Abstract
Objective
Mutational analysis of BCR::ABL1 kinase domain (KD) is a crucial component of clinical decision algorithms for chronic myeloid leukemia (CML) patients with failure or warning responses to tyrosine kinase inhibitor (TKI) therapy. This study aimed to detect BCR::ABL1 KD mutations in CML patients with treatment resistance and assess the concordance between NGS (next generation sequencing) and Sanger sequencing (SS) in detecting these mutations.
Results
In total, 12 different BCR::ABL1 KD mutations were identified by SS in 22.6% (19/84) of patients who were resistant to TKI treatment. Interestingly, NGS analysis of the same patient group revealed an additional four different BCR::ABL1 KD mutations in 27.4% (23/84) of patients. These mutations are M244V, A344V, E355A, and E459K with variant read frequency below 15%. No mutation was detected in 18 patients with optimal response to TKI therapy. Resistance to TKIs is associated with the acquisition of additional mutations in BCR::ABL1 KD after treatment with TKIs. Additionally, the use of NGS is advised for accurately determining the mutation status of BCR::ABL1 KD, particularly in cases where the allele frequency is low, and for identifying mutations across multiple exons simultaneously. Therefore, the utilization of NGS as a diagnostic platform for this test is very promising to guide therapeutic decision-making.
Similar content being viewed by others
Introduction
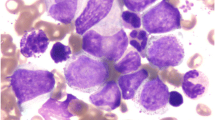
Chronic myeloid leukemia (CML) is a clonal myeloproliferative neoplasm characterized by the presence of the Philadelphia (Ph) chromosome derived from a reciprocal translocation between chromosome 9 and 22 (t(9;22)(q34;q11) to produce BCR::ABL1 oncogene [1, 2]. Imatinib mesylate (IM) was the first BCR::ABL1 tyrosine kinase inhibitor (TKI) approved as first-line therapy for CML due to its superior result in terms of response rates, progression-free and overall survival compared with the previous treatment options [3]. Despite the remarkable achievement of TKI therapy, 20–30% of patients developed a primary or secondary resistance to treatment during the disease course [4]. The most frequently described mechanism associated with resistance is the occurrence of point mutations in the BCR::ABL1 gene [5,6,7,8,9]. Therefore, after the emergence of resistance and factors such as low compliance and inadequate dosing are excluded, BCR::ABL1 KD mutation testing is indicated as per the recommendations of both ELN (European LeukemiaNet) and NCCN (National Comprehensive Cancer Network) [10,11,12,13].
Sanger sequencing (SS) is the recommended method for detecting BCR::ABL1 KD mutation because of its high efficiency and accuracy [14]. However, the analytic sensitivity of this method is limited, with the detection of 15–20% mutations in the wild-type background [13, 15]. Hence, there is a need to explore other methods such as NGS (next generation sequencing), which offer advantages in sensitivity, throughput and accuracy to determine BCR::ABL1 KD mutations. This study aimed to detect BCR::ABL1 KD mutations in CML patients with treatment resistance and assess the concordance between NGS and SS in detecting these mutations.
Methods
Participants and setting
This cross-sectional study was conducted on samples from CML patients with TKI resistance and those exhibiting optimal responses to TKI treatment. This study included samples from CML patients who received treatment with either imatinib or a second-generation TKI such as nilotinib or dasatinib. Samples from patients with Ph-positive (Ph+) acute lymphoblastic leukemia (ALL), patients with atypical CML and those on non-TKI therapy were excluded from this study.
The response to TKI therapy is defined according to European LeukemiaNet guidelines [11]. Patients with TKI resistance or treatment failure were those who failed to achieve a complete hematological response (CHR), complete cytogenetic response (CCR) and major molecular response (MMR) during treatment. Optimal responders were those who attained MMR BCR::ABL1 ≤ 1% and ≤ 0.1% at 6 and 12 months of TKI therapy, respectively. CHR was characterized by the normalization of peripheral blood counts, and the disappearance of palpable splenomegaly. CCR indicated the absence of Ph + cells in the karyotype. MMR or MR3 was defined as a BCR::ABL1 IS (International Scale) transcript level ≤ 0.1%. MR4 and MR4.5 were defined as BCR::ABL1 IS ≤ 0.01% and ≤ 0.0032% respectively.
