Abstract
Background
Chronic heart failure (HF) is known to increase the risk of develo** Alzheimer’s dementia significantly. Thus, detecting and preventing mild cognitive impairment, which is common in patients with HF, is of great importance. Serum biomarkers are increasingly used in neurological disorders for diagnostics, monitoring, and prognostication of disease course. It remains unclear if neuronal biomarkers may help detect cognitive impairment in this high-risk population. Also, the influence of chronic HF and concomitant renal dysfunction on these biomarkers is not well understood.
Methods
Within the monocentric Cognition.Matters-HF study, we quantified the serum levels of phosphorylated tau protein 181 (pTau) and neurofilament light chain (NfL) of 146 extensively phenotyped chronic heart failure patients (aged 32 to 85 years; 15.1% women) using ultrasensitive bead-based single-molecule immunoassays. The clinical work-up included advanced cognitive testing and cerebral magnetic resonance imaging (MRI).
Results
Serum concentrations of NfL ranged from 5.4 to 215.0 pg/ml (median 26.4 pg/ml) and of pTau from 0.51 to 9.22 pg/ml (median 1.57 pg/ml). We detected mild cognitive impairment (i.e., T-score < 40 in at least one cognitive domain) in 60% of heart failure patients. pTau (p = 0.014), but not NfL, was elevated in this group. Both NfL (ρ = − 0.21; p = 0.013) and pTau (ρ = − 0.25; p = 0.002) related to the cognitive domain visual/verbal memory, as well as white matter hyperintensity volume and cerebral and hippocampal atrophy. In multivariable analysis, both biomarkers were independently influenced by age (T = 4.6 for pTau; T = 5.9 for NfL) and glomerular filtration rate (T = − 2.4 for pTau; T = − 3.4 for NfL). Markers of chronic heart failure, left atrial volume index (T = 4.6) and NT-proBNP (T = 2.8), were further cardiological determinants of pTau and NfL, respectively. In addition, pTau was also strongly affected by serum creatine kinase levels (T = 6.5) and ferritin (T = − 3.1).
Conclusions
pTau and NfL serum levels are strongly influenced by age-dependent renal and cardiac dysfunction. These findings point towards the need for longitudinal examinations and consideration of frequent comorbidities when using neuronal serum biomarkers.
Similar content being viewed by others
Background
Alzheimer’s dementia (AD) is a growing medical and health economic challenge with a rapidly increasing incidence due to aging and already affects approximately 50 million people worldwide [1]. Whereas a strict dividing line was once conceptually drawn between AD and vascular dementia, it is now widely accepted that cardio- and cerebrovascular risk factors significantly increase the likelihood of develo** AD [2, 3]. In addition to stroke, chronic heart failure (HF) in particular predisposes to the development of AD, as shown in population-based studies [4, 5]. HF is a common and serious consequence of many cardiac diseases and carries a grave prognosis [6]. More than 50% of chronic HF patients show mild cognitive impairment interfering with their daily activities and affecting their drug compliance [7].
The ability of highly sensitive immunoassays to detect ultra-low serum levels of neuronal biomarkers has made them even more useful for prognostic or diagnostic purposes in numerous neurodegenerative diseases and dementia [8]. In particular, serum neurofilament light chain (NfL), a structural neuronal intermediate filament, has evolved as a promising biomarker in pre-clinical and clinical dementia [9,10,11]. Serum NfL is closely associated with brain volume loss and cognitive deficits in general [12]. In contrast, tau protein, which is expressed abundantly in neurons and—at lower levels—in astrocytes and oligodendrocytes, promotes microtubule assembly and stability [13]. Abnormal hyperphosphorylation leads to increased levels of phosphorylated tau 181 (pTau) in cerebral spinal fluid and serum. pTau emerged as a plasma and serum biomarker of cerebral tau and amyloid pathologies, which are hallmarks of AD [14, 15].
