Abstract
Gadolinium-based contrast agents (GBCA) are essential for diagnostic MRI examinations. GBCA are only used in small quantities on a per-patient basis; however, the acquisition of contrast-enhanced MRI examinations worldwide results in the use of many thousands of litres of GBCA per year. Data shows that these GBCA are present in sewage water, surface water, and drinking water in many regions of the world. Therefore, there is growing concern regarding the environmental impact of GBCA because of their ubiquitous presence in the aquatic environment. To address the problem of GBCA in the water system as a whole, collaboration is necessary between all stakeholders, including the producers of GBCA, medical professionals and importantly, the consumers of drinking water, i.e. the patients. This paper aims to make healthcare professionals aware of the opportunity to take the lead in making informed decisions about the use of GBCA and provides an overview of the different options for action.
In this paper, we first provide a summary on the metabolism and clinical use of GBCA, then the environmental fate and observations of GBCA, followed by measures to reduce the use of GBCA. The environmental impact of GBCA can be reduced by (1) measures focusing on the application of GBCA by means of weight-based contrast volume reduction, GBCA with higher relaxivity per mmol of Gd, contrast-enhancing sequences, and post-processing; and (2) measures that reduce the waste of GBCA, including the use of bulk packaging and collecting residues of GBCA at the point of application.
Critical relevance statement This review aims to make healthcare professionals aware of the environmental impact of GBCA and the opportunity for them to take the lead in making informed decisions about GBCA use and the different options to reduce its environmental burden.
Key points
• Gadolinium-based contrast agents are found in sources of drinking water and constitute an environmental risk.
• Radiologists have a wide spectrum of options to reduce GBCA use without compromising diagnostic quality.
• Radiology can become more sustainable by adopting such measures in clinical practice.
Graphical Abstract

Similar content being viewed by others
Background
Magnetic resonance imaging (MRI) is used to help diagnose a wide range of conditions affecting the parenchymal organs, blood vessels, heart, brain, spinal cord, and bones. It can also check the health of organs such as the liver, kidneys, ovaries, breasts, and the prostate. GBCA are administrated in MRI to increase the contrast of these images. This allows radiologists to better detect inflammation, neoplasia, and functional abnormality.
Increasing use of GBCA for MRI is causing widespread contamination of fresh water and drinking water systems. GBCA can degrade, contrary to previous assumptions that they are stable throughout the water cycle. There is a need to carefully investigate the possible adverse health effects of currently marketed GBCA, and to modify the current approach to the use of GBCA in daily practice in order to minimise unknown potential health risks [1].
To tackle the problem of GBCA in the water system as a whole, it is necessary for all stakeholders, from the contrast agent manufacturer to the drinking water consumer, to work together. The first step towards active cooperation is to raise awareness among health professionals [2].
There are several things that radiologists can do to further this goal. We can be more aware of how we can optimise contrast agent use, reduce contrast agent waste, and collect contrast agent residues at the point of application. The aim of this paper is to review appropriate strategies to reduce contamination of our water supply by gadolinium-based contrast agents.
Methods
For this narrative review, the literature was analysed using PubMed and Embase databases from January 2010 until May 2023. Multiple repetitive searches with search criteria including synonyms of “contrast agents”, “gadolinium-based”, “water”, “environment”, and “contamination” were performed for all clinically approved gadolinium-based contrast agents, with languages limited to English, Dutch, and German. Results from cross-referencing were added where appropriate.
Gadolinium-based contrast agents
Gadolinium (Gd) is the metal located in the middle of the lanthanide series. The toxicity of Gd3+ in biological systems is largely due to its ability to mimic cations, particularly calcium ions (Ca2+), but also magnesium, zinc, and iron. These should not be overlooked, particularly because of the role of these ions as coenzymes in various biochemical processes [3]. Due to the toxic nature of Gd3+ ions, they are chelated with organic ligands to form GBCA that have either a linear or a macrocyclic structure. Contrast agents can therefore be classified according to the nature of the molecular structure of the ligand, either linear (i.e. open-chain molecule) or macrocyclic (i.e. cyclic ligand) and either ionic (i.e. dissociation into charged particles occurs in solution) or non-ionic [3]. The structure of GBCA determines their complex stability and in vivo stability.
GBCA excretion
The normal elimination of GBCA follows an open 3-compartment pharmacokinetic model. The first compartment is the plasma in which the molecules are diluted, the second compartment is the extravascular extracellular space of tissues where there is effective capillary permeability (i.e. outside the brain), and the third compartment is a storage compartment without capillary permeability. The exact location of this third compartment is not entirely clear, but GBCA are retained in the skin, liver, spleen, kidney, brain, and bone [4].
The decay of the GBCA concentration is the result of distribution of the contrast medium from plasma to the extracellular volume (distribution phase, slope α) with an average half-value of 0.2 ± 0.1 h, of the rapid excretion of GBCA from plasma to urine by renal excretion (elimination phase, slope β) with an average half-value of 1.6 ± 0.2 h, and of the slow excretion from the storage compartment to plasma and urine (residual excretion phase, slope γ). The half-value for this residual excretion phase is 5–8 × longer for linear GBCA (30–48 h) than for macrocyclic GBCA (5–6 h). The residual excretion rate is closely related to the thermodynamic stability of the specific GBCA. The relative contribution of this slow elimination is higher for linear than for macrocyclic GBCA [4].
The residence time of GBCA within the body depends also on the renal function of the patient. The half-life for the rapid renal excretion of GBCA ranges from 1.6 h for healthy individuals up to 30 h for patients with severely reduced renal function [5, 6]. In the storage compartment, the retention time of linear GBCA is long, with a risk of dechelation or transmetalation, which may lead to gadolinium deposition. Theoretically, the long residence time in the storage compartment could increase the risk of transmetalation even for macrocyclic GBCA, but to date, no clinical symptoms have been described.
GBCA retention and deposition
GBCA are considered to be safe and adverse effects are seldomly observed. However, in 2006, there was an association established between GBCA and nephrogenic systemic fibrosis (NSF) [7]. More recently, concerns have increased, when Gd deposits were reported in brains, bone, skin, and other tissues following GBCA administration, even in healthy patients.
In 2014, hyperintensity of the dentate nucleus (DN) and the globus pallidus (GP) relative to the pons on unenhanced T1-weighted images was attributed to repeated administrations of linear GBCA in patients with brain tumours [8], multiple sclerosis, or brain metastases [9]. No hyperintensity could be demonstrated for macrocyclic GBCA, even after large doses [10, 11]. Later studies confirmed that the use of linear extracellular GBCA led to visible changes in signal intensity (SI) ratios and measurable Gd depositions in animal and human brains [12,13,14,15], including in the anterior pituitary gland [16]. Most of the deposited Gd was found in perivascular foci in the DN and GP [12], with co-localisation to parenchymal iron [15]. The amount of deposition was not dependent on age or sex [14].
The European Medicines Agency (EMA) has therefore issued a warning and suspended the use in the EU of certain linear GBCA that are considered to have the highest risk of causing gadolinium enhancement of the brain [17].
Current use of gadolinium-based contrast agents
Gadopentetate dimeglumine (Magnevist), the first contrast agent developed specifically for MRI, became available for clinical use in 1988. Subsequently, several forms of GBCA from different manufacturers came onto the market.
The patents on most, if not all, of the current MRI contrast agents have expired and generics have entered the market. In the last few years, a number of generic copies of gadoterate meglumine (Dotarem®, Guerbet, Roissy CDG, France) have been registered by the regulatory authorities [18].
Gadolinium-based contrast administration is expected to continue its upward trend. This is due to the increased availability of MRI scanners and the growing number of indications for MRI examinations.
