Abstract
Background
Alzheimer’s disease (AD) is caused by many intertwining pathologies involving metabolic aberrations. Patients with metabolic syndrome (MetS) generally show hyperglycemia and dyslipidemia, which can lead to the formation of aldehydic adducts such as acrolein on peptides in the brain and blood. However, the pathogenesis from MetS to AD remains elusive.
Methods
An AD cell model expressing Swedish and Indiana amyloid precursor protein (APP-Swe/Ind) in neuro-2a cells and a 3xTg-AD mouse model were used. Human serum samples (142 control and 117 AD) and related clinical data were collected. Due to the involvement of MetS in AD, human samples were grouped into healthy control (HC), MetS-like, AD with normal metabolism (AD-N), and AD with metabolic disturbance (AD-M). APP, amyloid-beta (Aß), and acrolein adducts in the samples were analyzed using immunofluorescent microscopy, histochemistry, immunoprecipitation, immunoblotting, and/or ELISA. Synthetic Aß1-16 and Aß17-28 peptides were modified with acrolein in vitro and verified using LC–MS/MS. Native and acrolein-modified Aß peptides were used to measure the levels of specific autoantibodies IgG and IgM in the serum. The correlations and diagnostic power of potential biomarkers were evaluated.
Results
An increased level of acrolein adducts was detected in the AD model cells. Furthermore, acrolein adducts were observed on APP C-terminal fragments (APP-CTFs) containing Aß in 3xTg-AD mouse serum, brain lysates, and human serum. The level of acrolein adducts was correlated positively with fasting glucose and triglycerides and negatively with high-density lipoprotein-cholesterol, which correspond with MetS conditions. Among the four groups of human samples, the level of acrolein adducts was largely increased only in AD-M compared to all other groups. Notably, anti-acrolein-Aß autoantibodies, especially IgM, were largely reduced in AD-M compared to the MetS group, suggesting that the specific antibodies against acrolein adducts may be depleted during pathogenesis from MetS to AD.
Conclusions
Metabolic disturbance may induce acrolein adduction, however, neutralized by responding autoantibodies. AD may be developed from MetS when these autoantibodies are depleted. Acrolein adducts and the responding autoantibodies may be potential biomarkers for not only diagnosis but also immunotherapy of AD, especially in complication with MetS.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is the most widespread dementia and afflicts aging populations worldwide. The cause of AD is the result of many intertwining pathologies. However, progressive neuronal loss found in AD is theorized to result from the accumulation of extracellular amyloid plaques comprised of amyloid-ß (Aß) which is generated through proteolytic cleavage of amyloid precursor protein (APP) by ß- and γ-secretases [1]. More and more investigations suggest that AD is strongly correlated with metabolic syndrome (MetS) involving oxidative stress and post-translational modification (PTM) [2,3,4]. MetS is a group of five conditions, namely obesity, hypertension, hyperglycemia, hypertriglyceridemia, and reduced high-density lipoprotein-cholesterol (HDL-C) in the blood. Imbalanced blood levels of glucose and lipids enhance lipid peroxidation, producing acrolein, 4-hydroxynonenal (HNE), and other aldehydic adducts in AD brain, cerebrospinal fluid (CSF), and blood. Nationwide surveys from Taiwan and Korea also supported that metabolic aberration could be a good indicator to diagnose the development of dementia specifically AD [5, 6]. However, the detailed mechanism of pathogenesis from MetS to AD remains elusive.
Studies suggest that increased lipid peroxidation in membranes causes increased levels of acrolein and HNE in the amygdala, hippocampus/parahippocampal gyrus, and inferior parietal lobule [1A, right panel). The bands looked blurry possibly due to long exposure in image development. It suggests that the AD cells may undergo metabolic disturbance with increased acrolein adducts probably formed on Aß peptides.