Samples from the TKI-resistant group were identified from those received by the Diagnostic Laboratory Haematology at Institute for Medical Research (IMR), National Institute of Health (NIH) from January 2017 to December 2020. All samples in this group had previously undergone Sanger sequencing at the Diagnostic Laboratory Haematology, which was the referral laboratory in the country for routine SS to detect BCR::ABL1 KD mutations. TKI responders patients were selected from the Pathology Laboratory at Hospital Tunku Azizah from January 2019 to December 2020. The Pathology Laboratory commonly received samples and conducted the detection and quantification of BCR::ABL1 transcripts at the time of diagnosis or during follow-up for CML patients.
Sample size estimation
The sample size for the study was determined using the OpenEpi software [16]. Based on the prevalence of BCR::ABL1 mutations in previous studies (22.7% [17], 22.4% [18] and 32.5% [19] in CML patients with imatinib resistance in Malaysia, a prevalence of 22.4% was considered. Accordingly, considering confidence interval at 95% and marginal error of 5%, a minimum number of 80 samples was required for this study.
cDNA synthesis
The archived RNA was quantified and checked for quality using NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific). RNA was previously extracted using the QIAamp RNA Blood Mini kit (Qiagen). Then, total cellular RNA (1 µg/µl) was reverse transcribed to cDNA using SuperScript IV First Strand Synthesis System (Thermo Fisher Scientific).
Mutational analysis of BCR::ABL1 KD by Sanger sequencing
Sanger sequencing was performed upon double-step PCR amplification of the BCR::ABL1 KD. The first-round amplification was performed using a forward primer on exon 12/13 of the BCR gene and a reverse primer on exon 10 of the ABL1-R gene. A 0.5 µl of the first PCR product was used as a template in second amplification of PCR. The ABL1 KD was amplified using three partially overlap** fragments, using set of primer that covers exon 4 until exon 10 ABL1 gene [20].
Sanger sequencing was performed on ABI3730XL 96 capillary Genetic Analyzer using BigDye® Terminator v3.1 Cycle Sequencing kit. The obtained sequences were visualized and aligned with Genbank reference sequence NM_005157.5 using CLC Main Workbench, version 7.0.2 (Qiagen).
Mutational analysis of BCR::ABL1 KD by next-generation sequencing
Semi-nested PCR was performed to amplify the BCR::ABL1 allele and followed by another PCR for ABL1 KD amplification using appropriate primers [20]. A total of 400ng of each purified PCR product was used as input for tagmentation and library preparation using the Illumina DNA Prep kit as per manufacturer instructions. The library was normalized to 2 nM and pooled for sequencing on an Illumina MiSeq. The FASTQ files generated were then uploaded to Illumina BaseSpace Sequence Hub (BSSH). These files were analyzed using DRAGEN RNA (Illumina Inc.) and produced an output VCard File (VCF) file for downstream analysis. The details of methodology for NGS are provided in the supplemental Methods.
Results
This study includes 84 CML patients who either do not respond or have lost their response to TKI therapy, as well as 18 CML patients who have achieved stable optimal responses to TKI therapy. The characteristics of patients are listed in Table 1.
Detection of BCR::ABL1 KD mutation
In total, 12 different BCR::ABL1 KD mutations were identified in 22.6% (19/84) of patients who were resistant to TKI treatment by SS (Fig. 1). NGS resulted in the detection of 16 different missense mutations in 27.4% (23/84) of TKI resistant patients (Fig. 2). Among the TKI-resistant patients, 14 carried one mutation, while 9 carried more than one mutation. NGS identified all true high-frequency mutations (> 15% frequency) found by SS and additional four low-frequency mutations (3 to 15% frequency). The additional mutations identified by NGS are M244V, A344V, E355A, and E459K (Table S1). No mutation was detected in patients with optimal response to TKI therapy by SS and NGS method.
Variant classification
Variants p.M244V, p.G250E, p.Y253H, p.E255K, p.T315I, p.F317L, p.E355G, p.F359C, and p.F359V have been classified as pathogenic/likely pathogenic by ClinVar. These mutations have a phenotypic association with CML and lymphoblastic leukemia. Notably, variant p.F317L identified in this study has two different nucleotide changes, c.949T > C and c.951 C > A. The variant p.F317L with nucleotide change c.951 C > A was classified as likely pathogenic while variant c.949T > C p.F317L was classified as VUS by ClinVar. Notably, six mutations (p.L387M, p.E453K, p.E459K, p.A344V, p.E355A, and p.K357T) identified in this study were not documented in ClinVar.
