Abstract
Background
In the initial phase of the SARS-CoV-2 pandemic, masking has been widely accepted in healthcare institutions to mitigate the risk of healthcare-associated infection. Evidence, however, is still scant and the role of masks in preventing healthcare-associated SARS-CoV-2 acquisition remains unclear.We investigated the association of variation in institutional mask policies with healthcare-associated SARS-CoV-2 infections in acute care hospitals in Switzerland during the BA.4/5 2022 wave.
Methods
SARS-CoV-2 infections in hospitalized patients between June 1 and September 5, 2022, were obtained from the “Hospital-based surveillance of COVID-19 in Switzerland”-database and classified as healthcare- or community-associated based on time of disease onset. Institutions provided information regarding institutional masking policies for healthcare workers and other prevention policies. The percentage of healthcare-associated SARS-CoV-2 infections was calculated per institution and per type of mask policy. The association of healthcare-associated SARS-CoV-2 infections with mask policies was tested using a negative binominal mixed-effect model.
Results
We included 2’980 SARS-CoV-2 infections from 13 institutions, 444 (15%) were classified as healthcare-associated. Between June 20 and June 30, 2022, six (46%) institutions switched to a more stringent mask policy. The percentage of healthcare-associated infections subsequently declined in institutions with policy switch but not in the others. In particular, the switch from situative masking (standard precautions) to general masking of HCW in contact with patients was followed by a strong reduction of healthcare-associated infections (rate ratio 0.39, 95% CI 0.30–0.49). In contrast, when compared across hospitals, the percentage of health-care associated infections was not related to mask policies.
Conclusions
Our findings suggest switching to a more stringent mask policy may be beneficial during increases of healthcare-associated SARS-CoV-2 infections at an institutional level.
Similar content being viewed by others
Background
The wearing of a medical mask has been shown to be associated with a decreased risk of acquiring severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) infection (1). In the living guideline on infection prevention and control of coronavirus disease (COVID-19), the World Health Organization (WHO) recommends all healthcare workers (HCW) to wear a well-fitting medical mask at all times within the health facility in areas of known or suspected community or cluster transmission (2). Inpatients are required to wear a medical mask if physical distancing of at least one metre cannot be maintained or when leaving their care area, provided there are no contraindications. The evidence base for this recommendation were five observational studies that found that implementing a universal masking policy in hospital systems was associated with a decreased risk of healthcare-acquired SARS-CoV-2 infection (3,4,5,6,7). It is acknowledged in the recommendation that these studies have limitations, mainly due to before-and-after design issues. Therefore, the certainty of evidence was considered “very low”. Nevertheless, as the literature provided only limited insight into associated detrimental effects, the WHO Guideline Development Group judged that the benefits of implementing universal mask use in healthcare facilities outweighed potential harms.
As a result of this recommendation, universal masking continues to be widely accepted in healthcare facilities worldwide, even with the emergence of the SARS-CoV-2 Omicron variant and widespread population immunity resulting from previous SARS-CoV-2 infection and/or vaccination (8). More recent evidence on this topic is currently unavailable, and expert opinion points towards using a mask for protection of all patients from all respiratory viral infections «when viral activity is elevated and for the most vulnerable patients year-round». However, these statements have been derived from mainly influenza-focused investigations (9).
In Switzerland, the mandatory indoor mask-wearing regulation was lifted on April 1, 2022, across all settings, including healthcare facilities. Thereafter, hospital policies on mask use were based on cantonal requirements or recommendations of Swissnoso, the Swiss National Center for Infection Control, that were regularly updated according to the epidemiological situation (10). Hence, masking policies varied between hospitals ever since, including the period of increased community circulation of BA.4/5 in summer 2022.
This study explores to what extent variation in institutional mask policy was associated with the occurrence of healthcare-associated SARS-CoV-2 infections in different institutions in Switzerland during the BA.4/5 2022 summer wave. We therefore analysed a national database that prospectively collected SARS-CoV-2 infections in hospitalized patients in large Swiss hospitals since 2020.
