Abstract
Background
CD146 is a tight junction-associated molecule involved in maintaining endothelial barrier, and balancing immune–inflammation response, in cardiovascular disease. Notably, peripheral CD146+ cells significantly upsurge under vessel dyshomeostasis such as acute myocardial injury (AMI), appearing to be a promising therapeutic target. In this study, with a new view of gene correlation, we aim at deciphering the complex underlying mechanism of CD146+ cells’ impact in the development of AMI.
Methods
Transcription dataset GSE 66,360 of CD146+ blood cells from clinical subjects was downloaded from NCBI. Pearson networks were constructed and the clustering coefficients were calculated to disclose the differential connectivity genes (DCGs). Analysis of gene connectivity and gene expression were performed to reveal the hub genes and hub gene clusters followed by gene enrichment analysis.
Results and conclusions
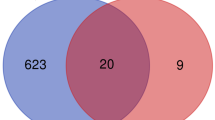
Among the total 23,520 genes, 27 genes out of 126 differential expression genes were identified as DCGs. These DCGs were found in the periphery of the networks under normal condition, but transferred to the functional center after AMI. Moreover, it was revealed that DCGs spontaneously crowded together into two functional models, CCL20 cluster and NR4A3 cluster, influencing the CD146-mediated signaling pathways during the pathology of AMI for the first time.
Similar content being viewed by others
Introduction
Cluster of differentiation 146 (CD146)/melanoma cell-associated molecule is an essential immunoglobulin-like protein initially discovered in metastatic melanoma [1]. It locates at endothelial tight junctions across all vessel beds, mediating physiological and pathological events under vascular dyshomeostasis [2, 3]. Pioneering researchers regard CD146 as a historical marker for isolating circulating endothelial cells that slough off inflamed vasculature [4]. Over several decades, CD146 has also been discovered in other cell types including mesenchymal stem cells [5], endothelial progenitor cells [6], macrophages [7], T helper 17 cells [8], B lymphocytes [9], T lymphocytes [9, 10], and natural killer cells [9]. The CD146+ circulating cells occupy about 2% of peripheral mononuclear cells in healthy individuals [9] and most notably, this percentage increases in certain conditions associated with vascular dysfunction like myocardial infarction, connective tissue diseases, and cancers [6, 11,12,13]. Moreover, CD146-activated T cells have shown an enhanced ability to interact with endothelium in adhesion, rolling, and transmigration, evidenced by human and murine studies [14, 15]. Given its multiple functions in vessel structure, angiogenesis, and lymphocyte activation and its enabled detection in the bloodstream, CD146 appears to be a potential target for vascular disorders [16,17,18].
Complex networks are of great interest to researchers in the fields of computational biology and bioinformatics [19,20,21]. It has been gradually extended from initial gene comparison to protein–protein network modeling, to protein–genetic investigation, and up to the disease–disease association exploration [22]. Most of the successful bioinformatics approaches that identify the initial key genes, however, have been based on only gene expression comparison and restrict the following analysis to the top differential expression genes (DEGs) without paying attention to the gene interaction rearrangement [23, 24]. Instead, the hub-structured network is an important motif that is, to our best knowledge, leading the genome-wide association characterization in complex networks [1: Figure S1B). The clustering coefficient fold-changes of NR4A3 and CCL20 were 15.7 and 10.2, respectively; and the gene expression fold-changes were 0.379 and 0.422, respectively. Gene connections are partly verified by the STRING datasets (Additional file 1: Figure S2).
CCL20 cluster and NR4A3 cluster formation in early-stage AMI. CCL20 and NR4A3 stay in the peripheral position of DCGs’ network under normal state (A). However, they shift to the primary position of DCGs’ network dominating two functional clusters under AMI stimulation (B). DCGs differential connectivity genes
Gene enrichment
Biological process analysis showed that DCGs were involved in response to organic substrates, positive regulation of leukocyte activation, immune response, immune system process, response to cytokine, and regulation of cytokine production. The CCL20 cluster was essential to the immune response, immune system process, and regulation of localization while the NR4A3 cluster was essential to cellular response to corticotropin-releasing hormone stimulus, positive regulation of leukocyte activation, and regulation of apoptotic process (Table 2).
