Abstract
Background
The incubation period is a crucial index of epidemiology in understanding the spread of the emerging Coronavirus disease 2019 (COVID-19). In this study, we aimed to describe the incubation period of COVID-19 globally and in the mainland of China.
Methods
The searched studies were published from December 1, 2019 to May 26, 2021 in CNKI, Wanfang, PubMed, and Embase databases. A random-effect model was used to pool the mean incubation period. Meta-regression was used to explore the sources of heterogeneity. Meanwhile, we collected 11 545 patients in the mainland of China outside Hubei from January 19, 2020 to September 21, 2020. The incubation period fitted with the Log-normal model by the coarseDataTools package.
Results
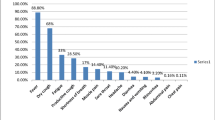
A total of 3235 articles were searched, 53 of which were included in the meta-analysis. The pooled mean incubation period of COVID-19 was 6.0 days (95% confidence interval [CI] 5.6–6.5) globally, 6.5 days (95% CI 6.1–6.9) in the mainland of China, and 4.6 days (95% CI 4.1–5.1) outside the mainland of China (P = 0.006). The incubation period varied with age (P = 0.005). Meanwhile, in 11 545 patients, the mean incubation period was 7.1 days (95% CI 7.0–7.2), which was similar to the finding in our meta-analysis.
Conclusions
For COVID-19, the mean incubation period was 6.0 days globally but near 7.0 days in the mainland of China, which will help identify the time of infection and make disease control decisions. Furthermore, attention should also be paid to the region- or age-specific incubation period.
Graphic Abstract

Similar content being viewed by others
Background
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus (SARS-CoV-2). It has spread over 223 countries and has been declared a pandemic on March 11, 2020 by World Health Organization [1]. The number of COVID-19 patients is rapidly increasing globally. More than 113.5 million confirmed cases and 2.5 million deaths were reported globally by March 2, 2021 [1]. The COVID-19 pandemic has become a worldwide public health issue.
The incubation period, known as the interval between initial infection and onset of disease, is an important index to characterize the spread of infectious disease and formulate quarantine measures. For example, the mean incubation period is often used to calculate the reproduction number, and the maximum incubation period is used to determine the duration of quarantine [2]. For COVID-19, its average incubation period has a wide range, ranging from 2.87 days [3] to 17.6 days [2]. The 14-day quarantine strategy faced a challenge because the incubation period of COVID-19 exceeded 14 days [87]. In this study, among 11 545 patients, more than 10% developed the disease 14 days after infection in the 11 545 patients. Consistent with the results in 218 patients with precise data, the most extended incubation period was 26 days, and 27 patients had an incubation period of more than 14 days. Based on available evidence, the most extended incubation period of COVID-19 was 34 days in Shanghai’s patients, far more than 14 days [4]. The extreme tail end of the incubation period may be affected by the sample size, the knowledge of SARS-CoV-2, and the observation period. Previous studies indicated that 5–10% of patients infected with SARS-CoV-2 had an incubation period longer than 14 days [88]. The above-mentioned evidence indicated that an extended quarantine period was needed to prevent the spread of SARS-CoV-2. When the quarantine interval was longer, more patients will be identified, and the epidemic will be controlled faster. Our findings suggested that the 21-day quarantine strategy will reduce the number of patients without symptoms by 80% compared with the 14-day quarantine strategy.
