similar diseases such as PD and AD [18,19,20,21]. More specifically, defective mitochondria generate reactive oxygen species (ROS) which oxidise proteins, lipids, and nucleic acids, accelerating the ageing process [22]. ROS is suggested to contribute to the accumulation of insoluble proteinaceous deposits, such as Lewy bodies in PD, and senile plaques and NFT in AD [23,24,25], and dysfunction of complex I in the oxidative phosphorylation (OXPHOS) system has been shown to accelerate 4R tau isoform formation in PSP cell lines [26] and is defective in the substantia nigra of PD patients [27, 28].
Mitochondria contain their own double-stranded, circular 16.6 kilo-base pair genome (mtDNA), independent to nuclear DNA (nDNA). mtDNA encodes 37 polypeptides, of which 13 encode vital OXPHOS subunits. An individual cell can contain hundreds to thousands of mtDNA copies which significantly affects cellular metabolic background [29]. mtDNA also contains stable single nucleotide polymorphisms which define individuals to specific haplogroups. Individual mtDNA haplogroups have distinctive metabolic demands [30, 31] and haplogroup bioefficiency has also been shown to affect ageing and risk of develo** many neurodegenerative diseases, including PD and AD [31,32,33,34].
Despite evidence reporting mitochondrial dysfunction in PSP, no studies have examined if mtDNA background influences PSP or CBD risk or if mtDNA variation can contribute to overall tau pathology severity. Thus, herein we examine the association of mtDNA background with PSP and CBD risk and tau pathology severity in two autopsy-defined series.
Methods
Study design
1042 pathologically confirmed PSP cases, 171 pathologically confirmed CBD cases, and 910 neurologically healthy controls were included. All subjects were of self-reported European descent. PSP samples were donated between 1998 and 2016 and CBD samples were collected between 1994 and 2017. All samples were obtained from the CurePSP Brain Bank at Mayo Clinic Jacksonville and were rendered by a single neuropathologist (DWD) following published criteria [8, 10, 35]. Controls were recruited from 1998 to 2015 through the clinical Neurology department at Mayo Clinic Jacksonville, Florida. Demographic information is summarised in Table 1. Age of onset and disease duration was unavailable for 606 PSP and was not available for CBD cases. This study was approved by the Mayo Clinic Institutional Review Board and individual written consent was obtained from all subjects, or their next of kin, prior to commencement.
Neuropathological assessment
Semi-quantitative tau pathology scores in PSP and CBD cases were determined by a single neuropathologist (DWD) using standardized histopathologic methods and phospho-tau immunochemistry. Scores were generated in a subset of cases (PSP: N = 764, CBD: N = 150) on a four-point severity scale (0 = none, 1 = mild, 2 = moderate, and 3 = severe) [36]. All sections from all cases were processed in an identical manner with phospho-tau monoclonal antibody (CP13, from Dr. Peter Davies, Feinstein Institute, Long Island, NY) and immunohistochemistry using a DAKO Autostainer. NFT (PSP: N = 764, CBD: N = 150), CB (PSP: N = 763, CBD: N = 150), TA/AP (PSP: N = 734, CBD: N = 150), and NT (PSP: N = 763, CBD: N = 149) were assessed, and overall scores in 17–20 different, vulnerable neuroanatomical regions in PSP/CBD were generated for each separate tau pathology measure (Additional file 1: Table S1). Mean semi-quantitative measures were then calculated for each PSP/CBD patient across all anatomical regions, where a higher overall score indicated more severe tau pathology. PSP/CBD patients who did not have tau scores in a given region for a given tau pathology measure had their scores imputed by using the mean of the values of the patients in the given disease group (PSP or CBD) who did have scores. Any patients with missing data for > 50% of neuroanatomical regions for a given tau pathology measure were not included in any analysis involving tau pathology measures. PSP and CBD cases were additionally assessed for Alzheimer-type pathology with thioflavin-S fluorescent microscopy. Thioflavin-S predominantly binds to 3R and 4R tau molecules which form paired-helical filaments in AD pathology [37, 38]. As PSP/CBD are pure 4R tauopathies, with straight filament NFT [39], thioflavin S is specifically used to assign Braak NFT stage and should not detect PSP/CBD NFT. Braak NFT stage [40] and Thal amyloid phase [41] were generated for each case based on the density and distribution of plaques and tangles, as previously detailed [42, 43] (Table 1).
