Abstract
Background
The study aimed to identify transcripts of specific ion channels in rat ventricular cardiomyocytes and determine their potential role in the regulation of ionic currents in response to mechanical stimulation. The gene expression levels of various ion channels in freshly isolated rat ventricular cardiomyocytes were investigated using the RNA-seq technique. We also measured changes in current through CaV1.2 channels under cell stretching using the whole-cell patch-clamp method.
Results
Among channels that showed mechanosensitivity, significant amounts of TRPM7, TRPC1, and TRPM4 transcripts were found. We suppose that the recorded L-type Ca2+ current is probably expressed through CaV1.2. Furthermore, stretching cells by 6, 8, and 10 μm, which increases ISAC through the TRPM7, TRPC1, and TRPM4 channels, also decreased ICa,L through the CaV1.2 channels in K+ in/K+ out, Cs+ in/K+ out, K+ in/Cs+ out, and Cs+ in/Cs+ out solutions. The application of a nonspecific ISAC blocker, Gd3+, during cell stretching eliminated ISAC through nonselective cation channels and ICa,L through CaV1.2 channels. Since the response to Gd3+ was maintained in Cs+ in/Cs+ out solutions, we suggest that voltage-gated CaV1.2 channels in the ventricular myocytes of adult rats also exhibit mechanosensitive properties.
Conclusions
Our findings suggest that TRPM7, TRPC1, and TRPM4 channels represent stretch-activated nonselective cation channels in rat ventricular myocytes. Probably the CaV1.2 channels in these cells exhibit mechanosensitive properties. Our results provide insight into the molecular mechanisms underlying stretch-induced responses in rat ventricular myocytes, which may have implications for understanding cardiac physiology and pathophysiology.
Similar content being viewed by others
Background
During the last five decades, scientists have collected a lot of evidence that mechanical stress has a significant impact on the electrophysiological properties of cardiomyocytes. This phenomenon, commonly referred to as mechanoelectric feedback, has been extensively studied [1] and is believed to play a crucial role in the pathophysiology of cardiac arrhythmias [2, 3]. In healthy hearts, this feedback mechanism can involve transmembrane cation fluxes through stretch-activated channels (SACs) [4], which can modulate the membrane potential of cardiac myocytes [5,6,7]. Scientific data have shown that localized stretching of single ventricular or atrial myocytes involves cation flux through cation-nonselective SACs [5], which in turn can affect the membrane potential of these cells. Stretch sensitivity is particularly high in hypertrophied ventricular cardiomyocytes from spontaneously hypertensive rats and in atrial and ventricular cardiomyocytes from patients with end-stage heart failure [8]. In general, the role of cardiomyocyte SACs is not limited to normal heart function but also plays a crucial role in various pathological conditions.
Several studies reported Ca2+ as well as Na+ and K+ permeability in SACs of tissue-cultured embryonic chick cardiac myocytes [9,10,11,12] and rat atrial myocytes [10]. Mechanical stretching has been suggested to increase the amplitude of Ca2+ transients by activating SACs, which, in turn, increases their Ca2+ permeability [12, 13].
Although the L-type Ca2+ channel is considered the main pathway of Ca2+ entry during an action potential (AP) in cardiomyocytes [14, 15], there are several studies showing that uniaxial stretching does not affect the L-type Ca2+ current (ICa,L) in single cardiomyocytes [16,17,18,19]. However, in our previous studies, we observed inhibition of ICa,L during uniaxial stretching using a glass stylus [6, 8]. This inhibition was attributed to the intracellular accumulation of Ca2+ due to the Ca2+ influx through SACs. To date, no studies have been conducted that examined the dependence of the value of ICa,L on the degree of axial cell stretching. Although there may be no significant changes in ICa,L by uniaxial stretch in a voltage clamp experiment, extra Ca2+ may still enter the cell through L-type Ca2+ channels during prolongation in the depolarization phase of AP due to delayed voltage-dependent inactivation, which partly contributes to the increase in the amplitude of the Ca2+transients [6, 20]. To examine the effects of cell stretching on L-type Ca2+ channels in rat ventricular myocytes, we investigated the operation of these channels under different degrees of dosed stretching.
In addition, to understand the function of operative SACs and Ca2+ channels, RNA reads encoding all existing channels in adult rat ventricular myocytes were examined. The data obtained showed the maximum number of RNA reads for the CaV1.2 channels, which exhibit additional mechanosensitive properties. Among mechanosensitive channels, we identified significant amounts of transcripts for transient receptor potential ion channels, including (melastatin) TRPM7, (canonical) TRPC1, and TRPM4.