At present, it is unclear, whether NfL or pTau serum levels indicate cognitive involvement in non-neurological diseases and if they are affected by internistic co-morbidity. In the present study of patients with chronic stable HF, 60% showed (mild) cognitive impairment, while the diagnosis of manifest dementia was an exclusion criterion at study entry [16, 17]. Thus, the Cognition.Matters-HF study offers the opportunity to test whether serum concentrations of both biomarkers may relate to subtle cognitive impairment and brain degeneration in this cohort, which is at high risk for develo** manifest dementia.
Methods
Study design
We made use of the clinical data and biomaterials collected in the course of the prospective, monocentric Cognition.Matters-HF study. Its design and applied methodology have been reported in detail previously [16, 17]. The study recruited adult patients with chronic stable HF according to the then-current guidelines of the European Society of Cardiology [18]. Patients with apparent neurological or psychiatric disease, history of clinical stroke, or carotid artery stenosis over 50% were not eligible. The selection criteria are summarized in Supplemental Table S1. Cognition.Matters-HF was conducted in compliance with the Declaration of Helsinki and approved by the local ethics committee (#245/10) [17].
Clinical evaluation
Physical examination, electrocardiography, echocardiography, and 6-min walk test were performed according to the standard operating procedures by the trained staff (for details, refer to Supplemental Methods) [16, 17]. The neurological evaluation included extensive clinical examination. Psychological testing was performed between 9 a.m. and 11 a.m. using a comprehensive test battery based on a taxonomy of attention dimensions (summarized in Supplemental Table S2). T-standardized output values accounting for the modifying effect of age, gender, and educational level were reported with a mean of 50 and a standard deviation of 10.
Cerebral magnetic resonance imaging
Brain MRI was performed at a 3-T scanner (Siemens MAGNETOM Trio, Siemens Healthcare, Erlangen, Germany) as described previously [17]. Briefly, the applied MRI protocol enabled the estimation of global and regional measures of brain structure degeneration by visual rating (Supplemental Table S3). The visual rating of cerebral atrophy ranged on a scale from 1 to 8. For the assessment of medial temporal lobe atrophy, Scheltens score ranging from 0 (normal) to 4 (severe atrophy) was applied, and the mean scores of both sides (left and right) were reported.
Laboratory analysis
Non-fasting venous blood samples were collected for routine clinical chemistry investigations at the certified facility of the University Hospital Würzburg. Participants were positioned seated for at least 5 min before puncture. Serum samples were processed immediately, i.e., remained at room temperature for 30 min and were centrifuged for 10 min at 2000 × g. The serum was aliquoted in dedicated fluid tissue tubes (Micronic, Lelystad, The Netherlands) and stored in the standardized interdisciplinary biomaterial bank at − 80 °C until analysis [19]. Serum NfL was measured using 5 (ProteinSimple™; San Jose, CA, USA) and pTau using the Simoa pTau-181 advantage kit (103377; Quanterix™, Billerica, MA, USA) on a Simoa HD-1 Analyzer instrument (Quanterix™, Billerica, MA, USA) in accordance with the manufacturer’s instructions. These measurements were performed blinded to the patients’ other results at the Department for Neurology of the University Hospital Ulm [9]. The inter-assay coefficient of variability for the human NF-L Ella instrument kit was 9.6% for high and 21.6% for low serum quality control, with a lower limit of quantification of 5.4 pg/ml. The intra-assay coefficient of variability of this assay has been validated elsewhere [20]. For the Simoa pTau-181 advantage kit, the inter-assay coefficient of variability was 7.0% for high and 11.2% for low-quality control. The intra-assay coefficient of variability was 1.4–9.3% for high- and 9.5–13.8% for low serum quality control. The lower limit of quantification for pTau was 0.222 pg/ml. Samples were measured in single determination and not grouped by cognitive parameters. For one sample, the NfL value was below the lower limit of quantification. Here, for the statistical calculations, the value of 5.4 pg/ml was used.
Data analysis
Statistical analysis was performed using the statistical software SPSS (version 26). To test for normal distribution, we used the Shapiro-Wilk test. Variables were natural log normalized if required. The few missing values (less than 1% missing) were imputed by the mean value of the respective variable. For nominal and ordinal data, the chi-squared test or Fisher’s exact test was used, according to the nature of the data. For correlation analysis, the Spearman rho coefficient was computed. To identify the metric correlates of NfL and pTau levels, univariable linear regression analysis was used and a trend test across quartiles was reported. All tests were performed 2-sided.