Acrolein adducts in the transfected cells and model mouse tissues. A Immunoblotting of the cell lysates. The transfected neuro-2a cells were analyzed with SDS-PAGE in triplicate. One gel was stained with CBB as a loading control. The other two gels were immunoblotted with anti-C-terminal APP and acrolein antibodies, respectively. The full-length APP (APP-FL) and APP C-terminal fragments (APP-CTFa and APP-CTFß) were indicated. B Morris Water Maze analyses. The time of the mice (n = 9) spent in the target quadrant at 2 and 9 months old was recorded and compared. C Congo red staining of Aß plaques in the mouse brain. Aß plaques in the cortex and hippocampus of the mice (n = 6) were stained. The plaque burden was quantified and compared. D APP immunoblotting of mouse serum and brain lysates. The IgG-removed serum and brain tissues of the mice at 9 months old were immunoblotted with anti-C-terminal APP antibody, and the gel stained with CBB was used as a loading control. The full-length APP (APP-FL), APP C-terminal fragments (APP-CTFs), and Aß oligomers were indicated. E APP immunoprecipitation and acrolein immunoblotting of mouse serum and brain lysates. The IgG-removed serum and brain tissues of the mice at 9 months old were immunoprecipitated with anti-C-terminal APP antibody and then subjected to immunoblotting with anti-acrolein antibody. A duplicated gel was stained with CBB as a loading control. The prestained protein ladder showed some luminance. AD, Alzheimer’s disease; APP, amyloid precursor protein; CBB, Coomassie brilliant blue; CTF, C-terminal fragment; IP, immunoprecipitation; M, marker; V, vector plasmid p-CAX; WT, wild-type. *** p < 0.001
To investigate the acrolein adduction in an animal model, we used 3xTg-AD mice and tested them using Morris water maze, histochemistry, immunoprecipitation, and immunoblotting. The water maze test revealed that 3xTg-AD mice spent a shorter time in the target quadrant than did WT with a statistical significance at 9 months old (p < 0.001) (Fig. 1B). Congo red-stained mouse brain sections showed an increased Aß plaque burden in AD mice compared to WT mice at 9 months old, especially in the cortical and hippocampal regions (Fig. 1C). Immunoblotting showed higher band intensity of APP isoforms and fragments including APP-CTFs which contain Aß peptides in the serum and brain lysates of the AD mice compared to WT mice (Fig. 1D). After the AD mouse model was verified, serum and brain lysates of the mice were used to analyze acrolein adduction. Pooled mouse serum and brain lysates were immunoprecipitated with a C-terminal APP antibody and then immunoblotted with acrolein. The level of acrolein adducts was increased obviously in the pooled AD mouse serum and brain lysates compared to those in WT mice, especially on APP-CTFs (Fig. 1E). These results further demonstrated the specific acrolein modification on Aß-containing peptides.
Correlation of acrolein adducts with MetS in AD patients
The levels of Aß and acrolein adducts in human serum were measured. The concentrations of biochemicals in routine clinical tests were provided by the Biobank as described in Materials and Methods. As shown in Fig. 2, the average levels of Aß and total protein seemed unchanged in the serum of AD patients compared to those of the control subjects, whereas acrolein adducts were significantly increased in AD serum (p < 0.001) (Fig. 2A). Interestingly, Pearson correlation analysis revealed that the level of acrolein adducts correlated positively with Aß and negatively with total protein (Fig. 2B). It suggests that acrolein adducts may be largely formed on Aß, which supports the findings in the AD models (Fig. 1A and E). Furthermore, the negative correlation of acrolein adducts with total protein in human serum may indicate a reduction of certain types of protein (i.e., antibodies) when acrolein adducts were increased in AD blood. Notably, significant correlations were also found between acrolein adducts and MetS parameters, including fasting glucose, triglycerides, and HDL-C (Fig. 2C). Therefore, both control and AD groups were further divided according to MetS-related laboratory test results as described in the “Materials and methods” section. However, the average age of the AD subjects was unexpectedly older than the control subjects with statistical significance. Therefore, Pearson correlation analysis was also performed to clarify the effects of age on these parameters, especially acrolein adducts, in the AD and non-AD control groups. It was plausible that age was not correlated with acrolein adducts or most of the tested parameters, except the negative correlation of age with total cholesterol and HDL-C in the control group (Table S1).
