Abstract
Background
Epicardial adipose tissue (EAT) is a type of ectopic fat with endocrine and paracrine functions. Aryl hydrocarbon receptor (AhR) is a ligand-activated transcription factor that responds to environmental stimuli. AhR expression is associated with obesity. In this cross-sectional study, we aimed to determine the relationship between circulating AhR concentrations and EAT.
Methods
A total of 30 men with obesity and 23 age-matched men as healthy controls were enrolled. Plasma AhR concentrations were determined at fasting. The EAT thickness was measured on the free wall of the right ventricle from the basal short-axis plane by magnetic resonance imaging.
Results
The participants with obesity had a higher plasma AhR level than the controls (81.0 ± 24.5 vs. 65.1 ± 16.4 pg/mL, P = 0.010). The plasma AhR level was positively correlated with EAT thickness (correlation coefficient = 0.380, P = 0.005). After adjusting for fasting glucose levels, plasma AhR levels were still significantly associated with EAT thickness (95% CI 0.458‒5.357, P = 0.021) but not with body mass index (P = 0.168).
Conclusion
Plasma AhR concentrations were positively correlated with EAT thickness on the free wall of the right ventricle in men. Further investigations are needed to evaluate the causal effects and underlying mechanisms between AhR and EAT.
Similar content being viewed by others
Introduction
There has been an increasing trend in body mass index (BMI) in recent decades, and obesity has become a health burden worldwide [1, 2]. The global mean BMI of adult males increased from 21.7 kg/m2 in 1975 to 24.2 kg/m2 in 2014, and the global proportion of adult males with a BMI ≥ 30 kg/m2 increased from 3.2% in 1975 to 10.8% in 2014 [3]. According to the Nutrition and Health Survey in Taiwan, the prevalence of adult obesity, defined as a BMI ≥ 27 kg/m2, sharply increased from 11.8% during 1993–1996 to 22.0% during 2013–2014 [4]. Compared to a BMI between 22 and 25 kg/m2, a BMI ≥ 30 kg/m2 is associated with an increased risk of mortality [5]. In addition to BMI, central obesity, measured using waist circumference, has an independent risk of mortality [6, 7]. Liu et al. [8] reported that waist circumference as well as BMI is important in predicting mortality in Chinese males with prediabetes. However, McNeely et al. [9] reported that the area of visceral fat at the level of the umbilicus was not a better predictor of mortality than BMI.
Epicardial adipose tissue (EAT) is the ectopic fat located between the myocardium and the visceral layer of the pericardium [10, 11]. EAT, as an endocrine and paracrine organ, physiologically exhibits metabolic, thermogenic, and cardioprotective characteristics [12]. However, excessive EAT thickness is associated with metabolic syndrome [13], insulin resistance [14], coronary artery disease [15], and changes in cardiac morphology [16, 17]. EAT is an independent risk factor for both coronary calcification and coronary atheromatous plaque; EAT may more directly reflect the presence of coronary artery disease than the area of abdominal visceral fat [18]. Therefore, EAT is an important risk factor for coronary heart disease [19, 20].
The aryl hydrocarbon receptor (AhR) is a ligand-activated transcription factor of the basic-helix-loop-helix family with a Per-ARNT-Sim domain for regulating downstream responses to environmental stimulation [21]. One of the most important AhR ligands is the environmental pollutant dioxin (2,3,7,8-tetrachlorodibenzo-p-dioxin, TCDD) [22]. The AhR complex (AhR/ligand/heat shock protein 90) is activated after ligand binding and translocates into the nucleus. The AhR/ligand complex can bind to the AhR nuclear translocator (ARNT) and trigger the promoters of target genes, including the cytochrome P450 (CYP) enzymes CYP1A1 and CYP1B1 [23]. Furthermore, the AhR complex also activates mitogen-activated protein kinases (MAPKs), leading to the activation of nuclear factor-kappaB and associated proinflammatory cytokines [24]. Circulating AhR concentrations are higher in subjects with overweight or obesity than in those with normal weight [25]. A high-fat diet can induce vascular AhR protein expression in mice, and inhibition of AhR can attenuate vascular dysfunction induced by a high-fat diet [26].