When identifying determinants of NfL and pTau, to reduce the overoptimism introduced by multiple testing for the 79 clinical parameters that were used for analysis, a false discovery rate approach using the Benjamini–Hochberg procedure was applied. Thus, identified correlates were then included in univariable regression models. Only significant parameters were included in a multivariable model. Here, we analyzed the correlates using an “enter” approach. Second, we fed the remaining correlates into another regression model, which then was reduced to the final model through backward elimination and reproduced by forward entry. The explained variance of a model was indicated by the coefficients of determination (R2). To address collinearity, we calculated the variance inflation factors for all parameters of the multivariable models [21]. It represents the ratio of the variance of a model’s regression coefficients divided by the variance of a single coefficient. As all inflation factors were < 5, multi-collinearity was considered unlikely.
Using the SPSS PROCESS macro, a simple mediation was performed to analyze whether the total effect (c) of identified correlates was (partly) mediated by one another. This was considered the case, when the effect on the mediator (a) and the effect of the mediator (b) were significant. Partial mediation was claimed, when both direct (c′) and indirect (ab) effects were significant.
Results
Patient characteristics
Serum samples from 146 HF patients exhibiting no focal neurological deficits were available for analysis. As described in Table 1 and reported earlier [17], their age ranged from 32 to 85 years with a mean of 63.8 ± 10.8 years and 15.1% of the participants were women. The mean left ventricular ejection fraction was 42.5 ± 8.2% (16.4% had a preserved ejection fraction defined as ≥ 50%), and 72% of the patients were in New York Heart Association (NYHA) functional class II or III. Ischemia was the predominant underlying cause of HF (65%), and 84% of all patients received optimal HF therapy according to then-current guidelines at the study start [18]. The mean estimated glomerular filtration rate (eGFR) was 66.5 ± 19.4 ml/min/1.73 m2, and 35.6% had a chronic kidney disease of at least grade 3 (defined as eGFR < 60 ml/min/1.73 m2).
Range of neuronal biomarkers
Serum concentrations of NfL ranged from 5.4 to 215.0 pg/ml with a median of 26.4 pg/ml (quartiles 16.7, 42.0). For pTau, the range was 0.51 to 9.22 pg/ml with a median of 1.57 (1.09, 2.41) pg/ml. The levels of both biomarkers did not differ between the sexes. The distribution of biomarkers is detailed in histograms in Fig. S1. Of note, NfL and pTau correlated to one another significantly (ρ = 0.57; p < 0.001).
NfL and pTau are related to memory function and brain atrophy
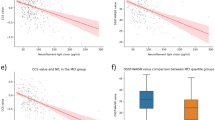
As depicted in Table 1, patients with cognitive impairment (defined as age-adjusted T-score < 40 in at least one domain) had higher levels of pTau, which was not the case for NfL. Also, they had a lower 6-min walking test distance as a measure of chronic HF, while age did not differ between the groups. When examining the distinct cognitive domains in more detail (Fig. 1; Supplemental Table S4), both NfL and pTau significantly correlated to the cognitive domain visual/verbal memory while only pTau related to the selectivity of attention. Furthermore, both biomarkers positively correlated with volume of WMH and cerebral and hippocampal atrophy (quantified by Scheltens score).