Correlation of acrolein adducts with specific metabolites in human serum. A Levels of Aß, acrolein adducts, and total protein (TP) in human serum samples. All the values were normalized with the mean of control. In the box plots, the dots represent the 5th and 95th percentiles; the error bars cover the 10th to 90th percentiles and the box covers the 25th to 75th percentiles; the solid and dash lines within the box represent the median and mean values, respectively. B Correlation of acrolein adducts with Aß and TP. Serum Aß and TP values were plotted against the level of acrolein adducts in control and AD subjects, respectively. The solid and broken lines represent the linear regression of the values in control and AD subjects, respectively. Pearson product moment correlation coefficients (r) of acrolein adducts with Aß and TP were shown with p values. C. Correlation of acrolein adducts with the metabolites related to metabolic syndrome. Serum fasting glucose (Glc), triglycerides (TG), and HDL-C values of control or AD subjects were plotted against the level of acrolein adducts. The solid and broken lines represent the regression of the values in control and AD subjects, respectively. Pearson product moment correlation coefficients (r) of acrolein adducts with Glc, TG, and HDL-C were shown with p values. Aß, amyloid-beta; AD, Alzheimer’s disease; Ctrl, control; HDL-C, high-density lipoprotein-cholesterol; TG, triglycerides; TP, total protein.*** p < 0.001
Clinical profile and laboratory test results of the four groups, namely HC, MetS, AD-N, and AD-M, were summarized with mean ± SD in Table 1 and p values in Table S2. As expected, significant differences in fasting glucose, triglycerides, and HDL-C were observed between the groups with and without metabolic disturbance due to the sorting criteria. Likewise, HbA1c, LDL-C, and creatinine were also significantly different between the groups owing to MetS-related conditions. Although the average concentrations of both HDL-C and LDL-C were significantly lower in AD-M than in the MetS group, they were not considered different because of the age effect as mentioned (Table S1). No statistical differences were seen in gender, ALT, total cholesterol, and total protein between the groups.
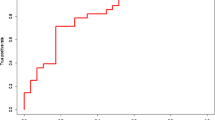
Enhanced acrolein-Aß adducts in the serum of AD patients with metabolic disturbance
Among the four groups, no significant difference in Aß level was observed (Fig. 3A). There were no significant differences in acrolein adducts observed among HC, MetS, and AD-N groups, either (Fig. 3B). Only in the AD-M group, the level of acrolein adducts was significantly increased compared to all other groups. The best AUC value of ROC analysis on acrolein adducts was observed in distinguishing AD-M from MetS (AUC = 0.729). These results suggest that acrolein adducts may be a better biomarker than Aß for not only AD pathology but also the pathogenesis from metabolic disturbance to neurodegeneration in AD.
Acrolein adducts on APP fragments and Aß peptides in human serum. A The relative levels of Aß in different groups of human serum sample. B The relative levels of acrolein adducts in different groups of human serum sample. All the values were normalized with the mean of healthy control (HC). The dots represent the 5th and 95th percentiles; the error bars cover the 10th to 90th percentiles and the box covers the 25th to 75th percentiles; the solid and dash lines within the box represent the median and mean values, respectively. The receiver operating characteristic curves were plotted with the area under curve values shown in brackets when the p value is < 0.001 between groups. C APP immunoprecipitation and acrolein immunoblotting of human serum. Pooled human serum samples from each group were IgG-removed and immunoprecipitated with anti-C-terminal APP antibody and then subjected to SDS-PAGE in triplicate. Two gels were immunoblotted with anti-C-terminal APP and acrolein antibodies, respectively. Another gel was stained with CBB as a loading control. The prestained protein ladder showed some luminance. Aß, amyloid beta; AD-M, Alzheimer’s disease with metabolic disturbance; AD-N, Alzheimer’s disease with normal metabolism; APP, amyloid precursor protein; CBB, Coomassie brilliant blue; HC, healthy control; IP, immunoprecipitation; M, marker; MetS, metabolic syndrome.***p < 0.001
To detect acrolein adducts in more detail, human serum samples were pooled and subjected to immunoprecipitation and immunoblotting. The major APP species appeared near 48 kDa, and a minor species was seen near 28 kDa in the serum samples (Fig. 3C). They have been suggested as truncated APP-CTFs [28]. The low molecular-weight fragments were highly reactive to anti-acrolein antibody, especially in AD-M samples. These results were consistent with the findings in AD models and the ELISA data from human subjects, indicating that the formation of acrolein-Aß adducts may be highly correlated with metabolic disturbance in AD pathogenesis.
In vitro acrolein-modified Aß analyses
To further analyze acrolein-Aß adducts and their responding autoantibodies, we used synthetic Aß1-16 and Aß17-28 peptides and modified them with acrolein in vitro. Acrolein modification of Aß was verified by LC–MS/MS. Native and modified peptides were identified as b-ion (N-terminal fragments) and y-ion (C-terminal fragments) series. Native Aß1-16 fragment ion showed the [M + H]+ at 1953.87 and Aß17-28 at 1324.67 (Figs. 4A and 5A and Table 2). The molecular weight of acrolein is 56.06 Da. When acrolein binds proteins, four different types of adduct including schiff-base (+ 38 Da), aza-michael (+ 56 Da), Ne-lysine (MP-lysine) (+ 76 Da), and FDP-lysine (+ 94 Da) can be formed [29]. Acrolein modification on synthetic Aß peptides were observed on H6, H13, H14, and K16 on Aß1-16, and K28 on Aß17-28 (Figs. 4B and 5B and Table 2). Mainly aza-michael adducts were found on histidine residues, while all four types of adduct were found on lysine residues with schiff-base in the majority. The highest intensity of acrolein adducts was seen on K28 (Fig. 5B), while the most spectral count of the adducts was on K16 (Table 2). These results were consistent with the finding of acrolein modification on Aß-containing peptides as seen in mouse serum and brain lysates (Fig. 1) and human serum (Fig. 3).
