Abstract
Background
Respiratory infectious diseases (RIDs) remain a pressing public health concern, posing a significant threat to the well-being and lives of individuals. This study delves into the incidence of seven primary RIDs during the period 2017–2021, aiming to gain deeper insights into their epidemiological characteristics for the purpose of enhancing control and prevention strategies.
Methods
Data pertaining to seven notifiable RIDs, namely, seasonal influenza, pulmonary tuberculosis (PTB), mumps, scarlet fever, pertussis, rubella and measles, in the mainland of China between 2017 and 2021 were obtained from the National Notifiable Disease Reporting System (NNDRS). Joinpoint regression software was utilized to analyze temporal trends, while SaTScan software with a Poisson probability model was used to assess seasonal and spatial patterns.
Results
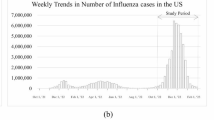
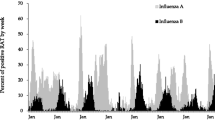
A total of 11,963,886 cases of the seven RIDs were reported during 2017–2021, and yielding a five-year average incidence rate of 170.73 per 100,000 individuals. Among these RIDs, seasonal influenza exhibited the highest average incidence rate (94.14 per 100,000), followed by PTB (55.52 per 100,000), mumps (15.16 per 100,000), scarlet fever (4.02 per 100,000), pertussis (1.10 per 100,000), rubella (0.59 per 100,000), and measles (0.21 per 100,000). Males experienced higher incidence rates across all seven RIDs. PTB incidence was notably elevated among farmers and individuals aged over 65, whereas the other RIDs primarily affected children and students under 15 years of age. The incidences of PTB and measles exhibited a declining trend from 2017 to 2021 (APC = −7.53%, P = 0.009; APC = −40.87%, P = 0.02), while the other five RIDs peaked in 2019. Concerning seasonal and spatial distribution, the seven RIDs displayed distinct characteristics, with variations observed for the same RIDs across different regions. The proportion of laboratory-confirmed cases fluctuated among the seven RIDs from 2017 to 2021, with measles and rubella exhibiting higher proportions and mumps and scarlet fever showing lower proportions.
Conclusions
The incidence of PTB and measles demonstrated a decrease in the mainland of China between 2017 and 2021, while the remaining five RIDs reached a peak in 2019. Overall, RIDs continue to pose a significant public health challenge. Urgent action is required to bolster capacity-building efforts and enhance control and prevention strategies for RIDs, taking into account regional disparities and epidemiological nuances. With the rapid advancement of high-tech solutions, the development and effective implementation of a digital/intelligent RIDs control and prevention system are imperative to facilitate precise surveillance, early warnings, and swift responses.
Graphical Abstract

Similar content being viewed by others
Background
Given the distinct transmission routes and modes of infection associated with respiratory infectious diseases (RIDs), many emerging and re-emerging RIDs have the potential to spread rapidly among susceptible populations worldwide. These RIDs persist as a significant public health challenge, imposing a global disease burden and jeopardizing individuals’ health and well-being [1, 2]. In the mainland of China, thirteen RIDs are subject to statutory reporting, with seasonal influenza and pulmonary tuberculosis (PTB) emerging as the most prevalent RIDs in recent decades [3]. In 2020, reported influenza morbidity stood at 81.58 per 100,000 individuals in the mainland of China, with a reported mortality rate of 0.005 per 100,000 [4]. Concurrently, PTB's notifiable incidence rate was 47.76 per 100,000, accompanied by a reported mortality rate of 0.14 per 100,000 [4]. Mumps, scarlet fever, pertussis, rubella and measles followed suit, representing five RIDs with comparatively elevated annual incidence rates that often clustered within specific regions [5,6,7,8,9,10,11,12]. Furthermore, the emergence and re-emergence of RIDs in recent years underscore the need for strengthen surveillance to enable early warnings and swift, effective responses. Consequently, a comprehensive elucidation of the demographic, temporal, seasonal, and spatial distribution characteristics of RIDs is crucial for the development of targeted, efficient interventions to curtail their propagation.