Materials and methods
Animals
The experiments were conducted in compliance with the Guide for the Care and Use of Laboratory Animals (8th edition, 2011) published by the US National Institutes of Health, and the experimental protocol was approved by the Ethics Committee of the Russian National Research Medical University. Male outbred Wistar rats (n = 34) weighing between 220 and 270 g (10–12 weeks) were housed in a standard T4 cage in a 12:12 h light : dark cycle and given ad libitum access to food for four weeks prior to the start of the experiment.
Solutions
Ca2+-free physiological salt solution (Ca2+-free PSS) containing (in mM: 118 NaCl, 4 KCl, 1 MgCl2, 1.6 NaH2PO4, 24 NaHCO3, 5 sodium pyruvate, 20 taurine, and 10 glucose, adjusted to pH 7.4 with NaOH (bubbled with carbogen 95% O2 + 5% CO2). Enzyme medium containing: Ca2+-free PSS supplemented with 10 µM CaCl2, 0.2 mg ml− 1 collagenase (Type II, Worthington, 225 U mg− 1), and 1 mg ml− 1 bovine serum albumin (Sigma). Before the actual experiments, cells were stored for at least 2 h in a modified Kraftbrühe (KB) medium, containing (mM): 50 L-glutamic acid, 30 KCl, 3 MgSO4 × 7H2O, 20 taurine, 10 glucose, 30 KH2PO4, 0.5 EGTA, and 20 HEPES, adjusted to pH 7.3 with KOH [6]. The isolated cells were stored in KB medium for up to 8 h. Ventricular cardiomyocytes were perfused with a solution (37 oC) containing (mM): 150 NaCl, 5.4 KCl, 1.8 CaCl2, 1.2 MgCl2, 20 glucose, and 5 HEPES, at pH 7.4, adjusted with NaOH (K+ out solution). Internal pipette solution containing (mM): 140 KCl, 5 Na2ATP, 5 MgCl2, 0.01 EGTA and 10 Hepes/KOH at pH 7.3 (K+ in solution). Later in the text, this configuration is referred to as K+ in/K+ out solutions. In some experiments, we suppressed inward rectifying K+ currents by substituting Cs+ for extracellular K+ and reduced outward rectifying K+ currents by replacing K+ with Cs+ in the intracellular (electrode) solution. Below in the text, this configuration is referred to as Cs+ in/Cs+ out solutions. For this, in a perfusion solution, 5.4 mM KCl was replaced by 5.4 mM CsCl (extracellular Cs+оut solution), while in the patch pipette solution, 140 mM KCl was replaced by 140 mM CsCl (intracellular Cs+ in solution) [5]. With suppressed K+ currents, the peak L-type Ca2+ current can be approximated by subtracting the late current (IL) from the most negative current surge [21]. A similar substitution was made to separate the effects of non-selective cation currents Ins [5, 6].
Isolated cardiomyocyte preparation
We followed a modified version of the previously described cell isolation procedure [5, 6]. Male Wister rats were anesthetized with an intraperitoneal injection of 80 mg kg-1 ketamine and 10 mg kg-1 xylazine, with heparin (1000 U kg-1) added to the anesthetic solution to prevent blood coagulation in the coronary vessels of the excised heart. The chest was opened, and the heart was rapidly excised and attached to a Langendorff apparatus with a constant flow of 1 ml min-1 at 37 °C to flush the coronary vessels in carbogen-bubbled Ca2+-free PSS for 5 min. After this initial perfusion, hearts were retrogradely perfused with the same PSS supplemented with Worthington type II collagenase (0.5 mg ml-1), 1 mg ml-1 bovine serum albumin (Sigma), and 10 µM CaCl2 for 18–20 min. The perfusate was continuously bubbled with carbogen (95% O2 + 5% CO2), and the temperature was equilibrated at 37 °C. The enzymes were then washed out with a modified KB medium [22], and the heart was disconnected from the perfusion system. The ventricles were then cut off, chopped, and gently triturated to release the cells into the KB medium. The resulting cell suspension was filtered and stored in KB medium at 22 °C prior to use.
mRNA isolation and purification
mRNA was isolated directly from cardiomyocytes using Oligo-dT25 Dyna beads® (Invitrogen). The mRNA-bound beads were washed in a Tris buffer solution containing lithium dodecyl sulfate (LiDS) or without LiDS (Buffer A: 10 mM TrisHCl (pH 7.5); 0.15 M LiCl; 1 mM EDTA; 0.1% LiDS; Buffer B: 10 mM TrisHCl (pH 7.5); 0.15 M LiCl; 1 mM EDTA). The beads were resuspended in RNase-free water (Sigma, Dorset, UK), and the mRNA was reverse transcribed using cloned AMV reverse transcriptase (Invitrogen). The resulting cDNA was stored at -80 °C until necessary.