Age, renal function, and severity of heart failure predict NfL and pTau serum levels
Next, to identify if clinical parameters affect the serum levels of NfL and pTau, trend tests across quartiles per biomarker were performed (Supplemental Tables S5 and S6). After adjustment for multiple testing and confirmation in univariate regression (Tables 2 and 3), the following interrelations emerged: Patients with higher NfL concentrations were older and had lower estimated glomerular filtration rate (eGFR), larger left atrial volume index (LAVI), lower levels of mean corpuscular hemoglobin concentration and thrombocytes, but higher levels of urea, NT-proBNP, hemoglobin A1c, and uric acid. Furthermore, they had higher systolic pressure, reduced 6-min walking distance, and lower levels of hemoglobin and alanine aminotransferase. High NfL levels were also associated with a longer duration of HF and a more frequent intake of diuretics. Likewise, patients with higher pTau concentrations were older and had lower eGFR, larger left atrial volume index (LAVI), and increased right ventricular diameter. Additionally, they exhibited higher levels of creatine kinase, uric acid, urea, and NT-proBNP, as well as lower levels of thrombocytes, ferritin, mean corpuscular hemoglobin concentration, and alanine aminotransferase.
In a multivariable setting, which included all significant clinical correlates, age and eGFR emerged as strong independent clinical predictors of both biomarkers (Tables 2 and 3). This was also the case for the cardiac parameters NT-proBNP and LAVI, respectively. Furthermore, creatine kinase (CK) and ferritin levels remained strongly related to serum pTau in the final clinical model. Correlation plots of significant predictors are displayed in Figs. 2 and 3. Final clinical models of both NfL and pTau explained variance well, as indicated by R2 of 0.47 and 0.58, respectively.
Cardiac and renal dysfunction partly mediate the effect of age on serum biomarkers
To discriminate if the identified predictors in the final, combined models have a direct or indirect (mediated) effect on the examined serum biomarkers, we performed a mediation analysis (Supplemental Tables S7 and S8). The effect of age on Ln(NfL) was partly mediated by eGFR and NT-proBNP. In line, eGFR and LAVI mediated the effect of age on Ln(pTau). Interestingly, the effect of CK on Ln(pTau) was not mediated by any of the mentioned parameters. These interrelations were finally visualized, as depicted in Fig. 4.
Independent association between biomarkers and cognitive domains
Next, we analyzed if the above-identified clinical correlates of both biomarkers also related to age-adjusted memory T-score (Supplemental Tables S9 and S10), which was the case for renal function in the clinical model. In a thus combined model, NfL and pTau remained independent correlates of visual/verbal memory T-score. pTau also related independently to the selectivity of attention, even when clinical correlates of pTau were considered (Supplemental Table S11).
Finally, we tested if correlates of NfL and pTau relate to volume of WMH, and cerebral and hippocampal atrophy (Supplemental Tables S12, S13 and S14). Age and systolic blood pressure evolved as significant predictors of Ln(WMH volume) along with Ln(NfL) in a combined model. Age, eGFR, and NT-proBNP predicted global atrophy, while NT-proBNP and age were significant predictors of hippocampal atrophy.
Discussion
This post hoc analysis in chronic stable HF patients of the well-phenotyped Cognition.Matters-HF study showed that mild cognitive impairment in this cohort is associated to subtle increases of pTau and NfL, especially regarding memory function. Serum levels of the neuronal biomarkers NfL and pTau were noticeably affected by numerous clinical routine parameters which are established indicators of comorbidity burden. Both NfL and pTau were strongly related to age and renal function and, in addition, were markedly affected by indicators of heart failure severity in the respective final model: NT-proBNP, an indicator of cardiac wall stress and congestion remained associated with NfL levels, and LAVI, an estimate of chronic elevation of cardiac filling pressures, as well as creatinine kinase, a marker of ongoing cardiac damage, remained associated with pTau. Of note, the absence of the association of left ventricular ejection fraction with both markers implies that our findings apply to the whole spectrum of HF, including reduced and preserved ejection fraction. These findings impact the interpretation of NfL and pTau in clinical research and care.
The current analysis was based on serum samples drawn at baseline from a thoroughly characterized cohort of chronic HF patients [17]. As our group has shown before, serum concentrations of NfL are comparable to measurements in plasma samples [9, 11]. For pTau, a very recent study similarly found comparable diagnostic performances and strong correlations between serum versus plasma [22]. A significant number of patients with HF in general [7] and within our cohort showed signs of cognitive impairment as 60% of patients exhibited deficits (T-score < 40) in at least one cognitive domain. We found independent associations of NfL and pTau to memory impairment in our cross-sectional analysis, even when clinical parameters were considered. This is in line with recently published relations of NfL and pTau to cognitive dysfunction in AD [24].
