Abstract
Background
Current methods fail to accurately predict women at greatest risk of develo** fetal growth restriction (FGR) or related adverse outcomes, including stillbirth. Sexual dimorphism in these adverse pregnancy outcomes is well documented as are sex-specific differences in gene and protein expression in the placenta. Circulating maternal serum microRNAs (miRNAs) offer potential as biomarkers that may also be informative of underlying pathology. We hypothesised that FGR would be associated with an altered miRNA profile and would differ depending on fetal sex.
Methods
miRNA expression profiles were assessed in maternal serum (> 36 weeks’ gestation) from women delivering a severely FGR infant (defined as an individualised birthweight centile (IBC) < 3rd) and matched control participants (AGA; IBC = 20–80th), using miRNA arrays. qPCR was performed using specific miRNA primers in an expanded cohort of patients with IBC < 5th (n = 15 males, n = 16 females/group). Maternal serum human placental lactogen (hPL) was used as a proxy to determine if serum miRNAs were related to placental dysfunction. In silico analyses were performed to predict the potential functions of altered miRNAs.
Results
Initial analyses revealed 11 miRNAs were altered in maternal serum from FGR pregnancies. In silico analyses revealed all 11 altered miRNAs were located in a network of genes that regulate placental function. Subsequent analysis demonstrated four miRNAs showed sexually dimorphic patterns. miR-28-5p was reduced in FGR pregnancies (p < 0.01) only when there was a female offspring and miR-301a-3p was only reduced in FGR pregnancies with a male fetus (p < 0.05). miR-454-3p was decreased in FGR pregnancies (p < 0.05) regardless of fetal sex but was only positively correlated to hPL when the fetus was female. Conversely, miR-29c-3p was correlated to maternal hPL only when the fetus was male. Target genes for sexually dimorphic miRNAs reveal potential functional roles in the placenta including angiogenesis, placental growth, nutrient transport and apoptosis.
Conclusions
These studies have identified sexually dimorphic patterns for miRNAs in maternal serum in FGR. These miRNAs may have potential as non-invasive biomarkers for FGR and associated placental dysfunction. Further studies to determine if these miRNAs have potential functional roles in the placenta may provide greater understanding of the pathogenesis of placental dysfunction and the differing susceptibility of male and female fetuses to adverse in utero conditions.
Highlights
-
Detection and treatment of pregnancies at high risk of fetal growth restriction (FGR) and stillbirth remains a major obstetric challenge; circulating maternal serum microRNAs (miRNAs) offer potential as novel biomarkers.
-
Unbiased analysis of serum miRNAs in women in late pregnancy identified a specific profile of circulating miRNAs in women with a growth-restricted infant.
-
Some altered miRNAs (miR-28-5p, miR-301a-3p) showed sexually dimorphic expression in FGR pregnancies and others a fetal-sex dependent association to a hormonal marker of placental dysfunction (miR-454-3p, miR-29c-3p).
-
miR-301a-3p and miR-28-5p could potentially be used to predict FGR specifically in pregnancies with a male or female baby, respectively, however larger cohort studies are required.
-
Further investigations of these miRNAs and their relationship to placental dysfunction will lead to a better understanding of the pathophysiology of FGR and why there is differing susceptibility of male and female fetuses to FGR and stillbirth.
Similar content being viewed by others
Introduction
Fetal growth restriction (FGR) is a pregnancy complication where the fetus fails to reach its genetically determined growth potential and is a significant cause of fetal morbidity and mortality [1]. FGR is associated with a range of placental abnormalities, including impaired growth, villous and vascular structural abnormalities, and impaired nutrient transport and endocrine function [2, 3]. Fetal growth restriction and associated placental dysfunction are linked to increased rates of stillbirth, death of a fetus in utero after 24 weeks gestation [4]. Stillbirth affects 1 in 240 pregnancies in the UK [5], thus identifying pregnancies with placental dysfunction at greatest risk of FGR and stillbirth is an important clinical aim [2].
The only current direct test of placental function in utero in routine clinical use for detection of FGR is Doppler ultrasound assessment of umbilical artery blood flow [2] however, although this screen is sensitive for detecting early-onset FGR (< 34 weeks’ gestation), it is not reliable for late-onset FGR which comprises the majority of all FGR cases [6]. Whilst other tests in late pregnancy such as measurement of placental hormones in maternal blood, e.g. placental growth factor (PlGF), human placental lactogen (hPL) have also been proposed to identify placental dysfunction, a recent systematic review and meta-analysis demonstrated such tests are insufficient to predict FGR pregnancies thus additional biomarkers are required [7].