Reactome pathway analysis revealed that DCGs were related to the immune system with regard to tasks such as signaling by interleukins, namely interleukin-1, interleukin-4 and interleukin-13, the innate immune system, and the dectin-2 family. The CCL20 cluster was essential to immune system, innate immune system, the dectin-2 family, and neutrophil degranulation while the NR4A3 cluster was essential to RNA Polymerase II Transcription, Generic Transcription Pathway, and MyD88 cascade initiated on plasma membrane (Table 2).
Discussion
CD146 is a junction-associated adhesion molecule that participates in immune and inflammatory pathological processes in the initiation and development of vascular diseases [2]. CD146-activated leukocytes are recruited to the inflamed endothelium to induce the expression of chemokines and cytokines and, in doing so, progressively destroy the blood vessel barrier. Our study finds that following AMI stimulation, in CD146+ human blood cells, 126 out of 23,520 genes show significant differential expression (P < 0.0001) and, among those, 27 genes show consistent connectivity changes and serve as DCGs. Unlike DEGs, DCGs are able to not only aggregate gene expression, but also encompass gene connectivity properties, internally coupling into functional gene clusters—NR4A3 cluster and CCL20 cluster—orchestrating the gene networks’ entire dynamics in CD146-associated AMI pathophysiology development. Meanwhile, NR4A3 and CCL20 are revealed as hub genes since they experienced both significant connectivity and expression changes after AMI stimuli. Furthermore, gene enrichment analysis shows that the DCGs are involved in inflammation–immune response, with CCL20 being principal to the immune response and regulation of localization; while, the NR4A3 cluster is principal to leukocyte activation, apoptotic process, and cellular response to corticotropin-releasing hormone stimulus. Such findings align with the well-known hypothesis that CD146-mediated inflammation plays an important role in the pathogenesis of AMI.
DCGs revealed by gene connectivity network
The network structural parameter analysis method is applied to weave the gene–gene correlation network. We identify DCGs which present steadily elevated connectivity under AMI conditions in both the discovery and validation cohorts, and further confirm the upregulation seen in the combination cohort. As expected, the gene expressions of DCGs are increased after AMI, but are not distinguishable from DEGs solely by expression signatures (data not shown). NR4A3 and CCL20 as Queryhighlight hub genes are also defined as AMI biomarkers after pre-filtering the comorbidity-relevant genes by the original Topol group [12]. SOCS3 tends to be the only “shared” AMI biomarker candidate revealed by other groups in which the same GSE66360 dataset is included as one of their study objects [27, 28]. Recognizing the CCL20, NR4A3, and SOCS3 as top DCGs substantiate previous outputs and, in turn, the validity of our method is enhanced. Therefore, we recommend the gene connectivity analysis, along with gene expression signature, to be used as a powerful and unbiased way for researchers to rank the importance of candidate DEGs.
The NR4A3 hub gene
NR4A3 belongs to the NR4A orphan nuclear receptor family (with NR4A2 and NR4A1), which plays an important role in AMI development. The JM Penninger group reports that NR4A3 is the highest-ranking gene in circulating human endothelial cells under atherosclerosis [37]. Transcription analysis of human left ventricular myocardium shows that NR4A3 upregulates during ischemia and reperfusion in normal and chronic ischemic myocardium [38]. Similarly, NR4A3 is found to be elevated 10 days post-left anterior descending artery ligation ischemia surgery in mice [39]. Overexpression of NR4A3 significantly reduces infarct size, preventing deterioration of left ventricular function and repression of neutrophil infiltration in the heart of mice after coronary artery ligation and relates to the activation of JAK2/STAT3 and the inhibition of STAT3-dependent NF-κB signaling pathways [40]. Additionally, it has to be pointed out that the NR4A subgroup, including NR4A3, is an immediate early response gene induced by diverse physiological stimuli, i.e., mechanical agitation, calcium, and inflammation cytokines [41]. This reinforces our data that, in very early-stage AMI, NR4A3 has a significant 16-fold clustering coefficient climb and 42% gene expression increase. Yet, despite these characteristics, implications of the nuclear factor NR4A3 in CD146+-related myocardial disorders remain a mystery.
