Abstract
Background
Activation of the aryl hydrocarbon receptor (AhR) can alter diurnal rhythms including those for innate lymphoid cell numbers, cytokine and hormone levels, and feeding behaviors. Because immune responses and antibody levels are modulated by exposure to AhR agonists, we hypothesized that some of the variation previously reported for the effects of AhR activation on fecal secretory immunoglobulin A (sIgA) levels could be explained by dysregulation of the diurnal sIgA rhythm.
Methods
C57Bl/6 J mice were exposed to peanut oil or 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD, 10 or 40 μg/Kg) and fecal sIgA levels were determined in samples collected every 4 h over 4 days.
Results
Fecal sIgA concentrations were not significantly different between light and dark phases of the photoperiod in either male or female mice, and there were no significant circadian rhythms observed, but TCDD exposure significantly altered both fecal mesor sIgA and serum IgA concentrations, in parallel, in male (increased) and female (biphasic) mice.
Conclusions
AhR activation can contribute to the regulation of steady state IgA/sIgA concentrations.
Similar content being viewed by others
Background
Immunoglobulin A (IgA) is the most abundant antibody isotype produced by B cells in the gut lamina propria, and IgA is the predominant isotype found in feces [38]. Export of IgA into the intestinal lumen is performed predominantly by mucosal epithelial cells. J chain-containing IgA multimers in the lamina propria are bound by poly-Ig receptors (pIgRs) on the basolateral side of epithelial cells. These IgA-J chain-pIgR complexes undergo transcytosis to the luminal side where proteolytic cleavage results in the release of secretory IgA (sIgA) into the intestinal lumen [34, 40].
sIgA acts in several ways to influence health. It plays a role in protection against mucosally-transmitted pathogens [1, 51, 58, 62, 67] and can influence the composition and function of commensal microbe populations in the gut [15, 24, 34, 47, 73]. In turn, gut microbiota can influence fecal sIgA concentrations and IgA production [17, 41, 64]. Moreover, components of food (e.g., peanuts, shellfish) can stimulate IgA production; sIgA may function to exclude those materials from the body and protect against development of allergies [59]. Like hormones, feeding behaviors, and metabolic processes, secretion and/or concentrations of fecal sIgA have been reported to vary with diurnal rhythmicity [6, 13, 25, 29, 35, 71].
The aryl hydrocarbon receptor (AhR) is a ligand-activated transcription factor of the Per-ARNT-Sim family of proteins that regulates cellular function through a canonical genomic pathway and several non-genomic pathways. The AhR is present in most cells of the body, but the level of expression can vary with cell type, location, and developmental state [16, 63]. In the absence of ligand binding, the AhR traffics in and out of the nucleus but exists primarily in the cytosol as a complex with chaperone proteins [12]. Ligand binding enhances retention of the AhR in the nucleus. Dimerization with the AhR nuclear translocator (ARNT) protein allows AhR:ARNT to function as a DNA binding complex that targets dioxin response elements, which regulate the expression of multiple genes associated with metabolism, circadian rhythms, immune function, hormone production, development, and other processes [37, 60, 66, 74, 75]. The AhR can also regulate cellular functions through non-genomic mechanisms such as via a ligand-activated E3 ubiquitin ligase activity and by regulating a cytosolic Src kinase pathway [36, 44, 52].
The AhR can be activated by a large number of chemically diverse agonists including drugs (e.g., leflunomide), environmental chemicals (e.g., benzo(a)pyrene), tryptophan metabolites (e.g., kynurenine) or photodegradation products (e.g., 6-formylindolo(3,2-b)carbazole), lipoxin A4, metabolites of hemoglobin, as well as various plant-derived compounds that are commonly found in food and the microbially-derived metabolites of those compounds [43, 55]. AhR agonist activity has been demonstrated in human blood using reporter assays, and these studies showed that the levels of AhR agonists changed significantly due to changes in diet alone [8, 57]. The function of the AhR has been most widely studied using the ligand 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD), a compound that has high AhR affinity and agonist activity [2, 60].
Activation of the AhR suppresses B cell activation and class switch recombination [31, 63, 68, 78]. These effects have been proposed as the reason for the widely reported suppression of systemic primary antibody responses after AhR activation in both male and female animals [14, 26, 52, 61]. Whereas antigen-specific serum immunoglobulin M (IgM) and immunoglobulin G (IgG) responses have been universally shown to be decreased by AhR activation, Warren et al. [72] found that blood levels of influenza-specific IgA were significantly increased after TCDD exposure in female mice. Interestingly, they also showed that influenza-specific sIgA levels were unchanged by TCDD exposure in bronchoalveolar lavage fluid. Another paradoxical observation was made by Chmill et al. [7], who found that ovalbumin-specific fecal sIgA concentrations were increased by TCDD exposure in female mice. The effects of AhR activation on total (steady state) sIgA concentrations have also been examined. Zhang et al. [77] found significantly elevated fecal sIgA levels in male mice exposed to 2,3,7,8-tetrachlorodibenzofuran (TCDF) within 7 days of oral treatment. Similarly, Benson and Shepherd [3] found significantly elevated fecal sIgA levels up to 13 days after exposure to TCDD in a mouse colitis model using both male and female mice. Interestingly, Culbreath et al. [9] showed that depletion of AhR agonists from feed could reduce fecal sIgA concentrations in mice. These findings suggest that blood IgA and/or secreted sIgA responses may be differentially impacted by AhR activation in comparison to IgM and IgG.