Since the introduction of GBCA in 1988, an estimated 750 million doses have been delivered, with an estimated use of 59 million doses per year in 2022. Overall, 30–45% of the MRI scans have used GBCA, largely depending on the anatomical area and specific imaging indication. There are high contributions by neuroradiology (ca. 40%) and cardiovascular radiology (ca. 20%) [19]. As a result, many thousands of litres — estimated at more than 590,000 L — of GBCA were used globally in 2022. This estimate is based on a total of approximately 59 million doses administered worldwide [19], and assuming that an average of 10 mL GBCA is used per MRI scan.
Manufacturers supply prefilled syringes, vials, and bottles in differing volumes, varying from 5 to 100 mL. According to manufacturers, there is a tendency to use more and more large packaging. In the Netherlands, we conducted a survey among the radiology departments of all hospitals, organised from the Radiological Society of The Netherlands. Of the 75 hospitals queried, 52 responded resulting in a response rate of 69%. We distinguished university hospitals, top clinical teaching hospitals, and general health organisations.
A question was raised about the ratio between the use of small packs (up to 20 mL) and larger packs (30 mL or more). More than 50% of university hospitals and top clinical teaching hospitals used bulk packs while 31% used exclusively small packs. Small packs, however, were dominant in general health organisations (58%) with bulk packs in only 23%.
Environmental fate of gadolinium-based contrast agents
Gd anomaly
Gadolinium belongs to the group of rare earth elements (REEs) or lanthanides, which are found in nature as a part of rocks and minerals. Weathering of these rocks and minerals mobilises REEs which can be present as dissolved species or associated with colloids. In general, gadolinium is not enriched in natural systems compared to its neighbouring REEs because of the similar physicochemical properties of these REEs [20].
The group of REEs or lanthanides contains 15 elements, (in order of their atomic mass) La, Ce, Pr, Nd, Pm, Sm, Eu, Gd, Tb, Dy, Ho, Er, Tm, Yb, and Lu.
The REE mobilisation process is influenced by pH, salinity, flow conditions, and bedrock lithology and will determine dissolved background REE and gadolinium content, which will differ between water systems [1]. However, their natural co-occurrence is rather constant which allows for the determination of anthropogenic gadolinium by applying a correction to the total amount of measured gadolinium based on the presence of all or some REEs.
Commonly used methods to calculate natural background gadolinium concentrations are extrapolation from either the heavier REE or the lighter REE, interpolation between a heavy and a light REE (for instance Sm and Tb), or a third order polynomial fit which is the preferred option [1].
A gadolinium anomaly greater than 1.5 is defined as significant [20, 21].
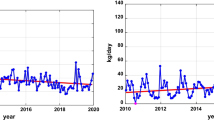
Positive Gd anomalies have been found in rivers worldwide, that flow through highly populated areas, including the Dutch Rhine-Meuse Delta which shows significant positive Gd anomalies. Besides this, positive Gd anomalies have been observed ubiquitously present in lakes, estuaries and coastal waters, groundwater and tap water [22]. This is caused by GBCA.
Targeted analysis
A large fraction of the REEs is removed during wastewater treatment which, results in a larger Gd anomaly in the effluent which is greater than in the influent [20]. For this reason, it is preferable to detect and quantify GBCA directly, rather than the gadolinium anomaly, to assess the impact of GBCA throughout the aquatic environment. Recent method developments using hyphenated hydrophilic interaction liquid chromatography (HILIC) and inductively coupled plasma-mass spectrometry (ICP-MS) have allowed for the extraction, separation, and detection of Dotarem (Gd-DOTA), Magnevist (Gd-DTPA), Gadovist (Gd-BT-DO3A), and Multihance (Gd-BOPTA) in various stages of drinking water production ranging from surface water to finished tap water. Reported limits of detection ranged between 8 and 14 pmol/Litre [23]. A further development has been the application of fully automated Ion Chromatography separation followed by ICP-MS which allows for high-throughput screening of surface water samples. The analysis of surface water samples was suitable for five complexes (Gd-HP-DO3A, Gd-BT-DO3A, Gd-DOTA, Gd- DTPA, and Gd-BOPTA) commonly administered in the EU [24].
Environmental observations of GBCA
GBCA have been reported in a wide variety of environmental matrices. This is partially due to their high dosage and partially due to their relative persistence and mobility.
Table 1 shows a (non-exhaustive) list of environmental observations of GBCA or anthropogenic gadolinium in various environmental aquatic compartments.
The most important route for GBCA into the aquatic environment is through the effluent of wastewater treatment plants (WWTPs) [20, 35]. A study published in 1986, prior to the widespread use of GBCA, showed no Gd anomaly in sewage sludge from Liverpool U.K. [20, 36]. Municipal WWTP influent from large, urban areas appear to contain less anthropogenic Gd on Sundays and Mondays, possibly since most MRI exams are conducted on weekdays [20, 37].
While GBCA are relatively non-toxic, free gadolinium ions are known to cause various pathological effects [38]. Any transformation process of GBCA that creates free gadolinium would therefore greatly increase its toxic effects.
Considering the high rate of excretion, within hours of application there is little change of biotransformation by the patient. However dwelling times, in sewage systems, in wastewater treatment plants and in the aquatic environment are much longer, increasing the likelihood of transformation through biotic and a-biotic processes. Transformation may occur under aerobic or anaerobic conditions during wastewater treatment. For instance during bank infiltration as a first drinking-water purification step. Additionally, advanced oxidation processes, such as the application of ozone, are increasingly employed during wastewater treatment or drinking water purification. The impact of these processes on the stability of GBCA is yet unknown.
Another pathway for the release of free gadolinium is transmetalation, in which the complexed Gd is replaced by another metal ion. In living organisms, Zn2+ may be able to replace Gd3+ because of its relative abundance. However, some drinking water suppliers rely on Fe3+ as a coagulant for the removal of suspended matter by increasing flocculation. Fe(III) has a strong tendency to hydrolyse and form various hydroxo-complexes [39] lowering the ambient pH of surface water by as much as 0,5 units. This may aid the transmetalation of GBCA.
Telgmann et al. [40] described the formation of 3 unknown Gd complexes during anaerobic sewage sludge treatment. Macke et al. [24] and Okabayashi et al. [41] have detected unknown and yet unidentified Gd complexes in surface water samples from the rivers Ems (Germany) and Muko (Japan). These complexes may be the result of transformation of GBCA or transmetalation leading to the formation of other unknown Gd-complexes.
As more becomes known about the presence of GBCA in the aquatic environment, interest in their potential effects has increased. However, few studies describe the environmental effects of GBCA which can be attributed to the relative difficulty of analysing GBCA in environmental samples. Perrat et al. [42] however, describe the accumulation of GBCA in freshwater bivalves (mussels), in gills and digestive glands, downstream of a wastewater treatment at the Mosel River (France). A review by Trapasso et al. [43] highlighted the scarcity of available data regarding the effects of Gd on aquatic organisms.
Measures to reduce GBCA
Various measures can be taken to reduce the use and the waste of GBCA, thereby reducing the amount of GBCA excreted into sewage water. Table 2 shows a list of opportunities to take measures to reduce GBCA. Below is an explanation of how to apply the measures.
Measures to reduce the use of gadolinium-based contrast agents
Preauthorisation of MRI requests
Preauthorisation of MRI requests by a radiologist provides assessment of the correct indication for the MRI examination and the correct application of contrast medium. Preauthorisation of MRI requests and the use of GBCA leads to a significant reduction in the use of this modality, with a reduction in imaging costs and a reduction in the use of GBCA [44].
Individualising the volume of intravenous GBCA in contrast-enhanced MRI
More conscious use of intravenous contrast is one way of tackling the problem at source. An increasing number of institutions have introduced individualised contrast volume, based on the clinical question and personalised to body weight.
Reducing the amount of contrast media for contrast-enhanced MRI
The contrast dose of GBCA can be reduced if (a) the relaxivity of the Gd-compound is higher than current standards, (b) the enhancement can be increased by scanning or postprocessing techniques, (c) if the diagnostic information from contrast-enhanced sequences can be obtained without GBCA, if (d) there is a non-Gd-based alternative contrast agent available, or (e) if the (amount of) enhancement is not critical for the clinical task at hand.