RNA sequencing and analysis
The obtained libraries were analyzed for concentration, size distribution, and quality using a dsDNA high sensitivity kit (Invitrogen, Carlsbad, CA, USA) on a Qubit 4 fluorometer (Thermo Fisher Scientific, Inc., Dreieich, Germany) and a high sensitivity D5000 kit (Agilent, Santa Clara, CA, USA) on a 4200 TapeStation. Libraries were normalized according to their molarity, pooled, and then quantified with a library quantification kit for Illumina platforms (Roche, Basel, Switzerland) using a StepOnePlus qPCR machine (Thermo Fisher Scientific, Inc., Dreieich, Germany). The resulting pooled libraries were loaded at 350 pM with 1% PhiX on an S2 FlowCell and sequenced in triplicate using a NovaSeq 6000 next-generation sequencer (Illumina, San Diego, CA, USA) with paired-end reads of 2 × 150 bp.
Raw FASTQ - sequenced reads were first assessed for quality using FastQC v0.11.5 (available online at http://www.bioinformatics.babraham.ac.uk/projects/fastqc/) [23]. The reads were then passed through Trimmomatic v0.36 [24] for quality trimming and adapter sequence removal. The surviving trimmed read pairs were then processed with Fastp [25] to remove poly-G tails and Novaseq/Nextseq-specific artifacts. Following the quality trimming, the reads were assessed again using FastQC. Post - QC and QT, the reads were aligned to the human reference genome GRCh38.p4 using HISAT2 [26] with default parameters, and the resulting SAM alignments were then converted to BAM format and coordinate sorted using SAM Tools v1.3.1 [27]. Finally, the sorted alignment files were analyzed with HTSeq-count v0.6.1p1 [28] using the options (-s no -t exon -I gene_id) for raw count generation.
Unless otherwise stated, all experiments were performed with at least three replicates, and the data are represented as the mean ± standard error (SE).
Compounds
In certain experiments, nifedipine (Sigma-Aldrich), a specific blocker of the L-type Ca2+ channel [29], was added to the bath solution at a concentration of 5–10 µM to assess the pharmacological specificity of the observed Ca2+ currents [30, 31]. At these concentrations, nifedipine selectively blocks ICa,L without affecting the T-type Ca2+ current (ICa,T), the fast Na+ current, the delayed rectifier current (IK), or the hyperpolarization-activated inward current [29]. Isoproterenol, a ß-adrenergic stimulator, dose-dependently stimulated ICa,L in isolated cardiac myocytes, reaching a plateau at 100 nM. The effect of isoproterenol (Sigma-Aldrich) (20 nM) on the peak current amplitudes of ICa,L at 0 mV was considered a test of the quality of isolated cells. Gadolinium (Gd3+) (Sigma-Aldrich), known as a non-specific blocker of mechanically gated channels in the ISAC (current through stretch activated channels) [5, 6], was added to the PSS (5 µM GdCl3), BAPTA (Tocris), and 1,2-bis(2-aminophenoxy)ethane-N,N,N’,N’-tetraacetic acid.
Mechanical stretch of the ventricular myocytes
The mechanical stimulation method used in this study has previously been described in detail. Here, we only report the peculiarities relevant to this study. After whole-cell access with the patch pipette (P), a fire-polished glass stylus (S) was attached to the membrane [5, 6, 22, 32]. When the stylus was newly polished and the surface membrane was clean, the attachment was successful in approximately 70% of the attempts. The stylus was then lifted 2 μm to prevent ‘scratching’ of the lower cell surface on the coverslip during the stretch. A motorized micromanipulator (MP 285, Sutter, Novato, Calif., USA, accuracy 0.2 μm) increased the S-P distance stepwise by up to 12 μm, with P being the fixed point [5, 22]. Stretch and release of stretch could be repeated 3–4 times with the same cell, on average. Our method was shown to stretch the cell surface locally, while the membrane in the line between P and S was stretched as expected (approximately 80% of the entire membrane surface remains unaffected) [5, 22]. The effect of mechanical stretching on the sarcomere pattern was imaged by a slow-scan CCD camera (Princeton Instruments, Trenton, N.J., USA) and evaluated by Meta Morph software (Universal Imaging, West Chester, PA, USA). S and P were positioned 40 μm apart before attaching them to the cell. Cell stretching by 4 μm (increasing the S - P distance) increased local stretching by approximately 6%, by 6 μm about 10%, by 8 μm about 14%, and by 10 μm about 18%. These values were less than expected but close to those previously obtained in isolated mouse cardiomyocytes. Presumably, the extent of local stretch decays from the cell surface to the interior of the cell, where the optical focus was set [6, 22].