Activation of the AhR alters diurnal rhythms in a way that is consistent with inhibition of the circadian clock [65, 74, 75]. In the gut, AhR activation leads to altered rhythms for innate lymphoid cell numbers and cytokine production [18]. AhR activation also dysregulates diurnal feeding behaviors and blood rhythms for corticosterone, prolactin, thyroid hormone, and melatonin [23, 49, 50]. Because sIgA concentrations have been reported to vary with diurnal rhythmicity [29, 71], we hypothesized that some of the variation reported for the effects of AhR activation on fecal sIgA levels could be explained by dysregulation of the sIgA rhythm. Our study found that fecal sIgA concentrations were not significantly different between light and dark phases of the photoperiod for either male or female mice, and there was no significant circadian rhythmicity. However, TCDD exposure significantly altered fecal sIgA concentrations in a sex- and dose-dependent manner.
Methods
Ethics statement
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Institutional Animal Care and Use Committee of the University of Northern Colorado. All efforts were made to minimize suffering. This study is reported in accordance with ARRIVE 2.0 guidelines [46].
Animal maintenance
C57Bl/6 J mice were maintained at the Animal Research Facility, University of Northern Colorado, on a standard 12-h light/dark (L/D) cycle with lights on at 0700 h Mountain Standard Time (Zeitgeber time, ZT0) and lights off at 1900 h Mountain Standard Time (ZT12). In Experiment 1 (diurnal rhythmicity), mice were housed individually for a period of approximately 5 days in polypropylene shoebox-style cages that had been modified such that approximately 80% of the floor space was comprised of a galvanized wire mesh (1/8th inch mesh size -- sufficient to allow fecal pellets to pass through). In Experiment 2 (Leishmania infection), animals were housed individually in Optimice® cages containing Tek-Fresh bedding (#7099, Envigo). All animals were provided with food (Rodent Diet 2016, Envigo) and deionized water ad libitum. Animals were euthanized with an overdose of CO2.
Treatments and infections
Experiment 1 (diurnal rhythmicity). TCDD was purchased from Cambridge Isotope Laboratories (Andover, MA) and solutions were prepared in peanut oil as described previously [11]. The concentration of TCDD was confirmed by gas chromatography using the method of [30]. Each animal (36 total, 18 of each sex, 6 per treatment group within each sex) was randomly assigned to a treatment group and was given peanut oil (vehicle) or TCDD (in peanut oil) at one of various doses by gavage (0.01 mL/g body weight). TCDD is a highly lipophilic compound that is poorly metabolized and which results in a half-life of approximately 8-11 days in C57BL/6 mice [39]. Thus, TCDD activation of the AhR in vivo is persistent.
Experiment 2 (Leishmania infection). Each animal (18 total, 9 per treatment group) was randomly assigned to a treatment group and was given peanut oil or TCDD as in Experiment 1. Leishmania major (LV39, RHO/SU/59/P, Neal, or P strain) promastigotes were maintained by biweekly passage through C57Bl/6 mice followed by re-isolation from foot lesions on a rotator at room temperature in Schnieder’s Insect medium supplemented with 10% (v/v) heat-inactivated fetal bovine serum, 5 μg/mL hemin, 50 μg/mL gentamycin, 100 U/mL penicillin, 100 μg/mL streptomycin, 10 mM Hepes, 116 μg/mL arginine, 36 μg/mL asparagine, 110 μg/mL sodium pyruvate, and 292 μg/mL L-glutamine [56]. One day after vehicle or TCDD treatment, mice were anesthetized and then infected by subcutaneous injection of 50 μL phosphate-buffered saline (PBS) containing 1 × 106 stationary-phase promastigotes into one rear foot pad.
Feces and serum collection
Experiment 1 (diurnal rhythmicity). Mice were acclimated to individual housing for 7 days, subsequently treated with vehicle or TCDD in the morning (approximately 0900 h), and 27 hours later each mouse was placed into a wire mesh-bottomed cage which was suspended above a piece of absorbent paper. At 1400 h on that day, a minimum of two fecal pellets were collected from the paper below each suspended cage and stored frozen (− 20 °C). A fresh piece of absorbent paper was then placed under each cage. In this way, feces were collected every 4 hours for 4 days with minimal interaction between animals and investigators. In the afternoon of the last day (1300 h - 1500 h), each animal was euthanized, and blood was collected. Serum was isolated and stored frozen (− 20 °C).
Experiment 2 (Leishmania infection). L. major-infected mice were euthanized in the afternoon (1300 h - 1500 h) on day 21 after infection (day 22 after vehicle or TCDD treatment). Blood was collected immediately by cardiac puncture and placed into serum separator vials (BD Biosciences). Serum was isolated and stored frozen (− 20 °C). A volume of feces approximating two pellets was collected from the colon of each mouse and frozen prior to processing.
Analysis of fecal and serum antibodies
Feces were thawed and extracted in PBS containing 1:100 protease inhibitor cocktail (P8340, Sigma-Aldrich Company) as described by Lycke et al. [33] Fecal extract was stored frozen (− 20 °C) prior to analysis. Antibody levels in dilutions of serum or fecal extract were determined by enzyme-linked immunosorbent assay (ELISA) using ELISA plates (Nunc MaxiSorp™ or equivalent) and the methods described previously [5, 33, 76]. Highly isotype-specific capture (unlabeled, #1040-01, Southern Biotech) and detection (biotinylated, #1040-08, Southern Biotech) goat anti-mouse antibodies were used with streptavidin-conjugated horseradish peroxidase (#443066, BD Biosciences), tetramethylbenzidine and hydrogen peroxide substrates (#5120-0047, Vector Laboratories), a SpectraMax 190 absorbance plate spectrophotometer (Molecular Devices), and SoftMax Pro software (ver. 5.4.1, Molecular Devices LLC). In Experiment 1 (diurnal rhythmicity), total IgA concentrations were estimated from standard curves generated using purified mouse monoclonal antibodies (#553476, mouse IgA-kappa, BD Biosciences). In Experiment 2 (Leishmania infection), the IgA level of each mouse was collected as the optical density value measured by the spectrophotometer.