Higher-relaxivity GBCA
The level of enhancement using GBCA depends on R1 relaxivity values and R1/R2 ratios of the GBCA [45]. Current standard compounds have a R1 relaxivity of 4.2–4.6 L/mmol s [46]. GBCA with a relatively higher in vivo relaxivity are gadobutrol (R1 in blood at 1.5 T = 5.3 L/mmol s) and gadobenate (R1 in blood at 1.5 T = 6.7 L/mmol s) [47]. The novel agent gadopiclenol has an even higher relaxivity (R1 in serum or plasma at 1.5 T = 12.8 L/mmol s) [48].
Given a standard dose of 0.1 mmol/kg with current standard compounds, correcting for differences in relaxivity theoretically results in a gadobutrol dose of ca. 0.075 mmol/kg and a gadobenate dose of 0.066 mmol/kg as the relaxivity-corrected ‘standard dose’ for these compounds. Such a relaxivity-corrected ‘standard dose’ for gadopiclenol might be even lower than the currently approved dose of 0.05 mmol/kg. However, few studies have so far performed back-to-back comparisons with this concept.
The BENEFIT study showed no significant differences between 0.05 mmol/kg gadobenate and 0.1 mmol/kg gadoterate in brain tumours [46]. For the detection of malignancy, the LEADER-75 study showed equivalent sensitivity between 0.075 mmol/kg gadobutrol and 0.1 mmol/kg gadoterate, when imaged at 1.5 T or 3 T [49]. Another study using reduced-dose gadobenate has demonstrated non-inferiority for visual lesion delineation, internal morphology, and contrast enhancement at 1.5 T and 3.0 T [50]. There is better visualisation of small or ring-enhancing metastases on half-dose delayed CE-T2w FLAIR than on half dose CE-T1w MRI [51].
Higher-relaxivity GBCA in the heart allows for using lower doses, even for cardiac MRI with late gadolinium enhancement (LGE) of myocardial ischemic scars [52,53,54] or for post RF ablation scars [55].
In multiple vascular territories, such as in peripheral arteries [56] or supra-aortic arteries [57], MRA (magnetic resonance angiography) with half dose gadobenate performs well. Lower doses are also suitable for time-resolved MRA [58, 59].
Reduced doses of gadobenate are non-inferior for liver MRI [60,61,62] and for dynamic contrast-enhancement (DCE) in prostate MRI [63]. Similar results have been achieved in breast MRI at 3 T, with either half dose gadobenate [64] or gadobutrol [65]. Half dose higher-relaxivity GBCA was sufficient for adequate 3 T imaging of bone and soft tissues in adults and children [66, 67], and for imaging synovitis in rheumatoid arthritis [68].
Increased enhancement through optimised acquisition
The level of enhancement of GBCA not only depends on relaxivity but also on the type of sequence and the field strength [69]. Enhancement is substantially higher at 3 T than at 1.5 T and is generally higher for T1w 3D gradient echo than for T1w 2D fast spin echo sequences. However, optimal enhancement after GBCA for a specific anatomical region and clinical indication requires careful optimisation of MRI parameters for each individual sequence. Nevertheless, this poses a potential approach to tailor the amount of contrast to field strength and minimise the use of GBCA by optimum choice of MRI sequence parameters [70].
Imaging at higher field strength allows GBCA doses to be reduced for neuroimaging. At 3.0 T a 50% dose gadopentetate has shown to give a significantly higher contrast-to-noise ratio (1.3-fold higher) than full-dose imaging at 1.5 T [71].
Nowadays, higher field strengths are the norm in abdominal MRI. Gadobenate doses may even be lowered further to a quarter dose in liver imaging in patients at risk for NSF [72].
Increased enhancement through postprocessing
Postprocessing using artificial intelligence techniques can create ‘virtual’ or ‘augmented’ contrast images. Augmented contrast images boost existing contrast enhancement while virtual post-contrast images use the information available on other sequences of the scan to estimate contrast-enhancement [73]. The latter only succeeds if the information is redundant, already there on other sequences.
Deep learning (DL) methods for brain MRI are still in their infancy but may reduce GBCA dose up to tenfold [74]. However, if there is no detectable enhancement in small lesions, it is very doubtful if further improvements in DL-based algorithms can solve this issue. Changes in contrast medium injection protocols may be necessary [74, 75]. Further research into the (potential) loss of diagnostic information is warranted.
Deep learning models with virtual enhancement have been used to delineate myocardial infarction areas without LGE that need the use of contrast agents [76, 77]. It can also improve contrast in low Gd-dose MRA studies in patients with congenital heart disease [78].
Alternative sequences requiring no GBCA for clinical task
Omitting GBCA-enhanced sequences has been studied in the follow-up of extra-axial brain masses and multiple sclerosis (MS). A meta-analysis on vestibular schwannomas showed that non-CE MRI protocols with T2w imaging are very reliable for the diagnosis and monitoring of these tumours in comparison with CE-T1w imaging [79]. Meningioma dimensions measured on pre-contrast T2w were equivalent to results on CE-T1w imaging [80].
Considering the very low incidence rate of new enhancing lesions in patients with non-progressive MS at follow-up, routine administration of GBCA in follow-up MRI is of limited value and does not change the diagnosis interval of disease progression [81]. In the French OFSEP and the MAGNIMS-CMSC-NAIMS consensus recommendations, the CE-MRI is not needed for routine follow-up but is optional for relapse or when new treatment is started [82, 83].
New MRI sequences are constantly being developed. Some provide information that renders contrast-enhanced MRI unnecessary for specific indications. Amide proton transfer (APT) imaging, for example, is a chemical exchange saturation transfer (CEST) technique offering potential clinical applications for diagnosis, characterisation, and treatment planning and monitoring in glioma patients [84]. Multiple other specialised non-contrast MR Angiography techniques (e.g. QISS) allow good vascular imaging without the use of GBCA and have been reviewed elsewhere [85, 86]. MR Fingerprinting has enabled GBCA-free characterisation of myocardial tissue characterisation [87].
Non-contrast MRA with steady-state free precession (SSFP) techniques allow for good quality non-contrast imaging. International guidelines state that non-CE MRA and CE-MRA are both acceptable imaging studies to measure aortic dimensions in patients with thoracic aortic disease and adults with congenital heart disease [88]. Diagnostic image quality can be achieved without the need for GBCA [89]. Non-contrast MRA, in particular balanced SSFP, works well in the analysis of renal artery stenoses [90, 91].
Time-of-flight magnetic resonance angiography (TOF-MRA) is mainly used for imaging brain arteries and carotid arteries. Phase-contrast imaging is often used in cardiac valvular flow imaging, where the data are used to quantify the shunt fraction and to assess the severity of valvular disease [92]. Arterial spin labelling (ASL) or pseudo-continuous ASL (pCASL) are mainly used in the brain for vascular and perfusion analysis, and may even allow for the depiction of a specific vascular territory by selectively labelling.
ASL perfusion imaging has several applications in the body. Taso provided an overview highlighting the ongoing challenges and solutions to enable more widespread use of this technique in clinical practice [93].
Non-contrast imaging has simplified the routine prostate MRI protocol. The resulting bi-parametric protocols (T2w and diffusion-weighted imaging) have shown good results in the diagnosis of prostate cancer [94,95,96]. For liver metastasis detection, non-contrast MRI with DWI was diagnostically comparable to CE-MRI protocols [97]. Non-contrast MRI is routine for 3D T2w MRCP [98], but gadoxetate T1w-MRC has added benefits for bile duct anatomy in transplantation patients [99], or to diagnose bile duct leakage following surgery or trauma [100]. More evidence is needed for non-contrast renal, pancreatic, gastro-intestinal, and adnexal MRI.