To investigate the effect of cell stretch at 4, 6, 8, and 10 μm on ICa,L values, measurements were taken. A standard elongation of 6 μm was used to study ICa,L on the background of cell elongation under the action of various compounds.
Whole-cell patch-clamp
A total of 113 cells (n = 113) were used in the experiments. Whole-cell patch-clamp recordings of K+, Ca2+, and non-selective (Ins) currents were obtained using an Axopatch 200B amplifier and pClamp 10 software (Molecular Devices, San Jose, CA, USA). The data were filtered at 2 kHz, sampled at 5 kHz, and analyzed using the same software. Myocytes were superfused in a small recording chamber (RC-26; Warner Instrument Corp., Brunswick, CT, USA) with a volume of 150 µl, which was mounted on an inverted microscope.
The borosilicate glass patch-clamp electrodes had tip resistances ranging from 1.5 to 2.5 MΩ when filled. Cell access was obtained by rupturing the patch after seal formation. Pulses of 140 ms and 350 ms were applied at 1 Hz, starting from a holding potential (Vhp) of − 45 mV, which caused the inactivation of tetrodotoxin (TTX)-sensitive Na+ currents. To evaluate membrane capacitance and access resistance, currents in response to trains of short (5 mV) pulses applied at − 45 mV were taken without compensation for capacitive and leak currents. Cells with similar geometry were selected based on their length and diameter (control rat ventricular cardiomyocytes had an average diameter of 25 ± 6 μm), and, on average, had a membrane capacitance of 150 ± 16 pF (n = 16) and an input resistance of 58 ± 5 MΩ (in 16 representative cells). Glass tools were adjusted to the same 40 μm S -P distance before the application of stretch to minimize the effect of differences in the size of the stretched membrane. Since the area of mechanical stretching was small and unknown, we did not divide the stretch-induced currents by the entire membrane capacitance.
Currents through L-type Ca2+ channels, membrane currents at the end of the pulse (late current: IL), and other currents were plotted as functions of their respective clamp step potentials. The seal resistance remained constant, i.e. it was 1.5 ± 0.3 GΩ before and 1.4 ± 0.4 GΩ during the stretch. Similarly, access resistance and membrane capacitance remained unaffected, indicating that the stretch-induced inward current was due to the activation of an ionic current rather than leakage around the seal. The zero current potential (V0) for IL was determined by the intercept of the resulting I/V curve with the voltage axis and corresponded to the resting membrane potential of a non-clamped cell (between − 70 and − 80 mV). Online records of net membrane current were carried out at Vhp = − 45 mV (time course) [6, 22, 33].
Typically, the measurements lasted approximately 30 min, during which time the access resistance and capacitive current remained stable. To obtain the current-voltage relations (I/V curves), a series of 20 pulses of 140 ms (or 350 ms) duration were applied, starting from Vhp = − 45 mV.
Freshly isolated brick-like cardiomyocytes can attach to the glass bottom in two different positions: edgewise, staying on the narrow side, and broadwise, staying on the broad side [34]. However, the response to stretching is identical in cardiomyocytes occupying both positions (edgewise and broadwise). On the other hand, the response to compression differs depending on the cell’s position [34, 35]. For our experiments, we selected cells that stayed on the narrow side (edgewise) and had similar sizes.
In this study, ICa,L recordings are presented in both absolute values (e.g., pA) and normalized form (e.g., pA/pF). However, changes in ICa,L in response to cell stretching or treatment with compounds are presented as the difference between ICa,L under control conditions and that under stretching or treatment conditions.
Statistics
Values are presented as means ± SD. To determine significant differences, we used Analysis of Variance (ANOVA) with the Bonferroni test as a post-hoc analysis. For cases where multiple factors were evaluated, a two-way ANOVA was performed. Statistical significance was set at p < 0.05.