Statistical analysis
In experiments examining diurnal rhythmicity, feces were collected from each of six animals per treatment group every 4 hours over 4 days. Fecal samples collected at the same time each day were considered replicates in accordance with guidelines set forth by Refinetti et al. [53] for assessing baseline diurnal rhythm presence/absence in the control group. To facilitate the analysis of the control and TCDD-exposed groups in the same statistical model, we expanded this replicate sampling approach to all mice in the study. These replicate values were averaged resulting in a sample size of n = 6 at each time point. Statistics regarding rhythmicity were calculated using the Cosinor program [53]. Other statistical analyses to identify differences between treatment groups or sample types using mixed analyses of variance were performed using SAS (ver. 9.4, SAS Institute Inc.) and graphically depicted using SigmaPlot (ver. 14, Systat Software). Hypothesis testing was performed by analysis of variance combined with post hoc all-pairwise t-tests to identify means that were significantly different (p < 0.05) using a stringency no lower than the Tukey test.
Results
Experiment 1: sIgA and IgA in female and male mice after TCDD exposure
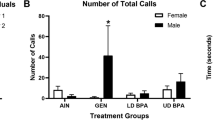
Beginning 1 day after vehicle or TCDD treatment, feces were collected every 4 hours for 4 days and analyzed for sIgA concentration. IgA levels in serum were determined at the end of the 4-day period. As shown in Figs. 1A and 2A, the highest sIgA levels in the feces of vehicle-treated control mice, (both female and male) were during the dark phase of the daily photoperiod. However, there were no significant differences between the mean values for the light and dark phases of either sex (Table 1). In addition, no significant circadian rhythmicity for fecal sIgA values in vehicle-treated animals of either sex was detected (Table 2). Among TCDD-treated animals at either dose (10 or 40 μg/Kg body weight), there were similarly no significant differences between sIgA mean values for the light and dark phases in either sex, and there was no significant circadian sIgA rhythmicity identified in either sex (Tables 1 & 2). However, when the - mesor values (arithmetic mean of all measured values) were calculated for female mice (Fig. 1B), a significant decrease of sIgA levels compared to vehicle-treated mice was observed at a moderate dose of 10 μg/Kg TCDD, whereas a significant increase compared to vehicle-treated mice was observed at a high dose of 40 μg/Kg. A different dose-response was observed in male mice (Fig. 2B), such that significantly higher fecal sIgA mesor values were observed in males treated with either the 10 or 40 μg/Kg TCDD dose compared to vehicle-treated controls. Serum IgA levels paralleled fecal mesor values in both female and male mice (Figs. 1C & 2C). Females given the lower TCDD dose had significantly lower serum IgA levels relative to controls, whereas females in the high dose group had significantly higher serum IgA levels relative to controls. Male mice contained higher serum IgA levels if given the low TCDD dose (not significant), and males in the high TCDD dose group showed significantly higher serum IgA levels.
sIgA and IgA levels after TCDD exposure in female mice. Mice were given vehicle or TCDD (n = 6 per treatment group), rested for 1 day, and then feces were collected at 4-hour intervals for 4 days as described in the Methods. A Mean fecal IgA levels (+ and/or – SEM) at each daily time-point. B Mesor fecal IgA values (+ SEM). C Mean serum IgA levels (+ SEM) on day 5. Different letters indicate means that are significantly different at the same time-point (p < 0.05). Abbreviations: immunoglobulin A, IgA; standard error of the mean, SEM; 2,3,7,8-tetrachlorodibenzo-p-dioxin, TCDD
sIgA and IgA levels after TCDD exposure in male mice. Mice were given vehicle or TCDD (n = 6 per treatment group), rested for 1 day, and then feces were collected at 4-hour intervals for 4 days as described in the Methods. A Mean fecal IgA levels (+ and/or – SEM) at each daily time-point. B Mesor fecal IgA values (+ SEM). C Mean serum IgA levels (+ SEM) on day 5. Different letters indicate means that are significantly different at the same time-point (p < 0.05). Abbreviations: immunoglobulin A, IgA; standard error of the mean, SEM; 2,3,7,8-tetrachlorodibenzo-p-dioxin, TCDD
Experiment 2: sIgA and IgA in Leishmania-infected female mice after TCDD exposure
We reported previously [5] that a single dose of TCDD (40 μg/Kg) given to female C57Bl/6 1 day prior to foot pad infection with L. major resulted in over 60% suppression of serum L. major-specific antibody levels (all isotypes) 3 weeks after infection. In this current study, using the same treatment and infection regimen, we were unable to detect L. major-specific sIgA in the feces of control or TCDD-treated female mice when sample collections were made in the early afternoon (1300 h - 1500 h). However, we did find that total fecal sIgA and total serum IgA levels were readily detected. As shown in Fig. 3A, exposure to TCDD at a high dose (40 μg/Kg) resulted in a significant increase of total fecal sIgA levels 3 weeks after exposure by approximately 1.6-fold, relative to control animals. In contrast, TCDD exposure had no significant impact on total serum IgA levels (Fig. 3B).