The CCL20 hub gene
CCL20, a C–C motif chemokine, is a chemoattractant for recruiting leukocytes to sites of injury and inflammation. CCL20 secretion is induced by pro-inflammatory chemokines and cytokines, such as CXCL12, IL17, IL1β, IL6, and is in part related to JAK/STAT pathway signaling in multiple cell types [42,43,44]. IL6 and soluble IL6 receptor stimulate STAT3 binding to the CCL20 promotor, and IL17 stimulates the phosphorylated NF-κB binding to the CCL20 promoter in murine astrocytes, facilitate neuroinflammation within the central nervous system [42]. In addition, the co-expression of CCL20 receptor CCR6 and CD146 is a marker of effector memory Th17 cells which mediate migration and is thought to be essential for inflammation in human psoriasis [8]. Moreover, it is reported that CCL20 levels are elevated in the serum of clinical patients with ischemic myocardial infarction [45, 46]. In vitro study shows that CCL20 expression increases in CD146+ human mesenchymal stromal cells at the early pro-inflammatory phase in fracture healing [47]. Thus, we hypothesize that CCL20 binding its receptor CCR6 is likely what drives the CD146-mediated vessel inflammation progress in early AMI phase.
Functional gene clusters
In terms of functional models, DCGs are self-organized into two clusters, the NR4A3 and CCL20 clusters, with 18 genes and 12 genes in each cluster, respectively. All genes are directly linked to its hub gene and partly linked to adjacent genes. Protein–protein connection analyzed by STRING database produces a structure that is greatly similar to our network pattern in which CCL20 connects with CXCL16, IL1R2, MMP9, NLRP3, BCL6 LILRB2, PELI1, CLEC4E, FCER1G, and NR4A3 connects with NR4A2, FOSL2, RNF144B, CDKN1A, SOCS3. A few of the gene–gene correlations within clusters are stated in inflammatory diseases. MMP9 activation correlates with CCL20 expression in astrocytes via Notch-1/Akt/NF-κB pathway promoting leukocyte migration across the blood–brain barrier [48]. NR4A2 and NR4A3 as orphan nuclear receptors mediate neutrophil number and survival in chronic inflammatory signals in multiple hematologic disorders [49,50,51]. FOSL2 acts as an activating protein-1 transcription factor promoting hematopoietic progenitor cells transition to macrophages and neutrophils in an SOCS3-dependent manner is reported [52]. Nevertheless, most of the cluster functions are rarely reported in AMI pathogenesis.
Taken together, NR4A3 and CCL20 clusters are novel functional modules in CD146+ cell-mediated immunoinflammatory balance, triggering increased susceptibility to vascular deterioration and accelerating myocardial injury. Meanwhile, we propose that NR4A3 and CCL20 are promising biomarkers for clinical diagnosis and potential therapeutic candidates since they largely impact the early AMI development. In-depth studies are necessary for understanding the mechanisms of peripheral CD146+ cells in cardiovascular disease.
Availability of data and materials
All data are included in the manuscript.
References
Lehmann JM, Holzmann B, Breitbart EW, Schmiegelow P, Riethmüller G, Johnson JP. Discrimination between benign and malignant cells of melanocytic lineage by two novel antigens, a glycoprotein with a molecular weight of 1,13,000 and a protein with a molecular weight of 76,000. Can Res. 1987;47(3):841–5.
Shih IM. The role of CD146 (Mel-CAM) in biology and pathology. J Pathol. 1999;189(1):4–11.
Tu T, Zhang C, Yan H, Luo Y, Kong R, Wen P, et al. CD146 acts as a novel receptor for netrin-1 in promoting angiogenesis and vascular development. Cell Res. 2015;25(3):275–87.
Widemann A, Sabatier F, Arnaud L, Bonello L, Al-Massarani G, Paganelli F, et al. CD146-based immunomagnetic enrichment followed by multiparameter flow cytometry: a new approach to counting circulating endothelial cells. J Thromb Haemost. 2008;6(5):869–76.