Results
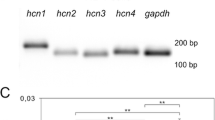
The levels of the channel’s gene expression
In this study, we used RNA-seq to measure the expression levels of various genes in freshly isolated rat ventricular cardiomyocytes. Our analysis revealed the presence of RNA reads encoding different ion channels, as summarized in Table 1 [36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92], and illustrated in Fig. 1. Specifically, we found that NaV channel transcripts were expressed in these cells, with NaV1.5 showing the highest number of RNA reads (3654.4 ± 581.2), followed by NaV1.1 (only 179 ± 30), [81, 82]. The expression of other NaV channels was minimal. Importantly, previous research has shown that NaV1.5 exhibits mechanosensitivity [81, 82], which may have physiological implications for the function of rat ventricular cardiomyocytes.
Our analysis revealed the presence of three CaV subfamilies: CaV1.2, CaV1.3, and CaV1.1, as shown in Fig. 1. Of these, the CaV1.2 channels had the highest number of RNA reads (1336.66 ± 71.8), with the transcripts of the other CaV channels being an order of magnitude smaller. In particular, previous studies have shown that CaV1.2 and CaV1.3 both exhibit mechanosensitivity [84] (Table 1; Fig. 1). When considering the L-type CaV channels, which are responsible for the L-type Ca2+ current, we found that the CaV1.2 transcripts were significantly more abundant than the CaV1.3 transcripts (17.33 ± 2.03), while the number of CaV1.1 transcripts was very low (Table 1). Based on these results, we conclude that CaV1.2 is likely the primary channel that contributes to the L-type Ca2+ current in rat ventricular cardiomyocytes and that CaV1.3 and CaV1.1 can be neglected. This finding is consistent with previous research indicating that CaV1.2 channels are the main contributors to the L-type Ca2+ current [84].
Among the multitude of KV channel transcripts (Fig. 1), the KV7.1 or KCNQ1 channel had the highest number of RNA reads (821.00 ± 77.20), consistent with previous studies showing its response to membrane stretch [88] and hypo-osmotic swelling [88, 89] (Table 1). The KV1.2 channel, which has also been shown to exhibit mechanosensitivity [67], was present in smaller quantities with 212.00 ± 10.02 RNA reads (Table 1; Fig. 1). In particular, the number of KV1.2 transcripts was 3.5 times less than that of the predominant KV7.1 (Fig. 1).
Among K2P channels, TREK-1/K2P2.1 had the highest number of RNA reads (153.00 ± 11.93) compared to others, consistent with its established mechanosensitivity [75,76,77]. TRAAK/K2P4.1 channels also exhibit mechanosensitivity [76, 93], although the number of detected RNA reads was very small (0.66 ± 0.33) (Table 1; Fig. 1). Interestingly, transcripts of the mechanosensitive channels TREK-2/K2P10.1, which are expressed in the atrial and ventricular cells of human and murine hearts [76], were not detected in our isolated rat ventricular myocytes.
The RNA-seq technique revealed the presence of several Kir channel transcripts (Fig. 1) in freshly isolated rat ventricular cardiomyocytes. Among them, Kir6.2 (1240.66 ± 57.1) was detected in the highest abundance and demonstrated mechanosensitivity only when associated with the sulfonylurea receptor 2 A (SUR2A) subunit [91] (Table 1; Fig. 1). Additionally, RNA reads were found for Kir6.1 channels (82.66 ± 6.49), which are also mechanosensitive [92]. However, unlike mouse ventricular cardiomyocytes, where Kir2.3 channels have been shown to be mechanosensitive [22], we did not detect any RNA reads for Kir2.3 channels in rat ventricular cardiomyocytes.
We identified three types of stretch-activated KCa (SAKCA), or BKCa channels, that exhibit mechanosensitivity [78]: calcium-activated potassium channel subunit beta-2 (KCNMB2) (6.6 ± 0.9), KCNMB4 (2.7 ± 0.9), and KCNMB1 (0.3 ± 0.3) (Table 1; Fig. 1). Although ATP-sensitive potassium channels (KATP) also exhibit mechanosensitivity in rats [41, 80], we did not investigate their presence in our study. Likewise, we did not analyze the expression of Kv7 (KCNQ) channels [88,89,90].