Activation of the AhR pathway is associated with myocardial ischemia–reperfusion injury through the regulation of mitochondrial oxidative stress and apoptosis [27]. The use of an AhR antagonist can attenuate myocardial injury in the rat myocardial ischemia–reperfusion model [28]. Vilahur et al. [29] also reported that ischemic postconditioning can induce a downregulation of the AhR pathway and reduce reperfusion-induced cell damage to improve cardiac function in pigs after myocardial infarction. Recently, Christensen et al. [30] reported that EAT thickness on the free wall of the right ventricle could significantly predict cardiovascular events and mortality in men. Both EAT thickness and AhR expression have a close relationship with obesity. However, the association between EAT thickness and circulating AhR levels has not been understood. We hypothesize that EAT thickness is positively correlated with circulating AhR levels. Therefore, we conducted a cross-sectional study to assess the EAT thickness and plasma AhR levels in men with and without obesity.
Materials and methods
Study design and subjects
This cross-sectional study was conducted at Taichung Veterans General Hospital, Taiwan. The inclusion criteria for study candidates were (1) male Han Chinese adults, (2) having metabolic syndrome defined by the International Diabetes Federation [31], and (3) having obesity defined by a BMI ≥ 27 kg/m2 [32]. The exclusion criteria were (1) a known medical history of diabetes mellitus, (2) a known endocrine disease, (3) a known psychological disorder, (4) severe systemic diseases including malignancies, established ischemic heart disease, or immune disorders, and (5) current use of medications that change body weight, including systemic steroids. In addition, we enrolled age-matched men with a BMI < 24 kg/m2 as healthy controls.
Procedures
After enrollment, anthropometric characteristics were measured in the morning after an overnight fast. The measurements of body height (Pharmacia Taiwan Inc., Taipei, Taiwan) and body weight (Detecto, Cardinal Scale Manufacturing Co., Webb City, MO, USA) were performed after participants removed their shoes and any heavy clothing. Waist circumference (kp-1508, King Life, Taipei, Taiwan) was measured at the level of the umbilicus after expiration with the participant breathing quietly and regularly. Blood pressure was detected using the Dinamap™ Vital Signs Monitor (Model 1846 SX/P, Critikon, Tampa, FL) after subjects had been sitting at rest for 10 min.
Biochemical assessments
Blood samples were collected during fasting. Serum samples were prepared for detecting levels of creatinine, total cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. Plasma samples were prepared for detecting levels of glucose, insulin, and AhR. A 75 g oral glucose tolerance test was performed to exclude patients with a diagnosis of diabetes mellitus based on plasma glucose levels ≥ 126 mg/dL at fasting or ≥ 200 mg/dL at 120 min [33].
Concentrations of cholesterol, triglycerides, and creatinine were measured by using commercial kits (Beckman Coulter, Fullerton, USA). Glucose levels were measured using an oxidase–peroxidase method (Wako Diagnostics, Tokyo, Japan). Insulin levels were measured using a commercial kit (Roche Diagnostics GmbH, Mannheim, Germany). AhR levels were determined using the quantitative sandwich enzyme immunoassay with a commercial kit (Cusabio, Wuhan, China). The coefficient of variability (CV) of intra-assay precision for AhR was < 8% based on twenty testes on one plate and the inter-assay CV was < 10%.
The homeostasis model assessment of insulin resistance (HOMA-IR) index was calculated using the following equation: fasting insulin (µIU/mL) × fasting glucose (mmol/L)/22.5 [34]. The estimated glomerular filtration rate (eGFR) was calculated according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation as follows: 141 × (serum creatinine [mg/dL]/0.9)−0.411 × 0.993age (years) if the serum creatinine level is ≤ 0.9 mg/dL or 141 × (serum creatinine [mg/dL]/0.9)−1.209 × 0.993age (years) if the serum creatinine level is > 0.9 mg/dL [35].
Magnetic resonance imaging (MRI) assessments
The parameters of the adipose component were assessed by MRI (Siemens Medical Systems, Iselin, New Jersey, USA), as reported in our previous study [36]. Briefly, EAT thickness was measured on the free wall of the right ventricle from the basal short-axis plane [37]. The average thickness was recorded using measurements at three equally spaced points (25%, 50%, and 75% of the full length) along the right ventricular free wall [38]. Participants were asked to hold their breath after expiration while cross-sectional images were taken. Images were transferred to a Siemens Leonardo workstation and the adipose tissue area was calculated using software (Leonardo, Siemens Healthcare, Germany) [39].