Take Wuhan as an example, after implementing a strict quarantine strategy of all residents on January 23, the number of new cases with COVID-19 decreased rapidly, with a 50% reduction after 14 days (February 6) and a 75% reduction after 28 days (February 20) [89]. However, the impact of the nucleic acid test on the development of quarantine strategies remained unknown. The nucleic acid test played a vital role in the prevention and control of the COVID-19 pandemic. A previous study reported that 8% of patients had a negative report of nucleic acid test after being quarantined for 14 days [90]. Cai et al. found that over 5% of patients had an incubation period of more than 14 days, which defined the incubation period as the interval from the earliest exposure to laboratory confirmation of COVID-19 or onset of symptoms and signs [91]. We hypothesized that, if only relying on clinical symptoms or nucleic acid test results, then the 14-day quarantine strategy will result in a part of patients not being recognized as confirmed cases. Therefore, adopting a 21-day quarantine strategy was recommended, particularly for places with insufficient detection resources or a high risk of being infected with SARS-CoV-2, such as contacting the patients infected with SARS-CoV-2 or coming from cities or countries where COVID-19 was epidemic.
In addition, the potential patients should be quarantined as soon as possible. We found that about 15% of patients had an incubation period of fewer than 3 days. In India, 25% of patients had an incubation period of fewer than 3 days (25th percentile: 3.0 days) [32]. One-third of patients in Singapore had an incubation period of less than or equal to 3 days [35]. Patients with COVID-19 were infectious before they developed symptoms [92]. Our study found that half of the patients developed symptoms within 7 days after infection. A meta-analysis showed that the mean serial interval of COVID-19 was 5.5 days [93]. Therefore, for COVID-19, the serial interval was shorter than the incubation period. We hypothesized that the spread of SARS-CoV-2 occurred on average 1.5 days before the onset of the disease. If all close contacts are quarantined on the 3rd day after infection, then more than 15% of the people infected with SARS-CoV-2 in close connections may have infected others. When COVID-19 patients and their close and sub-close contacts were quarantined for the first time, further transmission will be terminated.
The incubation period of COVID-19 varied with age. We found that the incubation period was different among age groups. In 218 patients, the incubation period presented a U-shaped curve with increasing age. The middle-aged group (41–60 years) had the shortest incubation period among the other groups, particularly the elderly group (≥ 61 years) and those aged 18–40 years. A similar age-specific distribution of incubation period was reported in the previous study with 136 patients, showing the shortest incubation period in patients aged 45 to 59 years [7]. Another study with 2 555 patients also found a U-shaped curve distribution of incubation period in patients [6]. The mechanism of the effect of age on the COVID-19 incubation period was unclear. Possible explanations include a less intense immune response, a delay in the onset of symptoms, and a shorter exposure time and exposure rate in the elderly and children.
Focusing on the incubation period among different SARS-CoV-2 variants is important. Our finding showed that the incubation period in the mainland of China was longer than that outside the mainland of China (6.5 days vs 4.6 days, P < 0.001). Phylogenetic network analysis revealed that the types of SARS-CoV-2 were different among Chinese, Europeans, and Americans in the early stage of the COVID-19 pandemic [94]. Therefore, we hypothesized that the incubation period of COVID-19 may be different among SARS-CoV-2 variants. Recently, an outbreak of SARS-CoV-2 variant B.1.617.2 occurred in Guangzhou, China. In this outbreak, the mean incubation period was 4.4 days (95% CI 3.9–5.0), which was shorter than that previously reported in China [95]. These evidences indicated that mutations affected the incubation period of COVID-19. However, more research was needed to explore the relationship of incubation period of COVID-19 with SARS-CoV-2 variants.
However, no difference in incubation period was observed between males and females. The previous study suggested that male was more susceptible to COVID-19, which may be due to the high plasma concentration of ACE2 [96]. However, our study did not observe a difference in incubation period by gender. Nie et al. also showed an insignificant difference in incubation period by gender (5 days vs 4 days; P = 0.22) [8]. Yang et al. presented a similar conclusion [97]. The evidence indicated that gender maybe not a factor affecting the incubation period of COVID-19.