Abbreviated MRI protocols (AMRI) are now employed for several indications, either non-contrast or with GBCA. For HCC screening, non-contrast AMRI has high sensitivity and specificity, superior to ultrasound [101]. AMRI has also been used in HCC surveillance, but hepatobiliary phase AMRI has slightly better sensitivity than non-contrast AMRI because of the higher lesion-to-liver contrast [87].
Non-contrast MRI is sufficient to diagnose osteomyelitis of the appendicular skeleton [102]. However, non-contrast MRI underestimated synovitis in patients with osteoarthritis [103], and in knee synovitis CE MRI scores correlated best with inflammatory infiltrates of synovial tissue [104]. In spine MRI, contrast-enhanced sequences are better in differentiating epidural fibrosis from disc herniation [105] and for characterisation of vertebral marrow infiltrative lesions [106]. The added value of GBCA is controversial for the diagnosis of spondylitis and its complications [107].
Alternative contrast agents
The class of ultra-small superparamagnetic iron oxide particles (USPIOs) may be an alternative to GBCA with a high safety profile. Their iron content results in a strong T1-relaxation effect, similar to that of GBCA. One such USPIO is ferumoxytol, which was developed as a drug for anaemia in dialysis patients, but retracted from the EU markets due to severe anaphylactoid reactions. Another USPIO particle is ferumoxtran-10 (Ferrotran, SPL B.V., Nijmegen, The Netherlands), which has a high lymphotropic effect. It has been extensively evaluated for the differentiation of normal from small metastatic lymph nodes in patients with solid tumours, including prostate, bladder and breast cancer. Due to its iron content and particle size, ferumoxtran-10 has a long intravascular half-life (days) and a good safety profile and could therefore be an excellent contrast agent for MRA, especially in cases where iodine or GBCA are contraindicated, such as patients with impaired renal function and renal transplantation [108].
Another SPIO MR-contrast agent, recently available in Europe again, is ferucarbotran (Resotran, b.e.imaging GmbH, Baden-Baden, Germany) intended for liver imaging and MR-Angiography. Due to the superparamagnetic properties of the iron oxide, the contrast medium predominantly shortens the T2 relaxation time and causes a distortion of the local magnetic field, both mechanisms having a pronounced signal loss in the vicinity of the iron oxide, particularly on the T2- and T2*-weighted pictures. The T2* effect is particularly pronounced after phagocytosis of Resotran® by cells of the reticuloendothelial system (RES) during the accumulation phase. As a result, SPIO-assisted MRI distinguishes between benign and malignant lesions based on their cellular composition and function (RES cells only in normal liver tissue and benign tumours). In addition, the high T1 relaxivity of Resotran® for dynamic imaging during the vascular phase and for vascular imaging using magnetic resonance imaging Angiography (MRA) can be used [109].
From a technical point of view, already iron-containing MR-contrast media can cover the most important MR-diagnostics fields. Ferucarbotran is registered in Europe (Germany) and ferumoxtran-10 is now tested in a phase III pivotal trial for lymph node detection in prostate cancer patients, the end of the study was expected in 2023.
To the best of our knowledge, the use of USPIO in patients does not pose any known risks to the environment. This is because the USPIO contrast media are metabolised in the patient’s body after intravenous administration, and iron is a physiological element that is used in non-toxic concentrations for MR imaging. The iron from the USPIO contrast media is metabolised in the body via the normal iron metabolic cycle, and there is no known excretion of USPIOs as particles after intravenous injection.
Manganese-based contrast agents have the potential to replace GBCA, but researchers have yet to address safety adequately [110].
Measures to reduce the waste of contrast media
Multi-patient injection system
The preferred method of administering the contrast agent in MRI scans is injection using a power injector. Multi-patient injection systems allow the use of vial/bottle sizes ranging from 10 to 100 mL. This allows the amount of contrast material injected to be individualised without increasing contrast material waste. The system works best by starting the day with a large bottle size (60, 65, or 100 mL) and then adjusting the bottle size at the end of the day to the expected total usage for the upcoming scan hours [111], considering the maximum usage time once the bottle stopper has been pierced. This time can vary up to 24 h, depending on the manufacturer.
A saline flush is applied. This is a secondary injection, also known as a saline chaser, following the administration of a contrast medium via a power injector.
The use of large packaging has the additional advantage of reducing overall packaging waste [112].
Manual administration is another method of administering the contrast agent. It is suitable in practices with a small number of patients for contrast-enhanced MRI (ceMRI) and do not have access to a multi-patient injection system.
Measures to collect residues of contrast media
Collection of residues of contrast media
Separate collection and disposal of contrast media waste through the hospital’s waste management system prevents contrast media from entering the sewerage system [2]. At our institution, each MRI suite has a special container to collect contrast media residues. These containers are disposed of through the hospital’s dedicated waste channels and destroyed in an incinerator. Previously, these residues were simply disposed of by pouring the contrast agent down the sink.
Gadolinium recycling services
Gadolinium recycling is a new practice. One contrast media manufacturer [113] offers a collection and recycling service for uncontaminated contrast media leftovers. Special containers are delivered to hospital radiology departments. They are collected by the manufacturer. The gadolinium is extracted from the substance and fed it into a further industrial use, a prolongation of product lifetime.
Measures to reduce the amount of contrast media in sewage water
Urine bags after contrast administration in outpatients
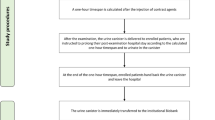
In The Netherlands [114] and in Germany [115] pilot studies were performed on outpatients after a contrast-enhanced CT scan. This method could also be used for outpatients after a contrast-enhanced MRI scan but no such studies of this are known to date. Disposable urine bags contain an absorbent material that holds the urine in place and can be sealed. Patients use the bags at home during the first four urination sessions after the administration of intravenous contrast media. The bags are disposed of via the household waste system.
Prolonged in-hospital time for outpatients
In Italy, the Greenwater study has started in which outpatients are asked to stay 1 h longer in hospital after a scheduled contrast-enhanced MRI examination and asked to urinate into a dedicated canister. The aim of the study is to assess the levels of GBCA in patients’ urine and to evaluate patient acceptance [116].
In The Netherlands, a study was conducted in which outpatients were asked to stay for at least 30 min longer in hospital after a scheduled ceCT examination. Patients received a urine bag for use during the first urination session. The excretion of iodinated contrast agent is roughly 20%, but varies in both terms of urine volume and the amount of contrast agent excreted [117]. Urine bags can also be applied by patients after ceMRI examinations.
Future directions
The healthcare sector is increasingly focused on sustainability. Efforts to reduce their environmental footprint and improve sustainability are being made by both hospitals and pharmaceutical companies. The expected scarcity of raw materials and the growing demand for contrast media present a problem that must be resolved.
Manufacturers are working on reducing water consumption, energy consumption, and eco-designed packaging as well as having programmes for optimising and recovering waste at industrial plants [118].
Manufacturers have recently developed a new generation of GBCA. These are so-called high-relaxivity macrocyclic contrast agents, whereby the doses to be used can be reduced by half or even more compared to products already available on the market for a longer time.
Bracco and Guerbet jointly developed gadopiclenol. These companies will collaborate on manufacturing and research and development for indications and will commercialise gadopiclenol, independently under separate brands upon regulatory approval. FDA and EMA approvals have been obtained. The brand names are respectively Vueway (Bracco Imaging) [119] and Elucirem (Guerbet) [120]. Both contrast agents are now used in patients at a number of hospitals in the USA.
Bayer launched gadoquatrane, a tetrameric macrocyclic contrast agent [121, 122]. This contrast agent is not yet available for routine patient care, further clinical development of the drug is underway. Bayer has initiated a phase III clinical development programme called Quanti, which aims to explore the effectiveness and safety of gadoquatrane [123].