Mass spectra of the native and acrolein-modified Aß1-16. The ion density (y-axis) was plotted against m/z ratio (x-axis). The b-ions (blue peaks) represent N-terminal fragments, whereas y-ions (red peaks) represents C-terminal fragments. Acrolein-modified histidine and lysine were pointed with arrows. A Native Aß1-16 peptide. B Acrolein-modified Aß1-16 at H6, H13, H14 or K16. Only the selected spectra were shown
Mass spectra of the native and acrolein-modified Aß17-28. The ion density (y-axis) was plotted against m/z ratio (x-axis). The b-ions (blue peaks) represents N-terminal fragments, whereas y-ions (red peaks) represents C-terminal fragments. Acrolein-modified histidine and lysine were pointed with arrows. A Native Aß17-28 peptide. B Acrolein-modified Aß17-28 at K28. Only the selected spectra were shown
Alterations in anti-acrolein autoantibodies in AD patients with metabolic disturbance
Pearson correlation analysis revealed a negative correlation of acrolein adducts with total protein, especially in AD blood (Fig. 2B). We hypothesize that the increase of acrolein adducts as seen in AD-M condition (Fig. 3B) may be due to the depletion of acrolein-responding autoantibodies which are supposed to be an abundant protein type to neutralize toxic acrolein adducts. To test this hypothesis, we measured anti-acrolein antibody isotypes IgG and IgM in the human serum samples using acrolein-modified synthetic Aß1-16 and Aß17-28 peptides as antigens in ELISA. Native Aß peptides were used as control items.
No differences were seen in the relative levels of IgG against native Aß peptides among all groups (Fig. S2A). However, the ratio of anti-Aß1-16 IgG to the peptide was reduced slightly in the AD-M group compared to HC although the ratio of anti-Aß17-28 IgG to the peptide remained no difference among all groups (Fig. S2B). Unlikely, the relative level of IgG against acrolein-modified Aß1-16 was increased in the AD-M group moderately when compared to MetS and largely when compared to HC (p < 0.001) with an AUC value of 0.711 in ROC analysis (Fig. 6A). Nevertheless, the level of IgG against acrolein-modified Aß17-28 showed the same among all groups. Notably, the ratio of anti-acrolein-Aß1-16 IgG to acrolein adducts became no difference among all groups, while the ratio of anti-acrolein-Aß17-28 IgG to acrolein adducts was reduced moderately in AD-M group compared to MetS (Fig. 6B). Since the immune responses shall depend on the antigen levels, the ratio of the antibody to the specific antigen may provide a more useful evaluation. Therefore, these results suggest that the responding IgG levels, despite anti-native Aß or anti-acrolein-modified Aß, were reduced with slight to moderate amounts when MetS patients developed AD.
Change of IgG autoantibodies against acrolein-Aß adducts in human serum. A The relative levels of IgG autoantibody recognizing acrolein-modified Aß1-16 and Aß17-28 peptides in each group. All the values were normalized with the mean of healthy control (HC). B The ratio of the responding IgG to acrolein adducts of each subject in each group. In the box plots, the dots represent the 5th and 95th percentiles. The error bars cover the 10th to 90th percentiles and the box covers the 25th to 75th percentiles. The solid and dashed lines within the box represent the median and mean values, respectively. The receiver operating characteristic curves were plotted with the area under curve values shown in brackets when the p value is < 0.001 between groups. Aß, amyloid beta; AD-M, Alzheimer’s disease with metabolic disturbance; AD-N, Alzheimer’s disease with normal metabolism; HC, healthy control; MetS, metabolic syndrome.**p < 0.01, ***p < 0.001
Similarly, both the level of IgM against native Aß1-16 and the ratio of anti-Aß1-16 IgM to the peptide were reduced moderately in the AD-M group compared to both MetS and HC (Fig. S3). In contrast, the level of IgM against acrolein-Aß17-28 and the ratio of both anti-acrolein-Aß1-16 and anti-acrolein-Aß17-28 IgM antibodies to acrolein adducts were reduced largely in AD-M group compared to MetS (p < 0.001) with AUC values from 0.693 to 0.755 in ROC analyses (Fig. 7). It was supportive in Pearson correlation analyses that the level of acrolein adducts was negatively correlated with anti-acrolein-Aß17-28 IgM although it was positively correlated with the specific IgG against native Aß1-16 in all samples (Table S3). These results suggest that the specific IgM autoantibodies against acrolein adducts, such as acrolein-Aß, were reduced largely when MetS patients developed AD and are potential biomarkers in AD pathology. In addition, acrolein-Aß adducts may be considered for the immunotherapy of AD, especially when AD is complexed with MetS.