There is strong epidemiological evidence that chronic HF predisposes to the development of AD [4, 5]. Accordingly, increased serum pTau in our HF cohort, which excluded patients with overt dementia at study entry, may indicate incipient AD development since serum/plasma pTau is considered a specific biomarker for AD [25]. This notion is based on observations showing that increased plasma pTau 181 correctly identified individuals who were amyloid β positive in positron emission tomography regardless of clinical diagnosis, and a positive association between higher levels of plasma pTau 181 levels and cortical tau protein deposition measured by F-18-Flortaucipir positron emission tomography [26]. Thus, serum/plasma pTau discriminated between AD and frontotemporal dementia. It will be interesting to sequentially measure serum pTau levels in HF patients to assess, whether these dynamics can predict clinical conversion from mild cognitive decline to overt AD.
With regard to morphologic brain changes, serum NfL and pTau correlated with WMH volume and hippocampal and cerebral atrophy in the univariable setting. In multivariable models including clinical parameters, only a slight association between Ln(NfL) and Ln(WMH volume) remained. The univariable associations of both biomarkers to visually rated global brain atrophy are in line with findings from patients with multiple sclerosis [27], frontotemporal dementia [9], AD [28], and also normal-aging individuals [12]. Furthermore, both biomarkers also positively correlated with the Scheltens score, which quantifies hippocampal atrophy, and has been related to the severity of cognitive symptoms in AD and Lewy body dementia [29, 30]. In patients with heart failure, hippocampal atrophy is a significant and independent predictor of memory impairment, executive dysfunction, and poor prognosis as reported earlier for the Cognition.Matters-HF study sample [17] and by others [31]. Finally, WMH are known to associate with diabetes, smoking, and hypertension and hence considered to be part of small vessel disease coinciding with demyelination, axonal loss, reduced glial density and atrophy [32], and accelerated cognitive decline [33]. Of note, our finding of an independent association of NfL with WMH lesion load in our cohort of HF patients devoid of focal neurological deficits confirms and substantiates an earlier study reporting such correlation in patients with AD [34].
We observed that clinical and laboratory factors profoundly influence NfL and pTau serum concentrations. Associations of NfL with aging are well known both in neurologically healthy subjects, whose brain atrophy during aging is thought to increase serum levels [12], as well as in neurological patients suffering from multiple sclerosis or stroke [35, 36]. While total tau protein in the serum increased with normal aging within a cognitively unaffected cohort [37], pTau values in the cerebrospinal fluid similarly showed a significant correlation with age [38]. Here, for the first time, we describe the association of serum pTau with increasing age and confirm age-dependent findings for NfL in a cohort of heart failure patients without neurological deficits. Interestingly, cardiac and renal dysfunction, but not MRI parameters partly mediated the effect of age on both biomarkers.
Previously, it has been reported that serum NfL levels are partially affected by renal function [36, 39], which was confirmed in our HF cohort, as eGFR negatively correlated with serum NfL. Moreover, we show that this also applies to serum pTau, which has not been reported so far, pointing towards an impaired clearance of these proteins.
Serum levels of creatine kinase evolved as another strong and independent predictor of pTau, but not NfL. This may be caused by the enzymatic activity of creatine kinase in the serum, leading to phosphorylation of tau protein. Furthermore, brain-derived BB isoforms of creatine kinase, diffusing into the serum upon neuronal damage, may increase total creatine kinase levels along with pTau levels. This novel finding can possibly be explained by the presence of tau protein in skeletal muscles [40].
The cross-sectional approach of the current study restricts the interpretation of NfL and pTau. However, the strength of this investigation lies in its extensive clinical work-up, including detailed cognitive testing that included five cognitive function domains instead of global tests. The high explained variance found for the overall models explaining serum NfL and pTau suggests that indeed relevant etiological factors were considered, thus stimulating further research in this direction.