In addition, Table 2 presents a list of mutations identified in current research and their corresponding sensitivity levels to the approved TKIs based on the previous study [12, 21,22,23,24,25,26,27,28,29,30,31,32,33]. The degree of sensitivity of mutations p.A344V, p.E355A, p.K357T, and p.E453K to TKI treatment has not been well established in clinical studies. Therefore, resistance profiles of these mutations were predicted using the web-based tool, SUSPECT-ABL (https://biosig.lab.uq.edu.au/suspect_abl/) [34]. Upon testing, all mutations were determined to be susceptible to imatinib, exhibiting change in protein stability, ddG (Delta Delta G) values of 0.19 for p.A344V, 0.28 for p.E355A, 0.19 for p.K357T and 0.37 for p.E453K. Figure 3 shows the locations of mutations and imatinib in ABL kinase domain.
Discussion
In this study, we described the development of laboratory assays using PCR and NGS-based approaches for BCR::ABL1 KD mutation detection. The NGS amplicon sequencing involves generating libraries from PCR products, pooled and subsequently sequenced on the Illumina MiSeq platform.
NGS assay identified 16 different BCR::ABL1 KD mutations in 27.4% (23/84) TKI-resistant patients. The variants detected at a frequency of 20% and above within BCR::ABL1 transcripts were categorized as ‘high-level’. In contrast, variants detected at a frequency less than 20% but greater than or equal to 3% of BCR::ABL1 transcripts were classified as ‘low-level’ [35]. In this study, Sanger sequencing was able to detect mutations with variant read frequency of more than 15%, therefore, identified 12 different mutations in 22.6% (19/84) TKI-resistant patients.
The current investigation shows the frequency of mutations by NGS detection in TKI-resistant patients is lower than in other studies, as reported 80% by Soverini et al. in 2016 [35], 33% by Duong et al. in 2017 [36], 59% by Erbilgin et al. in 2019 [37] and 30.9% by Liu et al. in 2020 [38]. According to a previous study by Kim et al. (2009), the proportion of patients in each phase of CML disease could affect the rate of mutations. The study found that a significant number of patients (63%) had BCR::ABL1 KD mutations, which could be attributed to the high number of patients in the advanced phase (35% in the accelerated phase and 40% in the blast phase) [39]. Therefore, the large portion of patients in the chronic phase included in this study (66.7%) could explain the lower mutation rate compared with other studies. The research conducted on identifying BCR::ABL1 KD mutation in Malaysian patients who are resistant to IM treatment was recorded at 22.4% [18], 22.7% [17], and 32.5% [19], which were consistent with our study. These previous studies have employed dHPLC followed by direct DNA sequencing as a mutation detection method.
The most common mutations type found in TKI-resistant patients by NGS detection were p.Y253H, p.T315I, p.E255K, and p.F359V. The occurrence of the mutations in the present study was reported as follows: p.Y253H in 8.3%, p.T315I in 7.1%, p.E255K in 4.8%, and p.F359V in 4.8%. The previous study conducted on the detection of BCR::ABL1 KD mutations by NGS reported that p.Y253H mutation occurs in 8.2–14.4%, p.T315I in 4.1–23%, p.E255K in 4.1–10% and p.F359V in 5.6–6.6% which was comparable to the results obtained in the current study [35, 36, 38]. Among TKI-resistant patients in the present study, 9 individuals were found to have multiple mutations. Multiple mutations may reflect either polyclonal or compound mutations [40]. Previous studies have reported that multiple mutations were associated with worse outcomes and poor molecular response [29, 40, 41].
The majority of mutations identified in this study are situated distally from the imatinib-binding site (Fig. 3), making it challenging to explain their resistance mechanism. A new machine learning-based tool called SUSPECT-ABL is utilized to assess mutations with unknown effects on TKIs. These mutations were predicted to be susceptible to imatinib, which aligns with their location further away from the drug-binding site (Fig. 3). In contrast, clinically resistant mutations tend to cluster around imatinib (Fig. 3). Despite showing superior performance compared to other machine learning and molecular dynamics-based prediction [34], accuracy of SUSPECT-ABL is primarily high for residues in close proximity to imatinib. This highlights the limitations of current in silico tools and underscores the need to employ a better predictor for drug efficacy beyond measuring drug affinity alone.