Change of IgM autoantibodies against acrolein-Aß adducts in human serum. A The relative levels of IgM autoantibody recognizing acrolein-modified Aß1-16 and Aß17-28 peptides in each group. All the values were normalized with the mean of healthy control (HC). B The ratio of the responding IgM to acrolein adducts of each subject in each group. In the box plots, the dots represent the 5th and 95th percentiles. The error bars cover the 10th to 90th percentiles and the box covers the 25th to 75th percentiles. The solid and dashed lines within the box represent the median and mean values, respectively. The receiver operating characteristic curves were plotted with the area under curve values shown in brackets when the p value is < 0.001 between groups. Aß, amyloid beta; AD-M, Alzheimer’s disease with metabolic disturbance; AD-N, Alzheimer’s disease with normal metabolism; HC, healthy control; MetS, metabolic syndrome.* p < 0.05, **p < 0.01, ***p < 0.001
Discussion
A recent Korean study demonstrates the association between MetS to developed AD in eight years [6]. It suggests that MetS patients are 11.48 times more prone to have AD than those without MetS. Statistical analysis of Taiwanese primary data from the National Health Insurance Research Database with encryption also reports the link between AD progressions from MetS [5]. This study explained the statistically significant relationship between dementia and worsen MetS compared to non-persistent MetS, improved MetS, or non-MetS in the follow-up period of 10 years. MetS is a prolonged state of oxidative stress which is resulted from abnormal metabolism of carbohydrates and lipids, inducing lipid peroxidation to generate aldehydic byproducts, especially acrolein adducts. Along with the accumulation of Aß in the diseased brain, the immune system may be stimulated to worsen AD progression.
In this study, acrolein adducts were found to correlate positively with triglycerides and negatively with HDL-C (Fig. 2C and Table S3). Research suggests that precautionary measurement in early (35–50 years) to middle (51–60 years) adulthood to maintain HDL-C and triglycerides levels may lower the risks of AD [30]. High circulating HDL levels have been linked to a lower risk of Alzheimer's disease in numerous epidemiological studies [24]. HDL appears to protect against memory loss, neuroinflammation, and cerebral amyloid angiopathy by lowering vascular Aß accumulation and attenuating Aß-induced endothelial inflammation. In contrast, high level of triglycerides can cause cognitive decline by blood brain barrier (BBB) dysfunction or amyloid metabolism imbalance [31]. However, cognitive function can be improved by coconut oil or medium-chain triglycerides. Omega-3 polyunsaturated fatty acids (ω-3-PUFAs) are key components of the neuronal membrane which acts as neuroprotective agent [32]. Impaired neurotransmission was observed in ω-3-PUFA-deficient animal [33]. Reduction in Aß production by altering APP pathological processing pathway is due to docosahexaenoic acid (22:6ω-3). A negative correlation was found in ω-3/ω-6 ratio with AD incidence and cognitive decline. Reduced docosahexaenoic acid and eicosapentaenoic acid (20:5ω-3) levels have been observed in AD brain autopsy, serum, and plasma.
Byproducts of PUFA oxidation are acrolein and HNE specifically from ω-6 PUFAs, such as arachidonic acid which is abundant in gray matter [2, 34]. Arachidonic acid oxidation in the presence of Aß in vitro produces HNE earlier than acrolein. It causes a high level of HNE at first and then leads to increased HNE-protein adducts but little extractable free HNE. In contrast, fewer acrolein-protein adducts and more extractable acrolein is produced. It has been shown that acrolein is much more toxic than HNE as seen in the primary culture of rat hippocampal neurons [37]. Polyamine like spermine helps for the suppression of Aß aggregation. A high level of acrolein forms conjugation with substrate and catalyst involved in tricarboxylic acid cycle, glycolysis, and carbon metabolism. These conjugations inhibit the energy metabolism under oxidative stress in AD conditions. Among acrolein-related risk factors for AD, smoking is also important due to increased oxidative stress and specially acrolein production. Impaired nitric oxide synthesis due to smoking alters glucose metabolism and cerebral blood flow in cerebral vascular endothelial cells of the brain. It stimulates Aß production, cerebral hypoperfusion, cytokine activation, and immune response, which are also helpful for AD diagnosis [38, 39].