The demand for raw materials in the world continues to grow as the wealth of citizens in emerging countries increases. This, together with developments within medical imaging techniques and modern treatment options, such as in oncology, contribute to an increasing global demand for contrast media. Currently, most of the gadolinium used in the production of contrast agents is sourced from Brazil, the USA, China, India, Sri Lanka, and Australia, making the industry vulnerable to production shortages and, ultimately, the limited (and easily exploitable) natural gadolinium resources. The expected scarcity of raw materials will force more companies to adopt sustainable resource management practices. In the long term it is desirable to be able to recycle contrast media from the urine of patients, and actually producing new GBCA out of the collected used material. This helps to save raw materials and contributes to a circular process.
Limitations
Sustainability within radiology is an evolving field and therefore limited public data is available. The measures listed to reduce the amount of gadolinium in our water environment all have their own limitations. However, taking all of these measures together may make a substantial contribution.
Conclusions
GBCA have been found in waste, surface, and drinking water in many parts of the world. In order to tackle the problem of GBCA in the water system as a whole, it is necessary for all stakeholders, from the producer of the contrast medium to the consumer of drinking water, to work together. If everyone in the chain plays their part, environmental exposure and subsequent downstream effects can be greatly mitigated. As healthcare professionals, we must take the lead in making informed decisions about the use of GBCA.
Availability of data and materials
Not applicable.
Abbreviations
- AMRI:
-
Abbreviated MRI
- ASL:
-
Arterial spin labelling
- DL:
-
Deep learning
- DN:
-
Dentate nucleus
- GBCA:
-
Gadolinium-based contrast agent/agents
- Gd:
-
Gadolinium
- GP:
-
Globus pallidus
- ICP-MS:
-
Inductively coupled plasma-mass spectrometry
- LGE:
-
Late gadolinium enhancement
- MS:
-
Multiple sclerosis
- NSF:
-
Nephrogenic systemic fibrosis
- REE:
-
Rare earth element/elements
- SSFP:
-
Steady-state free precession
- USPIO:
-
Ultra-small superparamagnetic iron oxide particle/particles
- WWTP:
-
Wastewater treatment plant/plants
References
Ebrahimi P, Barbieri M (2019) Gadolinium as an emerging microcontaminant in water resources: threats and opportunities. Geosciences 9:93. https://doi.org/10.3390/geosciences9020093
Dekker HM, Stroomberg GJ, Prokop M (2022) Tackling the increasing contamination of the water supply by iodinated contrast media. Insights Imaging. 13:30. https://doi.org/10.1186/s13244-022-01175-x
Lattanzio SM (2021) Toxicity associated with gadolinium-based contrast-enhanced contaminations. AIMS biophysics 8:198–220. https://doi.org/10.3934/biophy.2021015
Lancelot E (2016) Revisiting the pharmacokinetic profiles of gadolinium-based contrast agents: differences in long-term biodistribution and excretion. Invest Radiol. 51:691–700. https://doi.org/10.1097/RLI.0000000000000280
Van der Molen AJ, Geenen RW, Dekkers IA, et al (2022) Guideline safe use of contrast media, Part 3. Utrecht: Nederlandse Vereniging voor Radiologie. Available at: https://www.radiologen.nl/kwaliteit/richtlijnen-veilig-gebruik-van-contrastmiddelen-guidelines-safe-use-contrast-media. Accessed 19 Dec 2022
Schuhmann-Giampieri G, Krestin G (1991) Pharmacokinetics of Gd-DTPA in patients with chronic renal failure. Invest Radiol 26:975–979
Marckmann P, Skov L, Rossen K et al (2006) Nephrogenic systemic fibrosis: suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol. 17:2359–62. https://doi.org/10.1681/ASN.2006060601. (Epub 2006 Aug 2. PMID: 16885403)
Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841
Errante Y, Cirimele V, Mallio CA, Di Lazzaro V, Zobel BB, Quattrocchi CC (2014) Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Invest Radiol 49:685–690
Radbruch A, Weberling LD, Kieslich PJ et al (2015) High-signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted images: evaluation of the macrocyclic gadolinium-based contrast agent gadobutrol. Invest Radiol 50:805–810
Radbruch A, Haase R, Kieslich PJ et al (2017) No signal intensity increase in the dentate nucleus on unenhanced T1-weighted MR images after more than 20 serial injections of macrocyclic gadolinium-based contrast agents. Radiology 282:699–707
Davies J, Marino M, Smith APL et al (2021) Repeat and single dose administration of gadodiamide to rats to investigate concentration and location of gadolinium and the cell ultrastructure. Sci Rep 11:13950
El Hamrani D, Vives V, Buchholz R et al (2020) Effect of long-term retention of gadolinium on metabolism of deep cerebellar nuclei after repeated injections of gadodiamide in rats. Invest Radiol 55:120–128
Fretellier N, Granottier A, Rasschaert M et al (2019) Does age interfere with gadolinium toxicity and presence in brain and bone tissues: A comparative gadoterate versus gadodiamide study in juvenile and adult rats. Invest Radiol 54:61–71
Minaeva O, Hua N, Franz ES et al (2020) Nonhomogeneous gadolinium retention in the cerebral cortex after intravenous administration of gadolinium-based contrast agent in rats and humans. Radiology 294:377–385
Mallio CA, Messina L, Parillo M et al (2020) Anterior pituitary gland T1 signal intensity is influenced by time delay after injection of gadodiamide. Sci Rep 10:14967
EMA's final opinion confirms restrictions on use of linear gadolinium agents in body scans. Available at: https://www.ema.europa.eu/en/medicines/human/referrals/gadolinium-containing-contrast-agents. Accessed: 5 Dec 2023
Thomsen HS (2017) Generic gadolinium-based contrast agents: the future? Acta Radiol. 58:1285–1287. https://doi.org/10.1177/0284185117719576. (Epub 2017 Jul 10)
Bayer AG estimates, based on various internal and external data, 2023.