While several studies have explored the epidemiological features of various RIDs across different time frames and geographical locations in China [6,7,8,9,10,11,12,13,14], the present study stands apart due to its unique data sources and temporal scope. Leveraging data from the National Notifiable Disease Reporting System (NNDRS), this study provides a more comprehensive analysis, incorporating recent data and encompassing factors such as case categories (clinically diagnosed and laboratory-confirmed), gender, and occupation. The study’s focus centers on the demographic, temporal, seasonal, and spatial distribution characteristics of seven RIDs during the period 2017–2021, with the aim of furnishing valuable insights to inform effective control and prevention strategies.
Methods
Data collection
This study draws upon surveillance data for seven RIDs in the mainland of China spanning the years 2017 to 2021, sourced from the NNDRS. Among these RIDs, PTB, pertussis, measles, and scarlet fever are classified as category B infectious diseases, while seasonal influenza, mumps, and rubella fall under category C infectious diseases. The NNDRS is an internet-based real-time disease-reporting system that encompasses various healthcare facilities (community health centers, township health centers, and village clinics) across the mainland of China, boasting coverage of 55,077 health facilities in 31 provincial-level administrative divisions (PLADs) [15, 16]. The anonymized data for each reported case were compiled, encompassing demographic details (residential ID number, sex, age, and occupation) and clinical particulars (dates of symptom onset, diagnosis date, diagnosis category). Reported cases encompass both clinically diagnosed cases and laboratory-confirmed cases, aligned with the diagnosis criteria stipulated and disseminated by the National Health Commission of the People’s Republic of China [15, 16]. Clinically diagnosed cases are established based on primary symptoms, signs, and epidemiological links. In contrast, laboratory-confirmed cases entail a synthesis of clinical diagnosis and corroborating laboratory testing [15, 16].
Demographic data by age and sex for 31 PLADs and the country were culled from the National Bureau of Statistics of China (http://www.stats.gov.cn/english/Statisticaldata/AnnualData, accessed on April 20, 2023) [17]. The standard base map of China [GS(2019)1822] was sourced from the Standard Map Service (http://bzdt.ch.mnr.gov.cn/, accessed on April 20, 2023) under the Ministry of Natural Resources of the People's Republic of China.
Descriptive analysis
Incidence rates for both national and provincial levels were calculated on a monthly and annual basis, along with stratifications by sex and age groups. Visual representations in the form of bar graphs and scatter line plots were employed to depict trends in cases and incidence rates. Stacked plots and heat maps elucidated trends in occupation proportions and laboratory-confirmed cases, respectively. Seasonal attributes were visualized via radar charts, generated using SaTScan (version 10.1, Kulldorff and Information Management Services, Inc., Boston, MA, USA) outputs. Figures were crafted using R software with the ggplot2 package (version 4.0.0, R Development Core Team 2020) and OriginPro (version 2021, OriginLab Corporation, Northampton, MA, USA), while spatial characteristics were mapped using ArcGIS software (version 10.7, ESRI, Redlands, CA, USA).
Joinpoint regression analysis
Temporal trends were subjected to analysis using Joinpoint regression software (version 4.9.0.0, National Cancer Institute, Rockville, MD, USA) [18]. The default modeling method was the grid search method (GSM), while the Monte Carlo permutation test served as the default optimization strategy for the model. The Bayesian information criterion (BIC) was employed as a metric for gauging good fit [18]. The annual percent change (APC) serves as an indicator of the average annual percentage alteration in incidence rates and is represented by the slope of the fitted line. An APC > 0 (P < 0.05) denotes an increasing trend in incidence rates, whereas an APC < 0 (P < 0.05) signifies a decreasing trend. Conversely, trends lacking significant changes are denoted by APC values falling outside these ranges [13]. The APC is calculated using the following formula:
Note: y is incidence rate, x is year, β1 is regression coefficient.
