Abstract
Background
The experiences of biomarker-ineligible cognitively normal persons can inform trial conduct and the translation of preclinical Alzheimer’s disease (AD) into clinical practice.
Methods
We interviewed 33 persons whose “not elevated” brain amyloid imaging biomarker result made them ineligible for a preclinical AD trial.
Results
Most participants (n = 17) reported being informed that they did not demonstrate adequately elevated amyloid to qualify, whereas some (n = 14) reported being told they had no amyloid or plaques. Relief (n = 17) and disappointment related to not being able to participate (n = 12) were the most common reactions to results. Nearly all participants would have made healthy lifestyle changes if they had received an “elevated” result, would have another scan, and would participate in another AD prevention trial.
Conclusions
Although some participants may misconstrue results, disclosure of a “not elevated” amyloid result in the research setting causes little behavior change; willingness to participate in AD research remains.
Similar content being viewed by others
Background
Increasing evidence supports a hypothesis that dementia due to Alzheimer’s disease (AD) is the end result of a long pathophysiological process that begins years before symptoms [1]. This asymptomatic or preclinical stage offers an opportunity to test disease-modifying therapies to delay the onset of cognitive and behavioral symptoms due to AD [2, 3].
To achieve feasibility, clinical trials in preclinical AD enroll and randomize to drug or placebo only persons meeting specific biomarker criteria [4]. Few data are available as yet that are related to the safety [5, 6] and impact [7] of biomarker disclosure in cognitively normal persons, and available reports have understandably focused on reactions among participants who qualify to enroll [8,9,10,11].
Disclosure of biomarker results in the clinical trial setting most frequently involves communication of negative results, such as not elevated brain amyloid and consequent ineligibility. Potential negative implications of this disclosure include misunderstanding and reduced motivation for optimal health behaviors [12,13,14]. The impact on willingness to participate in future trials is unknown. To explore the implications of communicating negative biomarker results to cognitively normal individuals, we performed telephone interviews with participants who screen failed for a preclinical AD trial due to inadequate brain amyloid deposition, as demonstrated through amyloid positron emission tomography (PET).
Methods
Participants
We interviewed individuals recruited to the Anti-Amyloid treatment in Asymptomatic AD (A4) study [15] at a single site. The A4 study enrolled individuals aged 65–85 years who were cognitively unimpaired (Mini Mental State Examination score 25 to 30, global Clinical Dementia Rating of 0, Logical Memory II score of 6 to 18) and had “elevated” brain amyloid as measured by amyloid PET. Eligible participants were randomized to receive the monoclonal antibody against amyloid beta, solanezumab, or placebo. Criteria for the current study were having screen failed for the A4 study due to a “not elevated” amyloid PET scan. We excluded those enrolled in the Longitudinal Evaluation of Amyloid Risk and Neurodegeneration (LEARN) study (n = 4), a prospective cohort study that follows a subset of participants who screen failed from A4 due to a not elevated amyloid PET result.
Disclosure process
In the A4 study, all participants underwent a systematic process to disclose amyloid PET results [16]. The process mandates that disclosure be performed by a trained and qualified investigator, that education be provided at consent, that PET imaging be performed on a separate day from consent and disclosure to ensure participants have the opportunity to change their minds, and that the safety of disclosure be monitored before and after imaging through standardized assessments of depression, anxiety, suicidality, and distress. Results are disclosed as “elevated” or “not elevated” amyloid.
An educational study brochure is used as a tool accompanying the disclosure process. The brochure, informed consent, and disclosure process emphasize that amyloid imaging does not equate to a diagnosis of AD, that quantitative information on the risk and timing of future cognitive impairment and AD dementia among those with elevated amyloid is not known, and that individuals with a “not elevated” scan result could someday develop elevated amyloid or AD dementia.