Methods
Patient-level data
Patient-level data was obtained from the COVID-19 Hospital Based Surveillance System (CH-SUR) database, which captured the details of COVID-19 cases from 20 large adult and pediatric hospitals in Switzerland. The study design and procedures of the CH-SUR study have been described previously (11). Data extraction and processing for this study are detailed in the supplement. All laboratory confirmed COVID-19 episodes (including polymerase chain reaction tests and antigen tests) with hospitalization for > 24 hours reported to the database were included. The mandatory information on date of hospital entry, demographics and episode declaration (classification, date of symptom onset, date of COVID-19 testing, laboratory result), as reported on the case report form, were used for our analysis.
Episodes were classified as either healthcare-associated (if symptom onset was > 5 days after admission date), or community-associated (earlier symptom onset). The time limit of 5 days was chosen to account for the incubation time of the virus, in line with the national recommendations of Swissnoso for healthcare-associated COVID-19 at the time of database development (12). The classification was provided by the reporting institution and verified using the reported dates of hospital entry and symptom onset. Episodes classified as “unknown” or "acquired from another healthcare institution" by the reporting institution were treated as community-associated in our verification and analysis.
Institution-level data
All institutions participating in CH-SUR were invited to provide information about their infection prevention policies during the BA.4/5 wave, the time frame being set as 1 June to 31 August 2022, by means of a questionnaire. Questions included the total number of inpatient admissions and patient-days during this time period, mask policies (which could change over time), testing and screening policies and work policies for ill healthcare professionals; testing and screening policies as well as isolation precautions (including duration) for inpatients; and visitor restriction policies.
Mask policy – the main predictor variable – was classified as “standard precautions”, defined as wearing masks in contact with infected patients (policy 1); “mask in contact with patients”, defined as mandatory masking in contact with all patients regardless of diagnoses or symptoms (policy 2); “mask in contact with all contacts”, defined as mandatory masking in face-to-face contacts with all patients and also colleagues (policy 3) or “mask at all times”, indicating the policy where mask use was demanded regardless of activity or contact (policy 4). The term “mask” refers to at least a surgical mask. In most institutions, healthcare professionals could also opt for a respirator mask. If the mask policy changed during the time period considered, date(s) of switch were reported.
Inclusion and exclusion criteria
For this study, we extracted all episodes in patients hospitalized between June 1 and September 5, 2022, and with a derived infection date (five days before symptom onset) between June 1 and August 31, 2022. Episodes with conflicting classification, i.e. classified as community-associated by the reporting institution but with documented disease onset > 5 days after admission or classified as healthcare-associated despite disease onset being documented within 5 days after admission, were excluded. Additionally, we excluded episodes whose incubation period could not be attributed to a mask policy, e.g. episodes with a derived infection date between June 1 and June 5, 2022, in institutions that changed the mask policy during this time.
Outcome measures and statistical analysis
Data were summarized by calculating the percentage of healthcare-associated SARS-CoV-2 infections per institution and (for institutions with policy switch) per mask policy, as the number of healthcare-associated cases divided by the total number of cases with SARS-CoV-2 infections in the same institution under the same mask policy. Attribution of SARS-CoV-2 episodes to a mask policy was based on derived infection date. If an institution switched back to its initial policy at the end of the time window (hospitals 1, 3 and 4, see Fig. 1), the two periods with identical mask policy were pooled. Percentages are shown with 95% Wilson confidence intervals.
The percentage of healthcare-associated SARS-CoV-2 infections was also calculated per institution for the entire time window to examine its association with the mean duration of stay per patient, a known risk factor for healthcare-associated SARS-CoV-2 (13). Because mean duration of stay (number of patient-days divided by number of admissions) was reported by institutions for the entire time window, this analysis only shows between-hospital differences.
The association of mask policy with the relative frequency of healthcare-associated SARS-CoV-2 infections (per institution and mask policy) was tested with a negative binominal mixed-effect model, including the number of healthcare-associated SARS-CoV-2 infections as outcome, the log-transformed number of community-acquired SARS-CoV-2 infections as offset (to standardize the outcome), mask policy as main predictor and mean duration of patient stay as covariable. To account for intra-hospital clustering, the institutions were included as random effects. In a subgroup analysis, the effect of switching from standard precautions to any policy including the masking of HCW in contact with patients was investigated. Only three hospitals performed this type of switch in late June 2022. Therefore, the model included hospitals as fixed effect to account for all between-hospital differences, and the two policy types as predictor.