Conclusion
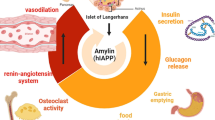
Based on the present data, we conclude that metabolic disturbance may induce acrolein production and form adducts largely on Aß through oxidative stress. These adducts may lead to alterations in the autoantibodies, in which an increased level helps to slow disease progression by neutralizing and degrading acrolein adducts, whereas a decreased level of autoantibodies may lead to worse neurodegeneration and cause severe AD. This study explains the close relationship between AD and MetS by suggesting the mechanism that acrolein adduction in MetS may deplete responding autoantibodies and cause neurodegeneration in AD (Fig. 8).
Proposed reactions of acrolein-Aß adduct formation and degradation in correlation with metabolic disturbance and neurodegeneration. Under metabolic disturbance, oxidation of lipids generates aldehydic byproducts such as acrolein, which further reacts with peptides such as Aß and forms adducts. These adducts are responsible for neurodegeneration. However, the responding autoantibodies may inhibit the disease progression by neutralizing and degrading these adducts. Depletion of the responding autoantibodies by acrolein adducts may lead to worse neurodegeneration
Availability of data and materials
Data sharing is not applicable to this article. All other data are available from the corresponding author on reasonable request.
Abbreviations
- Aß:
-
Amyloid-beta
- AD:
-
Alzheimer’s disease
- AD-M:
-
Alzheimer’s disease with metabolic disturbance
- AD-N:
-
Alzheimer’s disease with normal metabolism
- APP:
-
Amyloid precursor protein
- AUC:
-
Area under curve
- BBB:
-
Brain blood barrier
- BSA:
-
Bovine serum albumin
- CBB:
-
Coomassie brilliant blue
- Ctrl:
-
Control
- ELISA:
-
Enzyme-linked immunosorbent assay
- HbA1c:
-
Glycohemoglobin A1
- HC:
-
Healthy control
- HDL:
-
High-density lipoprotein-cholesterol
- HNE:
-
4-Hydroxynonenal
- LC–MS-MS:
-
Liquid chromatography with tandem mass spectrometry
- LDL-C:
-
Low-density lipoprotein-cholesterol
- MetS:
-
Metabolic syndrome
- PBS:
-
Phosphate buffer saline
- PUFA:
-
Polyunsaturated fatty acid
- ROC:
-
Receiver operating characteristic
- ROS:
-
Reactive oxygen species
- SDS-PAGE:
-
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis
References
Wolfe MS. The secretases of Alzheimer’s disease. Curr Top Dev Biol. 2003;54:233–61.
Bradley-Whitman MA, Lovell MA. Biomarkers of lipid peroxidation in Alzheimer disease (AD): an update. Arch Toxicol. 2015;89(7):1035–44.
Rojas-Gutierrez E, Munoz-Arenas G, Trevino S, Espinosa B, Chavez R, Rojas K, et al. Alzheimer’s disease and metabolic syndrome: A link from oxidative stress and inflammation to neurodegeneration. Synapse. 2017;71(10): e21990.
Shieh JC, Huang PT, Lin YF. Alzheimer’s Disease and Diabetes: Insulin Signaling as the Bridge Linking Two Pathologies. Mol Neurobiol. 2020;57(4):1966–77.
Fan YC, Chou CC, You SL, Sun CA, Chen CJ, Bai CH. Impact of Worsened Metabolic Syndrome on the Risk of Dementia: A Nationwide Cohort Study. J Am Heart Assoc. 2017;6(9):e004749.
Kim YJ, Kim SM, Jeong DH, Lee SK, Ahn ME, Ryu OH. Associations between metabolic syndrome and type of dementia: analysis based on the National Health Insurance Service database of Gangwon province in South Korea. Diabetol Metab Syndr. 2021;13(1):4.
Lovell MA, **e C, Markesbery WR. Acrolein is increased in Alzheimer’s disease brain and is toxic to primary hippocampal cultures. Neurobiol Aging. 2001;22(2):187–94.
Alfarhan M, Jafari E, Narayanan SP. Acrolein: A Potential Mediator of Oxidative Damage in Diabetic Retinopathy. Biomolecules. 2020;10(11):1579.