Verplanck PL, Furlong ET, Gray JL, Phillips PJ, Wolf RE, Esposito K (2010) Evaluating the Behavior of Gadolinium and Other Rare Earth Elements through Large Metropolitan Sewage Treatment Plants. Environ Sci Technol 44:3876–3882. https://doi.org/10.1021/es903888t
Rabiet M, Togola A, Brissaud F, Seidel JL, Elbaz-Poulichet BH, F, (2006) Consequences of treated water recycling as regards pharmaceuticals and drugs in surface and groundwaters of a medium-sized Mediterranean catchment. Environ Sci Technol 40:5282–5288
Klaver G, Verheul M, Bakker I, Petelet-Giraud E, Négrel P (2014) Anthropogenic Rare Earth Element in Rivers: Gadolinium and Lanthanum. Partitioning between the Dissolved and Particulate Phases in the Rhine River and Spatial Propagation through the Rhine-Meuse Delta (the Netherlands). Appl Geochem 47:186–197. https://doi.org/10.1016/j.apgeochem.2014.05.020
Birka M, Wehe CA, Hachmöller O, Sperling M, Karst U (2016) Tracing Gadolinium-Based Contrast Agents from Surface Water to Drinking Water by Means of Speciation Analysis. J Chromatogr A 1440:105–111. https://doi.org/10.1016/j.chroma.2016.02.050
Macke M, Derrick Quarles C, Sperling M, Karst U (2021) Fast and Automated Monitoring of Gadolinium-Based Contrast Agents in Surface Waters. Water Res 207:117836. https://doi.org/10.1016/j.watres.2021.117836
Kümmerer K, Helmers E (2000) Hospital Effluents as a Source of Gadolinium in the Aquatic Environment. Environ Sci Technol 34:573–577. https://doi.org/10.1021/es990633h
Kazumasa I, Fukushi M, Furukawa A et al (2020) Impact on Gadolinium Anomaly in River Waters in Tokyo Related to the Increased Number of MRI Devices in Use. Mar Pollut Bull 154:111148. https://doi.org/10.1016/j.marpolbul.2020.111148
Migaszewski ZM, Galuszka A (2016) The Use of Gadolinium and Europium Concentrations as Contaminant Tracers in the Nida River Watershed in South-Central Poland. Geological Quarterly 60:67–76. https://doi.org/10.7306/gq.1241
RIWA-Rijn 2022 de Jonge JA, Neefjes REM, Bannink AD, van Mourik IY, Stroomberg GJ (2022) Jaarrapport 2021 De Rijn. ISBN: 978–90–6683–186–5. RIWA- Rijn, Vereniging van Rivierwaterbedrijven
Hatje V, Bruland KW, Flegal AR (2016) Increases in Anthropogenic Gadolinium Anomalies and Rare Earth Element Concentrations in San Francisco Bay over a 20 Year Record. Environ Sci Technol 50:4159–4168. https://doi.org/10.1021/acs.est.5b04322
Johannesson KH, Palmore CD, Fackrell J et al (2017) Rare Earth Element Behavior during Groundwater-Seawater Mixing along the Kona Coast of Hawaii. Geochim Cosmochim Acta 198:229–258. https://doi.org/10.1016/j.gca.2016.11.009
Pereto C, Lerat-Hardy A, Baudrimont M, Coynel A (2023) European Fluxes of Medical Gadolinium to the Ocean: A Model Based on Healthcare Databases. Environ Int 173 (March). https://doi.org/10.1016/j.envint.2023.107868
Altomare AJ, Young NA, Beazley MJ (2020) A Preliminary Survey of Anthropogenic Gadolinium in Water and Sediment of a Constructed Wetland. J Environ Manage 255:109897
Schmidt K, Bau M, Merschel G, Tepe N (2019) Anthropogenic Gadolinium in Tap Water and in Tap Water-Based Beverages from Fast-Food Franchises in Six Major Cities in Germany. Sci Total Environ 687:1401–1408. https://doi.org/10.1016/j.scitotenv.2019.07.075
Wysocka IA, Rogowska AM, Paulina Kostrz-Sikora P (2023) “Investigation of Anthropogenic Gadolinium in Tap Water of Polish Cities: Gdańsk, Kraków, Warszawa, and Wrocław.” Environ Pollut 323. https://doi.org/10.1016/j.envpol.2023.121289
Kolpin DW, Furlong ET, Meyer MT et al (2002) Pharmaceuticals, hormones, and other organic wastewater contaminants in U.S. Streams, 1999–2000–A National Reconnaissance. Environ Sci Technol 36:1202–1211
Vivian CMG (1986) Rare earth element content of sewage sludges dumped at sea in Liverpool Bay, U.K. Environ Technol Lett 7:593–596
Möller P, Paces T, Dulski P, Morteani G (2002) Anthropogenic Gd in surface water, drainage system, and the water supply of the city of Prague, Czech Republic. Environ Sci Technol 36:2387–2394
Garcia J, Liu SZ, Louie AY (2017) Biological effects of MRI contrast agents: gadolinium retention, potential mechanisms and a role for phosphorus. Phil Trans R Soc A 375:20170180. https://doi.org/10.1098/rsta.2017.018
Stefánsson A (2007) Iron (III) Hydrolysis and Solubility at 25 Degrees C. Environ Sci Technol 41:6117–61123
Telgmann L, Wehe CA, Birka M et al (2012) Speciation and Isotope Dilution Analysis of Gadolinium-Based Contrast Agents in Wastewater. Environ Sci Technol 46(21):11929–11936. https://doi.org/10.1021/es301981z
Okabayashi S, Kawane L, Yusentri Mrabawani N et al (2021) Speciation Analysis of Gadolinium-Based Contrast Agents Using Aqueous Eluent-Hydrophilic Interaction Liquid Chromatography Hyphenated with Inductively Coupled Plasma-Mass Spectrometry. Talanta Volume 222: 121531. ISSN 0039–9140, https://doi.org/10.1016/j.talanta.2020.121531
Perrat E, Parant M, Py JS, Rosin C, Cossu-Leguille C (2017) Bioaccumulation of Gadolinium in Freshwater Bivalves. Environ Sci Pollut Res 24:12405–12415. https://doi.org/10.1007/s11356-017-8869-9
Trapasso G, Chiesa S, Freitas R, Pereira E (2021) What Do We Know about the Ecotoxicological Implications of the Rare Earth Element Gadolinium in Aquatic Ecosystems? Sci Total Environ 781:146273. https://doi.org/10.1016/j.scitotenv.2021.146273
Blachar A, Tal S, Mandel A et al (2006) Preauthorisation of CT and MRI examinations: assessment of a managed care Preauthorisation program based on the ACR Appropriateness Criteria and the Royal College of Radiology guidelines. J Am Coll Radiol. 3:851–9
Weinmann HJ, Bauer H, Ebert W et al (2002) Comparative studies on the efficacy of MRI contrast agents in MRA. Acad Radiol. 9:S135–6
Vaneckova M, Herman M, Smith MP et al (2015) The Benefits of High Relaxivity for Brain Tumor Imaging: Results of a Multicenter Intraindividual Crossover Comparison of Gadobenate Dimeglumine with Gadoterate Meglumine (The BENEFIT Study). AJNR Am J Neuroradiol. 36:1589–98
Rohrer M, Bauer H, Mintorovitch J, Requard M, Weinmann HJ (2005) Comparison of magnetic properties of MRI contrast media solutions at different field strengths. Invest Radiol 40:715–724
Loevner LA, Kolumban B, Hutóczki G et al (2023) Efficacy and Safety of Gadopiclenol for Contrast-Enhanced MRI of the Central Nervous System: The PICTURE Randomized Clinical Trial. Invest Radiol. 58:307–313. https://doi.org/10.1097/RLI.0000000000000944. (PMID: 36729404; PMCID: PMC10090311)
Liu BP, Rosenberg M, Saverio P et al (2021) Clinical efficacy of reduced-dose gadobutrol versus standard-dose gadoterate for contrast-enhanced MRI of the CNS: An international multicenter prospective crossover trial (LEADER-75). AJR Am J Roentgenol 217:1195–1205
DeLano MC, Spampinato MV, Chang EY et al (2021) Dose-Lowering in Contrast-Enhanced MRI of the Central Nervous System: A Retrospective, Parallel-Group Comparison Using Gadobenate Dimeglumine. Magn Reson Imaging. 54:1660–1675
** T, Ge M, Huang R et al (2021) Utility of contrast-enhanced T2 FLAIR for Imaging brain metastases using a half-dose high-relaxivity contrast agent. AJNR Am J Neuroradiol 42:457–463
Cheong BY, Duran C, Preventza OA, Muthupillai R (2015) Comparison of low-dose higher-relaxivity and standard-dose lower-relaxivity contrast media for delayed-enhancement MRI: A blinded randomized crossover study. AJR Am J Roentgenol 205:533–539