Espagnolle N, Guilloton F, Deschaseaux F, Gadelorge M, Sensébé L, Bourin P. CD 146 expression on mesenchymal stem cells is associated with their vascular smooth muscle commitment. J Cell Mol Med. 2014;18(1):104–14.
Delorme B, Basire A, Gentile C, Sabatier F, Monsonis F, Desouches C, et al. Presence of endothelial progenitor cells, distinct from mature endothelial cells, within human CD146+ blood cells. Thromb Haemost. 2005;94(6):1270.
Luo Y, Duan H, Qian Y, Feng L, Wu Z, Wang F, et al. Macrophagic CD146 promotes foam cell formation and retention during atherosclerosis. Cell Res. 2017;27(3):352–72.
Kamiyama T, Watanabe H, Iijima M, Miyazaki A, Iwamoto S. Coexpression of CCR6 and CD146 (MCAM) is a marker of effector memory T-helper 17 cells. J Dermatol. 2012;39(10):838–42.
Elshal MF, Khan SS, Takahashi Y, Solomon MA, McCoy JP. CD146 (Mel-CAM), an adhesion marker of endothelial cells, is a novel marker of lymphocyte subset activation in normal peripheral blood. Blood. 2005;106(8):2923–4.
Duda DG, Cohen KS, di Tomaso E, Au P, Klein RJ, Scadden DT, et al. Differential CD146 expression on circulating versus tissue endothelial cells in rectal cancer patients: implications for circulating endothelial and progenitor cells as biomarkers for antiangiogenic therapy. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(9):1449.
Had**icolaou A, Wu L, Fang B, Watson P, Hall F, Busch R. Relationship of CD146 expression to activation of circulating T cells: exploratory studies in healthy donors and patients with connective tissue diseases. Clin Exp Immunol. 2013;174(1):73–88.
Muse ED, Kramer ER, Wang H, Barrett P, Parviz F, Novotny MA, et al. A whole blood molecular signature for acute myocardial infarction. Sci Rep. 2017;7(1):1–9.
Fürstenberger G, Von Moos R, Senn H, Boneberg E. Real-time PCR of CD146 mRNA in peripheral blood enables the relative quantification of circulating endothelial cells and is an indicator of angiogenesis. Br J Cancer. 2005;93(7):793–8.
Guezguez B, Vigneron P, Lamerant N, Kieda C, Jaffredo T, Dunon D. Dual role of melanoma cell adhesion molecule (MCAM)/CD146 in lymphocyte endothelium interaction: MCAM/CD146 promotes rolling via microvilli induction in lymphocyte and is an endothelial adhesion receptor. J Immunol. 2007;179(10):6673–85.
Dagur PK, McCoy JP Jr. Endothelial-binding, proinflammatory T cells identified by MCAM (CD146) expression: characterization and role in human autoimmune diseases. Autoimmun Rev. 2015;14(5):415–22.
Leroyer AS, Blin MG, Bachelier R, Bardin N, Blot-Chabaud M, Dignat-George F. CD146 (cluster of differentiation 146) an adhesion molecule involved in vessel homeostasis. Arterioscler Thromb Vasc Biol. 2019;39(6):1026–33.
Gallastegi T, Soto B, Romero JM, Galán M, Escudero JR, Camacho M. MCAM/CD146 which is differentially expressed in vascular diseases, is a potential biomarker in abdominal aortic aneurysm. Eur J Vasc Endovasc Surg. 2019;58(6):e454.
Wang Z, Yan X. CD146, a multi-functional molecule beyond adhesion. Cancer Lett. 2013;330(2):150–62.
Milo R, Shen-Orr S, Itzkovitz S, Kashtan N, Chklovskii D, Alon U. Network motifs: simple building blocks of complex networks. Science. 2002;298(5594):824–7.
Zhao Z, Li C, Zhang X, Chiclana F, Viedma EH. An incremental method to detect communities in dynamic evolving social networks. Knowl-Based Syst. 2019;163:404–15.