Seasonal and spatial analysis
The examination of seasonal and spatial characteristics was conducted using the SaTScan software. This software employed a Poisson probability model to identify clusters of RIDs in terms of seasonality, with a temporal window encompassing 50%. The software detected spatial clusters of RIDs in different regions for the years 2017 and 2021, employing the Poisson probability model and a spatial window covering 50% of the study areas [19]. In order to avoid overlap of PLADs in clusters, we adjust the default parameter to remove “Gini Optimized Cluster Collection” and set “No Geographical Overlap” in clusters [19]. By juxtaposing observed and predicted events within each location window, assuming a random distribution, probable clusters were pinpointed. The cluster exhibiting the highest log-likelihood ratio (LLR) was deemed the most likely cluster, while others were ranked as secondary clusters in a specific sequence [19]. The concept of relative risk (RR) denoted the ratio of estimated risks within and outside the cluster, serving as an indicator of the elevated infection risk faced by individuals residing within the cluster compared to those outside it [19].
In the context of the seasonal analysis, the 31 PLADs in the mainland of China were stratified into two distinct regions: southern China (encompassing Anhui, Fujian, Guangdong, Guangxi, Guizhou, Hainan, Hubei, Hunan, Jiangsu, Jiangxi, Shanghai, Sichuan, Yunnan, Zhejiang and Chongqing) and northern China (covering Bei**g, Gansu, Hebei, Henan, Heilongjiang, Jilin, Liaoning, Inner Mongolia, Ningxia, Qinghai, Shandong, Shanxi, Shaanxi, Tian**, Tibet and ** tailored strategies for RIDs control and prevention. However, the five-year duration of available surveillance data and potential variations in reporting across regions and levels present certain limitations.
Conclusions
The incidence rates of seasonal influenza, PTB, mumps, and scarlet fever remain high, whereas pertussis, rubella, and measles have reached lower levels. The reported incidence rates of PTB and measles have experienced significant declines between 2017 and 2021. Peaks in reported incidence rates for seasonal influenza, mumps, scarlet fever, pertussis, and rubella were observed in 2019. Each of the seven RIDs demonstrates distinct epidemiological characteristics. While significant progress has been made in RIDs control and prevention, challenges persist. Urgent measures are needed to strengthen surveillance efforts and develop effective digital/intelligent systems for precise RIDs surveillance, early detection of emerging or re-emerging events, and prompt responses.
Availability of data and materials
The data is from the National Notifiable Disease Reporting System (NNDRS), and the application is based on the requirement of NNDRS.
Abbreviations
- RIDs:
-
Respiratory infectious diseases
- PTB:
-
Pulmonary tuberculosis
- NNDRS:
-
National notifiable disease reporting system
- APC:
-
Annual percentage changes
- PLADs:
-
Provincial-level administrative divisions
- GSM:
-
Grid search method
- BIC:
-
Bayesian information criterion
- RR :
-
Relative risk
- LLR :
-
Log-likelihood ratio
References
World Health Organization. Global Influenza Strategy 2019–2030. Available from: https://www.who.int/publications/i/item/9789241515320. Accessed 20 April 2023.
World Health Organization. World Health Statistics 2022. Available from: https://www.who.int/news/item/20-05-2022-world-health-statistics-2022. Accessed 20 April 2023.
Chinese Center for Disease Control and Prevention. Protocol of infectious disease reporting (2020). Available from http://www.chinacdc.cn/jkzt/crb/xcrxjb/201810/t20181017_195160.html. Accessed 1 August 2023.
National Health Commission of the People's Republic of China. Overview of national Notifiable disease in 2020. Available from: http://www.nhc.gov.cn/jkj/s3578/202103/f1a448b7df7d4760976fea6d55834966.shtml. Accessed 1 August 2023.
Zhang H, Chen C, Tang A, Wu B, Liu LJ, Wu MY, et al. Epidemiological investigation and virus tracing of a measles outbreak in Zhoushan Islands, China, 2019. Front Public Health. 2020;8: 600196. https://doi.org/10.3389/fpubh.2020.600196.