DNA preparation and genoty**
Genomic DNA and mtDNA was extracted from peripheral blood lymphocytes from control subjects and from frozen cerebellum brain tissue from PSP and CBD cases using Autogen Flex Star and Autogen 245T (Holliston, MA) methods respectively. mtDNA in all samples was genotyped on two high multiplex custom-designed iPlex assays (consisting of 39 mtDNA SNPs—Fig. 1) using Sequenom MassARRAY iPlex technology (MALDI-TOF MS) and iPlex® Gold chemistry technology [44]. PCR and sequence-specific extension primers were designed through Sequenom’s MassARRAY Typer 4.0 Designer software (version 0.2) (Additional file 1: Table S2), part of the Assay Design Suite (Agena Bioscience™, San Diego, USA), and were manufactured by Integrated DNA Technologies (IDT, San Diego, USA). Genotypes were determined by Sequenom MassARRAY® Bruker mass spectrometry (Agena Bioscience, San Diego, CA, USA) [44] and were accepted if intensities were > 5 from the base line intensity (< 5 was considered noise). Individuals with a genoty** call rate > 95% were accepted and had mtDNA haplogroups determined. Genoty** analysis was conducted using Sequenom’s Typer 4.0 Analyzer software (version 25.73). Additional details are provided in Additional file 1: Supplementary Methods.
Schematic overview of the mitochondrial phylotree and unique SNPs which define European mitochondrial haplogroups. Mitochondrial SNPs highlighted in red indicate SNPs genotyped using Sequenom iPlex technology (Agena Bioscience, San Diego, CA, USA) to determine mitochondrial DNA haplogroups. Adapted from Phylotree [45]
Mitochondrial DNA haplogroup assignment
Mitochondrial DNA haplogroups were manually defined to mitochondrial phylogeny [45, This is the first study to characterise the role of mtDNA background in susceptibility to PSP and CBD and in tau pathology severity in general. Our data suggests that mtDNA haplogroup background may influence CBD risk and may also modify tau aggregation formation in PSP. Though larger validation studies will be key (particularly for CBD due to the smaller sample size of this group), it will also be important for future studies to investigate how established nDNA risk factors, such as the MAPT H1 haplotype, interact with mtDNA genetic background with regard to susceptibility to disease and severity of tau pathology.Conclusions
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PSP:
-
Progressive supranuclear palsy
- CBD:
-
Corticobasal degeneration
- NFT:
-
neurofibrillary tangles
- NT:
-
neuropil threads
- TA:
-
tufted astrocytes
- CB:
-
oligodendroglial coiled bodies
- PD:
-
Parkinson’s disease
- AD:
-
Alzheimer’s disease
- 4R:
-
four-repeat tau isoform
- ROS:
-
reactive oxygen species
- OXPHOS:
-
oxidative phosphorylation
- mtDNA:
-
mitochondrial DNA
- nDNA:
-
nuclear DNA
- MALDI-TOF MS:
-
matrix-assisted laser desorption/ionization mass spectrometry
- OR:
-
odds ratio
- CI:
-
confidence interval
- MT-ND2:
-
NADH dehydrogenase subunit-2
- MT-CYB:
-
cytochrome-b subunit of complex III
- mtSNP:
-
mitochondrial DNA single nucleotide polymorphism
References
Schrag A, Ben-Shlomo Y, Quinn NP (1999) Prevalence of progressive supranuclear palsy and multiple system atrophy: a cross-sectional study. The Lancet 354(9192):1771–1775
Golbe LI (2008) The Epidemiology of Progressive Supranuclear Palsy. Elsevier, Handbook of Clinical Neurology, pp 457–459
Boxer AL, Yu J-T, Golbe LI, Litvan I, Lang AE, Höglinger GU (2017) Advances in progressive supranuclear palsy: new diagnostic criteria, biomarkers, and therapeutic approaches. Lancet Neurol 16(7):552–563
Gibb WRG, Luthert PJ, Marsden CD (1989) Corticobasal degeneration. Brain 112(5):1171–1192
Riley DE, Lang AE, Lewis A, Resch L, Ashby P, Hornykiewicz O, Black S (1990) Cortical-basal ganglionic degeneration. Neurology 40(8):1203–1212