Conclusions
Overall, we found a slight elevation of serum pTau in chronic HF patients with mild cognitive impairment as a possible surrogate marker for impending development of AD. Furthermore, our results have implications for the clinical use of NfL and pTau serum levels as biomarkers for neurodegeneration and dementia such as AD, frontotemporal lobe degeneration, and amyotrophic lateral sclerosis. These conditions predominantly develop in the elderly, who are also frequently burdened by multiple comorbidities. While renal function and other laboratory parameters are regularly available through routine investigations, our study identifies chronic HF as a major confounder of serum NfL and/or pTau that has not been taken into consideration in the numerous previous reports using NfL and pTau as surrogate markers for neurodegeneration and/or dementia.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Change history
15 January 2023
Missing Open Access funding information has been added in the Funding Note.
Abbreviations
- AD:
-
Alzheimer’s dementia
- eGFR:
-
Estimated glomerular filtration rate
- HF:
-
Heart failure
- LAVI:
-
Left atrial volume index
- NfL:
-
Neurofilament light chain
- pTau:
-
Phosphorylated tau protein
- WMH:
-
White matter hyperintensities
References
Breijyeh Z, Karaman R. Comprehensive review on Alzheimer’s disease: causes and treatment. Molecules. 2020;25(24):5789.
Zlokovic BV, Gottesman RF, Bernstein KE, Seshadri S, McKee A, Snyder H, et al. Vascular contributions to cognitive impairment and dementia (VCID): a report from the 2018 National Heart, Lung, and Blood Institute and National Institute of Neurological Disorders and Stroke Workshop. Alzheimers Dement. 2020;16(12):1714–33.
Knopman DS, Amieva H, Petersen RC, Chetelat G, Holtzman DM, Hyman BT, et al. Alzheimer disease. Nat Rev Dis Primers. 2021;7(1):33.
Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and Alzheimer disease: a population-based cohort study. Arch Intern Med. 2006;166(9):1003–8.
Manemann SM, Knopman DS, St Sauver J, Bielinski SJ, Chamberlain AM, Weston SA, et al. Alzheimer’s disease and related dementias and heart failure: a community study. J Am Geriatr Soc. 2022;70(6):1664–72.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Almeida OP, Garrido GJ, Beer C, Lautenschlager NT, Arnolda L, Flicker L. Cognitive and brain changes associated with ischaemic heart disease and heart failure. Eur Heart J. 2012;33(14):1769–76.
Kuhle J, Barro C, Andreasson U, Derfuss T, Lindberg R, Sandelius A, et al. Comparison of three analytical platforms for quantification of the neurofilament light chain in blood samples: ELISA, electrochemiluminescence immunoassay and Simoa. Clin Chem Lab Med. 2016;54(10):1655–61.
Steinacker P, Anderl-Straub S, Diehl-Schmid J, Semler E, Uttner I, von Arnim CAF, et al. Serum neurofilament light chain in behavioral variant frontotemporal dementia. Neurology. 2018;91(15):e1390–e401.
Mattsson N, Andreasson U, Zetterberg H, Blennow K, Alzheimer’s Disease Neuroimaging I. Association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol. 2017;74(5):557–66.
van der Ende EL, Meeter LH, Poos JM, Panman JL, Jiskoot LC, Dopper EGP, et al. Serum neurofilament light chain in genetic frontotemporal dementia: a longitudinal, multicentre cohort study. Lancet Neurol. 2019;18(12):1103–11.
Khalil M, Pirpamer L, Hofer E, Voortman MM, Barro C, Leppert D, et al. Serum neurofilament light levels in normal aging and their association with morphologic brain changes. Nat Commun. 2020;11(1):812.
Benussi A, Karikari TK, Ashton N, Gazzina S, Premi E, Benussi L, et al. Diagnostic and prognostic value of serum NfL and p-Tau181 in frontotemporal lobar degeneration. J Neurol Neurosurg Psychiatry. 2020;91(9):960–7.
Barthelemy NR, Horie K, Sato C, Bateman RJ. Blood plasma phosphorylated-tau isoforms track CNS change in Alzheimer’s disease. J Exp Med. 2020;217(11):e20200861.