Data collection
An interview guide was developed that was based on the experiences of the investigative team in performing the disclosure process and the literature related to the potential positive and adverse consequences of biomarker disclosure [12, 13, 17,18,19,20]. Interviews included both forced choice and open-ended questions. Topics included expectations for the scan, impression of the disclosed PET result, meaning of the PET result, and what it would have meant to receive an elevated result. We used the Impact of Events Scale (IES) to assess distress associated with disclosure [21]. Participants were asked whether and why their study partner accompanied them to the disclosure visit. We asked participants with whom they subsequently shared their PET results. We assessed whether participants had made changes in health and planning behaviors since screening, including diet, exercise, prescription medications, vitamins or supplements, long-term care insurance, and advance healthcare directives. If participants responded affirmatively, we inquired about the types of changes that were made. If participants responded negatively, we confirmed that the factor was “exactly the same as it was before screening for the A4 study.” We next asked whether participants would have made changes in each factor if they had received an elevated PET result. Likert scales were used to assess participants’ willingness to repeat PET imaging and to enroll in another trial.
Data analyses
Quantitative data were entered into a Research Electronic Data Capture (REDCap) database and summarized with descriptive statistics. We calculated the Pearson correlation coefficient to examine for a relationship between IES score and time since disclosure. We used Grubbs’ test to assess for outliers.
Interviews were recorded, transcribed, and entered into qualitative analysis software (NVivo version 11.0; QSR International, Melbourne, Australia). Two of us (JDG and CGC) reviewed a subset of transcripts to identify preliminary themes and engaged in a consensus-building exercise to arrive at themes for interview coding. We double-coded interviews, adjusting themes as necessary and intermittently assessing interrater consistency. In the event of a Cohen κ coefficient for reliability < 0.8, interviews were reviewed for coding consistency, and consensus was achieved. At the conclusion of data coding, we performed a final consensus exercise to ensure consistency in participants coded for each given qualitative theme. The final Cohen κ was > 0.9. For each theme, we report the frequency count of codes within that theme.
Ethics
The University of California Irvine Institutional Review Board approved this study. Informed consent was performed telephonically and was acknowledged in writing by the investigator performing the study interviews.
Results
Participants
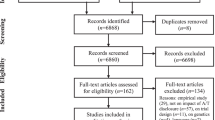
We interviewed 33 of 43 (77%) individuals eligible for this study. Seven individuals declined participation, and we were unable to reach three individuals after three attempts to contact them via telephone. Among those who declined, three were not interested, two were too busy, one had a family emergency, and one had a recent stroke. Participants interviewed were mostly white and highly educated, and about half reported a family history of dementia (Table 1). Interviews were performed between October 25, 2017, and December 12, 2017. The range of time between PET disclosure and study interview was 3–30 months (median, 20 months).
Meaning and impressions of PET results
Table 2 summarizes the types of responses participants gave when asked to describe their PET results, as disclosed by the A4 research team. The large majority of participants acknowledged that their results made them ineligible to continue in the A4 study. Just over half (n = 17) indicated that their amyloid result was “not elevated” or “not enough plaque.” Just under half (n = 14) reported being told that they had “no amyloid,” “no plaques,” or “clear scans.” For example, one 83-year-old female stated, “Um, in my own words I understood that I did not have any amyloids and my brain was clear. And that’s all I wanted to hear.”
Eight participants acknowledged that their scan results or risk for dementia could change in the future. Two participants indicated that they had been told they had inadequate neurofibrillary tangles to participate.
Reactions to PET results
The most common reaction to learning of a not elevated PET result was relief (n = 17). Twelve participants indicated that they were disappointed that they were not eligible to continue in the study (Table 3). One 67-year-old female stated, “Well, it was a relief on one hand, uh, to know that I didn’t have that condition. And then it was a little bit of a disappointment that I couldn’t be in the study. So, I guess it was more of a relief, but then I still wanted to know what I could do to help with finding a cure for the disease.”
Eleven participants indicated that they felt their risk for AD was reduced on the basis of their PET results; four indicated that they had no risk for AD. Twelve participants expected their PET results to be elevated, and eight expected the results they received; thirteen had no expectations. Two participants indicated a desire to learn more quantitative information about their PET results.