Several limitations should be stated in the present study. First, the current meta-analysis did not include studies published in languages other than Chinese or English because of language restrictions. Most of the included studies were from China. Secondly, information bias may also exist. As far as we know, this study had the largest sample size to date, but a part of patients was missing the date of onset. Although no significant difference in incubation periods was observed among the three estimation methods of the date of onset, the estimated date of onset may be biased from the actual date of onset. In addition, most patients had a doubly interval-censored data rather than precise date of infection. For extreme exposure intervals, we limited the exposure interval to 14 days, which might neglect a small part of the extreme incubation period. Third, in the 218 patients with precise data, the proportion of incubation period exceeding 14 days was higher than that in previous studies. This result would obtain an extreme right tail for the incubation period of COVID-19. Finally, the active contact tracing and testing (nucleic acid testing and antibody testing) may truncate the time between exposure to identifying infected persons. Therefore, caution should be taken when formulating quarantine strategies because the estimation of the incubation period did not involve nucleic acid tests and antibody tests.
Conclusions
This study provides evidence on the incubation period of COVID-19 to understand the transmission of disease and formulate preventive measures. The mean incubation period is 6.0 days globally, but it is longer in the mainland of China (6.5 days) than in other regions (4.6 days). The region- or age-specific incubation period should be paid attention to. Moreover, 10% of patients had an incubation period over 14 days in Chinese population, suggesting that the 14-day quarantine period may not be enough.
Availability of data and materials
The data used for this article is available from the corresponding author on reasonable request.
Abbreviations
- ACE2:
-
Angiotensin-converting enzyme 2
- CI :
-
Confidence interval
- COVID-19:
-
Coronavirus disease 2019
- CNKI:
-
China National Knowledge Infrastructure
- IQR:
-
Interquartile range
- 2019-nCoV:
-
Novel coronavirus 2019
- NCP:
-
Novel coronavirus pneumonia
- MOOSE:
-
Meta-analysis of observational studies in epidemiology
- R:
-
Range
- RT-PCR:
-
Reverse Transcription-Polymerase Chain Reaction
- SD :
-
Standard deviation
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
References
World Health Organization. COVID-19 weekly epidemiological update (2 March 2021). https://www.who.int/publications/m/item/weekly-epidemiological-update-2-march-2021. Accessed 4 Mar 2021.
Li ZY, Zhang Y, Peng LQ, Gao RR, **g JR, Wang JL, et al. Demand for longer quarantine period among common and uncommon COVID-19 infections: a sco** review. Infect Dis Poverty. 2021;10:56.
Chun JY, Baek G, Kim Y. Transmission onset distribution of COVID-19. Int J Infect Dis. 2020;99:403–7.
**e S, Zhang G, Yu H, Wang J, Wang S, Tang G, et al. The epidemiologic and clinical features of suspected and confirmed cases of imported 2019 novel coronavirus pneumonia in north Shanghai, China. Ann Transl Med. 2020;8:637.
You C, Deng Y, Hu W, Sun J, Lin Q, Zhou F, et al. Estimation of the time-varying reproduction number of COVID-19 outbreak in China. Int J Hyg Environ Health. 2020;228:113555.
**ao Z, **e X, Guo W, Luo Z, Liao J, Wen F, et al. Examining the incubation period distributions of COVID-19 on Chinese patients with different travel histories. J Infect Dev Ctries. 2020;14(4):323–7.
Kong TK. Longer incubation period of coronavirus disease 2019 (COVID-19) in older adults. Aging Med (Milton). 2020;3(2):102–9.
Nie X, Fan L, Mu G, Tan Q, Wang M, **e Y, et al. Epidemiological characteristics and incubation period of 7015 confirmed cases with coronavirus disease 2019 outside Hubei Province in China. J Infect Dis. 2020;222:26–33.
Qin J, You C, Lin Q, Hu T, Yu S, Zhou XH. Estimation of incubation period distribution of COVID-19 using disease onset forward time: a novel cross-sectional and forward follow-up study. Sci Adv. 2020;6:eabc1202.
Ren X, Li Y, Yang X, Li Z, Cui J, Zhu A, et al. Evidence for pre-symptomatic transmission of coronavirus disease 2019 (COVID-19) in China. Influ Other Respir Viruses. 2021;15:19–26.
Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–85.
Huang S, Li J, Dai C, Tie Z, Xu J, **ong X, et al. Incubation period of coronavirus disease 2019: new implications for intervention and control. Int J Environ Health Res. 2021. https://doi.org/10.1080/09603123.2021.1905781.
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207.
Guo CX, He L, Yin JY, Meng XG, Tan W, Yang GP, et al. Epidemiological and clinical features of pediatric COVID-19. BMC Med. 2020;18:250.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Xu L, Chen N, Zhang X, Chen Z. An evaluation of statistical, NMME and hybrid models for drought prediction in China. J Hydrol (Amst). 2018;566:235–49.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Zhang J, Litvinova M, Wang W, Wang Y, Deng X, Chen X, et al. Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study. Lancet Infect Dis. 2020;20:793–802.
National Health Commission of China. Chinese National COVID-19 Diagnosis and Treatment Plan (Trial Eight Edition). 2021. http://www.nhc.gov.cn/yzygj/s7653p/202104/7de0b3837c8b4606a0594aeb0105232b.shtml. Accessed 25 Aug 2021. (in Chinese)
Reich NG, Lessler J, Cummings DA, Brookmeyer R. Estimating incubation period distributions with coarse data. Stat Med. 2009;28:2769–84.
Linton NM, Kobayashi T, Yang Y, Hayashi K, Akhmetzhanov AR, Jung SM, et al. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020;9:538.
Sartwell PE. The distribution of incubation periods of infectious disease. 1949. Am J Epidemiol. 1995;141:386–94.
Huang QQ, Ritchie SC, Brozynska M, Inouye M. Power, false discovery rate and Winner’s Curse in eQTL studies. Nucleic Acids Res. 2018;46:e133.
Viego V, Geri M, Castiglia J, Jouglard E. Incubation period and serial interval of Covid-19 in a chain of infections in Bahia Blanca (Argentina). Cien Saude Colet. 2020;25:3503–10.
Wong J, Chaw L, Koh WC, Alikhan MF, Jamaludin SA, Poh WWP, et al. Epidemiological Investigation of the First 135 COVID-19 cases in Brunei: implications for surveillance, control, and travel restrictions. Am J Trop Med Hyg. 2020;103:1608–13.
Pongpirul WA, Wiboonchutikul S, Charoenpong L, Panitantum N, Vachiraphan A, Uttayamakul S, et al. Clinical course and potential predictive factors for pneumonia of adult patients with Coronavirus Disease 2019 (COVID-19): a retrospective observational analysis of 193 confirmed cases in Thailand. PLoS Negl Trop Dis. 2020;14:e0008806.
The SARS-CoV-2 Variant with Lineage B.1.351 Clusters Investigation Team. Linked transmission chains of imported SARS-CoV-2 variant B.1.351 across mainland France, January 2021. Euro Surveill. 2021;26:2100333.
de Laval F, Grosset-Janin A, Delon F, Allonneau A, Tong C, Letois F, et al. Lessons learned from the investigation of a COVID-19 cluster in Creil, France: effectiveness of targeting symptomatic cases and conducting contact tracing around them. BMC Infect Dis. 2021;21:457.
Bui LV, Nguyen HT, Levine H, Nguyen HN, Nguyen TA, Nguyen TP, et al. Estimation of the incubation period of COVID-19 in Vietnam. PLoS ONE. 2020;15:e0243889.
Bohm S, Woudenberg T, Chen D, Marosevic DV, Bohmer MM, Hansen L, et al. Epidemiology and transmission characteristics of early COVID-19 cases, 20 January–19 March 2020, in Bavaria, Germany. Epidemiol Infect. 2021;149:e65.
Bohmer MM, Buchholz U, Corman VM, Hoch M, Katz K, Marosevic DV, et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. Lancet Infect Dis. 2020;20:920–8.