Mielke MM, Hagen CE, Xu J, Chai X, Vemuri P, Lowe VJ, et al. Plasma phospho-tau181 increases with Alzheimer’s disease clinical severity and is associated with tau- and amyloid-positron emission tomography. Alzheimers Dement. 2018;14(8):989–97.
Frey A, Homola GA, Henneges C, Muhlbauer L, Sell R, Kraft P, et al. Temporal changes in total and hippocampal brain volume and cognitive function in patients with chronic heart failure-the COGNITION.MATTERS-HF cohort study. Eur Heart J. 2021;42(16):1569–78.
Frey A, Sell R, Homola GA, Malsch C, Kraft P, Gunreben I, et al. Cognitive deficits and elated brain lesions in patients with chronic heart failure. JACC Heart Fail. 2018;6(7):583–92.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975.
Geiger J, Both S, Kircher S, Neumann M, Rosenwald A, Jahns R. Hospital-integrated biobanking as a service – the Interdisciplinary Bank of Biomaterials and Data Wuerzburg (IBDW). Open J Bioresour. 2018;5.
Halbgebauer S, Steinacker P, Verde F, Weishaupt J, Oeckl P, von Arnim C, et al. Comparison of CSF and serum neurofilament light and heavy chain as differential diagnostic biomarkers for ALS. J Neurol Neurosurg Psychiatry. 2022;93(1):68–74.
Kim JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. 2019;72(6):558–69.
Kac PR, Gonzalez-Ortiz F, Simren J, Dewit N, Vanmechelen E, Zetterberg H, et al. Diagnostic value of serum versus plasma phospho-tau for Alzheimer’s disease. Alzheimers Res Ther. 2022;14(1):65.
**ao Z, Wu X, Wu W, Yi J, Liang X, Ding S, et al. Plasma biomarker profiles and the correlation with cognitive function across the clinical spectrum of Alzheimer’s disease. Alzheimers Res Ther. 2021;13(1):123.
Ramani S, Berard JA, Walker LAS. The relationship between neurofilament light chain and cognition in neurological disorders: a sco** review. J Neurol Sci. 2021;420:117229.
Karikari TK, Ashton NJ, Brinkmalm G, Brum WS, Benedet AL, Montoliu-Gaya L, et al. Blood phospho-tau in Alzheimer disease: analysis, interpretation, and clinical utility. Nat Rev Neurol. 2022;18(7):400–18.
Thijssen EH, La Joie R, Wolf A, Strom A, Wang P, Iaccarino L, et al. Diagnostic value of plasma phosphorylated tau181 in Alzheimer’s disease and frontotemporal lobar degeneration. Nat Med. 2020;26(3):387–97.
Barro C, Benkert P, Disanto G, Tsagkas C, Amann M, Naegelin Y, et al. Serum neurofilament as a predictor of disease worsening and brain and spinal cord atrophy in multiple sclerosis. Brain. 2018;141(8):2382–91.
Kang MS, Aliaga AA, Shin M, Mathotaarachchi S, Benedet AL, Pascoal TA, et al. Amyloid-beta modulates the association between neurofilament light chain and brain atrophy in Alzheimer’s disease. Mol Psychiatry. 2021;26(10):5989–6001.
Elder GJ, Mactier K, Colloby SJ, Watson R, Blamire AM, O’Brien JT, et al. The influence of hippocampal atrophy on the cognitive phenotype of dementia with Lewy bodies. Int J Geriatr Psychiatry. 2017;32(11):1182–9.
Halliday G. Pathology and hippocampal atrophy in Alzheimer’s disease. Lancet Neurol. 2017;16(11):862–4.
Niizeki T, Iwayama T, Ikeno E, Watanabe M. Prognostic importance of hippocampal atrophy in patients with chronic heart failure. Am J Cardiol. 2019;123(7):1109–13.
Wardlaw JM, Valdes Hernandez MC, Munoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015;4(6):001140.