Rudolph A, Messroghli D, von Knobelsdorff-Brenkenhoff F et al (2015) Prospective, randomized comparison of gadopentetate and gadobutrol to assess chronic myocardial infarction applying cardiovascular magnetic resonance. BMC Med Imaging. 15:55
D’Angelo T, Grigoratos C, Mazziotti S et al (2017) High-throughput gadobutrol-enhanced CMR: a time and dose optimisation study. J Cardiovasc Magn Reson. 19:83
Chubb H, Karim R, Roujol S et al (2018) The reproducibility of late gadolinium enhancement cardiovascular magnetic resonance imaging of post-ablation atrial scar: a cross-over study. J Cardiovasc Magn Reson. 20:21
Achenbach M, Figiel JH, Burbelko M, Heverhagen JT (2010) Prospective comparison of image quality and diagnostic accuracy of 0.5 molar gadobenate dimeglumine and 1.0 molar gadobutrol in contrast-enhanced run-off magnetic resonance angiography of the lower extremities. J Magn Reson Imaging. 32:1166–71
Dehkharghani S, Qiu D, Albin LS, Saindane AM (2015) Dose reduction in contrast-enhanced cervical MR angiography: field strength dependency of vascular signal intensity, contrast administration, and arteriographic quality. AJR Am J Roentgenol 204:W701–W706
Lee YJ, Kim BS, Koo JS et al (2015) Supra-aortic low-dose contrast- enhanced time-resolved magnetic resonance (MR) angiography at 3 T: comparison with time-of-flight MR angiography and high-resolution contrast-enhanced MR angiography. Acta Radiol 56:673–680
Raczeck P, Fries P, Massmann A et al (2021) Diagnostic Performance of a Lower-dose Contrast-Enhanced 4D Dynamic MR Angiography of the Lower Extremities at 3 T Using Multisegmental Time-Resolved Maximum Intensity Projections. J Magn Reson Imaging. 54:763–774
Homayoon B, Diwakar H, Strovski E et al (2014) Half-dose gadobenate dimeglumine versus standard-dose gadodiamide in dynamic magnetic resonance imaging of non-cirrhotic livers: a retrospective intra-individual crossover comparison. Abdom Imaging. 39:955–962
Schneider G, Maas R, Kool LS et al (2003) Low-dose gadobenate dimeglumine versus standard dose gadopentetate dimeglumine for contrast-enhanced magnetic resonance imaging of the liver: an intra-individual crossover comparison. Invest Radiol 38:85–94
Kamali M, Clarke SE, Costa AF (2020) Evaluation of liver MRI examinations with two dosages of gadobenate dimeglumine: a blinded intra-individual study. Abdom Radiol (NY) 45:36–44
He D, Chatterjee A, Fan X et al (2018) Feasibility of dynamic contrast- enhanced magnetic resonance imaging using low-dose gadolinium: comparative performance with standard dose in prostate cancer diagnosis. Invest Radiol 53:609–615
Clauser P, Helbich TH, Kapetas P et al (2019) Breast lesion detection and characterization with contrast-enhanced magnetic resonance imaging: Prospective randomized intraindividual comparison of gadoterate meglumine (0.15 mmol/kg) and gadobenate dimeglumine (0.075 mmol/kg) at 3T. J Magn Reson Imaging. 49:1157–1165
Melsaether AN, Kim E, Mema E, Babb JS, Kim SG (2019) Preliminary study: Breast cancers can be well seen on 3T breast MRI with a half-dose of gadobutrol. Clin Imaging 58:84–89
Costelloe CM, Murphy WA, Haygood TM et al (2011) Comparison of half-dose and full-dose gadolinium MR contrast on the enhancement of bone and soft tissue tumors. Skeletal Radiol 40:327–333
Colafati GS, Rossi E, Carducci C et al (2018) Half-dose versus full-dose macrocyclic gadolinium at 3-T magnetic resonance imaging in paediatric bone and soft-tissue disease. Pediatr Radiol 48:1724–1735
Weide Kamm C, Lodemann KP, Grisar J et al (2013) Contrast-enhanced MR imaging of hand and finger joints in patients with early rheumatoid arthritis: Do we really need a full dose of gadobenate dimeglumine for assessing synovial enhancement at 3T? Radiology 268:161–169
Elster AD. T1 shortening by Gad. Available at: http://mriquestions.com/why-does-gd-shorten-t1.html. Accessed 5 Feb 2024
Bapst B, Amegnizin JL, Vignaud A et al (2020) Post-contrast 3D T1-weighted TSE MR sequences (SPACE, CUBE, VISTA/BRAINVIEW, isoFSE, 3D MVOX): Technical aspects and clinical applications. J Neuroradiol. 47:358–368. https://doi.org/10.1016/j.neurad.2020.01.085. (Epub 2020 Feb 1 PMID: 32017974)
Krautmacher C, Willinek WA, Tschampa HJ et al (2005) Brain tumors: Full- and half-dose contrast-enhanced MR imaging at 3.0 T compared with 1.5 T - Initial experience. Radiology. 237:1014–1019
De Campos ROP, Heredia V, Ramalho M et al (2011) Quarter-dose (0.025 mmol/kg) gadobenate dimeglumine for abdominal MRI in patients at risk for nephrogenic systemic fibrosis: Preliminary observations. AJR Am J Roentgenol. 196:545–552
Pasquini L, Napolitano A, Pignatelli M et al (2022) Synthetic Post-Contrast Imaging through Artificial Intelligence: Clinical Applications of Virtual and Augmented Contrast Media. Pharmaceutics. 14:2378. https://doi.org/10.3390/pharmaceutics14112378
Luo H, Zhang T, Gong NJ et al (2021) Deep learning-based methods may minimize GBCA dosage in brain MRI. Eur Radiol 231:6419–6428
Ammari S, Bône A, Balleyguier C et al (2022) Can deep learning replace gadolinium in neuro-oncology: A reader study. Invest Radiol 57:99–107
Zhang N, Yang G, Gao Z et al (2019) Deep Learning for Diagnosis of Chronic Myocardial Infarction on Nonenhanced Cardiac Cine MRI. Radiology. 291:606–617
Zhang Q, Burrage MK, Lukaschuk E et al (2021) Toward Replacing Late Gadolinium Enhancement With Artificial Intelligence Virtual Native Enhancement for Gadolinium-Free Cardiovascular Magnetic Resonance Tissue Characterization in Hypertrophic Cardiomyopathy. Circulation. 144:589–599
Montalt-Tordera J, Quail M, Steeden JA, Muthurangu V (2021) Reducing contrast agent dose in cardiovascular MR Angiography with deep learning. J Magn Reson Imaging 54:795–805
Kim DH, Lee S, Hwang SH (2019) Non-contrast magnetic resonance imaging for diagnosis and monitoring of vestibular schwannomas: A systematic review and meta-analysis. Otol Neurotol 40:1126–1133
Rahatli FK, Donmez FY, Kesim C, Haberal KM, Turnaoglu H, Agildere AM (2019) Can unenhanced brain magnetic resonance imaging be used in routine follow up of meningiomas to avoid gadolinium deposition in brain? Clin Imaging 53:155–161
Eichinger P, Schön S, Pongratz V et al (2019) Accuracy of unenhanced MRI in the detection of new brain lesions in multiple sclerosis. Radiology 291:429–435
Brisset JC, Kremer S, Hannoun S et al (2020) New OFSEP recommendations for MRI assessment of multiple sclerosis patients: Special consideration for gadolinium deposition and frequent acquisitions. J Neuroradiol. 47:250–258
Wattjes MP, Ciccarelli O, Reich DS et al (2021) 2021 MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. 20:653–670
Wamelink IJHG, Kuijer JPA, Padrela BE et al (2023) Reproducibility of 3 T APT-CEST in Healthy Volunteers and Patients With Brain Glioma. J Magn Reson Imaging. 57:206–215
Cavallo AU, Koktzoglou I, Edelman RR et al (2019) Noncontrast Magnetic Resonance Angiography for the Diagnosis of Peripheral Vascular Disease. Circ Cardiovasc Imaging. 12:e008844
Edelman RR, Koktzoglou I (2019) Noncontrast MR angiography: An update. J Magn Reson Imaging. 49:355–373
Velasco C, Cruz G, Lavin B et al (2022) Simultaneous T1, T2, and T1ρ cardiac magnetic resonance fingerprinting for contrast agent-free myocardial tissue characterization. Magn Reson Med. 87:1992–2002