Distress due to PET results
IES scores of most participants (n = 31) at the time of interview were indicative of subclinical distress related to learning their PET results (Table 1). One score indicated mild distress, and one indicated moderate distress. There was a weak negative correlation between time since disclosure and IES score (r = − 0.17). Grubb’ test indicated the moderate distress score was an outlier (p < 0.05). After this case was removed, there was no relationship between time since disclosure and IES score (r = − 0.07).
Role of study partner
When asked about the involvement of the study partner in the disclosure visit, 14 participants indicated that their partner was present, whereas 19 indicated they received their results alone. When asked why they received their results alone, 12 indicated that the involvement of the partner was not necessary, 10 said that involving the partner in the disclosure visit would have been inconvenient, and 8 said that they were unaware that the partner could attend the disclosure visit. For example, a 70-year-old female reported, “I didn’t know that was an option. Otherwise, I would’ve included him. I wasn’t advised that I could bring someone. I don’t remember being advised. Maybe I was but I don’t remember it.” Four participants who had their partner present reported that the partner provided needed support during the disclosure visit. When the same individual was asked if she would have preferred that her partner be present for the disclosure visit, she responded, “Yes, I think so. Just to have a supportive person there.”
Sharing of PET results
Every participant shared his or her amyloid PET result with more than one other person, most commonly spouses (n = 29), adult children (n = 28), and friends (n = 28). Nineteen participants shared their results with their primary care physician. The reasons for sharing were to keep others in their lives informed about their health (n = 21), as a means to encourage others to participate in research studies (n = 9), to confirm their cognitive health to others (n = 8), and to provide relief to others in their lives, primarily family members (n = 5).
Health behaviors
None of the participants acknowledged making lifestyle changes deemed negative to health (e.g., reduced exercise or poorer diet) since learning their PET results. A few (n = 5) indicated that they had made positive changes in health behaviors as a result of heightened sensitivity to brain health. Nearly all participants indicated that they would have made a lifestyle change had their scan results been elevated, including changing their diet (n = 25), exercise (n = 24), prescription medications (n = 22), and vitamins or supplements (n = 24).
Planning behaviors
Half of participants already had long-term care insurance (n = 16), and nearly all had an advance directive in place (n = 32). Seven participants lacking long-term care insurance indicated they would have made a change had their results been elevated. The participant without an advance directive indicated she would have established one had her result been elevated. Of participants with advance directives, six would have made changes had their scan results been elevated. Though most did not describe a specific change, two indicated they would have altered choices related to life-sustaining therapy and do-not-resuscitate orders.
Future trial participation
When asked the likelihood of participating in another AD prevention trial, some participants indicated that they would be very (n = 21) or somewhat (n = 12) likely to do so. The comments by one 66-year-old female are representative of those of the other participants: “Very likely. I had a good experience with as far as I got with the first one. So, another opportunity to do something slightly different would uh, I’d be very happy to participate.”
Nearly every participant (n = 30) indicated that they would be very (n = 21) or somewhat (n = 9) likely to undergo another amyloid PET scan if given the opportunity. Table 4 outlines themes of participant reasons for and against undergoing repeat amyloid imaging. Reasons to repeat testing outnumbered reasons not to and included to assess for change in amyloid status, to help with research, to learn AD risk, and curiosity. Reasons not to undergo repeat testing included negative experiences or discomfort with imaging and feeling that additional testing was unnecessary.
Discussion
Clinical trials frequently disclose AD biomarker results to cognitively normal individuals. Disclosure processes focus on educating potential subjects about what is known and not known about amyloid imaging, minimizing negative reactions, and ensuring the safety of those who are informed that AD biomarkers are present [16, 22]. Better understanding of the impact of learning a “negative” result is needed, given that this will be the most common type of information disclosed in future trials and ultimately in large public health screening campaigns when effective therapies are developed. This study of individuals who learned they did not have an elevated amyloid result shows how trial participants understood, reacted to, and used this information as well as whether they would participate in another study.
A majority of participants reported that they were informed they had insufficient amyloid to qualify for the trial, but nearly half of participants described a result that was different from the A4 disclosure materials (Table 2). These participants reported being told they had no amyloid or plaques in the brain. Similarly, only a few participants acknowledged that the results of their amyloid PET scan could change over time. These findings may reinforce the need to emphasize before and after disclosure that an amyloid PET result can change.