Puzo C, Labriola C, Sugarman MA, Tripodis Y, Martin B, Palmisano JN, et al. Independent effects of white matter hyperintensities on cognitive, neuropsychiatric, and functional decline: a longitudinal investigation using the National Alzheimer’s Coordinating Center Uniform Data Set. Alzheimers Res Ther. 2019;11(1):64.
Walsh P, Sudre CH, Fiford CM, Ryan NS, Lashley T, Frost C, et al. The age-dependent associations of white matter hyperintensities and neurofilament light in early- and late-stage Alzheimer’s disease. Neurobiol Aging. 2021;97:10–7.
Lee EJ, Lim YM, Kim S, Choi L, Kim H, Kim K, et al. Clinical implication of serum biomarkers and patient age in inflammatory demyelinating diseases. Ann Clin Transl Neurol. 2020;7(6):992–1001.
Korley FK, Goldstick J, Mastali M, Van Eyk JE, Barsan W, Meurer WJ, et al. Serum NfL (neurofilament light chain) levels and incident stroke in adults with diabetes mellitus. Stroke. 2019;50(7):1669–75.
Lue LF, Pai MC, Chen TF, Hu CJ, Huang LK, Lin WC, et al. Age-dependent relationship between plasma Abeta40 and Abeta42 and total tau levels in cognitively normal subjects. Front Aging Neurosci. 2019;11:222.
Jaworski J, Psujek M, Bartosik-Psujek H. Total-tau and phospho-tau(181Thr) in cerebrospinal fluid of neurologically intact population increase with age. Folia Biol (Praha). 2009;55(4):126–31.
Akamine S, Marutani N, Kanayama D, Gotoh S, Maruyama R, Yanagida K, et al. Renal function is associated with blood neurofilament light chain level in older adults. Sci Rep. 2020;10(1):20350.
Wilczynski GM, Engel WK, Askanas V. Cyclin-dependent kinase 5 colocalizes with phosphorylated tau in human inclusion-body myositis paired-helical filaments and may play a role in tau phosphorylation. Neurosci Lett. 2000;293(1):33–6.
Acknowledgements
We thank the multidisciplinary Cognition.Matters-HF team for the excellent support in the conduct of this comprehensive study.
Funding
This publication was supported by the Open Access Publication Fund of the University of Wuerzburg. This work was supported by grants from the Bundesministerium für Bildung und Forschung [01EO1004 and 01EO1504] through the Comprehensive Heart Failure Center, habilitation grant (AF), and UNION-CVD Clinician Scientist Program grant (413657723; JT) by the Interdisciplinary Center of Clinical Research Würzburg. CM, SF and AF were funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation, project number: 453989101). Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
AF, GS, and SS conceptualized the study. JT wrote the manuscript and drafted the illustrations. MO, RS, DG, GH, PS, PO, CM, SF, and MP read and contributed to the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Cognition.Matters-HF was conducted in compliance with the Declaration of Helsinki and approved by the local ethics committee of the University of Würzburg (#245/10) [17], and written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Methods. Table S1.
Inclusion and exclusion criteria. Table S2. Outcome of the cognitive test battery. Table S3. Imaging protocol and sequence parameters. Table S4. Correlation of biomarkers to cognitive domains and brain morphology. Table S5. Extended clinical characteristics of NfL quartiles. Table S6. Extended clinical characteristics of pTau quartiles. Table S7. Mediation analysis of parameters affecting serum levels of Ln(NfL). Table S8. Mediation analysis of parameters affecting serum levels of Ln(pTau). Table S9. Regression analysis of visual/verbal memory T-score with NfL. Table S10. Regression analysis of visual/verbal memory T-score with pTau. Table S11. Regression analysis of selectivity of attention T-score with pTau. Table S12. Regression analysis of cerebral atrophy. Table S13. Regression analysis of hippocampal atrophy. Table S14. Regression analysis of Ln (WMH volume). Figure S1. Histograms of serum NfL and pTau.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Traub, J., Otto, M., Sell, R. et al. Serum phosphorylated tau protein 181 and neurofilament light chain in cognitively impaired heart failure patients. Alz Res Therapy 14, 149 (2022). https://doi.org/10.1186/s13195-022-01087-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-022-01087-4