sIgA and IgA levels after 3 weeks in female mice. Mice were given vehicle or TCDD (n = 9 per treatment group) and then infected with L. major the following day as described in Methods. Feces and serum were collected 21 days after infection. The mean optical density (OD) values for IgA (+ SEM) are shown for A feces and B serum. * Indicate a mean that is significantly different from peanut oil controls (0 μg/Kg TCDD, p < 0.05). Abbreviations: immunoglobulin A, IgA; Leishmania major, L. major; optical density, OD; standard error of the mean, SEM; 2,3,7,8-tetrachlorodibenzo-p-dioxin
Discussion
To examine the diurnal variation of total (steady state) fecal sIgA levels in mice, we collected fecal pellets from animals of each sex every 4 hours over 4 days. In control (vehicle-treated) mice, we found no significant diurnal variation of fecal sIgA concentrations in either sex (Figs. 1A & 2A, Tables 1 & 2). These results contrasted with those from previous studies that suggested sIgA diurnal rhythms are present in saliva and feces of both male and female mice, with peak sIgA concentrations found during the light phase [6, 29, 71]. It should be noted that these previous studies did not collect samples repeatedly from the same animals over multiple days as recommended for modeling rhythmicity [53]. Given that the total fecal mass produced by rodents increases during the dark phase when they are most active [[13]; C. Foxx, personal observation], the concentration of sIgA in feces may not be reflective of the amount excreted during different times of the day. Indeed, when sIgA concentrations and fecal masses were used to calculate sIgA excretion rates in rats, peak excretion was found to occur during the dark phase [13, 25, 48, 54]. For this reason, the total fecal sIgA excreted by mice in our study most likely occurred during the dark phase.
The only significant effects of TCDD exposure on fecal sIgA concentrations in Experiment 1 of this study were for mesor values which changed in a dose- and sex-dependent manner (Figs. 1B & 2B). These results were paralleled by similar significant changes in serum IgA concentrations in both sexes (Figs. 1C & 2C). As discussed in Background, sIgA has been shown to provide protection against some mucosally-transmitted pathogens, to regulate gut microbe populations, and to potentially protect against development of allergies [1, 15, 24, 34, 47, 51, 58, 59, 62, 67, 73]. Extrapolation of our results might suggest that AhR activation could either inhibit or enhance resistance to intestinal pathogens and tolerance to allergens, depending on the agonist and its dose. However, because of the complexity of immune regulation and disease resistance, experimental evidence obtained using disease models would be more appropriate to explore such possibilities. Recent studies demonstrate that gut microbial community dynamics are influenced by the expression and activation of the AhR [42, 77]. Because members of the gut microbiota can influence fecal sIgA concentrations and IgA production [17, 41, 64], one explanation for the altered sIgA levels seen here in this study could be indirect regulation due to altered gut microbe populations. Alternatively, because sIgA can influence the composition and function of both pathogenic and commensal microbe populations [15, 24, 34, 47, 73], altered sIgA concentrations may be responsible, at least in part, for AhR-mediated changes in gut microbe diversity.
The impact of AhR activation on total fecal sIgA concentrations was examined previously by three different research groups. Kinoshita et al. [28] were the first to report a significant alteration, and they found that TCDD exposure (up to 20 μg/Kg body weight) dose-dependently decreased fecal sIgA concentrations in female C57Bl/6 mice, an effect that persisted for up to 3 weeks. Interestingly, Benson and Shepherd [3] found significantly elevated fecal sIgA levels up to 13 days after exposure to TCDD (30 μg total dose) in a mouse colitis model using both male and female C57Bl/6 mice. Similarly, Zhang et al. [77] found significantly elevated fecal sIgA levels within 7 days of treatment in male C57Bl/6 mice exposed to TCDF (24 μg/Kg total dose) or 2.4 μg/Kg TEQ [4]). For female mice, the results of our study are consistent with each of these previous studies, and collectively these results suggest that sIgA levels can be both reduced and increased by AhR activation, with the specific effect being dependent upon the dose of the AhR agonist as follows: 1) low to moderate doses of TCDD (≤ 20 μg/Kg) suppress fecal sIgA concentrations ([28], and Fig. 1B), but 2) high doses of TCDD (≥ 30 μg/Kg) enhance fecal sIgA concentrations ([3], and Fig. 1B). In male mice, the results are less clear. Ishikawa et al. [22] found that male pups exposed to TCDD through nursing had significantly lower sIgA in their feces (the mothers were exposed to an undisclosed “low dose” of TCDD, possibly 1 μg/Kg). In contrast, adult male mice given an AhR activating dose of 2.4 μg/Kg TEQ or higher experienced elevated sIgA levels within 2 weeks ([3, 77]; Figs. 1B & 2B). These results suggest that male mice may also experience a dose-dependent dichotomous impact on total fecal sIgA concentrations after AhR activation. However, the data also suggest that male mice may display a greater sensitivity than female mice to AhR activation, and the threshold for transition from suppression to enhancement is less definitive. It must be acknowledged that the only antibody isotype we examined in feces was IgA, and the possibility exists that other fecal antibody isotypes may be similarly impacted by TCDD exposure.