We observed several transcripts for nonselective cation TRP channels, many of which are known to be mechanically gated (listed in descending order of RNA reads). In particular, mechanosensitive TRPM7 (333.5 ± 31.5) [36,37,38,39, 94], TRPC1 (146.66 ± 6.96) [40, 42, 43], TRPM4 (179.66 ± 5.93) [44,45,46,47, 95], TRPV2 (21.66 ± 2.03) [48, 49], TRPC3 (5.0 ± 3.0) [50,51,52,53,54,55, 96], TRPV4 (5.5 ± 0.5) [56,57,58], TRPV1 (2.00 ± 0.58) [59, 60], TRPM3 (1.3 ± 0.9) [61], TRPC5 (1.3 ± 0.9) [62, 97], TRPA1 (1.0 ± 0.9) [63,64,65], and TRPC6 (1.0 ± 1.0) [22, 47, 66, 67, 97] were among the most abundant.
We also identified two additional stretch-activated channels, Piezo 1 (145.33 ± 8.01) [71,72,73, 98, 99], and Piezo 2 (6.0 ± 2.0) [73, 74], that were present in the ventricular cardiomyocytes of rats.
The data presented here and below reveal an intriguing observation: While many ion channels have been studied in terms of their response to membrane stretch, only a few have been thoroughly investigated. However, among those that have been studied, all demonstrate a certain degree of mechanosensitivity. On the basis of this, it is plausible to speculate that mechanosensitivity is a ubiquitous characteristic of ion channels and that all channels, irrespective of their gating mechanism, should respond to membrane stretch and tension.
Definition and analysis of L-type Ca 2+ current
In this study, two methods were used to estimate the current through L-type Ca2+ channels (ICa,L) in K+ in/K+ out solutions. The first method involved evaluating the time course of ICa,L by subtracting the late current at the end of the 140 ms pulse from the negative peak current (Fig. 2A). The second method involved determining the current-voltage (I/V) relationship for ICa,L by subtracting the current at the same potential in the presence of 5 or 10 µM nifedipine from the maximum point of the negative peak current (Fig. 2B). The value of IL at 0 mV was almost equal to the current in the presence of nifedipine (Fig. 2A). The negative peak current at 0 mV in control conditions (blue track) and in the presence of 10 µM nifedipine (red track), which selectively blocks L-type Ca2+ channels, was used to estimate ICa,L. ICa,L was calculated by taking the difference between the negative peak current and the current in the presence of nifedipine (or by subtracting the late current at the end of the 140 ms or 350 ms pulse at a frequency of 1 Hz). Since the I/V relation of IL in control (green triangles) completely coincides with the I/V relation for ICa,L in the presence of nifedipine (red circles) in the range from − 80 mV to + 50 mV (Fig. 2B), the calculation method presented in previous study for K+ in/K+ out solutions was applied [21], whereas ICa,L was estimated as the difference between the negative current at − 10 mV (blue circle) and either the current in the presence of nifedipine at − 10 mV (red circle) or the late current at − 10 mV in control (green triangles) (Fig. 2B).
It should be noted that in K+ in/K+ out solutions, the positive peak on the I/V relation for ICa,L between − 30 and − 70 mV (Fig. 2B: blue circles) is associated with the positive currents in response to voltage steps in this potential range and was first demonstrated by Josephson and Sperelakis (1982), [100]. However, not all subsequent studies on ICa,L took this positive peak into account.
Evaluation of ICa,L and Ins in K+ in/K+ out and Cs+ in/Cs+ out solutions. The membrane potential (Vm) was maintained at Vhp = − 45 mV. A: Raw recordings of IL and ICa,L (blue trace) and recordings in the presence of nifedipine (red trace) in K+ in/K+ out solutions. B: Current-voltage (I/V) relationships for IL (green triangles) and peak ICa,L (blue circles) under control conditions and in the presence of nifedipine (red circles). C: Raw recordings of IL and ICa,L (blue trace) and recordings in the presence of nifedipine (red trace) in Cs+ in/Cs+ out solutions, where K+ currents are suppressed. D: I/V curves for IL (blue triangles) and ICa,L (blue circles) under control conditions and in the presence of nifedipine (red circles)
Figure 2 C shows that in Cs+ in/Cs+ out solutions, the negative peak current at 0 mV in control conditions (blue track) and in the presence of 10 µM nifedipine (red track) were used to estimate ICa,L by taking the difference between the peak current and the current in the presence of nifedipine or the late current at the end of the pulse. Figure 2D shows the I/V relations for ICa,L in control conditions (blue circles) and in the presence of nifedipine (red circles). In this case, ICa,L was calculated as the difference between the negative current (blue circles) and the current in the presence of nifedipine (red circles) or when the current equals 0 nA. The I/V relations for IL measured at the end of the pulse are shown under control conditions (blue triangles) and in the presence of nifedipine (red triangles). Our experiments used an internal pipette solution containing 0.01 mM EGTA, and under these conditions, we measured the ICa,L value when cells were stretched by 4, 6, 8, and 10 μm. Previous studies have shown that the reduction of ICa,L, even by a stretch of 10 μm, was no longer observed when the cells were pre-dialyzed with 5 mM BAPTA, i.e., control ICa,L and ICa,L during stretch superimposed [6]. To study ICa,L in the context of cell elongation under the action of various compounds, a standard elongation of 6 μm was used in this study.