Statistical analysis
All continuous data are presented as the mean ± standard deviation, and categorical data are presented as numbers (percentages). The chi-square test was used to detect significant differences in categorical variables. The data distributions of plasma AhR levels were examined using the Kolmogorov–Smirnov test and were compatible with a normal distribution in both the obesity and control groups (P = 0.128 and 0.106, respectively). An independent sample t test was conducted to detect significant differences in variables between the two groups. The correlation coefficient (r) was estimated using Pearson’s correlation test. Linear regression analysis was used to analyze the association between clinical factors and plasma AhR levels. Fasting glucose was used as the variable for glucose dysregulation in the regression analysis because of strong multicollinearity between fasting glucose, fasting insulin, and HOMA IR. A two-sided P value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS 22.0 (IBM, Armonk, NY, USA).
Results
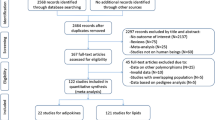
A total of 66 candidates were enrolled in this study, including 40 men in the obesity group and 26 men in the control group. Ten subjects in the obesity group and three subjects in the control group were excluded from the analyses after assessment (Fig. 1).
The characteristics of the 53 participants enrolled in the data analyses are shown in Table 1. There was no significant difference in age between the obesity and control groups (43 ± 11 vs. 39 ± 11 years, P = 0.184). The participants with obesity had a higher body weight (97.8 ± 13.5 vs. 67.1 ± 7.1 kg, P < 0.001), BMI (33.7 ± 4.2 vs. 22.5 ± 1.6 kg/m2, P < 0.001), waist circumference (109.3 ± 9.6 vs. 82.1 ± 6.4 cm, P < 0.001), and EAT thickness (6.8 ± 1.8 vs. 3.2 ± 1.4 mm, P < 0.001) than the controls. The participants with obesity also had higher blood pressures (systolic: 135 ± 18 vs. 115 ± 10 mmHg, P < 0.001; diastolic: 79 ± 13 vs. 69 ± 7 mmHg, P = 0.001; respectively), higher fasting glucose levels (5.5 ± 0.5 vs. 5.1 ± 0.4 mmol/L, P = 0.005), higher fasting insulin levels (18.4 ± 11.6 vs. 6.3 ± 2.6 µIU/mL, P < 0.001), higher HOMA-IR (4.5 ± 3.0 vs. 1.4 ± 0.7, P < 0.001), higher fasting triglyceride levels (2.2 ± 0.8 vs. 1.0 ± 0.3 mmol/L, P < 0.001), and lower HDL cholesterol levels (1.1 ± 0.2 vs. 1.5 ± 0.3, P < 0.001) than the controls. However, there was no significant difference in the proportion of current smokers, total cholesterol levels, and the eGFR between these two groups (P > 0.05 for all the variables).
The participants with obesity had a higher plasma AhR level than the controls (81.0 ± 24.5 vs. 65.1 ± 16.4 pg/mL, P = 0.010; Fig. 2). Furthermore, when the data of all the enrolled participants were analyzed, plasma AhR levels showed significant correlation with the thickness of EAT (r = 0.380, P = 0.005; Fig. 3A). However, the correlation between plasma AhR level and EAT thickness was not statistically significant in the obesity group (r = 0.202, P = 0.284; Fig. 3B) and in the control group (r = 0.157, P = 0.474; Fig. 3C). The univariable regression analysis results showed that plasma AhR levels were significantly associated with EAT thickness, BMI, and fasting glucose levels. The multivariable linear regression analysis results showed that plasma AhR levels were significantly associated with EAT thickness (regression coefficient = 2.907, 95% confidence interval 0.458‒5.357, P = 0.021; Table 2), but were not associated with BMI (P = 0.168) after adjustment with fasting glucose levels.