Data from several studies suggest that the sensitivity of mice to AhR-mediated immune regulation can depend on the sex of the animal [20, 27, 70]. One study examined a potential mechanism for this sex-dependent variation [10]. In that study, a greater sensitivity of male C57Bl/6 mice to suppression of an allogeneic graft rejection response was observed after AhR activation with 3,4,5,3′4’5′-hexachlorobiphenyl (HxCB, 10 mg/Kg). They found that castrated male mice were no more sensitive to HxCB-induced immune suppression than female mice. The authors suggested that AhR activation may increase the sensitivity of the immune system to testes-derived factor(s), and/or that HxCB treatment alters the production of testes-specific immunomodulatory factor(s). Given that blood testosterone levels were significantly reduced by HxCB-treatment in sham-castrated male mice, testosterone is not a likely contributor to altered immunity in this model. The potential effect of HxCB exposure on other hormones and testes-derived immunomodulatory factors remain to be seen, and further exploration of the mechanisms underlying AhR-sex interactions is warranted.
AhR activation causes suppression of naive B cell activation and suppression of class switch recombination from IgM to IgG and IgA [68, 78]. Therefore, a reasonable expectation could be to find significantly lower concentrations of serum antibodies in mice after TCDD exposure. This has been the exclusive observation after AhR activation for non-IgA total antibody levels using multiple models [45, 79] as well as for total IgA levels under some AhR agonist exposure regimens as discussed above. It has also been the exclusive observation for antigen-specific non-IgA isotypes after antigen challenge [19, 21, 32]. However, for antigen-specific IgA responses, the opposite appears to occur. Using a female mouse influenza infection model, Warren et al. and Vorderstrasse et al. [69, 72] independently found that TCDD exposure significantly elevated influenza-specific blood IgA levels at doses of 10 μg/Kg and lower (lower than those shown here) to elevate total IgA concentrations. Given that per cell antibody production has been found to be unaltered by AhR activation [78], a clear mechanistic explanation for increasing either blood or fecal IgA levels is lacking.
Conclusions
AhR activation can contribute to the regulation of steady-state IgA/sIgA concentrations.
Availability of data and materials
The datasets used and/or analyzed during the current study are included as supplemental materials.
Abbreviations
- AhR:
-
Aryl hydrocarbon receptor
- ARNT:
-
AhR nuclear translocator
- ELISA:
-
Enzyme-linked immunosorbent assay
- HxCB:
-
3,4,5,3′4’5′-hexachlorobiphenyl
- IgA:
-
Immunoglobulin A
- IgG:
-
Immunoglobulin G
- IgM:
-
Immunoglobulin M
- L/D:
-
Light/dark
- PBS:
-
Phosphate-buffered saline
- pIgR:
-
Poly-Ig receptor
- sIgA:
-
Secretory IgA
- TCDD:
-
2,3,7,8-tetrachlorodibenzo-p-dioxin
- TCDF:
-
2,3,7,8-tetrachlorodibenzofuran
- ZT:
-
Zeitgeber time
References
Apter FM, Michetti P, Winner LS 3rd, Mack JA, Mekalanos JJ, Neutra MR. Analysis of the roles of antilipopolysaccharide and anti-cholera toxin immunoglobulin a (IgA) antibodies in protection against vibrio cholerae and cholera toxin by use of monoclonal IgA antibodies in vivo. Infect Immun. 1993;61(12):5279–85.
Aylward LL, Brunet RC, Carrier G, Hays SM, Cushing CA, Needham LL, et al. Concentration-dependent TCDD elimination kinetics in humans: toxicokinetic modeling for moderately to highly exposed adults from Seveso, Italy, and Vienna, Austria, and impact on dose estimates for the NIOSH cohort. J Expo Sci Environ Epidemiol. 2005;15:51–65.
Benson JM, Shepherd DM. Aryl hydrocarbon receptor activation by TCDD reduces inflammation associated with Crohn's disease. Toxicol Sci. 2011;120(1):68–78.
Bhavsar SP, Reiner EJ, Hayton A, Fletcher R, MacPherson K. Converting toxic equivalents (TEQ) of dioxins and dioxin-like compounds in fish from one toxic equivalency factor (TEF) scheme to another. Environ Int. 2008;34(7):915–21.
Bowers OJ, Sommersted KB, Sowell RT, Boling GE, Hanneman WH, Titus RG, et al. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) reduces Leishmania major burdens in C57BL/6 mice. Am J Trop Med Hyg. 2006;75(4):749–52.
Burns P, Oddi S, Forzani L, Tabacman E, Reinheimer J, Vinderola G. Variability in gut mucosal secretory IgA in mice along a working day. BMC Res Notes. 2018;11(1):98.
Chmill S, Kadow S, Winter M, Weighardt H, Esser C. 2,3,7,8-Tetrachlorodibenzo-p-dioxin impairs stable establishment of oral tolerance in mice. Toxicol Sci. 2010;118(1):98–107.
Connor KT, Harris MA, Edwards MR, Budinsky RA, Clark GC, Chu AC, et al. AH receptor agonist activity in human blood measured with a cell-based bioassay: evidence for naturally occurring AH receptor ligands in vivo. J Expo Sci Environ Epidemiol. 2008;18:369–80.
Culbreath C, Tanner SM, Yeramilli VA, Berryhill TF, Lorenz RG, Martin CA. Environmental-mediated intestinal homeostasis in neonatal mice. J Surg Res. 2015;198(2):494–501.
De Krey GK, Baecher-Steppan L, Deyo JA, Smith B, Kerkvliet NI. Polychlorinated biphenyl-induced immune suppression: castration, but not adrenalectomy or RU 38486 treatment, partially restores the suppressed cytotoxic T lymphocyte response to alloantigen. J Pharmacol Exp Ther. 1993;267(1):308–15.