Other potential improvements to the disclosure process include a greater focus on who can be present. Some participants were unaware that their study partner could join them at the disclosure visit. The role of the study partner in this process, and in preclinical AD trials more broadly, remains an area of active study [23, 24]. Although most participants in this study felt that the presence of the partner during disclosure was unnecessary, a smaller portion felt that the partner provided needed support. Sixteen participants indicated that they would have felt concern or distress had they received an elevated result (data not shown). In this scenario, support from a study partner might have been valuable to them. Optimizing the process of disclosure, including ensuring that participants have adequate support to cope with results, will be necessary to ensure the safety and satisfaction of future trial participants.
Only two participants voiced a desire to learn more information about their disclosed result (Table 3). This is in contrast to a recent study of individuals with elevated amyloid in which 40% voiced displeasure with not receiving more information about their PET result [7]. Quantitative biomarker results are not provided in preclinical AD trials, in part because the optimal thresholds for identifying those at greatest risk for cognitive decline are uncertain [25, 26]. Given this, the criteria for biomarker eligibility may change in future preclinical AD trials. Our results indicate that people who fail screening on the basis of biomarker test results will be likely to participate in additional trials if invited. In fact, most were interested in undergoing repeat amyloid imaging, for reasons including curiosity, desire to learn about changes in risk for AD dementia, and desire to contribute to research.
Ongoing research seeks to assess the safety of AD biomarker disclosure, with preliminary studies indicating disclosure does not cause clinical depression or anxiety [6]. Not surprisingly, the majority of participants in this study did not experience distress in response to learning their biomarker results. One participant, however, did experience intrusive thoughts related to the disclosure process and scored in the moderate range on the IES. Specifically, this participant communicated concerns regarding not asking for or receiving enough information about the result and worry that the result could change in the future. It is possible her reaction resulted from subjective cognitive complaints left unexplained. This would be consistent with previously reported feelings of ambiguity and frustration among participants with mild cognitive impairment (MCI) in response to a test that fails to provide additional diagnostic information when symptoms are present [27, 28]. Nevertheless, the most common reaction to the disclosed information in this sample, as in studies of MCI [27], was relief. Notably, the second most common reaction was disappointment in not being able to contribute to the study.
Few people used their amyloid PET scan results to change behavior. None used the disclosed information to justify adoption of unhealthy lifestyle choices. A few developed a heightened sensitivity to issues of brain health and initiated or improved behaviors, such as eating a healthier diet or exercising more. Most, however, made no lifestyle changes. Nearly all speculated that they would have changed their behavior had their result shown elevated amyloid. These preliminary results are important to future screening campaigns, suggesting that in the setting of a substantive education program, the risk for people using screening information to justify unhealthy lifestyle choices (e.g., greater consumption of high-fat or high cholesterol foods, reduced exercise), which could increase risk for future cognitive impairment [29], may be low. But people may also be less motivated to adopt healthy behaviors. Based on current understanding and available prevention strategies [30], the recommendations for lifestyle and medical choices are no different for individuals who do or do not demonstrate elevated amyloid. All individuals undergoing screening should be educated and empowered to adopt risk-reducing lifestyle strategies.
Learning that they have increased risk of develo** AD dementia due to elevated amyloid may cause some individuals to set up advance healthcare directives and other medicolegal arrangements such as living wills [14]. Reduced motivation to complete such arrangements due to biomarker outcomes could have negative implications, especially for individuals who are at high risk for other causes of late-life disability, such as stroke or myocardial infarction, even if their risk for AD is relatively lower. A high proportion of participants in this study had advance healthcare directives and long-term care insurance. Seven of 17 participants without long-term care insurance indicated they would have established a policy had they received an elevated PET result. The one participant who did not have an advance healthcare directive indicated that she would have established one had her result been elevated. Collectively, these findings indicate the need for future trials to further emphasize medicolegal recommendations for study participants, regardless of the outcome of biomarker testing.