Dugger BN, Tu M, Murray ME, Dickson DW (2011) Disease specificity and pathologic progression of tau pathology in brainstem nuclei of Alzheimer’s disease and progressive supranuclear palsy. Neurosci Lett 491(2):122–126
Fujioka S, Algom AA, Murray ME, Strongosky A, Soto-Ortolaza AI, Rademakers R, Ross OA, Wszolek ZK, Dickson DW (2013) Similarities between familial and sporadic autopsy-proven progressive supranuclear palsy. Neurology 80(22):2076–2078
Höglinger Günter U, Respondek G, Stamelou M, Kurz C, Josephs Keith A, Lang Anthony E, Mollenhauer B, Müller U, Nilsson C, Whitwell Jennifer L, Arzberger T, Englund E, Gelpi E, Giese A, Irwin David J, Meissner Wassilios G, Pantelyat A, Rajput A, Swieten John C, Troakes C, Antonini A, Bhatia Kailash P, Bordelon Y, Compta Y, Corvol JC, Colosimo C, Dickson Dennis W, Dodel R, Ferguson L, Grossman M, Kassubek J, Krismer F, Levin J, Lorenzl S, Morris Huw R, Nestor P, Oertel Wolfgang H, Poewe W, Rabinovici G, Rowe James B, Schellenberg Gerard D, Seppi K, Eimeren T, Wenning Gregor K, Boxer Adam L, Golbe Lawrence I, Litvan I, Null N, Boxer Adam L, Rajput A, Pantelyat A, Antonini A, Lang Anthony E, Giese A, Mollenhauer B, Colosimo C, Kurz C, Nilsson C, Troakes C, Irwin David J, Dickson Dennis W, Gelpi E, Krismer F, Schellenberg Gerard D, Respondek G, Rabinovici G, Wenning Gregor K, Höglinger Günter U, Morris Huw R, Litvan I, Rowe James B, Kassubek J, Corvol JC, Whitwell Jennifer L, Levin J, van Swieten J, Bhatia Kailash P, Josephs Keith A, Seppi K, Golbe Lawrence I, Stamelou M, Grossman M, Nestor P, Dodel R, Lorenzl S, van Eimeren T, Arzberger T, Müller U, Meissner Wassilios G, Poewe W, Oertel Wolfgang H, Compta Y, Bordelon Y (2017) Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov Disord 32(6):853–864
Dickson DW (1999) Neuropathologic differentiation of progressive supranuclear palsy and corticobasal degeneration. J Neurol 246(2):6–15
Dickson DW, Bergeron C, Chin SS, Duyckaerts C, Horoupian D, Ikeda K, Jellinger K, Lantos PL, Lippa CF, Mirra SS, Tabaton M, Vonsattel JP, Wakabayashi K, Litvan I (2002) Office of rare diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 61(11):935–946
Sanchez-Contreras MY, Kouri N, Cook CN, Serie DJ, Heckman MG, Finch NA, Caselli RJ, Uitti RJ, Wszolek ZK, Graff-Radford N, Petrucelli L, Wang L-S, Schellenberg GD, Dickson DW, Rademakers R, Ross OA (2018) Replication of progressive supranuclear palsy genome-wide association study identifies SLCO1A2 and DUSP10 as new susceptibility loci. Mol Neurodegener 13(1):37
Kovacs GG (2015) Invited review: Neuropathology of tauopathies: principles and practice. Neuropathol Appl Neurobiol 41(1):3–23
Ries V, Oertel WH, Höglinger GU (2011) Mitochondrial dysfunction as a therapeutic target in progressive supranuclear palsy. J Mol Neurosci 45(3):684
Kouri N, Ross OA, Dombroski B, Younkin CS, Serie DJ, Soto-Ortolaza A, Baker M, Finch NCA, Yoon H, Kim J, Fujioka S, McLean CA, Ghetti B, Spina S, Cantwell LB, Farlow MR, Grafman J, Huey ED, Ryung Han M, Beecher S, Geller ET, Kretzschmar HA, Roeber S, Gearing M, Juncos JL, Vonsattel JPG, Van Deerlin VM, Grossman M, Hurtig HI, Gross RG, Arnold SE, Trojanowski JQ, Lee VM, Wenning GK, White CL, Höglinger GU, Müller U, Devlin B, Golbe LI, Crook J, Parisi JE, Boeve BF, Josephs KA, Wszolek ZK, Uitti RJ, Graff-Radford NR, Litvan I, Younkin SG, Wang L-S, Ertekin-Taner N, Rademakers R, Hakonarsen H, Schellenberg GD, Dickson DW (2015) Genome-wide association study of corticobasal degeneration identifies risk variants shared with progressive supranuclear palsy. Nat Commun 6:7247
Heckman MG, Brennan RR, Labbé C, Soto AI, Koga S, DeTure MA, Murray ME, Petersen RC, Boeve BF, van Gerpen JA, Uitti RJ, Wszolek ZK, Rademakers R, Dickson DW, Ross OA (2019) Association of MAPT subhaplotypes with risk of progressive supranuclear palsy and severity of tau pathology. JAMA Neurol 76(6):710–717