Information about possible confounders (testing and screening policy, isolation precautions policy, visitor regulations, vaccination status) was not included in statistical analyses because, a) there was not much variation among institutions, and because b) the sample size did not allow more variables to be considered.
All analyses were performed in R, Version 4.02 (R Foundation, Vienna, Austria) using the packages lme4 and glmmTMB. Two-tailed tests were performed and p-values < 0.05 were considered statistically significant.
Results
Fourteen hospitals participated in the study and provided institution-level data. Patient-level data were obtained from CH-SUR for these 14 hospitals. The dataset comprised 4’023 records which met the inclusion criteria; 115 reports were identified as duplicates belonging to the same episode, 316 were excluded due to symptom onset before June 6 (i.e. derived infection date outside the time window), 612 exclusions were made based on incomplete or inconsistent data. This also led to exclusion of one institution. Therefore, 13 institutions ended up being included in the analysis. Among the remaining 2’980 episodes, 444 (14.9%) were identified as healthcare-associated SARS-CoV-2 infection (see web-only Supplementary figure S1).
Six out of the 13 (46%) included institutions reported a switch to a more stringent policy between June 20 and June 30, 2022. Two institutions switched from policy 1 (standard precautions) to policy 2 (during patient contacts), two from policy 2 to policy 3, (with all contacts) and two switched from policy 1 or 2 to policy 4 (at all times). Three of these institutions made simultaneous changes to mask policy for visitors, requiring them to wear a mask when prior to that no restrictions were present. An overview of policies is given in Fig. 1. Other precautionary policies are detailed in the Supplement.
Distribution of percentage of healthcare-associated infections between June 1 and August 31, 2022
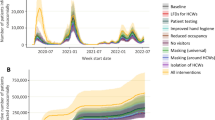
The total number of SARS-CoV-2 infections increased until mid-June in the six institutions that switched to a more stringent mask policy, and until early July in the institutions without policy switch (Fig. 2). Subsequently the number of SARS-CoV-2 infections declined in both groups of institutions.
In institutions with policy switch, the percentage of healthcare-associated SARS-CoV-2 infections sharply increased before the switch, followed by a sharp and continuing decrease after the switch. Conversely, in institutions without policy switch, the percentage of healthcare-associated SARS-CoV-2 fluctuated with a slightly increasing trend until mid August (Fig. 2).
Weekly percentage of health-care associated infections (rich colors) and overall SARS-CoV-2 infection number per week (transparent colors), separately for institutions with and without mask policy switch. The red bar indicates the time period during which six institutions switched to a more stringent mask policy
Percentage of healthcare-associated infections
Across institutions, there was a wide variation in the percentage of healthcare-associated SARS-CoV-2 infections. This variation was related to the mean duration of patient stay: hospitals with longer stays reported higher percentages of healthcare-associated SARS-CoV-2 infections (Fig. 3). Furthermore, statistical modelling revealed a statistically significant association of healthcare-associated infection rates with mask policies after adjusting for mean duration of patient stay (Table 1): compared with standard precautions, all other mask policies were associated with a reduced rate of healthcare-associated infections (rate ratios; RR < 1).
Percentage of healthcare-associated SARS-CoV-2 infections in relation to mean duration of patient stay. Each circle represents one hospital, circle size is proportional to hospital size (total number of patient-days from June to August 2022); hospital 11 is not included due to missing data on duration of patient stay
For institutions with policy switch, Fig. 4 shows that in 4/6 (66%) institutions the percentage of healthcare-associated SARS-CoV-2 infection decreased with change to a more stringent mask policy. All hospitals switching from policy 1 to a policy requiring at least general masking with patients reported much lower percentages of healthcare-associated SARS-CoV-2 infection after the policy change (RR 0.39, 95% CI 0.30 to 0.49). Conversely, among institutions without change in mask policy, there was no clear association between percentage of healthcare-associated SARS-CoV-2 infection and mask policy (Fig. 4).