DeKrey GK, Teagarden RE, Lenberg JL, Titus RG. 2,3,7,8-tetrachlorodibenzo-p-dioxin slows the progression of experimental cutaneous Leishmaniasis in susceptible BALB/c and SCID mice. PLoS One. 2013;8:e76259.
Denison MS, Soshilov AA, He G, DeGroot DE, Zhao B. Exactly the same but different: promiscuity and diversity in the molecular mechanisms of action of the aryl hydrocarbon (dioxin) receptor. Toxicol Sci. 2011;124(1):1–22.
Eriksson E, Royo F, Lyberg K, Carlsson HE, Hau J. Effect of metabolic cage housing on immunoglobulin a and corticosterone excretion in faeces and urine of young male rats. Exp Physiol. 2004;89(4):427–33.
Esser C, Rannug A, Stockinger B. The aryl hydrocarbon receptor in immunity. Trends Immunol. 2009;30(9):447–54.
Fagarasan S, Kawamoto S, Kanagawa O, Suzuki K. Adaptive immune regulation in the gut: T cell-dependent and T cell-independent IgA synthesis. Annu Rev Immunol. 2010;28:243–73.
Frericks M, Meissner M, Esser C. Microarray analysis of the AHR system: tissue-specific flexibility in signal and target genes. Toxicol Appl Pharmacol. 2007;220(3):320–32.
Fritz JH, Rojas OL, Simard N, McCarthy DD, Hapfelmeier S, Rubino S, et al. Acquisition of a multifunctional IgA+ plasma cell phenotype in the gut. Nature. 2012;481:199–203.
Godinho-Silva C, Domingues RG, Rendas M, Raposo B, Ribeiro H, da Silva JA, et al. Light-entrained and brain-tuned circadian circuits regulate ILC3s and gut homeostasis. Nature. 2019;574:254–8.
Harper N, Connor K, Steinberg M, Safe S. An enzyme-linked immunosorbent assay (ELISA) specific for antibodies to TNP-LPS detects alterations in serum immunoglobulins and isotype switching in C57BL/6 and DBA/2 mice exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxing and related compounds. Toxicology. 1994;92:155–67.
Hinsdill R, Couch D, Speirs R. Immunosuppresssion in mice induced by dioxin (TCDD) in feed. J Environ Pathol Toxicol. 1980;4:401–25.
Inouye K, Ito T, Fujimaki H, Takahashi Y, Takemori T, Pan X, et al. Suppressive effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) on the high-affinity antibody response in C57BL/6 mice. Toxicol Sci. 2003;74(2):315–24.
Ishikawa S. Children's immunology, what can we learn from animal studies (3): impaired mucosal immunity in the gut by 2,3,7,8-tetraclorodibenzo-p-dioxin (TCDD): a possible role for allergic sensitization. J Toxicol Sci. 2009;34(Suppl 2):SP349–61.
Jones MK, Weisenburger WP, Sipes IG, Russell DH. Circadian alterations in prolactin, corticosterone, and thyroid hormone levels and down-regulation of prolactin receptor activity by 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Appl Pharmacol. 1987;87(2):337–50.
Kamada N, Seo SU, Chen GY, Nunez G. Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol. 2013;13:321–35.
Kasanen I, Inhila K, Savontaus E, Voipio HM, Okva K, Mering S, et al. Diurnal rhythms of blood glucose, serum ghrelin, faecal IgA and faecal corticosterone in rats subjected to restricted feeding using the diet board. Lab Anim. 2018;52(1):29–37.
Kerkvliet NI. Recent advances in understanding the mechanisms of TCDD immunotoxicity. Int Immunopharmacol. 2002;2(2-3):277–91.
Kerkvliet NI, Baecher-Steppan L. Suppression of allograft immunity by 3,4,5,3′,4′,5′-hexachlorobiphenyl. I. Effects of exposure on tumor rejection and cytotoxic T cell activity in vivo. Immunopharmacology. 1988;16:1–12.
Kinoshita H, Abe J, Akadegawa K, Yurino H, Uchida T, Ikeda S, et al. Breakdown of mucosal immunity in gut by 2,3,7,8-tetraclorodibenzo-p-dioxin (TCDD). Environ Health Prev Med. 2006;11(5):256–63.
Kobayashi R, Taguchi C, Yonenaga S, Arikawa K, Uchiyama T, Kono T, et al. Circadian rhythm affects the dynamics of S-IgA mucosal secretion. Int J Oral-Med Sci. 2015;14(1):1–7.
Laberton J, Griffin D, Arbogast B, Inman R, Deinzer M. The determination of polychlorodibenzo-p-dioxins in pentachlorophenol and wood treatment solutions. Am Ind Hyg Assoc J. 1979;40(9):816–22.
Lu H, Crawford RB, Suarez-Martinez JE, Kaplan BL, Kaminski NE. Induction of the aryl hydrocarbon receptor-responsive genes and modulation of the immunoglobulin M response by 2,3,7,8-tetrachlorodibenzo-p-dioxin in primary human B cells. Toxicol Sci. 2010;118(1):86–97.
Lundberg K, Gronvik KO, Dencker L. 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) induced suppression of the local immune response. Int J Immunopharmacol. 1991;13(4):357–68.
Lycke N, Erlandsson L, Ekman L, Schon K, Leanderson T. Lack of J chain inhibits the transport of gut IgA and abrogates the development of intestinal antitoxic protection. J Immunol. 1999;163(2):913–9.