Limitations of this study include that participants were recruited from a single site, where a single investigator primarily performed the disclosure process. The homogenous sample may not be representative of participant reactions to negative amyloid imaging results delivered across a large multisite trial by multiple investigators, let alone outside the research setting. Assessment of site heterogeneity in disclosure processes and effects on participant responses will be an important area of future research. Participants were predominantly white, female, and highly educated, potentially limiting generalizability to different groups. Whether the ten eligible individuals who we were unable to reach or who declined participation responded differently to learning their amyloid PET results than those who did participate is unknown. There was a wide range in the durations between disclosure and data collection. This could have introduced a confounding variable if, for example, emotional reactions to learning a PET result change over time. The variability in time since disclosure may also have caused heterogeneity in the accuracy of reported experiences.
Conclusions
These results suggest that the disclosure process in the A4 study was effective and safe in ineligible participants, though important opportunities to improve the process may exist. Disclosure did not result in adoption of unhealthy behaviors among participants; however, most indicated that there were risk-reducing strategies that they would have implemented had they received an elevated result. Communicating the need to adopt such strategies to all participants will be important in future preclinical AD trials, as well as in future public health campaigns that aim to identify appropriate candidates for disease-delaying therapies.
References
Donohue MC, Sperling RA, Petersen R, Sun CK, Weiner MW, Aisen PS, Alzheimer’s Disease Neuroimaging Initiative. Association between elevated brain amyloid and subsequent cognitive decline among cognitively normal persons. JAMA. 2017;317(22):2305–16.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM, Iwatsubo T, Jack CR Jr, Kaye J, Montine TJ, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92.
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, DeKosky ST, Gauthier S, Selkoe D, Bateman R, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13(6):614–29.
Burns JM, Klunk WE. Predicting positivity for a new era of Alzheimer disease prevention trials. Neurology. 2012;79(15):1530–1.
Lim YY, Maruff P, Getter C, Snyder PJ. Disclosure of positron emission tomography amyloid imaging results: a preliminary study of safety and tolerability. Alzheimers Dement. 2016;12(4):454–8.
Burns JM, Johnson DK, Liebmann EP, Bothwell RJ, Morris JK, Vidoni ED. Safety of disclosing amyloid status in cognitively normal older adults. Alzheimers Dement. 2017;13(9):1024–30.
Mozersky J, Sankar P, Harkins K, Hachey S, Karlawish J. Comprehension of an elevated amyloid positron emission tomography biomarker result by cognitively normal older adults. JAMA Neurol. 2018;75(1):44–50.
Bemelmans SA, Tromp K, Bunnik EM, Milne RJ, Badger S, Brayne C, Schermer MH, Richard E. Psychological, behavioral and social effects of disclosing Alzheimer’s disease biomarkers to research participants: a systematic review. Alzheimers Res Ther. 2016;8(1):46.
Molinuevo JL, Cami J, Carne X, Carrillo MC, Georges J, Isaac MB, Khachaturian Z, Kim SY, Morris JC, Pasquier F, et al. Ethical challenges in preclinical Alzheimer’s disease observational studies and trials: results of the Barcelona summit. Alzheimers Dement. 2016;12(5):614–22.
Vanderschaeghe G, Schaeverbeke J, Bruffaerts R, Vandenberghe R, Dierickx K. From information to follow-up: Ethical recommendations to facilitate the disclosure of amyloid PET scan results in a research setting. Alzheimers Dement (N Y). 2018;4:243–51.
de Wilde A, van Buchem MM, Otten RHJ, Bouwman F, Stephens A, Barkhof F, Scheltens P, van der Flier WM. Disclosure of amyloid positron emission tomography results to individuals without dementia: a systematic review. Alzheimers Res Ther. 2018;10(1):72.
Roberts JS, Dunn LB, Rabinovici GD. Amyloid imaging, risk disclosure and Alzheimer’s disease: ethical and practical issues. Neurodegener Dis Manag. 2013;3(3):219–29.