As demonstrated earlier in K+ in/K+ out solutions, the late current (IL) at the end of the pulse reflects the cell’s response to stretching. Stretch-induced changes in IL exhibit an outward rectifying voltage dependence with a reversal potential (Erev) of − 16 mV [5, 6]. To calculate stretch-induced current (ΔSIL), we take the difference between the control current values (CIL) and the current values in the presence of cell stretching (SIL) at − 45 or − 80 mV (ΔSIL(−45) and ΔSIL(−80)) [5].
In our earlier work conducted on isolated mouse ventricular cardiomyocytes [5, 6], as well as in studies by our colleagues on the same cells [22], it was found that in K+ in/K+ out solutions, the net current was composed of Ins (current through stretch-activated non-selective cation channels), IK1 (inwardly rectifying potassium current), and Io (presumably the sum of several outwardly rectifying currents, such as K+ currents through TREK channels [76, 77] or the outwardly rectifying canonical transient receptor potential-6 (TRPC6) channels [66]. Cell stretch can modify net membrane currents (ΔSIL) by modulating both K+ and Ins currents [5]. However, our present studies investigating the RNA transcripts of ion channels and their mechanosensitivity reveal significant differences in the channel spectrum of ventricular cardiomyocytes in adult rats (see below).
To distinguish the effects on Ins, we used two methods: first, we eliminated inward rectifying K+ currents by substituting extracellular K+ with Cs+ and second, we decreased outward rectifying K+ currents by replacing intracellular K+ with Cs+. In this case, the current through stretch-activated channels (ISAC) was calculated as the difference between the control current values (CIns) and the current values on the background of cell stretching (SIns) at − 45 or − 80 mV (ISAC(−45) and ISAC(−80)). We used the same approach to measure the differential current in response to specific compounds (ΔIX) (where “X” represents the compound) at − 45 or − 80 mV [5, 6].
Under our experimental conditions, isolated cardiomyocytes maintained their fundamental properties, as demonstrated by the significant increase in ICa,L peak current amplitudes at 0 mV in response to 20 nM isoproterenol in K+ in/K+ out and Cs+ in/Cs+ out solutions (not shown), which is consistent with previous literature reports for this compound [101].
Local stretch increased net currents I L and decreased I Ca,L in K + in /K + out solutions (time-course and voltage-dependence)
Figure 3A.1 illustrates the effect of a 6 μm cell stretch on time-dependent net membrane currents in K+ in/K+ out solutions. At control, the registered holding current (the current at Vhp = − 45 mV (Ihc)) was + 0.44 nA (label C, Fig. 3A.1), and stretch changed this current (SIhc) to + 0.27 nA (label S, Fig. 3A1). The stretch-induced difference of the holding current ΔSIhc was (-) 0.17 nA ((-) 0.19 ± 0.01 nA, n = 14) at − 45 mV. The minus sign (-) emphasizes that cell stretch leads to more negative values of the initial net holding current at the level of Vhp = − 45 mV. The pulse to 0 mV induced the L-type Ca2+ current (ICa,L) that activated and inactivated over time. The stretch attenuated the L-type Ca2+ current (Fig. 3A.1), which was estimated as the difference between the negative peak current Imax and the current at the end of the pulse in control (IL) (from |1.55| nA to |1.11| nA during the stretch). The module for ICa,L was used because the current value was calculated as a distance (Fig. 3A.1, B.2, C.2) from the starting point (the value of ICa,L on the background of nifedipine = IL, in the positive region) to the point Imax, in the negative region. The time course of the stretch - induced difference of the L-type Ca2+ current in the control and during the stretch (ΔSItcCa,L) was (+) 0.44 nA ((+) 0,44 ± 0.07 nA, n = 7). The plus sign indicates that cell stretching at the Vhp = − 45 mV led to a shift of negative ICa,L to more positive values compared to the initial values, resulting in a decrease in the negative area.