Chen JA, Chen Z, Won H, Huang AY, Lowe JK, Wojta K, Yokoyama JS, Bensimon G, Leigh PN, Payan C, Shatunov A, Jones AR, Lewis CM, Deloukas P, Amouyel P, Tzourio C, Dartigues JF, Ludolph A, Boxer AL, Bronstein JM, Al-Chalabi A, Geschwind DH, Coppola G (2018) Joint genome-wide association study of progressive supranuclear palsy identifies novel susceptibility loci and genetic correlation to neurodegenerative diseases. Mol Neurodegener 13(1):41
Keogh MJ, Chinnery PF (2015) Mitochondrial DNA mutations in neurodegeneration. Biochim Biophys Acta Bioenergetics 1847(11):1401–1411
Albers DS, Swerdlow RH, Manfredi G, Gajewski C, Yang L, Parker WD Jr, Beal MF (2001) Further evidence for mitochondrial dysfunction in progressive supranuclear palsy. Exp Neurol 168(1):196–198
Rego AC, Oliveira CR (2003) Mitochondrial dysfunction and reactive oxygen species in excitotoxicity and apoptosis: implications for the pathogenesis of neurodegenerative diseases. Neurochem Res 28(10):1563–1574
Swerdlow RH, Golbe LI, Parks JK, Cassarino DS, Binder DR, Grawey AE, Litvan I, Bennett JP Jr, Wooten GF, Parker WD (2000) Mitochondrial dysfunction in cybrid lines expressing mitochondrial genes from patients with progressive supranuclear palsy. J Neurochem 75(4):1681–1684
Angelova PR, Barilani M, Lovejoy C, Dossena M, Viganò M, Seresini A, Piga D, Gandhi S, Pezzoli G, Abramov AY, Lazzari L (2018) Mitochondrial dysfunction in Parkinsonian mesenchymal stem cells impairs differentiation. Redox Biol 14:474–484
Roy J, Galano J-M, Durand T, Guennec J-YL, Lee JC-Y (2017) Physiological role of reactive oxygen species as promoters of natural defenses. FASEB J 31(9):3729–3745
Choi J, Rees HD, Weintraub ST, Levey AI, Chin L-S, Li L (2005) Oxidative modifications and aggregation of Cu, Zn-superoxide dismutase associated with Alzheimer and Parkinson diseases. J Biol Chem 280(12):11648–11655
Giasson BI, Ischiropoulos H, Lee VMY, Trojanowski JQ (2002) The relationship between oxidative/nitrative stress and pathological inclusions in Alzheimer’s and Parkinson’s diseases 1,211 Guest Editors: Mark A. Smith and George Perry22. This article is part of a series of reviews on “Causes and Consequences of Oxidative Stress in Alzheimer’s Disease”. Free Radic Biol Med 32(12):1264–1275
Jenner P (2003) Oxidative stress in Parkinson’s disease. Ann Neurol 53(S3):S26–S38
Bruch J, Xu H, De Andrade A, Höglinger G (2014) Mitochondrial complex 1 inhibition increases 4-repeat isoform tau by SRSF2 upregulation. PLoS ONE 9(11):e113070
Schapira AHV, Cooper JM, Dexter D, Clark JB, Jenner P, Marsden CD (1990) Mitochondrial complex I deficiency in Parkinson’s disease. J Neurochem 54(3):823–827
Puspita L, Chung SY, Shim J-W (2017) Oxidative stress and cellular pathologies in Parkinson’s disease. Mol Brain 10(1):53
Malik AN, Czajka A (2013) Is mitochondrial DNA content a potential biomarker of mitochondrial dysfunction? Mitochondrion 13(5):481–492
Gómez-Durán A, Pacheu-Grau D, López-Gallardo E, Díez-Sánchez C, Montoya J, López-Pérez MJ, Ruiz-Pesini E (2010) Unmasking the causes of multifactorial disorders: OXPHOS differences between mitochondrial haplogroups. Hum Mol Genet 19(17):3343–3353
Chinnery PF, Gomez-Duran A (2018) Oldies but goldies mtDNA population variants and neurodegenerative diseases. Front Neurosci 12:682
Latsoudis H, Spanaki C, Chlouverakis G, Plaitakis A (2008) Mitochondrial DNA polymorphisms and haplogroups in Parkinson’s disease and control individuals with a similar genetic background. J Hum Genet 53(4):349–356