Discussion
The main finding of the present study was that plasma AhR concentrations were positively correlated with the thickness of EAT on the free wall of the right ventricle in men. In the linear regression analyses, plasma AhR levels showed a better correlation with EAT thickness than the correlation with BMI or waist circumference. AhR overexpression is associated with obesity and obesity-related inflammation. Rojas et al. [40] reported that visceral adipocytes detected using fluorescence microscopy significantly decreased after AhR antagonist treatment in male mice after high-fat diet feeding, but subcutaneous adipocytes did not significantly respond to AhR antagonist treatment. Similarly, Xu et al. [41] reported that visceral fat, presented as the weight of epididymal white adipose tissue, significantly decreased in AhR-deficient mice compared with wild-type mice after high-fat diet feeding. Moreover, glucose levels, insulin resistance, and inflammatory cytokines were also lower in AhR-deficient mice than in wild-type mice after high-fat diet feeding. Notably, high-fat diet increased the expression of AhR protein in the aorta of male mice [26], but decreased the expression of AhR protein in the liver tissues [42]. Therefore, high-fat diet may enhance the circulating levels of AhR by increasing the vascular AhR protein, but may not increase the AhR protein in the other tissues. Serum AhR levels have been reported to be higher in patients with a BMI ≥ 25 kg/m2 than in those with a BMI < 25 kg/m2 [25], and Wang et al. [43] also reported that serum AhR levels were inversely correlated with β-cell function presented as an insulinogenic index. The strength of our study is that EAT thickness was shown to have a better correlation with plasma AhR levels than BMI and waist circumference.
AhR plays an important role in adipocyte differentiation, and activation of AhR can significantly promote peroxisome proliferator-activated receptor γ (PPARγ) decay, which was shown to be involved in the mechanism of proteasome-dependent degradation in an in vitro study [44]. AhR activation induced not only adipogenesis but also vascular endothelial dysfunction in an in vivo model of male mice [45]. Distel et al. [46] reported that PPARγ agonists could increase lipid turnover and decrease fatty acid release from EAT in an animal model of rats. Atherosclerotic plaque showed an earlier onset and greater severity in dioxin-treated mice than in those without dioxin exposure [47]. AhR expression, presented as mRNA extracted from peripheral blood mononuclear cells, was higher in patients with coronary artery disease than in controls [48]. In a meta-analysis study, dioxin exposure was significantly associated with the mortality risk of ischemic heart disease [49]. Therefore, higher AhR expression might not only increase atherosclerotic risk but also facilitate EAT to release cytokines and fatty acids, causing adverse myocardial remodeling in ischemic cardiomyopathy [50, 51].
AhR expression has been observed in various tissues and cells, including the endothelium [52, 53]. Without ligand binding, AhR is present in an inactive complex in the cytoplasm; after ligand binding, AhR undergoes transformation and shuttles from the cytoplasm into the nucleus, followed by activation of AhR target genes [54]. Beranek et al. [55] reported a positive correlation between serum levels of AhR and CYP1A1, which is one of the most well-known downstream regulators of the AhR signaling pathway. Hu et al. [56] reported that serum levels of AhR and CYP1A1 were significantly increased in patients with atopic dermatitis and the disease severity significantly correlated with AhR expression in the peripheral blood mononuclear cells. Furthermore, Ramos-García et al. reported that high serum AhR levels were associated with Alzheimer’s disease [57]. High circulating AhR levels are also associated with obesity and glucose dysregulation [25, 43]. Therefore, a high circulating AhR level may serve as a biomarker for the excessive activation of the AhR pathway involved in inflammatory mechanism. In the present study, we observed a significantly positive correlation between plasma AhR levels and EAT thickness. Although we could not demonstrate the causal relationship between plasma AhR levels and EAT in this cross-sectional study, the results of our study suggest that plasma AhR levels reflect the EAT thickness which indicates the cardiovascular risk. Previous studies have demonstrated that AhR pathway is a potential therapeutic target for ischemic heart disease [58]. However, further studies are required to assess the pathophysiological mechanisms involving the AhR signaling pathway and excessive EAT.
There are several limitations of the present study. First, in this cross-sectional study, we did not determine the causal relationship between increased circulating AhR levels and EAT accumulation. Second, we did not directly investigate the mechanisms underlying the association between AhR and EAT. Third, we did not assess the source of plasma AhR in the subjects. Fourth, we could not differentiate the phenotypes of epicardial adipocytes based on MRI. Wang et al. [59] reported that a conversion from brown adipose tissue to white adipose tissue can induce the local development of coronary atherosclerosis. Finally, we only enrolled male adults without diabetes mellitus because previous studies reported that the association between EAT cardiovascular risk was stronger in males than in the females [30, 60]. Moreover, plasma AhR levels are higher in the male patients with pancreatic cancer than in the female patients with pancreatic cancer [61]. Furthermore, AhR activation induces different responses in males and females regarding glucose regulation [62]. This study included participants from the Han Chinese ethnicity. Therefore, our findings need to be verified further in other populations.