Discussion
In the present investigation, we analysed data for healthcare-associated SARS-CoV-2 infection during the BA.4/5 wave in summer 2022 in dependence of mask and other policies in 13 Swiss hospitals. We could demonstrate the tendency for a decline in healthcare-associated SARS-CoV-2 infections with more stringent mask policies when the percentage of healthcare-associated infection rose. This has been found to correlate with the level of community transmission, which is reflected in our results given the setting of the BA.4/5 wave (14). Although no clear association could be found for the mask policies themselves in the inter-institutional comparison, an intra-institutional switch was associated with a reduction in healthcare-associated SARS-CoV-2 infections. In institutions without a policy switch, the distribution of healthcare-associated infections percentages was similar to community-acquired infections that mirrored the epidemiological curve of the BA.4/5 wave in Switzerland. The course of percentages of healthcare-associated infections in these showed a much slighter increase and even periods of decrease. The factors contributing to this development should be investigated further, but cannot be answered by the data at hand.
We further observed that for other prevention measure policies regarding visitors, HCWs and patients such as repeated testing, social distancing or isolation precautions the majority of institutions were in concordance, with some taking to a more cautious approach. Also, in contrast to mask policies, only few switches were observed regarding other policies.
Overall, our findings suggest that a switch to a more stringent mask policy in acute care institutions is associated with a reduction of healthcare-associated acquisition of SARS-CoV-2. The association of stringent mask policies with prevention of healthcare-associated transmission has been demonstrated for SARS-CoV-2 (15, 16), as well as other respiratory viral diseases, including RSV (17, 18), SARS (19, 20) and influenza (21). For the latter, a strict mask policy for staff on wards with at least three cases led to a 50% reduction in healthcare-associated influenza cases over three consecutive influenza seasons. The acquisition of viral respiratory disease by HCW has been shown to be reduced after introducing the use of masks, not only for SARS-CoV-2 (22,23,24) but also for Middle East Respiratory Syndrome-Coronavirus (25) and influenza (26). Due to missing data, we could not evaluate the latter relation in the current study.
However, considering the small number of hospitals included in this analysis and given the varying percentages of healthcare-associated infections overall, the association observed should be interpreted with caution. Since a change in mask policy is most commonly part of an intervention bundle, the correlation may not be attributable to mask use exclusively. Implementation of infection prevention bundles may also be a precautionary reaction to a rise in community transmission levels before this translates to an increase of healthcare-associated infections or result from intra-institutional outbreaks. Other factors such as testing and screening policies for patients and HCW, isolation precautions and visitor regulations, room occupancies, vaccination status of both HCW and patients or institutional custom regarding working with confirmed SARS-CoV-2 infections have not been taken into account but must be expected to also influence the rate of healthcare-associated SARS-CoV-2 infections (27,28,29,30). Finally, the change in policy creates awareness by influencing the daily routine of HCW, which may also contribute to the association found.
Limitations
Our study has several limitations. First, these data are from a limited number of institutions in a single country during the 2022 SARS-CoV-2 Omicron Summer wave. They cannot necessarily be generalized to other geographical regions, other viral variants and other epidemiological and seasonal circumstances. Second, due to sample size limitations, we were not able to include other policy measures or vaccination status in our statistical models and other factors, such as regional differences in community transmission levels may influence the frequency of healthcare-associated SARS-CoV-2 infections but could not be taken into account. Third, the reasons for a policy switch were not documented and may also reflect precaution in light of rising community transmission levels or be the reaction to intra-institutional outbreak situations which may confound the results. However, we would expect this to result in a more conservative estimate of healthcare-associated SARS-CoV-2 infections’ percentages and the consistency of our approach ensures the internal validity of our results.
Conclusion
Our findings support the use of masks in the prevention of healthcare-associated SARS-CoV-2 infection and a switch to a more stringent policy may be beneficial, especially when the rate of healthcare-associated infections increases.
Data availability
The dataset supporting the conclusions of this article are available on request from the Hospital-based surveillance of COVID-19 in Switzerland (CH-SUR) main investigators which can be contacted here [https://www.unige.ch/medecine/hospital-covid/].
Abbreviations
- SARS-CoV-2:
-
severe acute respiratory syndrome coronavirus type 2
- COVID-19:
-
coronavirus disease 2019
- HCW:
-
healthcare workers
- WHO:
-
World Health Organization
- CH-SUR:
-
COVID-19 Hospital Based Surveillance System (CH-SUR)
- CCER:
-
Geneva Ethics Committee
- BASEC:
-
Business Administration System for Ethics Committees
- RR:
-
Rate ratio
References
Chou R, Dana T, Jungbauer R, Weeks C, McDonagh MS. Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings: A Living Rapid Review. Ann Intern Med. 2020;173(7):542–55.