Liu Y-Y, Slotine J-J, Barabási A-L. Controllability of complex networks. Nature. 2011;473(7346):167–73.
Goh K-I, Cusick ME, Valle D, Childs B, Vidal M, Barabási A-L. The human disease network. Proc Natl Acad Sci. 2007;104(21):8685–90.
Akat KM, Morozov P, Brown M, Gogakos T, Da Rosa JC, Mihailovic A, et al. Comparative RNA-sequencing analysis of myocardial and circulating small RNAs in human heart failure and their utility as biomarkers. Proc Natl Acad Sci. 2014;111(30):11151–6.
Eicher JD, Wakabayashi Y, Vitseva O, Esa N, Yang Y, Zhu J, et al. Characterization of the platelet transcriptome by RNA sequencing in patients with acute myocardial infarction. Platelets. 2016;27(3):230–9.
**ao M, Zheng WX, Jiang G, Cao J. Stability and bifurcation analysis of arbitrarily high-dimensional genetic regulatory networks with hub structure and bidirectional coupling. IEEE Trans Circuits Syst I Regul Pap. 2016;63(8):1243–54.
De Domenico M, Nicosia V, Arenas A, Latora V. Structural reducibility of multilayer networks. Nat Commun. 2015;6(1):1–9.
Cheng M, An S, Li J. Identifying key genes associated with acute myocardial infarction. Medicine. 2017. https://doi.org/10.1097/MD.0000000000007741.
Ge WH, Lin Y, Li S, Zong X, Ge ZC. Identification of biomarkers for early diagnosis of acute myocardial infarction. J Cell Biochem. 2018;119(1):650–8.
Qiu L, Liu X. Identification of key genes involved in myocardial infarction. Eur J Med Res. 2019;24(1):22.
Guo Y, Wu C, Guo M, Liu X, Keinan A. Gene-based nonparametric testing of interactions using distance correlation coefficient in case-control association studies. Genes. 2018;9(12):608.
Wang Y, Chi X, Meng D. The application of network structure analysis in the study of disease mechanisms. In: 2019 IEEE International Conference on Bioinformatics and Biomedicine (BIBM). IEEE: Piscataway; 2019.
Opsahl T. Triadic closure in two-mode networks: redefining the global and local clustering coefficients. Soc Netw. 2013;35(2):159–67.
Wang Y, Kou Y, Meng D. Network structure analysis identifying key genes of autism and its mechanism. Comput Math Methods Med. 2020. https://doi.org/10.1155/2020/3753080.
Galton F. Typical laws of heredity. III Nature. 1877;15(389):512–4.
Jeong H, Tombor B, Albert R, Oltvai ZN, Barabási A-L. The large-scale organization of metabolic networks. Nature. 2000;407(6804):651–4.
Jeong H, Mason SP, Barabási A-L, Oltvai ZN. Lethality and centrality in protein networks. Nature. 2001;411(6833):41–2.
Barrett P, Topol EJ. TCT-639 NR4A3 as a gene expression marker of acute atherosclerotic plaque rupture in STEMI. J Am Coll Cardiol. 2013;62(18 Supplement 1):B194.
Gabrielsen A, Lawler PR, Yongzhong W, Steinbrüchel D, Blagoja D, Paulsson-Berne G, et al. Gene expression signals involved in ischemic injury, extracellular matrix composition and fibrosis defined by global mRNA profiling of the human left ventricular myocardium. J Mol Cell Cardiol. 2007;42(4):870–83.
Haubner BJ, Adamowicz-Brice M, Khadayate S, Tiefenthaler V, Metzler B, Aitman T, et al. Complete cardiac regeneration in a mouse model of myocardial infarction. Aging. 2012;4(12):966.
Jiang Y, Feng Y-P, Tang L-X, Yan Y-L, Bai J-W. The protective role of NR4A3 in acute myocardial infarction by suppressing inflammatory responses via JAK2-STAT3/NF-κB pathway. Biochem Biophys Res Commun. 2019;517(4):697–702.