Conclusions
Our results demonstrated that plasma AhR concentrations were significantly higher in men with obesity than in those without obesity. In particular, plasma AhR concentrations were positively correlated with the thickness of EAT on the free wall of the right ventricle, and the correlation was better than that with BMI after adjusting for the fasting glucose levels.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AhR:
-
Aryl hydrocarbon receptor
- ARNT:
-
Aryl hydrocarbon receptor nuclear translocator
- BMI:
-
Body mass index
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CV:
-
Coefficient of variability
- CYP:
-
Cytochrome P450
- EAT:
-
Epicardial adipose tissue
- eGFR:
-
Estimated glomerular filtration rate
- HDL:
-
High-density lipoprotein
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- MAPK:
-
Mitogen-activated protein kinase
- MRI:
-
Magnetic resonance imaging
- PPARγ:
-
Peroxisome proliferator-activated receptor γ
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Li M, Gong W, Wang S, Li Z. Trends in body mass index, overweight and obesity among adults in the USA, the NHANES from 2003 to 2018: a repeat cross-sectional survey. BMJ Open. 2022;12(12):e065425.
NCD Risk Factor Collaboration. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 192 million participants. Lancet. 2016;387(10026):1377–96.
Chang HC, Yang HC, Chang HY, Yeh CJ, Chen HH, Huang KC, Pan WH. Morbid obesity in Taiwan: prevalence, trends, associated social demographics, and lifestyle factors. PLoS ONE. 2017;12(2):e0169577.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82.
Bigaard J, Tjonneland A, Thomsen BL, Overvad K, Heitmann BL, Sorensen TI. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res. 2003;11(7):895–903.
Kim YH, Kim SM, Han KD, Jung JH, Lee SS, Oh SW, Park HS, Rhee EJ, Lee WY, Yoo SJ. Waist circumference and all-cause mortality independent of body mass index in Korean population from the national health insurance health checkup 2009(-)2015. J Clin Med. 2019;8(1):72.
Liu L, Gao B, Wang J, Yang C, Wu S, Wu Y, Chen S, Li Q, Zhang H, Wang G, et al. Joint association of body mass index and central obesity with cardiovascular events and all-cause mortality in prediabetic population: a prospective cohort study. Obes Res Clin Pract. 2019;13(5):453–61.
McNeely MJ, Shofer JB, Leonetti DL, Fujimoto WY, Boyko EJ. Associations among visceral fat, all-cause mortality, and obesity-related mortality in Japanese Americans. Diabetes Care. 2012;35(2):296–8.
Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005;2(10):536–43.
Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007;153(6):907–17.
Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab. 2011;22(11):450–7.
Pierdomenico SD, Pierdomenico AM, Cuccurullo F, Iacobellis G. Meta-analysis of the relation of echocardiographic epicardial adipose tissue thickness and the metabolic syndrome. Am J Cardiol. 2013;111(1):73–8.
Iacobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab. 2005;90(11):6300–2.
Eroglu S, Sade LE, Yildirir A, Bal U, Ozbicer S, Ozgul AS, Bozbas H, Aydinalp A, Muderrisoglu H. Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr Metab Cardiovasc Dis. 2009;19(3):211–7.
Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. Am J Cardiol. 2004;94(8):1084–7.
Iacobellis G. Relation of epicardial fat thickness to right ventricular cavity size in obese subjects. Am J Cardiol. 2009;104(11):1601–2.
Oikawa M, Owada T, Yamauchi H, Misaka T, Machii H, Yamaki T, Sugimoto K, Kunii H, Nakazato K, Suzuki H, et al. Epicardial adipose tissue reflects the presence of coronary artery disease: comparison with abdominal visceral adipose tissue. Biomed Res Int. 2015;2015:483982.
Hendricks S, Dykun I, Balcer B, Totzeck M, Rassaf T, Mahabadi AA. Epicardial adipose tissue is a robust measure of increased risk of myocardial infarction—a meta-analysis on over 6600 patients and rationale for the EPIC-ACS study. Medicine. 2021;100(52):e28060.