Chen C, Lu J, Peng W, Mak MS, Yang Y, Zhu Z, et al. Acrolein, an endogenous aldehyde induces Alzheimer’s disease-like pathologies in mice: A new sporadic AD animal model. Pharmacol Res. 2022;175: 106003.
Chen C, Chen Y, Lu J, Chen Z, Wang C, Pi R. Acrolein-conjugated proteomics in brains of adult C57BL/6 mice chronically exposed to acrolein and aged APP/PS1 transgenic AD mice. Toxicol Lett. 2021;344:11–7.
Moghe A, Ghare S, Lamoreau B, Mohammad M, Barve S, McClain C, et al. Molecular mechanisms of acrolein toxicity: relevance to human disease. Toxicol Sci. 2015;143(2):242–55.
Kwon D. Guardians of the brain: how a special immune system protects our grey matter. Nature. 2022;606(7912):22–4.
Angiolillo A, Gandaglia A, Arcaro A, Carpi A, Gentile F, Naso F, et al. Altered Blood Levels of Anti-Gal Antibodies in Alzheimer’s Disease: A New Clue to Pathogenesis? Life (Basel). 2021;11(6):538.
Wang BZ, Zailan FZ, Wong BYX, Ng KP, Kandiah N. Identification of novel candidate autoantibodies in Alzheimer’s disease. Eur J Neurol. 2020;27(11):2292–6.
DeMarshall CA, Nagele EP, Sarkar A, Acharya NK, Godsey G, Goldwaser EL, et al. Detection of Alzheimer’s disease at mild cognitive impairment and disease progression using autoantibodies as blood-based biomarkers. Alzheimers Dement (Amst). 2016;3:51–62.
Agrawal S, Abud EM, Snigdha S, Agrawal A. IgM response against amyloid-beta in aging: a potential peripheral protective mechanism. Alzheimers Res Ther. 2018;10(1):81.
Liu YH, Wang J, Li QX, Fowler CJ, Zeng F, Deng J, et al. Association of naturally occurring antibodies to ß-amyloid with cognitive decline and cerebral amyloidosis in Alzheimer's disease. Sci Adv. 2021;7(1):eabb0457.
Renuka Sanotra M, Huang WC, Silver S, Lin CY, Chang TC, Nguyen DPQ, et al. Serum levels of 4-hydroxynonenal adducts and responding autoantibodies correlate with the pathogenesis from hyperglycemia to Alzheimer’s disease. Clin Biochem. 2022;101:26–34.
Lin CY, Sheu JJ, Tsai IS, Wang ST, Yang LY, Hsu IU, et al. Elevated IgM against Nepsilon-(Carboxyethyl)lysine-modified Apolipoprotein A1 peptide 141–147 in Taiwanese with Alzheimer’s disease. Clin Biochem. 2018;56:75–82.
Tsai YF, Yang DJ, Ngo TH, Shih CH, Wu YF, Lee CK, et al. Ganglioside Hp-s1 Analogue Inhibits Amyloidogenic Toxicity in Alzheimer’s Disease Model Cells. ACS Chem Neurosci. 2019;10(1):528–36.
Ting LL, Lu HT, Yen SF, Ngo TH, Tu FY, Tsai IS, et al. Expression of AHI1 Rescues Amyloidogenic Pathology in Alzheimer’s Disease Model Cells. Mol Neurobiol. 2019;56(11):7572–82.
Guze SB. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Am J Psychiatry. 1995;152(8):1228.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–44.
Button EB, Robert J, Caffrey TM, Fan J, Zhao W, Wellington CL. HDL from an Alzheimer’s disease perspective. Curr Opin Lipidol. 2019;30(3):224–34.
Chen GF, Xu TH, Yan Y, Zhou YR, Jiang Y, Melcher K, et al. Amyloid beta: structure, biology and structure-based therapeutic development. Acta Pharmacol Sin. 2017;38(9):1205–35.
Liu J, Yang B, Ke J, Li W, Suen WC. Antibody-Based Drugs and Approaches Against Amyloid-beta Species for Alzheimer’s Disease Immunotherapy. Drugs Aging. 2016;33(10):685–97.
Uen YH, Liao CC, Lin JC, Pan YH, Liu YC, Chen YC, et al. Analysis of differentially expressed novel post-translational modifications of plasma apolipoprotein E in Taiwanese females with breast cancer. J Proteomics. 2015;126:252–62.
Sheu JJ, Yang LY, Sanotra MR, Wang ST, Lu HT, Kam RSY, et al. Reduction of AHI1 in the serum of Taiwanese with probable Alzheimer’s disease. Clin Biochem. 2020;76:24–30.