Ghezzi D, Marelli C, Achilli A, Goldwurm S, Pezzoli G, Barone P, Pellecchia MT, Stanzione P, Brusa L, Bentivoglio AR, Bonuccelli U, Petrozzi L, Abbruzzese G, Marchese R, Cortelli P, Grimaldi D, Martinelli P, Ferrarese C, Garavaglia B, Sangiorgi S, Carelli V, Torroni A, Albanese A, Zeviani M (2005) Mitochondrial DNA haplogroup K is associated with a lower risk of Parkinson’s disease in Italians. Eur J Hum Genet 13(6):748–752
Ridge PG, Maxwell TJ, Corcoran CD, Norton MC, Tschanz JT, O’Brien E, Kerber RA, Cawthon RM, Munger RG, Kauwe JSK (2012) Mitochondrial genomic analysis of late onset Alzheimer’s disease reveals protective haplogroups H6A1A/H6A1B: the cache county study on memory in aging. PLoS ONE 7(9):e45134
Litvan I, Hauw JJ, Bartko JJ, Lantos PL, Daniel SE, Horoupian DS, McKee A, Dickson D, Bancher C, Tabaton M, Jellinger K, Anderson DW (1996) Validity and reliability of the preliminary NINDS neuropathologic criteria for progressive supranuclear palsy and related disorders. J Neuropathol Exp Neurol 55(1):97–105
Koga S, Parks A, Kasanuki K, Sanchez-Contreras M, Baker MC, Josephs KA, Ahlskog JE, Uitti RJ, Graff-Radford N, van Gerpen JA, Wszolek ZK, Rademakers R, Dickson DW (2017) Cognitive impairment in progressive supranuclear palsy is associated with tau burden. Movement Disord 32(12):1772–1779
Buée L, Delacourte A (1999) Comparative biochemistry of tau in progressive supranuclear palsy, corticobasal degeneration, FTDP-17 and Pick’s disease. Brain Pathol (Zurich, Switzerland) 9(4):681–693
Pérez M, Valpuesta JM, de Garcini EM, Quintana C, Arrasate M, López Carrascosa JL, Rábano A, García de Yébenes J, Avila J (1998) Ferritin is associated with the aberrant tau filaments present in progressive supranuclear palsy. Am J Pathol 152(6):1531–1539
Santa-María I, Pérez M, Hernández F, Avila J, Moreno FJ (2006) Characteristics of the binding of thioflavin S to tau paired helical filaments. J Alzheimers Dis 9(3):279–285
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82(4):239–259
Thal DR, Rüb U, Orantes M, Braak H (2002) Phases of Aβ-deposition in the human brain and its relevance for the development of AD. Neurology 58(12):1791–1800
Murray ME, Lowe VJ, Graff-Radford NR, Liesinger AM, Cannon A, Przybelski SA, Rawal B, Parisi JE, Petersen RC, Kantarci K, Ross OA, Duara R, Knopman DS, Jack CR Jr, Dickson DW (2015) Clinicopathologic and 11C-Pittsburgh compound B implications of Thal amyloid phase across the Alzheimer’s disease spectrum. Brain 138(Pt 5):1370–1381
Zhao N, Liu C-C, Van Ingelgom AJ, Linares C, Kurti A, Knight JA, Heckman MG, Diehl NN, Shinohara M, Martens YA, Attrebi ON, Petrucelli L, Fryer JD, Wszolek ZK, Graff-Radford NR, Caselli RJ, Sanchez-Contreras MY, Rademakers R, Murray ME, Koga S, Dickson DW, Ross OA, Bu G (2018) APOE ε2 is associated with increased tau pathology in primary tauopathy. Nature Communications 9(1):4388
Gabriel S, Ziaugra L, Tabbaa D (2009) SNP genoty** using the sequenom MassARRAY iPLEX platform. Curr Protoc Hum Genet 60(1):2.12.1–2.12.18
van Oven M, Kayser M (2009) Updated comprehensive phylogenetic tree of global human mitochondrial DNA variation. Hum Mutat 30(2):E386–E394
Lott MT, Leipzig JN, Derbeneva O, **e HM, Chalkia D, Sarmady M, Procaccio V, Wallace DC (2013) mtDNA variation and analysis using mitomap and mitomaster. Curr Protoc Bioinform 44(123):1–26
Torroni A, Huoponen K, Francalacci P, Petrozzi M, Morelli L, Scozzari R, Obinu D, Savontaus ML, Wallace DC (1996) Classification of European mtDNAs from an analysis of three European populations. Genetics 144(4):1835–1850
Barshad G, Zlotnikov-Poznianski N, Gal L, Schuldiner M, Mishmar D (2019) Disease-causing mutations in subunits of OXPHOS complex I affect certain physical interactions. Sci Rep 9(1):9987
Cerezo M, Černý V, Carracedo Á, Salas A (2009) Applications of MALDI-TOF MS to large-scale human mtDNA population-based studies. Electrophoresis 30(21):3665–3673
Acknowledgements