Organization WH. Infection prevention and control in the context of coronavirus disease (COVID-19): A living guideline. Updated Chapter: Mask use, Part 1: Health care settings.; 2022 25 April 2022.
Wang DD, O'Neill WW, Zervos MJ, McKinnon JE, Allard D, Alangaden GJ, et al. Association Between Implementation of a Universal Face Mask Policy for Healthcare Workers in a Health Care System and SARS-CoV-2 Positivity Testing Rate in Healthcare Workers. J Occup Environ Med. 2021;63(6):476–81.
Seidelman JL, Lewis SS, Advani SD, Akinboyo IC, Epling C, Case M, et al. Universal masking is an effective strategy to flatten the severe acute respiratory coronavirus virus 2 (SARS-CoV-2) healthcare worker epidemiologic curve. Infect Control Hosp Epidemiol. 2020;41(12):1466–7.
Temkin E, Schwaber MJ, Vaturi A, Nadir E, Zilber R, Barel O, et al. Effect of a national policy of universal masking and uniform criteria for severe acute respiratory coronavirus virus 2 (SARS-CoV-2) exposure on hospital staff infection and quarantine. Infect Control Hosp Epidemiol. 2022;43(6):757–63.
Lan FY, Christophi CA, Buley J, Iliaki E, Bruno-Murtha LA, Sayah AJ, et al. Effects of universal masking on Massachusetts healthcare workers’ COVID-19 incidence. Occup Med (Lond). 2020;70(8):606–9.
Wang X, Ferro EG, Zhou G, Hashimoto D, Bhatt DL. Association Between Universal Masking in a Health Care System and SARS-CoV-2 Positivity Among Health Care Workers. JAMA. 2020;324(7):703–4.
Shenoy ES, Babcock HM, Brust KB, Calderwood MS, Doron S, Malani AN, et al. Universal Masking in Health Care Settings: A Pandemic Strategy Whose Time Has Come and Gone, For Now. Ann Intern Med. 2023;176(6):859–61.
Klompas M, Baker MA, Rhee C, Baden LR. Strategic Masking to Protect Patients from All Respiratory Viral Infections. N Engl J Med. 2023;389(1):4–6.
Swissnoso. Swissnoso Empfehlungen zu COVID-19-Vorsorgemassnahmen in Akutspitälern v3.1. 2022 21. Juni 2022.
Thiabaud A, Iten A, Balmelli C, Senn L, Troillet N, Widmer A, et al. Cohort profile: SARS-CoV-2/COVID-19 hospitalised patients in Switzerland. Swiss Med Wkly. 2021;151:w20475.
Swissnoso. Swissnoso - Prevention & control of healthcare-associated COVID-19 outbreaks. 2020.
Mo Y, Eyre DW, Lumley SF, Walker TM, Shaw RH, O'Donnell D, et al. Transmission of community- and hospital-acquired SARS-CoV-2 in hospital settings in the UK: A cohort study. PLoS Med. 2021;18(10):e1003816.
Suwono B, Brandl M, Hecht J, Eckmanns T, Haller S. Epidemiology of healthcare-associated SARS-CoV-2 outbreaks in Germany between March 2020 and May 2022. J Hosp Infect. 2023;134:108–20.
Lawton T, Butler M, Peters C. Airborne protection for staff is associated with reduced hospital-acquired COVID-19 in English NHS trusts. J Hosp Infect. 2022;120:81–4.
Zhang GQ, Pan HQ, Hu XX, He SJ, Chen YF, Wei CJ, et al. The role of isolation rooms, facemasks and intensified hand hygiene in the prevention of nosocomial COVID-19 transmission in a pulmonary clinical setting. Infect Dis Poverty. 2020;9(1):104.
Hall CB, Douglas RG Jr. Nosocomial respiratory syncytial viral infections. Should gowns and masks be used? Am J Dis Child. 1981;135(6):512–5.
French CE, McKenzie BC, Coope C, Rajanaidu S, Paranthaman K, Pebody R, et al. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016;10(4):268–90.
Yin WW, Gao LD, Lin WS, Gao LD, Lin WS, Du L, et al. [Effectiveness of personal protective measures in prevention of nosocomial transmission of severe acute respiratory syndrome]. Zhonghua Liu **ng Bing Xue Za Zhi. 2004;25(1):18–22.