In summary, the result of this study demonstrates that NGS is more sensitive than Sanger sequencing method for detecting BCR::ABL1 KD mutations in CML patients, thus emphasizing the crucial role of NGS assays in advancing the understanding of mutation-associated TKI resistance in CML. The flexibility and capacity to assess multiple targets in a single run render NGS a valuable tool, considering its potential to revolutionize the detection and characterization of mutations in CML. Moreover, these findings indicate that integrating NGS into clinical practice has the potential to significantly impact therapeutic decision-making, ultimately leading to improved patient outcomes in the management of CML.
Limitation
The current study could not prove that NGS able to detect emerging BCR::ABL1 KD mutations earlier than Sanger sequencing. The present study also was not able to distinguish between polyclonal and compound mutations in BCR::ABL1 KD since the long-range (LR)-NGS and fragment subcloning was not performed due to limited budget. The samples included in this study were selected from only a single center and thus the findings may not be representative of the general population of TKI resistant CML patients in Malaysia. Due to financial and time constraint, only 84 samples were able to recruit in the current study.
Data availability
The data are not publicly available due to ethical restrictions by the Medical Research Ethics Committee (MREC) Ministry of Health Malaysia (NMRR-19-3693-52311). A Table S1 has been attached. The remaining data are available from the corresponding author upon reasonable request, subject to the permission of Medical Research & Ethics Committee Ministry of Health Malaysia.
Abbreviations
- bp:
-
base pairs
- cDNA:
-
complementary DNA
- CML:
-
Chronic myeloid leukemia
- ddG:
-
Delta Delta G
- DNA:
-
Deoxyribonucleic acid
- ELN:
-
European LeukemiaNet
- IM:
-
imatinib mesylate
- IS:
-
International Scale
- KD:
-
Kinase domain
- NCCN:
-
National Comprehensive Cancer Network
- NGS:
-
Next generation sequencing
- PCR:
-
Polymerase chain reaction
- RNA:
-
Ribonucleic acid
- SS:
-
Sanger sequencing
- TKI:
-
Tyrosine kinase inhibitor
- VCF:
-
VCard File
References
Ren R. Mechanisms of BCR-ABL in the pathogenesis of chronic myelogenous leukaemia. Nat Rev Cancer. 2005;5(3):172–83. https://doi.org/10.1038/nrc1567.
Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2018 update on diagnosis, therapy and monitoring. Am J Hematol. 2018;93(3):442–59. https://doi.org/10.1002/ajh.25011.
Deininger M, O’Brien SG, Guilhot F, Goldman JM, Hochhaus A, Hughes TP, et al. International Randomized Study of Interferon vs STI571 (IRIS) 8-Year follow up: sustained survival and low risk for progression or events in patients with newly diagnosed chronic myeloid leukemia in Chronic Phase (CML-CP) treated with Imatinib. Blood. 2009;114(22):1126.
Quintás-Cardama A, Kantarjian H, Cortes J. Imatinib and beyond–exploring the full potential of targeted therapy for CML. Nat Rev Clin Oncol. 2009;6(9):535–43. https://doi.org/10.1038/nrclinonc.2009.112.
La Rosée P, Deininger M. Resistance to Imatinib: mutations and Beyond. Semin Hematol. 2010;47:335–43. https://doi.org/10.1053/j.seminhematol.2010.06.005.
Patel AB, O’Hare T, Deininger MW. Mechanisms of resistance to ABL kinase inhibition in chronic myeloid leukemia and the development of next generation ABL kinase inhibitors. Hematol Oncol Clin North Am. 2017;31(4):589–612. https://doi.org/10.1016/j.hoc.2017.04.007.
Majumdar A, Katara R, Mishra A, Gupta A, Sharma DK, Srivastava AK et al. A Retrospective Analysis of BCR-ABL1 Kinase Domain Mutations in the Frontline Drug Intolerant or Resistant Chronic Myeloid Leukemia Patients: An Indian Experience from a High-End Referral Laboratory. South Asian J Cancer. 2022;(EFirst). https://doi.org/10.1055/s-0042-1757911.