Patrikar SR, Kotwal A, Bhatti VK, Banerjee A, Chatterjee K, Kunte R, et al. Incubation period and reproduction number for novel coronavirus 2019 (COVID-19) infections in India. Asia Pac J Public Health. 2020;32:458–60.
Vivian Thangaraj JW, Murhekar M, Mehta Y, Kataria S, Brijwal M, Gupta N, et al. A cluster of SARS-CoV-2 infection among Italian tourists visiting India, March 2020. Indian J Med Res. 2020;151:438–43.
Tan WYT, Wong LY, Leo YS, Toh M. Does incubation period of COVID-19 vary with age? A study of epidemiologically linked cases in Singapore. Epidemiol Infect. 2020;148:e197.
Pung R, Chiew CJ, Young BE, Chin S, Chen MI, Clapham HE, et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–46.
Lee H, Kim K, Choi K, Hong S, Son H, Ryu S. Incubation period of the coronavirus disease 2019 (COVID-19) in Busan, South Korea. J Infect Chemother. 2020;26:1011–3.
Ki M, Task Force for -nCo V. Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-nCoV) disease in Korea. Epidemiol Health. 2020;42:e2020007.
Alwafi H, Naser AY, Qanash S, Brinji AS, Ghazawi MA, Alotaibi B, et al. Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc. 2021;14:839–52.
Ario AR, Mirembe BB, Biribawa C, Bulage L, Kadobera D, Wamala R. Timing of onset of symptom for COVID-19 from publicly reported confirmed cases in Uganda. Pan Afr Med J. 2021;38:168.
Ai J, Wang Y, Chen J, Liu X, Fan W, Huang G, et al. The cross-sectional study of hospitalized COVID-19 patients in **angyang. Hubei province. New Med. 2020;30:355–63 (in Chinese).
An R, Chen Z, Ayidar B, Nurahamat D, Wang Y, Liu ZQ, et al. Analysis of clinical characteristics of COVID - 19 infection pneumonia in Ili area. **njiang Med J. 2021;51(170–73):69.
Chen M, Jia HJ, Wang H, Zheng X, Wang Q. Infection status of coronavirus disease 2019 cases and close contacts in Fuzhou. Fujian. Dis Surveill. 2020;35:608–12 (in Chinese).
Chen G, Wu MZ, Qin CJ, Wu BB, Luo WR, Liu L, et al. Epidemiological analysis of 18 patients with COVID-19. Eur Rev Med Pharmacol Sci. 2020;24:12522–6.
Dai J, Yang L, Zhao J. Probable longer incubation period for elderly COVID-19 cases: analysis of 180 contact tracing data in Hubei Province, China. Risk Manag Healthc Policy. 2020;13:1111–7.
Duan Y, Jiang R, Kang W, Zhao A, Huang M. Clinical features of patients with new coronavirus pneumonia admitted to ICU in Shanxi province. J Shanxi Med Univ. 2020;51:852–7 (in Chinese).
Fang D, Ma JY, Guan J, Wang M, Song Y, Tian D, et al. Manifestations of digestive system of hospitalized patients with coronavirus disease 2019 in Wuhan, China: a single-center descriptive study. Chin J Dig. 2020;40:151–6 (in Chinese).
Fu Y, Meng Z, Yu G, Fu K, Liu A, Hu JH, et al. Analysis of epidemiology and clinical characteristics in 24 patients with COVID-19 in Liuzhou. Intern Med China. 2020;15:392–5 (in Chinese).
Han T, Hua L, He S, Zhou Y, Hou C, Chen J, et al. The epidemiological characteristics of cluster transmission of coronavirus disease 2019 (COVID-19): a multi-center study in Jiangsu Province. Am J Transl Res. 2020;12:6434–44.
Jia J, Hu X, Yang F, Song X, Dong L, Zhang J, et al. Epidemiological characteristics on the clustering nature of COVID-19 in Qingdao City, 2020: a descriptive analysis. Disaster Med Public Health Prep. 2020;14:643–7.