Seto WH, Tsang D, Yung RW, Ching TY, Ng TK, Ho M, et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). Lancet. 2003;361(9368):1519–20.
Ambrosch A, Luber D, Klawonn F, Kabesch M. A strict mask policy for hospital staff effectively prevents nosocomial influenza infections and mortality: monocentric data from five consecutive influenza seasons. J Hosp Infect. 2022;121:82–90.
Dorr T, Haller S, Muller MF, Friedl A, Vuichard D, Kahlert CR, et al. Risk of SARS-CoV-2 Acquisition in Health Care Workers According to Cumulative Patient Exposure and Preferred Mask Type. JAMA Netw Open. 2022;5(8):e2226816.
Pan Z, Zhang H, Yang J, Tang S, Cheng Z, Wu K, et al. Surgical Masks for Protection of Health Care Personnel Against Covid-19: Results from an Observational Study. Clin Invest Med. 2021;44(2):E48–54.
Lai X, Zhou Q, Zhang X, Tan L. What influences the infection of COVID-19 in healthcare workers? J Infect Dev Ctries. 2020;14(11):1231–7.
Ki HK, Han SK, Son JS, Park SO. Risk of transmission via medical employees and importance of routine infection-prevention policy in a nosocomial outbreak of Middle East respiratory syndrome (MERS): a descriptive analysis from a tertiary care hospital in South Korea. BMC Pulm Med. 2019;19(1):190.
MacIntyre CR, Chughtai AA, Rahman B, Peng Y, Zhang Y, Seale H, et al. The efficacy of medical masks and respirators against respiratory infection in healthcare workers. Influenza Other Respir Viruses. 2017;11(6):511–7.
Cronin CJ, Evans WN. Nursing home quality, COVID-19 deaths, and excess mortality. J Health Econ. 2022;82:102592.
Brody BD, Shi Z, Shaffer C, Eden D, Wyka K, Parish SJ, et al. Universal COVID-19 testing and a three-space triage protocol is associated with a nine-fold decrease in possible nosocomial infections in an inpatient psychiatric facility. Psychiatry Res. 2021;302:114036.
Klompas M, Baker MA, Griesbach D, Tucker R, Gallagher GR, Lang AS, et al. Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From Asymptomatic and Presymptomatic Individuals in Healthcare Settings Despite Medical Masks and Eye Protection. Clin Infect Dis. 2021;73(9):1693–5.
Rivett L, Sridhar S, Sparkes D, Routledge M, Jones NK, Forrest S et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020;9.
Acknowledgements
None.
Funding
The CH-SUR database is supported by the Federal Office of Public Health (333.0–20/1). T.D. received a grant from Swiss Academy of Medical Sciences (YTCR 12/22).
Author information
Authors and Affiliations
Contributions
SPK, PK, MS and DF conceptualized the study, planned the statistical analysis and were involved in interpreting the data and writing the manuscript together with TD. SG was responsible for statistical analysis of the data provided. MS, VGC, SMB and OK were involved in the data management and analysis at CH-SUR database. All authors critical reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
The CH-SUR project was submitted and approved by the Geneva Ethics Committee (CCER) and by all hospitals’ local Ethics Committee through the Swissethics Business Administration System for Ethics Committees (BASEC) submission system, under reference 2020 − 00827 (COVID-19) and 2018 − 00577 (Influenza).
Consent for publication
Not applicable.
Competing interests
P.W.S. received travel grants from Pfizer and Gilead, honoraria as a speaker and advisory board member from Pfizer, and honoraria from Gilead as an advisory board member outside of the submitted work. U.H. is a member of the Meta Data Safety Monitoring Board for CEPI (Coalition for Epidemic Preparedness Innovations). S. T.-S. and R. S. are active as Editors of Antimicrobial Resistance & Infection Control. The other authors report no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dörr, T., Güsewell, S., Flury, D. et al. Association of institutional masking policies with healthcare-associated SARS-CoV-2 infections in Swiss acute care hospitals during the BA.4/5 wave (CH-SUR study): a retrospective observational study. Antimicrob Resist Infect Control 13, 64 (2024). https://doi.org/10.1186/s13756-024-01422-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-024-01422-4