Soverini S, Branford S, Nicolini FE, Talpaz M, Deininger MWN, Martinelli G, et al. Implications of BCR-ABL1 kinase domain-mediated resistance in chronic myeloid leukemia. Leuk Res. 2014;38(1):10–20. https://doi.org/10.1016/j.leukres.2013.09.011.
Gibbons DL, Pricl S, Posocco P, Laurini E, Fermeglia M, Sun H, et al. Molecular dynamics reveal BCR-ABL1 polymutants as a unique mechanism of resistance to PAN-BCR-ABL1 kinase inhibitor therapy. Proc Natl Acad Sci. 2014;111(9):3550–5. https://doi.org/10.1073/pnas.1321173111.
Radich JP, Deininger M, Abboud CN, Altman JK, Berman E, Bhatia R, et al. Chronic myeloid leukemia, Version 1.2019, NCCN Clinical Practice guidelines in Oncology. J Natl Compr Canc Netw. 2018;16(9):1108–35. https://doi.org/10.6004/jnccn.2018.0071.
Hochhaus A, Baccarani M, Silver RT, Schiffer C, Apperley JF, Cervantes F, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020;34(4):966–84. https://doi.org/10.1038/s41375-020-0776-2.
National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in oncology: Chronic Myeloid Leukemia. Version 1.2023. https://www.nccn.org/professionals/physician_gls/pdf/cml.pdf (2023). Accessed 5 Feb 2023.
Soverini S, Hochhaus A, Nicolini FE, Gruber F, Lange T, Saglio G, et al. BCR-ABL kinase domain mutation analysis in chronic myeloid leukemia patients treated with tyrosine kinase inhibitors: recommendations from an expert panel on behalf of European LeukemiaNet. Blood. 2011;118(5):1208–15. https://doi.org/10.1182/blood-2010-12-326405.
Machova Polakova K, Polivkova V, Rulcova J, Klamova H, Jurcek T, Dvorakova D, et al. Constant BCR-ABL transcript level > or = 0.1% (IS) in patients with CML responding to imatinib with complete cytogenetic remission may indicate mutation analysis. Exp Hematol. 2010;38(1):20–6. https://doi.org/10.1016/j.exphem.2009.10.003.
Alikian M, Gerrard G, Subramanian PG, Mudge K, Foskett P, Khorashad JS, et al. BCR-ABL1 kinase domain mutations: methodology and clinical evaluation. Am J Hematol. 2012;87(3):298–304. https://doi.org/10.1002/ajh.22272.
Sullivan KM, Dean A, Soe MM. On academics: OpenEpi: a web-based epidemiologic and Statistical Calculator for Public Health. Public Health Rep. 2009;124(3):471–4. https://doi.org/10.1177/003335490912400320.
Yap E, Tumian NR, Azma RZ, Sharifah NA, Salwati S, Hamidah NH, et al. Primary imatinib resistance in chronic myeloid leukemia patients in a develo** country: BCR-ABL kinase domain mutations or BCR-ABL independent mechanisms? Malays J Pathol. 2017;39(2):107–13.
Elias MH, Baba AA, Azlan H, Rosline H, Sim GA, Padmini M, et al. BCR-ABL kinase domain mutations, including 2 novel mutations in imatinib resistant Malaysian chronic myeloid leukemia patients-frequency and clinical outcome. Leuk Res. 2014;38(4):454–9. https://doi.org/10.1016/j.leukres.2013.12.025.
Elias MH, Baba AA, Husin A, Abdullah AD, Hassan R, Sim GA, et al. Contribution of BCR-ABL kinase domain mutations to imatinib mesylate resistance in Philadelphia chromosome positive Malaysian chronic myeloid leukemia patients. Hematol Rep. 2012;4(4):e23.
Soverini S. Abl kinase domain mutations as a mechanism of resistance to tyrosine kinase inhibitors in Philadelphia-positive leukemias: biological, clinical and prognostic relevance [PhD thesis]. University of Bologna. http://amsdottorato.unibo.it/440/1/Simona_Soverini_Tesi_di_dottorato.pdf (2007). Accessed 7 Jan 2022.
Soverini S, Colarossi S, Gnani A, Rosti G, Castagnetti F, Poerio A, et al. Contribution of ABL kinase domain mutations to imatinib resistance in different subsets of Philadelphia-positive patients: by the GIMEMA Working Party on chronic myeloid leukemia. Clin Cancer Res. 2006;12(24):7374–9. https://doi.org/10.1158/1078-0432.Ccr-06-1516.