Jiang G, Wang C, Song L, Wang X, Zhou Y, Fei C, et al. Aerosol transmission, an indispensable route of COVID-19 spread: case study of a department-store cluster. Front Environ Sci Eng. 2021;15:46.
Jiang Y, Huang J, Zhong Y, Li Y, Wei S, Huang S, et al. Epidemiological investigation on a cluster epidemic of COVID-19. Mod Prev Med. 2020;47:3807–10 (in Chinese).
** X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002–9.
Lai C, Yu R, Wang M, **an W, Zhao X, Tang Q, et al. Shorter incubation period is associated with severe disease progression in patients with COVID-19. Virulence. 2020;11:1443–52.
Lai CKC, Ng RWY, Wong MCS, Chong KC, Yeoh YK, Chen Z, et al. Epidemiological characteristics of the first 100 cases of coronavirus disease 2019 (COVID-19) in Hong Kong Special Administrative Region, China, a city with a stringent containment policy. Int J Epidemiol. 2020;49:1096–105.
Li X, Geng X, Zhao X, Liu L, Wang W, Cui L, et al. A comprehensive analysis of 47 COVID-19 cases in **an City. J Shandong Univ (Health Sci). 2020;58:23–7 (in Chinese).
Li C, Guo H, Zheng Q, Huang B, He F, Xu J, et al. Analysis of clinical features and outcomes of young female patients with mild COVID-19. Int J Respir. 2020;40:978–81 (in Chinese).
Li X, Zhang W, Li J, An S, **ang R, Zhang M, et al. Epidemiological characteristics of coronavirus disease 2019 in the elderly in Shandong Province. Chin J Mult Organ Dis Elder. 2020;19:191–4. (in Chinese)
Li X, M. L, Zhou L, Li M, Z M, **ang R, et al. Epidemiological analysis of corona virus disease 2019 in southern Shandong region. Chin J Integr Tradit West Med Intensive Crit Care. 2020;27:35–8. (in Chinese)
Liu P, Niu R, Chen J, Tang Y, Tang W, Xu L, et al. Epidemiological and clinical features in patients with coronavirus disease 2019 outside of Wuhan, China: special focus in asymptomatic patients. PLoS Negl Trop Dis. 2021;15:e0009248.
Liu H, Gao J, Wang Y, Jie J, Luo J, Xu Y, et al. Epidemiological and clinical characteristics of 2019 novel coronavirus disease (COVID-19) in Jilin, China: a descriptive study. Medicine (Baltimore). 2020;99:e23407.
Liu L, Du Y, Bai JY, Li J, Luo Y, Wang L, et al. Analysis of early characteristics of patients with novel coronavirus infection in Kunming City, Yunnan Province. China. Chin J Zoonoses. 2020;36(424–26):28 (in Chinese).
Liu L, **g L, Li Y, Tian Y, You J, Cui J, et al. Clustering of 2019 novel coronavirus disease cases in Liaoning province:reported data-base analysis. Chin J Public Health. 2020;36:473–6. (in Chinese)
Liu G, Wang X, Lu JA, Zhao X, Lei Z, Li J, et al. The epidemic characteristics of uovel coronavirus infected pneumonia in Uingxia Hui Autonomous Region. J Ningxia Med Univ. 2020;42:109–13. (in Chinese)
Lu W, Zhou L, Chen W, Xu R, Li Y, Zhang P. Clinical characteristics of coronavirus disease 2019 in Dongguan: a retrospective study. Hainan Med J. 2021;32:85–7. (in Chinese)
Luo L, Go D. Epidemiological analysis of COVID-19 outbreak in Bazhong City in 2020. Parasitoses Infect Dis. 2020;18:117–20. (in Chinese)
Ng TC, Cheng HY, Chang HH, Liu CC, Yang CC, Jian SW, et al. Comparison of estimated effectiveness of case-based and population-based interventions on COVID-19 containment in Taiwan. JAMA Intern Med. 2021;181:913–21.