Packer M. Epicardial adipose tissue may mediate deleterious effects of obesity and inflammation on the myocardium. J Am Coll Cardiol. 2018;71(20):2360–72.
Rejano-Gordillo CM, Marin-Diaz B, Ordiales-Talavero A, Merino JM, Gonzalez-Rico FJ, Fernandez-Salguero PM. From nucleus to organs: insights of aryl hydrocarbon receptor molecular mechanisms. Int J Mol Sci. 2022;23(23):14919.
Falandysz J, Fernandes A, Gregoraszczuk E, Rose M. The toxicological effects of halogenated naphthalenes: a review of aryl hydrocarbon receptor-mediated (dioxin-like) relative potency factors. J Environ Sci Health, Part C Environ Carcinog Ecotoxicol Rev. 2014;32(3):239–72.
Fisher JM, Jones KW, Whitlock JP Jr. Activation of transcription as a general mechanism of 2,3,7,8-tetrachlorodibenzo-p-dioxin action. Mol Carcinog. 1989;1(4):216–21.
Denison MS, Soshilov AA, He G, DeGroot DE, Zhao B. Exactly the same but different: promiscuity and diversity in the molecular mechanisms of action of the aryl hydrocarbon (dioxin) receptor. Toxicol Sci. 2011;124(1):1–22.
Andac-Ozturk S, Koc G, Soyocak A. Association of aryl hydrocarbon receptor (AhR) serum level and gene rs10247158 polymorphism with anthropometric, biochemical parameters and food consumption in overweight/obese patients. Int J Clin Pract. 2021;75(9):e14436.
da Silva JF, Bolsoni JA, da Costa RM, Alves JV, Bressan AFM, Silva LEV, Costa TJ, Oliveira AER, Manzato CP, Aguiar CA, et al. Aryl hydrocarbon receptor (AhR) activation contributes to high-fat diet-induced vascular dysfunction. Br J Pharmacol. 2022;179(12):2938–52.
Wang B, Xu A. Aryl hydrocarbon receptor pathway participates in myocardial ischemia reperfusion injury by regulating mitochondrial apoptosis. Med Hypotheses. 2019;123:2–5.
Wang JX, Wang BB, Yuan SZ, Xue K, Zhang JS, Xu AJ. Blocking the aryl hydrocarbon receptor alleviates myocardial ischemia/reperfusion injury in rats. Curr Med Sci. 2022;42(5):966–73.
Vilahur G, Cubedo J, Casani L, Padro T, Sabate-Tenas M, Badimon JJ, Badimon L. Reperfusion-triggered stress protein response in the myocardium is blocked by post-conditioning. Systems biology pathway analysis highlights the key role of the canonical aryl-hydrocarbon receptor pathway. Eur Heart J. 2013;34(27):2082–93.
Christensen RH, von Scholten BJ, Hansen CS, Jensen MT, Vilsboll T, Rossing P, Jorgensen PG. Epicardial adipose tissue predicts incident cardiovascular disease and mortality in patients with type 2 diabetes. Cardiovasc Diabetol. 2019;18(1):114.
Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome: a global public health problem and a new definition. J Atheroscler Thromb. 2005;12(6):295–300.
Pan WH, Lee MS, Chuang SY, Lin YC, Fu ML. Obesity pandemic, correlated factors and guidelines to define, screen and manage obesity in Taiwan. Obes Rev. 2008;9(Suppl 1):22–31.
American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(1):S17–38.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Liang KW, Tsai IC, Lee WJ, Lee IT, Lee WL, Lin SY, Wan CJ, Fu CP, Ting CT, Sheu WH. MRI measured epicardial adipose tissue thickness at the right AV groove differentiates inflammatory status in obese men with metabolic syndrome. Obesity. 2012;20(3):525–32.
Villasante Fricke AC, Iacobellis G. Epicardial adipose tissue: clinical biomarker of cardio-metabolic risk. Int J Mol Sci. 2019;20(23):5989.
Wang TD, Lee WJ, Shih FY, Huang CH, Chang YC, Chen WJ, Lee YT, Chen MF. Relations of epicardial adipose tissue measured by multidetector computed tomography to components of the metabolic syndrome are region-specific and independent of anthropometric indexes and intraabdominal visceral fat. J Clin Endocrinol Metab. 2009;94(2):662–9.