Hughes T, Saglio G, Branford S, Soverini S, Kim DW, Müller MC, et al. Impact of baseline BCR-ABL mutations on response to nilotinib in patients with chronic myeloid leukemia in chronic phase. J Clin Oncol. 2009;27(25):4204–10. https://doi.org/10.1200/jco.2009.21.8230.
Bradeen HA, Eide CA, O’Hare T, Johnson KJ, Willis SG, Lee FY, et al. Comparison of imatinib mesylate, dasatinib (BMS-354825), and nilotinib (AMN107) in an N-ethyl-N-nitrosourea (ENU)-based mutagenesis screen: high efficacy of drug combinations. Blood. 2006;108(7):2332–8. https://doi.org/10.1182/blood-2006-02-004580.
Tanneeru K, Guruprasad L. Ponatinib is a pan-BCR-ABL kinase inhibitor: MD simulations and SIE study. PLoS ONE. 2013;8(11):e78556. https://doi.org/10.1371/journal.pone.0078556.
Byrgazov K, Lucini CB, Valent P, Hantschel O, Lion T. BCR-ABL1 compound mutants display differential and dose-dependent responses to ponatinib. Haematologica. 2018;103(1):e10–2. https://doi.org/10.3324/haematol.2017.176347.
Hochhaus A, La Rosée P, Müller MC, Ernst T, Cross NC. Impact of BCR-ABL mutations on patients with chronic myeloid leukemia. Cell Cycle. 2011;10(2):250–60. https://doi.org/10.4161/cc.10.2.14537.
Soverini S, Martinelli G, Colarossi S, Gnani A, Castagnetti F, Rosti G, et al. Presence or the emergence of a F317L BCR-ABL mutation may be associated with resistance to dasatinib in Philadelphia chromosome-positive leukemia. J Clin Oncol. 2006;24(33):e51–2. https://doi.org/10.1200/jco.2006.08.9128.
Cortes JE, Kantarjian H, Shah NP, Bixby D, Mauro MJ, Flinn I, et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med. 2012;367(22):2075–88. https://doi.org/10.1056/NEJMoa1205127.
Zabriskie MS, Eide CA, Tantravahi SK, Vellore NA, Estrada J, Nicolini FE, et al. BCR-ABL1 compound mutations combining key kinase domain positions confer clinical resistance to ponatinib in Ph chromosome-positive leukemia. Cancer Cell. 2014;26(3):428–42. https://doi.org/10.1016/j.ccr.2014.07.006.
Kayastha GK, Ranjitkar N, Gurung R, Kc RK, Karki S, Shrestha R, et al. The use of Imatinib resistance mutation analysis to direct therapy in Philadelphia chromosome/BCR-ABL1 positive chronic myeloid leukaemia patients failing Imatinib treatment, in Patan Hospital, Nepal. Br J Haematol. 2017;177(6):1000–7. https://doi.org/10.1111/bjh.14683.
Cang S, Liu D. P-loop mutations and novel therapeutic approaches for imatinib failures in chronic myeloid leukemia. J Hematol Oncol. 2008;1:15. https://doi.org/10.1186/1756-8722-1-15.
Jabbour E, Parikh SA, Kantarjian H, Cortes J. Chronic myeloid leukemia: mechanisms of resistance and treatment. Hematol Oncol Clin North Am. 2011;25(5):981 – 95, v. https://doi.org/10.1016/j.hoc.2011.09.004.
Soverini S, Colarossi S, Gnani A, Castagnetti F, Rosti G, Bosi C, et al. Resistance to dasatinib in Philadelphia-positive leukemia patients and the presence or the selection of mutations at residues 315 and 317 in the BCR-ABL kinase domain. Haematologica. 2007;92(3):401–4. https://doi.org/10.3324/haematol.10822.
Zhou Y, Portelli S, Pat M, Rodrigues CHM, Nguyen T-B, Pires DEV, et al. Structure-guided machine learning prediction of drug resistance mutations in Abelson 1 kinase. Comput Struct Biotechnol J. 2021;19:5381–91. https://doi.org/10.1016/j.csbj.2021.09.016.