** K, Lei M, Gou Y, Tao Z, Yao G, Hu C, et al. Epidemiologic characteristics of COVID-19 in Guizhou Province, China. J Infect Dev Ctries. 2021;15:389–97.
She K, Zhang D, Qi C, Liu T, Jia Y, Zhu Y, et al. Epidemiological characteristics and incubation period of coronavirus disease 2019 in Anhui Province. J Shandong Univ (Health Sci). 2020;58:44–52. (in Chinese)
Shen J, Yu J, Yan Y, Sang Y, Qin L, Na M, et al. Clinical and chest HRCT characteristics in family group outbreak of novel coronavirus pneumonia. J Dalian Med Univ. 2020;42:32–6. (in Chinese)
Tian S, Hu N, Lou J, Chen K, Kang X, **ang Z, et al. Characteristics of COVID-19 infection in Bei**g. J Infect. 2020;80:401–6.
Wang P, Lu JA, ** Y, Zhu M, Wang L, Chen S. Statistical and network analysis of 1212 COVID-19 patients in Henan, China. Int J Infect Dis: IJID. 2020;95:391–8.
Wang Y, Liao B, Guo Y, Li F, Lei C, Zhang F, et al. Clinical characteristics of patients infected with the novel 2019 coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infect Dis. 2020;7:ofaa187.
Wang X, Zhou Q, He Y, Liu L, Ma X, Wei X, et al. Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur Respir J. 2020;55:2000544.
Wang W, Zhou S, Ying J, **e D, Zhang Q, Sun Y. Epidemiological characteristics of cluster outbreaks of COVID-19 in Neijiang. South China J Prev Med. 2020;46:243–6. (in Chinese)
Wu Y, Zhuang X, Huang H, Lin YT. Epidemiological and clinical characteristics of 41 cases of coronavirus disease 2019. Chin J Integr Tradit West Med Intensive Crit Care. 2020;27:390–3. (in Chinese)
**a XY, Wu J, Liu HL, **a H, Jia B, Huang WX. Epidemiological and initial clinical characteristics of patients with family aggregation of COVID-19. J Clin Virol. 2020;127:104360.
Yu X, Sun X, Cui P, Pan H, Lin S, Han R, et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai. China Transbound Emerg Dis. 2020;67:1697–707.
Yuan X, Qin D, Tian F, Che F, Zheng Q, Heng X. Epidemiological and clinical characteristics of patient with COVID-19. J Mol Imaging. 2020;43:381–6. (in Chinese)
Zhao C, Xu Y, Zhang X, Zhong Y, Long L, Zhan W, et al. Public health initiatives from hospitalized patients with COVID-19. China J Infect Public Health. 2020;13:1229–36.
Zhang T, Ding S, Zeng Z, Cheng H, Zhang C, Mao X, et al. Estimation of incubation period and serial interval for SARS-CoV-2 in Jiangxi, China, and an updated meta-analysis. J Infect Dev Ctries. 2021;15:326–32.
Zhong ZF, Huang J, Yang X, Peng JL, Zhang XY, Hu Y, et al. Epidemiological and clinical characteristics of COVID-19 patients in Hengyang, Hunan Province, China. World J Clin Cases. 2020;8:2554–65.
Zhou Y, Ming J, Liu S. Epidemiologic characteristics and double-buffered strategy for patients in orthopedic surgery during the novel coronavirus outbreak: Wuhan’s experience. Eur J Med Res. 2021;26:39.
Zhu N, Chen S, Yang GP, Ning S, Li X, Nian Y, et al. Analysis of the path from discovery of novel coronavirus disease 2019 cases to its diagnosis in Shaanxi Province. J **’an Jiaotong Univ (Med Sci). 2020;41:923–6. (in Chinese)
Lu QB, Zhang Y, Liu MJ, Zhang HY, Jalali N, Zhang AR, et al. Epidemiological parameters of COVID-19 and its implication for infectivity among patients in China, 1 January to 11 February 2020. Euro Surveill. 2020;25:2000250.