Maxwell MA, Muscat GE. The NR4A subgroup: immediate early response genes with pleiotropic physiological roles. Nucl Recept Signal. 2006;4(1):nrs.04002.
Meares GP, Ma X, Qin H, Benveniste EN. Regulation of CCL20 expression in astrocytes by IL-6 and IL-17. Glia. 2012;60(5):771–81.
Beider K, Abraham M, Begin M, Wald H, Weiss ID, Wald O, et al. Interaction between CXCR4 and CCL20 pathways regulates tumor growth. PloS ONE. 2009;4(4):e5125.
Hosokawa Y, Shindo S, Hosokawa I, Ozaki K, Matsuo T. IL-6 trans-signaling enhances CCL20 production from IL-1β-stimulated human periodontal ligament cells. Inflammation. 2014;37(2):381–6.
Lin C-F, Su C-J, Liu J-H, Chen S-T, Huang H-L, Pan S-L. Potential effects of CXCL9 and CCL20 on cardiac fibrosis in patients with myocardial infarction and isoproterenol-treated rats. J Clin Med. 2019;8(5):659.
Safa A, Rashidinejad H, Khalili M, Dabiri S, Nemati M, Mohammadi M, et al. Higher circulating levels of chemokines CXCL10, CCL20 and CCL22 in patients with ischemic heart disease. Cytokine. 2016;83:147–57.
Herrmann M, Stanić B, Hildebrand M, Alini M, Verrier S. In vitro simulation of the early proinflammatory phase in fracture healing reveals strong immunomodulatory effects of CD146-positive mesenchymal stromal cells. J Tissue Eng Regen Med. 2019;13(8):1466–81.
Song J, Wu C, Korpos E, Zhang X, Agrawal SM, Wang Y, et al. Focal MMP-2 and MMP-9 activity at the blood-brain barrier promotes chemokine-induced leukocyte migration. Cell Rep. 2015;10(7):1040–54.
McMorrow JP, Murphy EP. Inflammation: a role for NR4A orphan nuclear receptors? Biochem Soc Trans. 2011;39(2):688–93.
Prince LR, Prosseda SD, Higgins K, Carlring J, Prestwich EC, Ogryzko NV, et al. NR4A orphan nuclear receptor family members, NR4A2 and NR4A3, regulate neutrophil number and survival. Blood J Am Soc Hematol. 2017;130(8):1014–25.
Liu H, Liu P, Shi X, Yin D, Zhao J. NR4A2 protects cardiomyocytes against myocardial infarction injury by promoting autophagy. Cell Death Discov. 2018;4(1):1–11.
Croker BA, Mielke LA, Wormald S, Metcalf D, Kiu H, Alexander WS, et al. Socs3 maintains the specificity of biological responses to cytokine signals during granulocyte and macrophage differentiation. Exp Hematol. 2008;36(7):786–98.
Acknowledgements
The authors would like to acknowledge the authors of primary study, the Topol group.
Funding
This research was supported by the Cultivation Project of Young and Innovative Talents in Universities of Shandong Province and by NSFC Grant 11501331. Support of T.W., J.M.S. and S.P.M. from NIH R01 NS096186.
Author information
Authors and Affiliations
Contributions
YW, DM and TW did the overall design of the study. JMS was the language editor for the manuscript. CL contributed to the igraph figures. All authors were involved in the analysis of the data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not required. The data are available in the NCBI database.
Consent for publication
Not required.
Competing interests
No competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
A CCL20 cluster genes. B NR4A3 cluster genes. Figure S2. Protein-protein connection of DCGs by STRING database.
Additional file 2: Table S1.
Power-law indexes of degree distribution for the control network in the discovery and validation cohorts. Table S2. Clustering coefficients of DCGs in the discovery cohort, the validation cohort, and the discovery + validation cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Yh., Li, Cx., Stephenson, J.M. et al. NR4A3 and CCL20 clusters dominate the genetic networks in CD146+ blood cells during acute myocardial infarction in humans. Eur J Med Res 26, 113 (2021). https://doi.org/10.1186/s40001-021-00586-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-021-00586-8