Hiratzka LF, Creager MA, Isselbacher EM et al (2016) Surgery for aortic dilatation in patients with bicuspid aortic valves: A Statement of Clarification from the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 133:680–686
Pennig L, Wagner A, Weiss K et al (2021) Comparison of a novel Compressed SENSE accelerated 3D modified relaxation-enhanced angiography without contrast and triggering with CE-MRA in imaging of the thoracic aorta. Int J Cardiovasc Imaging 37:315–329
Lal H, Singh RKR, Yadav P, Yadav A, Bhadauria D, Singh A (2021) Non-contrast MR angiography versus contrast enhanced MR angiography for detection of renal artery stenosis: a comparative analysis in 400 renal arteries. Abdom Radiol (NY) 46:2064–2071
Maki JH, Wilson GJ, Eubank WB, Glickerman DJ, Pipavath S, Hoogeveen RM (2007) Steady-state free precession MRA of the renal arteries: breath-hold and navigator-gated techniques vs. CE-MRA. J Magn Reson Imaging 26:966–973
Wymer DT, Patel KP, Burke WF 3rd, Bhatia VK (2020) Phase-Contrast MRI: Physics, Techniques, and Clinical Applications. Radiographics 40:122–140. https://doi.org/10.1148/rg.2020190039. (PMID: 31917664)
Taso M, Aramendía-Vidaurreta V, Englund EK et al (2023) Update on state-of-the-art for arterial spin labeling (ASL) human perfusion imaging outside of the brain. Magn Reson Med. 89:1754–1776. https://doi.org/10.1002/mrm.29609. (Epub 2023 Feb 6 PMID: 36747380)
Park KJ, Choi SH, Kim MH, Kim JK, Jeong IG (2021) Performance of Prostate Imaging Reporting and Data System version 2.1 for diagnosis of prostate cancer: A systematic review and meta-analysis. J Magn Reson Imaging 54:103–112
Pecoraro M, Messina E, Bicchetti M et al (2021) The future direction of imaging in prostate cancer: MRI with or without contrast injection. Andrology 9:1429–1443
Tamada T, Kido A, Yamamoto A et al (2021) Comparison of biparametric and multiparametric MRI for clinically significant prostate cancer detection with PI-RADS version 2.1. J Magn Reson Imaging 53:283–291
Hwang JA, Kim YK, Min JH, Song KD, Sohn I, Ahn HS (2019) Non-contrast liver MRI as an alternative to gadoxetic acid-enhanced MRI for liver metastasis from colorectal cancer. Acta Radiol 60:441–450
Kang SK, Heacock L, Doshi AM, Ream JR, Sun J, Babb JS (2017) Comparative performance of non- contrast MRI with HASTE vs. contrast-enhanced MRI/3D-MRCP for possible choledocholithiasis in hospitalized patients. Abdom Radiol (NY) 42:1650–1658
Choi SH, Kim KW, Kwon HJ et al (2019) Clinical usefulness of gadoxetic acid-enhanced MRI for evaluating biliary anatomy in living donor liver transplantation. Eur Radiol. 29:6508–6518
Boraschi P, Donati F, Pacciardi F et al (2019) Gadoxetate Disodium-Enhanced MR Cholangiography for Evaluation of Biliary-Enteric Anastomoses: Added Value Beyond Conventional T2-Weighted Images. AJR Am J Roentgenol. 213:W123–W133
Gupta P, Soundararajan R, Patel A, Kumar-M P, Sharma V, Kalra N (2021) Abbreviated MRI for hepatocellular carcinoma screening: A systematic review and meta-analysis. J Hepatol. 75:108–119
Labiste CC, McElroy E, Subhawong TK, Banks JS (2022) Systematic review: investigating the added diagnostic value of gadolinium contrast agents for osteomyelitis in the appendicular skeleton. Skeletal Radiol. 51:1285–1296
De Vries BA, Breda SJ, Sveinsson B et al (2021) Detection of knee synovitis using non-contrast-enhanced qDESS compared with contrast-enhanced MRI. Arthritis Res Ther 23:55
Shakoor D, Demehri S, Roemer FW, Loeuille D, Felson DT, Guermazi A (2020) Are contrast- enhanced and non-contrast MRI findings reflecting synovial inflammation in knee osteoarthritis: A meta-analysis of observational studies. Osteoarthritis Cartilage 28:126–136
Passavanti Z, Leschka S, Wildermuth S, Forster T, Dietrich TJ (2020) Differentiating epidural fibrosis from disc herniation on contrast-enhanced and unenhanced MRI in the postoperative lumbar spine. Skeletal Radiol 49:1819–1827
Zidan DZ, Elghazaly HA (2014) Can unenhanced multiparametric MRI substitute gadolinium- enhanced MRI in the characterization of vertebral marrow infiltrative lesions? Egypt J Radiol Nucl Med 45:443–453
Prasetyo M, Sirath AS, Wicaksono KP, Prihartono J, Setiawan SI (2020) Non-contrast versus contrast-enhanced MR in the diagnosis of spondylitis: A quantitative concordance- analysis. Eur J Radiol Open 7:100306
Zamecnik P, Israel B, Feuerstein J et al (2022) Ferumoxtran-10-enhanced 3-T Magnetic Resonance Angiography of Pelvic Arteries: Initial Experience. Eur Urol Focus. 8:1802–1808. https://doi.org/10.1016/j.euf.2022.03.001. (Epub 2022 Mar 23 PMID: 35337778)
Resotran_Produktmonographie_E_210x148_122022_ES.pdf, december 2022. www.bendergruppe.com
Davis KA, Lazar B (2021) Manganese-Based Contrast Agents as a Replacement for Gadolinium. Radiol Technol. 93:36–45
Struik F, Futterer JJ, Prokop WM (2020) Performance of single-use syringe versus multi-use MR contrast injectors: a prospective comparative study. Sci Rep. 10:3946. https://doi.org/10.1038/s41598-020-60697-w
Lindsey JS, Frederick-Dyer K, Carr JJ, Cooke E, Allen LM, Omary RA (2023) Modeling the Environmental and Financial Impact of Multi-dose vs. Single-dose Iodinated Contrast Media Packaging and Delivery Systems. Acad Radiol. 30:1017–1023. https://doi.org/10.1016/j.acra.2022.12.029. (Epub 2023 Jan 6 PMID: 36621442)
re:contrast | Bayer Radiology www.radiology.bayer.com
Hoogenboom J, Bergema K, van Vliet BJM, Hendriksen A (2021) Eindrapportage Brede Plaszakkenproef
Röntgenkrontrastmittel in der Ruhr: Pilotproject. www.merkmal-ruhr.de
Zanardo M, Cozzi A, Cardani R et al (2023) Reducing contrast agent residuals in hospital wastewater: the GREENWATER study protocol. Eur Radiol Exp. 7:27. https://doi.org/10.1186/s41747-023-00337-w. (PMID: 37142839; PMCID: PMC10160294)
Dekker HM, Oostveen L, Woude van der WJ, Prokop M (2022) How can we reduce the amount of excreted iodine in waste water by collecting the first urine after CT. ESUR 2022
Bracco (2021) Sustainability Report 2020
Bracco’s VUEWAY™ (gadopiclenol) injection now in hospitals | Bracco
Guerbet - Guerbet announces U.S. Food and Drug Administration (FDA) approval of Elucirem™ (Gadopiclenol)
Lohrke J, Berger M, Frenzel T et al (2022) Preclinical profile of gadoquatrane: a novel tetrameric, macrocyclic high relaxivity gadolinium-based contrast agent. Invest Radiol. 57:629–638. https://doi.org/10.1097/RLI.0000000000000889. (Epub 2022 Jun 13. PMID: 35703267; PMCID: PMC9444293)
Hoffmann B (2022) R5A-SPNR-11 - Pharmacokinetics, safety and tolerability of the novel tetrameric, high relaxivity, macrocyclic gadolinium-based contrast agent gadoquatrane for CE-MRI (abstract RSNA 2022)
Bayer begins Phase III assessment of MRI contrast agent | AuntMinnieEurope
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HD, GS, AvdM, and MP conceived the idea and structure of this review. HD, GS, AvdM, and MP drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
G.S. works for the Association of River Water Works. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dekker, H.M., Stroomberg, G.J., Van der Molen, A.J. et al. Review of strategies to reduce the contamination of the water environment by gadolinium-based contrast agents. Insights Imaging 15, 62 (2024). https://doi.org/10.1186/s13244-024-01626-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-024-01626-7