Lee IT, Lee WJ, Tsai IC, Liang KW, Lin SY, Wan CJ, Fu CP, Sheu WH. Brain-derived neurotrophic factor not associated with metabolic syndrome but inversely correlated with vascular cell adhesion molecule-1 in men without diabetes. Clin Chim Acta. 2012;413(9–10):944–8.
Rojas IY, Moyer BJ, Ringelberg CS, Tomlinson CR. Reversal of obesity and liver steatosis in mice via inhibition of aryl hydrocarbon receptor and altered gene expression of CYP1B1, PPARalpha, SCD1, and osteopontin. Int J Obes. 2020;44(4):948–63.
Xu CX, Wang C, Zhang ZM, Jaeger CD, Krager SL, Bottum KM, Liu J, Liao DF, Tischkau SA. Aryl hydrocarbon receptor deficiency protects mice from diet-induced adiposity and metabolic disorders through increased energy expenditure. Int J Obes. 2015;39(8):1300–9.
Ma Y, Chen K, Lv L, Wu S, Guo Z. Ferulic acid ameliorates nonalcoholic fatty liver disease and modulates the gut microbiota composition in high-fat diet fed ApoE(-/-) mice. Biomed Pharmacother. 2019;113:108753.
Wang JS, Lee WJ, Lee IT, Lin SY, Lee WL, Liang KW, Lin SJ, Sheu WH. Negative association between serum aryl hydrocarbon receptor concentrations and beta-cell function in patients with no history of diabetes undergoing coronary angiography. J Diabetes. 2018;10(12):958–64.
Dou H, Duan Y, Zhang X, Yu Q, Di Q, Song Y, Li P, Gong Y. Aryl hydrocarbon receptor (AhR) regulates adipocyte differentiation by assembling CRL4B ubiquitin ligase to target PPARgamma for proteasomal degradation. J Biol Chem. 2019;294(48):18504–15.
Fehsel K, Schwanke K, Kappel BA, Fahimi E, Meisenzahl-Lechner E, Esser C, Hemmrich K, Haarmann-Stemmann T, Kojda G, Lange-Asschenfeldt C. Activation of the aryl hydrocarbon receptor by clozapine induces preadipocyte differentiation and contributes to endothelial dysfunction. J Psychopharmacol. 2022;36(2):191–201.
Distel E, Penot G, Cadoudal T, Balguy I, Durant S, Benelli C. Early induction of a brown-like phenotype by rosiglitazone in the epicardial adipose tissue of fatty Zucker rats. Biochimie. 2012;94(8):1660–7.
Dalton TP, Kerzee JK, Wang B, Miller M, Dieter MZ, Lorenz JN, Shertzer HG, Nerbert DW, Puga A. Dioxin exposure is an environmental risk factor for ischemic heart disease. Cardiovasc Toxicol. 2001;1(4):285–98.
Huang S, Shui X, He Y, Xue Y, Li J, Li G, Lei W, Chen C. AhR expression and polymorphisms are associated with risk of coronary arterial disease in Chinese population. Sci Rep. 2015;5:8022.
Humblet O, Birnbaum L, Rimm E, Mittleman MA, Hauser R. Dioxins and cardiovascular disease mortality. Environ Health Perspect. 2008;116(11):1443–8.
Jiang DS, Zeng HL, Li R, Huo B, Su YS, Fang J, Yang Q, Liu LG, Hu M, Cheng C, et al. Aberrant epicardial adipose tissue extracellular matrix remodeling in patients with severe ischemic cardiomyopathy: insight from comparative quantitative proteomics. Sci Rep. 2017;7:43787.
Hao S, Sui X, Wang J, Zhang J, Pei Y, Guo L, Liang Z. Secretory products from epicardial adipose tissue induce adverse myocardial remodeling after myocardial infarction by promoting reactive oxygen species accumulation. Cell Death Dis. 2021;12(9):848.
Abel J, Haarmann-Stemmann T. An introduction to the molecular basics of aryl hydrocarbon receptor biology. Biol Chem. 2010;391(11):1235–48.