Macpherson AJ, Geuking MB, McCoy KD. Homeland security: IgA immunity at the frontiers of the body. Trends Immunol. 2012;33(4):160–7.
Martchenko A, Martchenko SE, Biancolin AD, Brubaker PL. Circadian rhythms and the gastrointestinal tract: relationship to metabolism and gut hormones. Endocrinology. 2020;161(12):bqaa167.
Matsumura F. The significance of the nongenomic pathway in mediating inflammatory signaling of the dioxin-activated ah receptor to cause toxic effects. Biochem Pharmacol. 2009;77(4):608–26.
McIntosh BE, Hogenesch JB, Bradfield CA. Mammalian per-Arnt-Sim proteins in environmental adaptation. Annu Rev Physiol. 2010;72:625–45.
Mestecky J, McGhee JR. Immunoglobulin a (IgA): molecular and cellular interactions involved in IgA biosynthesis and immune response. Adv Immunol. 1987;40:153–245.
Miniero R, De Felip E, Ferri F, di Domenico A. An overview of TCDD half-life in mammals and its correlation to body weight. Chemosphere. 2001;43(4-7):839–44.
Mkaddem SB, Christou I, Rossato E, Berthelot L, Lehuen A, Monteiro RC. IgA, IgA receptors, and their anti-inflammatory properties. Curr Top Microbiol Immunol. 2014;382:221–35.
Moon C, Baldridge MT, Wallace MA, Burnham CA, Virgin HW, Stappenbeck TS. Vertically transmitted faecal IgA levels determine extra-chromosomal phenotypic variation. Nature. 2015;521(7550):90–3.
Murray IA, Nichols RG, Zhang L, Patterson AD, Perdew GH. Expression of the aryl hydrocarbon receptor contributes to the establishment of intestinal microbial community structure in mice. Sci Rep. 2016;6:33969.
Nguyen LP, Bradfield CA. The search for endogenous activators of the aryl hydrocarbon receptor. Chem Res Toxicol. 2008;21(1):102–16.
Ohtake F, Baba A, Takada I, Okada M, Iwasaki K, Miki H, et al. Dioxin receptor is a ligand-dependent E3 ubiquitin ligase. Nature. 2007;446:562–6.
North CM, Crawford RB, Lu H, Kaminski NE. 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated suppression of toll-like receptor stimulated B-lymphocyte activation and initiation of plasmacytic differentiation. Toxicol Sci. 2010;116(1):99–112.
Percie du Sert N, Hurst V, Ahluwalia A, Alam S, Avey MT, Baker M, et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. PLOS Biol. 2020;18:e3000410. https://doi.org/10.1371/journal.pbio.3000410.
Peterson DA, McNulty NP, Guruge JL, Gordon JI. IgA response to symbiotic bacteria as a mediator of gut homeostasis. Cell Host Microbe. 2007;2(5):328–39.
Pihl L, Hau J. Faecal corticosterone and immunoglobulin a in young adult rats. Lab Anim. 2003;37(2):166–71.
Pohjanvirta R, Tuomisto J. 2,3,7,8-Tetrachlorodibenzo-p-dioxin enhances responsiveness to post-ingestive satiety signals. Toxicology. 1990;63(3):285–99.
Pohjanvirta R, Tuomisto J, Linden J, Laitinen J. TCDD reduces serum melatonin levels in long-Evans rats. Pharmacol Toxicol. 1989;65(3):239–40.
Price GA, McFann K, Holmes RK. Immunization with cholera toxin B subunit induces high-level protection in the suckling mouse model of cholera. PLoS One. 2013;8(2):e57269.
Quintana FJ, Sherr DH. Aryl hydrocarbon receptor control of adaptive immunity. Pharmacol Rev. 2013;65(4):1148–61.
Refinetti R. Circadian physiology. 3rd ed. CRC Press: Taylor Francis Group; 2016.
Royo F, Bjork N, Carlsson HE, Mayo S, Hau J. Impact of chronic catheterization and automated blood sampling (Accusampler) on serum corticosterone and fecal immunoreactive corticosterone metabolites and immunoglobulin a in male rats. J Endocrinol. 2004;180(1):145–53.
Safe S, Chadalapaka G, Jutooru I. Aryl hydrocarbon receptor ligands: toxic, biochemical, and therapeutic effects. In: Eldridge JC, Stevens J, editors. Endocrine toxicology. New York: Informa Healthcare; 2010. p. 189–209.
Sazhnev V, DeKrey GK. The growth and infectivity of Leishmania major is not altered by in vitro exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin. BMC Res Notes. 2018;11(1):642.
Schlezinger JJ, Bernard PL, Haas A, Grandjean P, Weihe P, Sherr DH. Direct assessment of cumulative aryl hydrocarbon receptor agonist activity in sera from experimentally exposed mice and environmentally exposed humans. Environ Health Perspect. 2010;118(5):693–8.
Srivastava R, Kashyap A, Kumar M, Nath G, Jain AK. Mucosal IgA & IL-1beta in helicobacter pylori infection. Indian J Clin Biochem. 2013;28(1):19–23.
Stefka AT, Feehley T, Tripathi P, Qiu J, McCoy K, Mazmanian SK, et al. Commensal bacteria protect against food allergen sensitization. Proc Natl Acad Sci U S A. 2014;111(36):13145–50.
Stejskalova L, Dvorak Z, Pavek P. Endogenous and exogenous ligands of aryl hydrocarbon receptor: current state of art. Curr Drug Metab. 2011;12(2):198–212.