Soverini S, De Benedittis C, Polakova KM, Linhartova J, Castagnetti F, Gugliotta G, et al. Next-generation sequencing for sensitive detection of BCR-ABL1 mutations relevant to tyrosine kinase inhibitor choice in imatinib-resistant patients. Oncotarget. 2016;7(16):21982–90. https://doi.org/10.18632/oncotarget.8010.
Duong CQ, Cuong N, Thien T, Nguyen LV, Huy QP, Hien T, et al. Utilization of Next-Generation Deep sequencing to analyze BCR-ABL1 kinase domain mutation for Imatinib-resistant chronic myeloid leukemia patients in Vietnam. J Leuk. 2017;05. https://doi.org/10.4172/2329-6917.1000235.
Erbilgin Y, Eskazan AE, Hatirnaz Ng O, Salihoglu A, Elverdi T, Firtina S, et al. Deep sequencing of BCR-ABL1 kinase domain mutations in chronic myeloid leukemia patients with resistance to tyrosine kinase inhibitors. Leuk Lymphoma. 2019;60(1):200–7. https://doi.org/10.1080/10428194.2018.1473573.
Liu J, Yang H, Xu X, Yi S, Meng L. Mutations in the BCR-ABL1 kinase domain in patients with chronic myeloid leukaemia treated with TKIs or at diagnosis. Oncol Lett. 2020;20(2):1071–6. https://doi.org/10.3892/ol.2020.11650.
Kim SH, Kim D, Kim DW, Goh HG, Jang SE, Lee J, et al. Analysis of bcr-abl kinase domain mutations in Korean chronic myeloid leukaemia patients: poor clinical outcome of P-loop and T315I mutation is disease phase dependent. Hematol Oncol. 2009;27(4):190–7. https://doi.org/10.1002/hon.894.
Khorashad JS, Kelley TW, Szankasi P, Mason CC, Soverini S, Adrian LT, et al. BCR-ABL1 compound mutations in tyrosine kinase inhibitor-resistant CML: frequency and clonal relationships. Blood. 2013;121(3):489–98. https://doi.org/10.1182/blood-2012-05-431379.
Akram AM, Iqbal Z, Akhtar T, Khalid AM, Sabar MF, Qazi MH, et al. Presence of novel compound BCR-ABL mutations in late chronic and advanced phase imatinib sensitive CML patients indicates their possible role in CML progression. Cancer Biol Ther. 2017;18(4):214–21. https://doi.org/10.1080/15384047.2017.1294289.
Acknowledgements
The authors would like to thank the Director General of Health Malaysia for approval to publish this scientific paper. We would also like to thank the Deputy Director General of Health (Research and Technical Support) and the Director of the Institute for Medical Research (IMR) for their support.
Funding
This work was supported by the Ministry of Health Malaysia, (JPP-IMR 19–037) and UiTM MyRA Research Grant (600-RMC/GPM ST 5/3 (002/2021)).
Author information
Authors and Affiliations
Contributions
ZAS, YMY and FA designed the study. ZAS, YMY and FA wrote the manuscript, which was revised by NRK, ENMS, EE, SSMS, NA. MKNMK contributed to the analysis and substantially revised the manuscript. WKD, JA and NAA performed molecular experiments. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Medical Research and Ethics Committee (MREC), Ministry of Health, Malaysia [(NMRR-19-3693-52311) (Ref. no. KKM/NIHSEC/P20-186(6); date approval 3/2/2020)]. The RNA sample utilised in the present research was sourced from the Pathology Laboratory at Hospital Tunku Azizah and Diagnostic Laboratory Haematology at Institute for Medical Research (IMR), National Institute of Health (NIH). The samples were used in routine lab tests for detection and quantification of BCR::ABL1 transcripts and BCR::ABL1 mutation detection and would be discarded if not used for research purposes. Patients’ medical records were accessed from January 2017 to December 2020. The investigator recorded the information in a way that ensures subjects cannot be identified either directly or indirectly through associated identifiers. Both the archival of medical records and study data will be deleted upon completion of the research. Therefore, the informed consent was waived by the MREC committee that reviewed the entire study protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Seman, Z.A., Ahid, F., Kamaluddin, N.R. et al. Mutation analysis of BCR-ABL1 kinase domain in chronic myeloid leukemia patients with tyrosine kinase inhibitors resistance: a Malaysian cohort study. BMC Res Notes 17, 111 (2024). https://doi.org/10.1186/s13104-024-06772-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-024-06772-1