Dabir P, Marinic TE, Krukovets I, Stenina OI. Aryl hydrocarbon receptor is activated by glucose and regulates the thrombospondin-1 gene promoter in endothelial cells. Circ Res. 2008;102(12):1558–65.
Soshilov AA, Motta S, Bonati L, Denison MS. Transitional states in ligand-dependent transformation of the aryl hydrocarbon receptor into its DNA-binding form. Int J Mol Sci. 2020;21(7):2474.
Beranek M, Fiala Z, Kremlacek J, Andrys C, Krejsek J, Hamakova K, Palicka V, Borska L. Serum levels of aryl hydrocarbon receptor, cytochromes P450 1A1 and 1B1 in patients with exacerbated psoriasis vulgaris. Folia Biol. 2018;64(3):97–102.
Hu YQ, Liu P, Mu ZL, Zhang JZ. Aryl hydrocarbon receptor expression in serum, peripheral blood mononuclear cells, and skin lesions of patients with atopic dermatitis and its correlation with disease severity. Chin Med J. 2020;133(2):148–53.
Ramos-Garcia NA, Orozco-Ibarra M, Estudillo E, Elizondo G, Gomez Apo E, Chavez Macias LG, Sosa-Ortiz AL, Torres-Ramos MA. Aryl hydrocarbon receptor in post-mortem hippocampus and in serum from young, elder, and Alzheimer’s patients. Int J Mol Sci. 2020;21(6):1983.
Yi T, Wang J, Zhu K, Tang Y, Huang S, Shui X, Ding Y, Chen C, Lei W. Aryl hydrocarbon receptor: a new player of pathogenesis and therapy in cardiovascular diseases. Biomed Res Int. 2018;2018:6058784.
Wang J, Chen D, Cheng XM, Zhang QG, Peng YP, Wang LJ, He SQ, Gong JB. Influence of phenotype conversion of epicardial adipocytes on the coronary atherosclerosis and its potential molecular mechanism. Am J Transl Res. 2015;7(10):1712–23.
Mancio J, Pinheiro M, Ferreira W, Carvalho M, Barros A, Ferreira N, Vouga L, Ribeiro VG, Leite-Moreira A, Falcao-Pires I, et al. Gender differences in the association of epicardial adipose tissue and coronary artery calcification: EPICHEART study: EAT and coronary calcification by gender. Int J Cardiol. 2017;249:419–25.
Masoudi S, Hassanzadeh Nemati A, Fazli HR, Beygi S, Moradzadeh M, Pourshams A, Mohamadkhani A. An increased level of aryl hydrocarbon receptor in patients with pancreatic cancer. Middle East J Dig Dis. 2019;11(1):38–44.
Jackson EN, Thatcher SE, Larian N, English V, Soman S, Morris AJ, Weng J, Stromberg A, Swanson HI, Pearson K, et al. Effects of aryl hydrocarbon receptor deficiency on PCB-77-induced impairment of glucose homeostasis during weight loss in male and female obese mice. Environ Health Perspect. 2019;127(7):77004.
Acknowledgements
The authors thank the Biostatistics Task Force of Taichung Veterans General Hospital, Taichung, Taiwan, for carrying out statistical analysis.
Funding
This work was supported by a grant from Taichung Veterans General Hospital, Taichung, Taiwan [Grant Number TCVGH-1123501C] and the Ministry of Science and Technology, Taiwan [Grant Number MOST 110-2314-B-075A-004-MY3]. The funding agencies did not have any role in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
YC participated in data interpretation and the writing of the manuscript. WM participated in the writing of the manuscript. YL contributed to data interpretation. JW contributed to data interpretation. KL participated in the study design, data collection, and data interpretation. WJ participated in the study design and data collection. HL contributed to the study design and data collection. WS participated in the study design, data collection, and data interpretation. IL contributed to the study design, the collection, the interpretation of the data, and the revision of the manuscript. IL is the guarantor of this work, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Taichung Veterans General Hospital, Taiwan (IRB TCVGH No: C07220A) and written consent was obtained before the start of any procedure.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, YC., Ma, WC., Li, YH. et al. Plasma aryl hydrocarbon receptor associated with epicardial adipose tissue in men: a cross-sectional study. Diabetol Metab Syndr 15, 188 (2023). https://doi.org/10.1186/s13098-023-01166-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01166-y