Yang N, Shen Y, Shi C, Ma AHY, Zhang X, Jian X, et al. In-flight transmission cluster of COVID-19: a retrospective case series. Infect Dis (Lond). 2020;52:891–901.
Shi P, Gao Y, Shen Y, Chen E, Chen H, Liu J, et al. Characteristics and evaluation of the effectiveness of monitoring and control measures for the first 69 Patients with COVID-19 from 18 January 2020 to 2 March in Wuxi, China. Sustain Cities Soc. 2021;64:102559.
Cimolai N. In pursuit of the right tail for the COVID-19 incubation period. Public Health. 2021;194:149–55.
Bikbov B, Bikbov A. Maximum incubation period for COVID-19 infection: do we need to rethink the 14-day quarantine policy? Travel Med Infect Dis. 2021;40:101976.
Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323:1915–23.
Dickens BL, Koo JR, Lim JT, Sun H, Clapham HE, Wilder-Smith A, et al. Strategies at points of entry to reduce importation risk of COVID-19 cases and reopen travel. J Travel Med. 2020;27:taaa141.
Cai Y, Liu J, Yang H, Wang M, Guo Q, Huang D, et al. Association between incubation period and clinical characteristics of patients with COVID-19. J Int Med Res. 2020;48:300060520956834.
Guan Q, Liu M, Zhuang YJ, Yuan Y, Wang SS, Li J, et al. Epidemiological investigation of a family clustering of COVID-19. Zhonghua Liu **ng Bing Xue Za Zhi. 2020;41:629–33. (in Chinese)
Hussein M, Toraih E, Elshazli R, Fawzy M, Houghton A, Tatum D, et al. Meta-analysis on serial intervals and reproductive rates for SARS-CoV-2. Ann Surg. 2020;273:416–23.
Forster P, Forster L, Renfrew C, Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci USA. 2020;117:9241–3.
Zhang M, **ao J, Deng A, Zhang Y, Zhuang Y, Hu T, et al. Transmission dynamics of an outbreak of the COVID-19 Delta variant B.1.617.2—Guangdong Province, China, May–June 2021. China CDC Weekly. 2021;7:584–6.
Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–7.
Yang L, Dai J, Zhao J, Wang Y, Deng P, Wang J. Estimation of incubation period and serial interval of COVID-19: analysis of 178 cases and 131 transmission chains in Hubei province, China. Epidemiol Infect. 2020;148:e117.
Acknowledgements
The authors would like to thank everyone who supported this study, especially thank Professor Junyuan Yang, Professor **chao Duan, and Professor Xuezhi Li.
Funding
The work was funded by the National Natural Science Foundation of China (NO.82073618 and NO.82002147); the Key Scientific Research Projects in Colleges and Universities of Henan Province [20A330004]; the National Science and Technology Specific Projects (NO.2018ZX10301407).
Author information
Authors and Affiliations
Contributions
SC and CC designed and implemented this research; CC wrote the manuscript; JG, PZ, MY, and RL collected and screened individual information on COVID-19 patients; CC, DZ, and DD analyzed the data; JX made some suggestions and polished the language; SC provided advice for the revision of the paper; GD initiated this project, interpreted the results, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Zhengzhou University Medical Ethics Committee (Zhengzhou, China). The information on all cases was collected from publicly available sources, and consent to participate was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Supplementary Information
Additional file 1.
Additional Table S1.
Additional file 2.
Additional Figures S1–S8.
Additional file 3.
Additional Figure S9.
Additional file 4.
Additional Figure S10.
Additional file 5.
Additional Figure S11.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, C., Zhang, D., Dang, D. et al. The incubation period of COVID-19: a global meta-analysis of 53 studies and a Chinese observation study of 11 545 patients. Infect Dis Poverty 10, 119 (2021). https://doi.org/10.1186/s40249-021-00901-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40249-021-00901-9