Mao Y, Zhang N, Zhu B, Liu JL, He RX. A descriptive analysis of the Spatio-temporal distribution of intestinal infectious diseases in China. BMC Infect Dis. 2019;19(1):766. https://doi.org/10.1186/s12879-019-4400-x.
Jiang H, Liu MY, Zhang YJ, Yin JF, Li ZW, Zhu CD, et al. Changes in incidence and epidemiological characteristics of pulmonary tuberculosis in Mainland China, 2005–2016. JAMA Netw Open. 2021;4(4): e215302. https://doi.org/10.1001/jamanetworkopen.2021.5302.
Jiang Y, Dou XF, Yan CQ, Wan L, Liu HC, Li MC, et al. Epidemiological characteristics and trends of notifiable infectious diseases in China from 1986 to 2016. J Glob Health. 2020;10(2): 020803. https://doi.org/10.7189/jogh.10.020803.
Deng LL, Han YJ, Wang JL, Liu HC, Li GL, Wang DY, et al. Epidemiological characteristics of notifiable respiratory infectious diseases in mainland China from 2010 to 2018. Int J Environ Res Public Health. 2023;20(5):3946. https://doi.org/10.3390/ijerph20053946.
Mao Y, He RX, Zhu B, Liu JL, Zhang N. Notifiable respiratory infectious diseases in china: a spatial-temporal epidemiology analysis. Int J Environ Res Public Health. 2020;17(7):2301. https://doi.org/10.3390/ijerph17072301.
Ma C, Rodewald L, Hao LX, Su Q, Zhang Y, Wen N, et al. Progress Toward Measles Elimination—China, January 2013–June 2019. MMWR Morb Mortal Wkly Rep. 2019;68(48):1112–6. https://doi.org/10.15585/mmwr.mm6848a2.
Ning G, Gao Y, Wu D, Li J, Li Y, Shao Z, et al. Epidemiology of pertussis in China, 2011–2017. Chin J Vaccine Immun. 2018;24(3):264–73. https://doi.org/10.19914/j.cjvi.2018.03.004. (in Chinese).
Li Y, Ma C, Hao L, Wang F, Wen N, Yang H, et al. Epidemiology of rubella in China, 2018–2019. Chin J Vaccine Immun. 2021;27(1):62–6. https://doi.org/10.19914/j.CJVI.2021003. (in Chinese).
Cui J, Zhang Y, Su X. Spatiotemporal scan statistic of scarlet fever in China, 2010–2019. Dis Surveil. 2023;38(3):1–7. https://doi.org/10.3784/jbjc.202209300433.
Dong YH, Wang LP, Burgner DP, Miller JE, Song Y, Ren X, et al. Infectious diseases in children and adolescents in China: analysis of national surveillance data from 2008 to 2017. BMJ. 2020;369: m1043. https://doi.org/10.1136/bmj.m1043.
Geng MJ, Zhang HY, Yu LJ, Lv CL, Wang T, Che TL, et al. Changes in notifiable infectious disease incidence in China during the COVID-19 pandemic. Nat Commun. 2021;12(1):6923. https://doi.org/10.1038/s41467-021-27292-7.
National Bureau of Statistics of China. Annual data. 2021. http://www.stats.gov.cn/english/Statisticaldata/AnnualData. Accessed 20 April 2023.
Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51. https://doi.org/10.1002/(sici)1097-0258(20000215)19:3%3c335::aid-sim336%3e3.0.co;2-z.
Kulldorff M. Prospective time periodic geographical disease surveillance using a scan statistic. J R Stat Soc. 2001;164:61–72. https://doi.org/10.1111/1467-985X.00186.
Du M, Wang RT, Yuan J, Lv X, Yan WX, Liu Q, et al. Trends and disparities in 44 national notifiable infectious diseases in China: an analysis of national surveillance data from 2010 to 2019. J Med Virol. 2023;95(1): e28353. https://doi.org/10.1002/jmv.28353.