Stockinger B, Di Meglio P, Gialitakis M, Duarte JH. The aryl hydrocarbon receptor: multitasking in the immune system. Annu Rev Immunol. 2014;32:403–32.
Su B, Moog C. Which antibody functions are important for an HIV vaccine? Front Immunol. 2014;5:289.
Sulentic CE, Kaminski NE. The long winding road toward understanding the molecular mechanisms for B-cell suppression by 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Sci. 2011;120(Suppl 1):S171–91.
Suzuki K, Maruya M, Kawamoto S, Sitnik K, Kitamura H, Agace WW, et al. The sensing of environmental stimuli by follicular dendritic cells promotes immunoglobulin a generation in the gut. Immunity. 2010;33(1):71–83.
Tischkau SA. Mechanisms of circadian clock interactions with aryl hydrocarbon receptor signalling. Eur J Neurosci. 2020;51(1):379–95.
Tkachenko A, Henkler F, Brinkmann J, Sowada J, Genkinger D, Kern C, et al. The Q-rich/PST domain of the AHR regulates both ligand-induced nuclear transport and nucleocytoplasmic shuttling. Sci Rep. 2016;6:32009.
Uren TK, Wijburg OL, Simmons C, Johansen FE, Brandtzaeg P, Strugnell RA. Vaccine-induced protection against gastrointestinal bacterial infections in the absence of secretory antibodies. Eur J Immunol. 2005;35(1):180–8.
Vaidyanathan B, Chaudhry A, Yewdell WT, Angeletti D, Yen WF, Wheatley AK, et al. The aryl hydrocarbon receptor controls cell-fate decisions in B cells. J Exp Med. 2017;214(1):197–208.
Vorderstrasse BA, Bohn AA, Lawrence BP. Examining the relationship between impaired host resistance and altered immune function in mice treated with TCDD. Toxicology. 2003;188(1):15–28.
Vos J, Kreeftenberg J, Engel H, Minderhoud A, van Noorle JL. Studies on 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced immune suppression and decreased resistance to infection: endotoxin hypersensitivity, serum zinc concentrations and effect of thymosin treatment. Toxicology. 1978;9:75–86.
Wada M, Orihara K, Kamagata M, Hama K, Sasaki H, Haraguchi A, et al. Circadian clock-dependent increase in salivary IgA secretion modulated by sympathetic receptor activation in mice. Sci Rep. 2017;7:8802.
Warren TK, Mitchell KA, Lawrence BP. Exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) suppresses the humoral and cell-mediated immune responses to influenza a virus without affecting cytolytic activity in the lung. Toxicol Sci. 2000;56(1):114–23.
Wei M, Shinkura R, Doi Y, Maruya M, Fagarasan S, Honjo T. Mice carrying a knock-in mutation of Aicda resulting in a defect in somatic hypermutation have impaired gut homeostasis and compromised mucosal defense. Nat Immunol. 2011;12(3):264–70.
Xu CX, Krager SL, Liao DF, Tischkau SA. Disruption of CLOCK-BMAL1 transcriptional activity is responsible for aryl hydrocarbon receptor-mediated regulation of Period1 gene. Toxicol Sci. 2010;115(1):98–108.
Xu CX, Wang C, Krager SL, Bottum KM, Tischkau SA. Aryl hydrocarbon receptor activation attenuates Per1 gene induction and influences circadian clock resetting. Toxicol Sci. 2013;132(2):368–78.
Yang DM, Fairweather N, Button LL, McMaster WR, Kahl LP, Liew FY. Oral salmonella typhimurium (AroA-) vaccine expressing a major leishmanial surface protein (gp63) preferentially induces T helper 1 cells and protective immunity against leishmaniasis. J Immunol. 1990;145(7):2281–5.
Zhang L, Nichols RG, Correll J, Murray IA, Tanaka N, Smith PB, et al. Persistent organic pollutants modify gut microbiota-host metabolic homeostasis in mice through aryl hydrocarbon receptor activation. Environ Health Perspect. 2015;123(7):679–88.
Zhang Q, Kline DE, Bhattacharya S, Crawford RB, Conolly RB, Thomas RS, et al. All-or-none suppression of B cell terminal differentiation by environmental contaminant 2,3,7,8-tetrachlorodibenzo-p-dioxin. Toxicol Appl Pharmacol. 2013;268(1):17–26.
Zhou J, Henriquez J, Crawford RB, Kaminski NE. Suppression of the IgM response by aryl hydrocarbon receptor activation in human primary B cells involves impairment of immunoglobulin secretory processes. Toxicol Sci. 2018;163(1):319–29.
Acknowledgments
The authors are grateful to Max Avrukin, Alex Hunter, Grant Cooper, and Matt Turnipseed for their technical assistance throughout Experiment 1.
Funding
Funds for this study were provided by the University of Northern Colorado.
Author information
Authors and Affiliations
Contributions
CF, MM, AK, DA, GD: substantial contributions to study conception and design; data acquisition, analysis and interpretation. CF, AK, DA, GD: manuscript drafting and revision. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures using animals were carried out at the University of Northern Colorado in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health, USA, and with the approval of the University’s Animal Care and Use Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Foxx, C.L., Nagy, M.R., King, A.E. et al. TCDD exposure alters fecal IgA concentrations in male and female mice. BMC Pharmacol Toxicol 23, 25 (2022). https://doi.org/10.1186/s40360-022-00563-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40360-022-00563-9