We would like to thank the patients, donors, and caregivers who participated in this research, without who this work would not have been possible. We would like to acknowledge the continuous commitment, technical support and teamwork offered by Linda G. Rousseau, Virginia R. Phillips, and Monica Castanedes-Casey for tissue characterization. This work was supported in part by; the Mayo Clinic Florida Tau Center WithOut Walls (NINDS U54-NS100693); - an American Parkinson Disease Association (APDA), Mayo Clinic Information and Referral Center, and an APDA Center for Advanced Research. Samples included in this study were clinical controls or brain donors to the brain bank at Mayo Clinic in Jacksonville which is supported by CurePSP and the Tau Consortium. RRV designed the genotype assays and performed all laboratory analysis whilst MGH conducted, and is responsible for, all statistical data analysis. OAR had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The funding organizations and sponsors had no role in any of the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Funding
OAR and DWD are both supported by NINDS Tau Center without Walls Program (U54-NS100693) and NIH (UG3-NS104095). OAR is supported by NIH (P50-NS072187; R01-NS078086; U54-NS100693; U54-NS110435), DOD (W81XWH-17-1-0249) The Michael J. Fox Foundation, The Little Family Foundation, the Mayo Clinic Foundation, and the Center for Individualized Medicine. DWD receives research support from the NIH (P50-AG016574; U54-NS100693; P01-AG003949), CurePSP, the Tau Consortium, and the Robert E. Jacoby Professorship. ZKW is partially supported by the Mayo Clinic Center for Regenerative Medicine, the gifts from The Sol Goldman Charitable Trust, and the Donald G. and Jodi P. Heeringa Family, the Haworth Family Professorship in Neurodegenerative Diseases fund, and The Albertson Parkinson’s Research Foundation. SK is supported by a post-doctoral fellowship from the Karin & Sten Mortstedt CBD Solutions AB.
Author information
Authors and Affiliations
Contributions
RRV designed the genoty** assays, performed all genoty** and quality control assessments, and drafted the manuscript. NT assisted with genoty** some samples. MGH and PWJ performed all statistical analysis and MGH provided manuscript improvements. AISB provided training for genoty** design and methods. RLW prepared DNA extracts for all samples from donated human tissues. SK and DWD provided brain tissue samples for all cases and DWD performed neuropathological assessments of PSP and CBD cases. RJU and ZKW recruited clinical patients and organised blood collections. OAR lead the study and oversaw all method developments and analysis and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Mayo Clinic Institutional Review Board and individual written consent was obtained from all participants, or their next of kin, prior to commencement.
Consent for publication
Not applicable.
Competing interests
ZKW serves as PI or Co-PI on Abbvie, Inc. (M15-562 and M15-563), Biogen, Inc. (228PD201) Grant, and Biohaven Pharmaceuticals, Inc. (BHV4157-206 and BHV3241-301). He serves as PI of the Mayo Clinic American Parkinson Disease Association (APDA) Information and Referral Center, and as Co-PI of the Mayo Clinic APDA Center for Advanced Research. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.:
Supplementary tables, figures, and methods.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Valentino, R.R., Tamvaka, N., Heckman, M.G. et al. Associations of mitochondrial genomic variation with corticobasal degeneration, progressive supranuclear palsy, and neuropathological tau measures. acta neuropathol commun 8, 162 (2020). https://doi.org/10.1186/s40478-020-01035-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-020-01035-z