Wang LQ, Wang WB. Temporal trends in notification and mortality of tuberculosis in china, 2004–2019: a joinpoint and age-period-cohort analysis. Int J Environ Res Public Health. 2021;18(11):5607. https://doi.org/10.3390/ijerph18115607.
Huang F, **a YY, Chen H, Wang N, Du X, Chen W, et al. The impact of the COVID-19 epidemic on tuberculosis control in China. Lancet Reg Health West Pac. 2020. https://doi.org/10.1016/j.lanwpc.2020.100032.
Cheng J, Sun YN, Zhang CY, Yu YL, Tang LH, Peng H, et al. Incidence and risk factors of tuberculosis among the elderly population in China: a prospective cohort study. Infect Dis Poverty. 2020;9(1):13. https://doi.org/10.1186/s40249-019-0614-9.
Zeng X, **e Y, Chen T, Huang W, Tang J, Li X, et al. Analysis of influenza outbreak characteristics in China from 2019 to 2020. Int J Virol. 2021;5:359–63 (in Chinese).
Su QR, Ma C, Wen N, Fan CX, Yang H, Wang HQ, et al. Epidemiological profile and progress toward rubella elimination in China. 10 years after nationwide introduction of rubella vaccine. Vaccine. 2018;36(16):2079–85. https://doi.org/10.1016/j.vaccine.2018.03.013.
Zou X, Zhou L, Wu HZ, Chen L, Zhou FJ, Gong C, et al. The role of tuberculosis control institutes in delivering tuberculosis information to domestic migrants in China: a multi-level analysis of a nationwide cross-sectional survey. Int J Infect Dis. 2019;86:94–101. https://doi.org/10.1016/j.ijid.2019.06.021.
Dong Z, Wang QQ, Yu SC, Huang F, Liu JJ, Yao HY, et al. Age-period-cohort analysis of pulmonary tuberculosis reported incidence, China, 2006–2020. Infect Dis Poverty. 2022;11(1):85. https://doi.org/10.1186/s40249-022-01009-4.
World Health Organization. The End TB Strategy. Available from: https://www.who.int/tb/End_TB_brochure.pdf?ua=1. Accessed 20 April 2023.
National Health Commission of the People’s Republic of China. Administrative Measures for tuberculosis Prevention and Control. Available from: http://www.nhc.gov.cn/wjw/c100022/202201/e7341575797e4dd5beb4307e5cd31a7c.shtml. Accessed 20 April 2023.
Xu WB, Zhang Y, Wang HL, Zhu Z, Mao NY, Mulders MN, et al. Global and national laboratory networks support high quality surveillance for measles and rubella. Int Health. 2017;9(3):184–9. https://doi.org/10.1093/inthealth/ihx017.
Acknowledgements
We thank all healthcare workers and facilities at different levels and areas for their contribution to notifiable infectious diseases, as well as the Chinese Center for Disease Control and Prevention for sharing the data.
Funding
None.
Author information
Authors and Affiliations
Contributions
L-LD implemented the study, managed and analyzed the data, wrote, reviewed, and edited the manuscript. G-XH, D-YW, X-R and T-C designed the study, provide the idea, interpreted the data, critical review and edited the manuscript. Y-JH, and Z-WL provided support in data management and drafted and revised the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The information in our study was from the NNDRS, which is routine surveillance, and all case information was anonymized.
Consent for publication
All the authors have written the informed consent and agreed with the publication of this paper.
Competing interests
The authors declare that they have no competing conflict of interest.
Supplementary Information
Additional file 1
: Figure S1. The spatial distributions for incidence rates of the seven RIDs in 2017 and 2021.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Deng, Ll., Han, Yj., Li, Zw. et al. Epidemiological characteristics of seven notifiable respiratory infectious diseases in the mainland of China: an analysis of national surveillance data from 2017 to 2021. Infect Dis Poverty 12, 99 (2023). https://doi.org/10.1186/s40249-023-01147-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-023-01147-3