Grill JD, Johnson DK, Burns JM. Should we disclose amyloid imaging results to cognitively normal individuals? Neurodegener Dis Manag. 2013;3(1):43–51.
Sheffrin M, Stijacic Cenzer I, Steinman MA. Desire for predictive testing for Alzheimer’s disease and impact on advance care planning: a cross-sectional study. Alzheimers Res Ther. 2016;8(1):55.
Sperling RA, Rentz DM, Johnson KA, Karlawish J, Donohue M, Salmon DP, Aisen P. The A4 study: stop** AD before symptoms begin? Sci Transl Med. 2014;6(228):228fs213.
Harkins K, Sankar P, Sperling R, Grill JD, Green RC, Johnson KA, Healy M, Karlawish J. Development of a process to disclose amyloid imaging results to cognitively normal older adult research participants. Alzheimers Res Ther. 2015;7(1):26.
Lingler JH, Klunk WE. Disclosure of amyloid imaging results to research participants: has the time come? Alzheimers Dement. 2013;9(6):741–4 e2.
Leuzy A, Zimmer ER, Heurling K, Rosa-Neto P, Gauthier S. Use of amyloid PET across the spectrum of Alzheimer’s disease: clinical utility and associated ethical issues. Amyloid. 2014;21(3):143–8.
Arias JJ, Karlawish J. Confidentiality in preclinical Alzheimer disease studies: when research and medical records meet. Neurology. 2014;82(8):725–9.
Karlawish J. Addressing the ethical, policy, and social challenges of preclinical Alzheimer disease. Neurology. 2011;77(15):1487–93.
Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–18.
Lingler JH, Butters MA, Gentry AL, Hu L, Hunsaker AE, Klunk WE, Mattos MK, Parker LA, Roberts JS, Schulz R. Development of a standardized approach to disclosing amyloid imaging research results in mild cognitive impairment. J Alzheimers Dis. 2016;52(1):17–24.
Grill JD, Karlawish J. Study partners should be required in preclinical Alzheimer’s disease trials. Alzheimers Res Ther. 2017;9(1):93.
Largent EA, Karlawish J, Grill JD. Study partners: essential collaborators in discovering treatments for Alzheimer’s disease. Alzheimers Res Ther. 2018;10(1):101.
Landau SM, Horng A, Jagust WJ, Alzheimer’s Disease Neuroimaging Initiative. Memory decline accompanies subthreshold amyloid accumulation. Neurology. 2018;90(17):e1452–60.
Leal SL, Lockhart SN, Maass A, Bell RK, Jagust WJ. Subthreshold amyloid predicts tau deposition in aging. J Neurosci. 2018;38(19):4482–9.
Grill JD, Cox CG, Kremen S, Mendez MF, Teng E, Shapira J, Ringman JM, Apostolova LG. Patient and caregiver reactions to clinical amyloid imaging. Alzheimers Dement. 2017;13(8):924–32.
Beard RL, Neary TM. Making sense of nonsense: experiences of mild cognitive impairment. Sociol Health Illn. 2013;35(1):130–46.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–28.
Leshner AI, Landis S, Stroud C, Downey A. Preventing cognitive decline and dementia: a way forward. Washington, DC: National Academies Press; 2017.
Acknowledgements
We thank the participants in this study for their time and contributions. We thank Guerry Peavy for comments on a draft of the manuscript.
Funding
The A4 study is a public-private partnership funded in part by the National Institute on Aging and Eli Lilly. JDG and CGC are funded by National Institutes of Health grant AG016573.
Availability of data and materials
Interviews, guides, and raw data are available upon request from the corresponding author.
Author information
Authors and Affiliations
Contributions
JDG, CGC, KH, and JK all contributed to the design of the study, were involved in drafting the manuscript and revising it critically for important intellectual content, and gave final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of University of California, Irvine. All participants gave telephonic informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Grill, J.D., Cox, C.G., Harkins, K. et al. Reactions to learning a “not elevated” amyloid PET result in a preclinical Alzheimer’s disease trial. Alz Res Therapy 10, 125 (2018). https://doi.org/10.1186/s13195-018-0452-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-018-0452-1