Lasse M, Stampfli AR, Orban T, Bothara RK, Gerrard JA, Fairbanks AJ, et al. Reaction dynamics and residue identification of haemoglobin modification by acrolein, a lipid-peroxidation by-product. Biochim Biophys Acta Gen Subj. 2021;1865(12): 130013.
Zhang X, Tong T, Chang A, Ang TFA, Tao Q, Auerbach S, et al. Midlife lipid and glucose levels are associated with Alzheimer's disease. Alzheimers Dement. 2023;19(1):181–93.
Dimache AM, Salaru DL, Sascau R, Statescu C. The Role of High Triglycerides Level in Predicting Cognitive Impairment: A Review of Current Evidence. Nutrients. 2021;13(6):2118.
Cutuli D, De Bartolo P, Caporali P, Laricchiuta D, Foti F, Ronci M, et al. n-3 polyunsaturated fatty acids supplementation enhances hippocampal functionality in aged mice. Front Aging Neurosci. 2014;6:220.
Mett J. The Impact of Medium Chain and Polyunsaturated omega-3-Fatty Acids on Amyloid-beta Deposition, Oxidative Stress and Metabolic Dysfunction Associated with Alzheimer’s Disease. Antioxidants (Basel). 2021;10(12):1991.
Bradley MA, Markesbery WR, Lovell MA. Increased levels of 4-hydroxynonenal and acrolein in the brain in preclinical Alzheimer disease. Free Radic Biol Med. 2010;48(12):1570–6.
Endo R, Uchiyama K, Lim SY, Itakura M, Adachi T, Uchida K. Recognition of acrolein-specific epitopes by B cell receptors triggers an innate immune response. J Biol Chem. 2021;296: 100648.
Selkoe DJ. Treatments for Alzheimer’s disease emerge. Science. 2021;373(6555):624–6.
Lu Y, Liu J, Tong A, Lu Y, Lv L. Interconversion and Acrolein-Trap** Capacity of Cardamonin/Alpinetin and Their Metabolites In Vitro and In Vivo. J Agric Food Chem. 2021;69(40):11926–36.
Toda N, Okamura T. Cigarette smoking impairs nitric oxide-mediated cerebral blood flow increase: Implications for Alzheimer’s disease. J Pharmacol Sci. 2016;131(4):223–32.
Durazzo TC, Mattsson N, Weiner MW, Alzheimer's Disease Neuroimaging I. Smoking and increased Alzheimer's disease risk: a review of potential mechanisms. Alzheimers Dement. 2014;10(3 Suppl):S122–45.
Acknowledgements
The authors thank Dr. Ching-Yu Lin at Taipei Medical University for his suggestions on the experiments as well as Yu-Tung Cheng, Gabriela Chelsea Suhartanto, and Yuyi Huang at Taipei Medical University and Hui-Wen Chang at Taipei Medical University Hospital for their assistance on the sample processing.
Funding
This study was supported by the National Science and Technology Council (108–2622-B-038–001, 111-2314-B-532-001) and the Department of Health, Taipei City Government (11201–62-033), Taiwan (R.O.C.).
Author information
Authors and Affiliations
Contributions
MRS and YFL designed the study. SHK, CKL, CHH, WCH and YFL provided critical materials. TCC and IUH collected samples. MRS and FYT acquired the data. MRS, SHK, CKL and YFL analyzed and interpretated the data. MRS, SHK, CKL and YFL wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal procedures were approved by the Institutional Animal Care and Use Committee in Taipei Medical University (LAC-2019–0448). Human serum was used as per the Code of Ethics of the World Medical Association and approved by Taipei Medical University Joint Institutional Review Board (N201802044).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Pearson correlation of age with the tested variables. Table S2. Statistical significance of demographic and clinical data (p value) between the groups. Table S3. Correlation of all tested variables. Fig. S1. Acrolein structure. PubChem, Acrolein. National Center for Biotechnology Information, 2022. Retrieved from https://pubchem.ncbi.nlm.nih.gov/compound/Acrolein. Fig. S2. Levels of IgG autoantibodies against native Aß peptides in human serum. Fig. S3. Levels of IgM autoantibodies against native Aß peptides in human serum.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sanotra, M.R., Kao, SH., Lee, CK. et al. Acrolein adducts and responding autoantibodies correlate with metabolic disturbance in Alzheimer’s disease. Alz Res Therapy 15, 115 (2023). https://doi.org/10.1186/s13195-023-01261-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-023-01261-2