MicroRNAs are short (~ 20 nucleotide) RNA molecules that post-transcriptionally regulate gene expression by mediating mRNA destabilisation and translational repression [8]. miRNAs are produced in all cells and tissues, including the placenta, where they regulate growth, differentiation, survival and vascular development [9,10,11,12]. Vascular maldevelopment and altered trophoblast turnover and function are features of placental dysfunction observed in FGR and pregnancies ending in stillbirth [13] suggesting that the underlying pathology may be a consequence of altered miRNA levels in the placenta. miRNAs have also been shown to be released from tissues, including the placenta, into the circulation either in complexes with proteins such as Argonaute 2 or contained within extracellular vesicles (EVs) [14,15,16]. In the maternal circulation, specific alterations to miRNA signatures are associated with pregnancy pathologies such as pre-eclampsia (PE), gestational diabetes and pre-term labour [17,18,19,20]. Furthermore, in pregnant mice, plasma miRNAs have been proposed to offer a non-hormonal biomarker for direct indication of placental dysfunction [21], suggesting that circulating miRNAs may also offer promise as biomarkers to predict FGR and associated placental dysfunction in human pregnancy.
Indeed, changes in circulating miRNAs in pregnancies complicated by FGR have been reported [22,23,24,25], however, none of the miRNAs currently identified have sufficient diagnostic accuracy for use as biomarkers for FGR. This is likely due to key differences between study design, for example the analysis of a limited number of preselected candidate miRNAs rather than global profiling of miRNAs [22, 26]; differences in gestational ages of when serum was drawn between studies [24, 25]; analysing miRNA content in isolated EVs in some studies versus total serum in others [24]; and analysing obstetric populations with mixed FGR subtypes including women with PE and FGR [23]. To date, no published studies have stratified for fetal sex, a variable known to affect both rates of FGR, stillbirth and placental miRNA expression [27,28,29,30]. Therefore, we constructed our study to perform unbiased assessment of miRNAs, instead of selecting for specific candidate miRNAs; to profile total serum rather than EV enriched serum; to use a well-defined FGR population with no other known obstetric/medical complications; to stratify for fetal sex; to use in silico analyses to identify miRNAs involved in placental regulatory networks; and to combine analysis of miRNA expression profiles with levels of a known marker of placental dysfunction. We hypothesised that using this methodology, we would identify miRNA profiles that were associated with both FGR and placental dysfunction and that these miRNA profiles may be dependent on the presence of a male or female fetus.
Methods
Participants and clinical samples
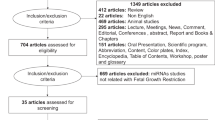
Study participants were pregnant women receiving antenatal care at St Mary’s Hospital, Manchester, recruited to the MFHRG Biobank (ethical approval: North West REC (08/H1010/55 + 5)). Written informed consent was obtained and detailed demographic and biophysical data were recorded. Exclusion criteria were multiple pregnancy, pre-term deliveries (< 36 weeks gestation), known fetal anomalies, pre-eclampsia or hypertension, maternal diabetes or any other co-existing obstetric/medical complications. Maternal serum samples were collected in the third trimester (27–42 weeks’ gestation). Briefly maternal venous blood drawn into serum gel tubes (Sarstedt, Numbrecht, Germany) was allowed to clot for 30 min and centrifuged at 3000 g for 10 min. Aliquots were immediately frozen at − 80 °C for analysis. After delivery, obstetric outcome data were collected and the individualised birthweight centile (IBC) calculated using Gestation Related Optimal Weight (GROW) Centile Calculator version 6.7 [31]. Babies were considered FGR when IBC < 5th centile. All FGR samples were matched on a 1:1 basis to appropriately grown (AGA; IBC ≥ 20 ≤ 80th centile) fetuses for the following maternal demographic and biophysical characteristics: infant sex (50:50 female to male), gestation at time of blood sampling, and gestation at delivery. Initial miRNA array profiling was performed on a subset of maternal serum samples drawn between 36–37 weeks’ gestation where primary selector was delivery of a baby with severe FGR (IBC < 3rd centile) (n = 4/group; Table 1). For all other analyses, a larger cohort of 62 participants’ samples (male n = 15, female n = 16; per group; Table 2), were included and FGR was defined as IBC < 5th centile. In both array samples and the larger cohort, only infant birthweight and IBC were significantly different by design between groups (array samples p < 0.05, larger cohort p < 0.0001, Mann–Whitney; Tables 1 and 2).
RNA isolation
Total RNA was extracted from 200 µl of maternal serum using the miRCURY RNA Isolation Kit—Biofluid (Exiqon, Denmark) following the manufacturers’ protocol, with inclusion of an on column DNAse digestion step. For increased reproducibility, a carrier RNA (1 µg MS2 phage RNA; Roche, UK)) was added prior to extraction along with RNA spike-in controls (UniSp2, UniSp4, UniSp5 Exiqon, cat no. 203203) to monitor the technical quality of the RNA isolation, cDNA synthesis and the presence of PCR inhibitors. Samples contaminated by haemolysis where ΔCt miR-23a-3p–miR-451a was > 7 were excluded. Standard methods of RNA yield/purity are inaccurate due to carrier RNA, however we adhered to best practise guidelines by standardising input amounts based on isolating from identical starting volumes and using the same volume of purified RNA for all downstream processes [32].
miRNA array profiling
Isolated maternal serum RNA (19 µl) was reverse transcribed in 95-µl reactions using the miRCURY LNA™ Universal RT microRNA PCR system (Exiqon, Denmark) then diluted 50 × before analysis using the miRCURY LNA™ Universal RT microRNA PCR Human panel I + II Array plates (Exiqon, Denmark) which detects 752 individual miRNAs (list of all miRNAs profiled contained in Additional file 1). Sample quality control was monitored using spike-ins for RNA isolation efficiency (UniSp2, UniSp4, UniSp5) and cDNA synthesis control (UniSp6). Individual miRNA Ct values in each sample, were normalised to the global mean of a panel of 194 miRNA Ct values detected in the same sample (the 194 miRNAs were detected in all samples) as recommended by Mestdagh et al. [33]. The stability of the average of the 194 microRNAs was higher across samples/groups than any single miRNA in the dataset as measured by NormFinder software [34]. The coefficient of variation (CoV) for the array was 0.00024–0.048%. Detection of statistical differences between patient groups was performed using a paired t-test followed by Benjamini and Hochberg multiple testing correction, using the software R/Bioconductor [35]. miRNAs with fold-change increase or decrease of more than 1.2-fold (≤ 0.83 ≥ 1.2) change p < 0.05 were considered significant.
Bioinformatic analysis of altered miRNAs
A list of all 11 miRNAs altered in maternal serum from FGR pregnancies was uploaded to Ingenuity Knowledge Base (Ingenuity Pathway Analysis (IPA), Qiagen, Redwood City, www.qiagen.com/ingenuity) and miRNET version 2.0 [
Sex-specific differences in miRNA expression between placentas of male and female fetuses may also contribute to the observed differences between published studies. We found sex differences in miR-526b, miR-454-3p and miR-29c-3p in maternal serum, independent of fetal growth. miR-454-3p and miR-29c-3p are also expressed in a sex-dependent manner in other tissues [39, 40, 54] so accounting for fetal sex when considering the contribution of these miRNAs to disease processes is of obvious importance.
Here, we also report that two miRNAs, miR-28-5p and miR-301a-3p are altered in FGR pregnancies only when there is a female or male baby, respectively. Whilst there are no reports of sex-differences in miR-28-5p during pregnancy, the reduction of miR-301a-3p only in FGR pregnancies with a male fetus, is consistent with previous reports of sexual dimorphic changes in miR-301a-3p in maternal serum in pre-eclampsia (PE) [43]. It is possible therefore, that miR-301a-3p and miR-28-5p could be used to predict FGR specifically in pregnancies with male or female babies. Caution should be taken however, since the heterogeneity of FGR pathophysiology means these miRNAs may only be useful in predicting FGR in the subpopulation of FGR cases in which they were originally identified, that is where the infant is < 3rd centile at birth. Prospective studies in a large independent cohort are required to assess this.
In addition to the potential biomarker utility of these miRNAs, in silico analyses reveal potential functional roles for the altered miRNAs. These miRNAs are enriched in functional networks associated with cellular response to stress, cell proliferation and vascular development. Since these are all hallmarks of placental dysfunction in FGR pregnancies [13, 81, 82], it is possible that they may contribute to the aetiology of FGR by impacting on placental function. Indeed placental sexual dimorphism is well documented [28, 30, 45, 83, 84] with male fetuses having increased susceptibility to adverse perinatal outcomes [64, 85, 86]. It would therefore be interesting to assess whether the sexually dimorphic profiles observed for serum miRNAs are also reflected in placental tissue, and whether the miRNAs have functional roles in the placenta. Indeed, the relationship between some of the altered miRNAs and hPL—a marker of placental dysfunction together with a functional study showing that overexpression of miR-454-3p in trophoblast increases proliferation and invasion whilst reducing apoptosis [55], would support this hypothesis. Roles for the altered miRNAs in other tissues combined with information on their validated targets also provides further support for roles of these miRNAs in regulation of placental function.
IGF-I, a critical regulator of normal human placental development [87, 88], is a validated gene target of miR-28-5p [89] and is strongly associated with FGR in both animal models [90] and human pregnancies [91]. In a study of healthy pregnancies, IGF-I concentrations in cord blood were found to be higher in women carrying a female infant [92]. Target genes of miR-29c-3p and miR-301a-3p in cell death and survival pathways [93,94,95] may be relevant to FGR as these are known to be altered in FGR pregnancies [77, 96, 97], however further studies are required to assess this.
Perspectives and significance
This manuscript contributes to an increasing understanding of miRNAs in the maternal circulation and how these may be used to predict differing susceptibility of male and female fetuses to FGR and stillbirth. These studies have identified sexually dimorphic miRNA profiles in maternal circulation in pregnancies, specifically those that result in FGR infants. Further studies to establish where these miRNAs originate and investigate potential roles for these miRNAs in the placenta may provide greater understanding of the pathogenesis of placental dysfunction. In addition, it is possible that sex-specific altered circulating miRNAs could contribute to the differences in frequency of pregnancy complications such as increased incidence of term pre-eclampsia and GDM and stillbirth in women carrying a male fetus [86, 98]. At present, fetal sex is not considered in the management of pregnancy conditions, thus the management of cases included here and the observation of increased frequency of complications will not have altered depending upon fetal sex.
Identifying novel predictive biomarkers that can be used in conjunction with existing techniques is important for better predicting late-onset FGR and stillbirth and reducing associated morbidity and mortality [99]. Existing algorithms to detect late-onset placental dysfunction (UAD impedance and PlGF/sFlt1 ratio in maternal serum) [100] may be strengthened by inclusion of one or more of these miRNAs or combining miRNAs with recently identified circulating mRNA markers such as EMP1, which is increased in women who subsequently suffered a stillbirth [101]. Further studies on an extended sample set are necessary to test this hypothesis. Including fetal sex in these algorithms (which would be necessary to interpret the miRNA data) may be challenging as fetal sex is not always accurately determined on ultrasound, parents may not wish to know the sex of their baby and in some states (e.g. India), antenatal determination of fetal sex is prohibited. Nevertheless, the clinical utility of combinations of biomarkers (including fetal sex) should be explored, and if deemed effective in reducing fetal mortality and morbidity, fetal sex could be included.
Conclusions
Our study has identified a distinct profile of circulating miRNAs in women with FGR infants < 3rd centile. Two of these miR-28-5p and miR-454-3p, were also altered in a larger population of pregnancies with infants < 5th centile. Further analyses identified sexually dimorphic changes in some of the altered miRNAs; both miR-28-5p and miR-301a-3p to be altered in maternal serum in FGR pregnancies according to infant sex and miR-29c-3p and miR-454-3p showed sexually dimorphic relationship to placental dysfunction. Furthermore, these altered miRNAs are linked to placental regulatory gene networks. Further investigations to determine the source of these miRNAs and their relationship to placental dysfunction will lead to a better understanding of the relationship between circulating miRNAs and placental dysfunction in FGR and may enable the development of future treatments for placental dysfunction. Ultimately, further studies are required to determine the potential for these altered miRNAs to provide potential biomarkers to predict differing susceptibility of male and female fetuses to FGR and stillbirth.