The I/V curves in Fig. 3A.2 show the voltage dependence of IL and ICa,L, and their modulation by a 6 μm stretch. Before stretching, the IL - I/V curve was N-shaped and crossed the voltage axis (zero current potential V0) at − 78 mV (− 75 ± 3 mV, n = 7; equivalent to the resting potential of the non-clamped cell). The modest stretch shifted the net currents IL to more negative values: ΔSIL(− 45) is (-) 0.15 nA ((-) 0.16 ± 0.02 nA, n = 7) at − 45 mV and ΔSIL(−80) is (-) 0.24 nA ((-) 0.26 ± 0.03 nA, n = 7) at − 80 mV. The V0 also shifted to -70 mV (− 66 ± 3 mV, n = 7) with the stretch.
During cell stretching, although the changes in the SIL(− 45) current occur in the positive range, their values are lower than the control values of IL(−45). The minus (-) sign of ΔSIL(−45) emphasizes that cell stretch leads to a change in the curve toward more negative values. Similarly, for IL(−80), which is usually in the negative range, cell stretch further increases this negative current SIL(−80), leading to a negative differential current ΔSIL(−80) that only shows the direction of its change. The I/V curves recorded before and during the stretch crossed each other close to 0 mV, and at positive potentials, the late current increased with the stretch. The I/V curve of ICa,L decreased during the 6 μm stretch by ΔSICa,L = (+) 0.38 nA ((+) 0.32 ± 0.04 nA, n = 7) compared to the control values.
Upon stretching to 8 μm, the holding current SIhc decreased to values close to 0 (label S, Fig. 3B.1), compared to the control holding current (label C, the beginning of the blue tracesin this figure). In this case, the stretch-induced difference in the holding current ΔSIhc was (-) 0.41 nA ((-) 0.42 ± 0.02 nA, n = 7) at Vhp = − 45 mV. The pulse at 0 mV induced ICa,L, and the stretch attenuated ICa,L (Fig. 3B.1, negative current wave from blue in control to red during the stretch) from |1.55| nA in control to |0.94| nA. During time course registration, the stretch-induced difference of L-type Ca2+ current in control and during the stretch, ΔSItcCa,L equals (+) 0.61 nA ((+) 0,60 ± 0.04 nA, n = 7).
Stretching by 8 μm shifted the I/V relation to more negative currents than a 6 μm stretch (Fig. 3B.2): At − 45 mV, the stretch-induced difference in current was ΔSIL(−45) = (-) 0.29 nA ((-) 0.37 ± 0.06 nA, n = 7), while at − 80 mV, it was ΔSIL(−80) = (-) 0.57 nA ((-) 0.60 ± 0.09 nA, n = 7), and V0 was depolarized to -56 mV (− 54 ± 3 mV, n = 7). The I/V curve of ICa,L during the stretch showed a further decrease in SICa,L, resulting in an increase in the differential current ΔSICa,L to (+) 0.52 nA ((+) 0.52 ± 0.02 nA, n = 7).
The maximum stretch of 10 μm caused a shift in the holding current SIhc to the negative region with values equal to − 0.16 nA (label S, the beginning of the red traces in Fig. 3C.1, compared to label C, the beginning of the blue traces). The stretch-induced difference in the holding current ΔSIhc was (-) 0.61 nA ((-) 0.74 ± 0.10 nA, n = 7) at − 45 mV. This stretch resulted in a further reduction of ICa,L (Fig. 3C.1: negative current wave from blue in control to red during the stretch) from |1.55| nA in control to |0.77| nA. When registering the time course, ΔSItcCa,L was equal to (+) 0.78 nA ((+) 0.77 ± 0.04 nA, n = 6).
Stretching the cell by 10 μm caused a larger shift in the I/V relationship to more negative currents compared to an 8 μm stretch (Fig. 3C.2): ΔSIL(−45) was (-) 0.57 nA ((-) 0.71 ± 0.09 nA, n = 6) at − 45 mV, while ΔSIL(−80) was (-)1.33 nA ((-)1.41 ± 0.15 nA, n = 6) at − 80 mV, and depolarized V0 to − 35 mV (− 39 ± 3 mV, n = 6). During this stretch, the I/V curve of ICa,L showed a larger decrease in SICa,L, resulting in an increased differential current ΔSICa,L of (+) 0.66 nA ((+) 0.65 ± 0.05 nA, n = 6).
Reduction of ICa,L in K+ in/K+ out solutions during local stretching of cardiomyocytes by 6, 8, and 10 μm. Vhp = − 45 mV. A: (6 μm stretch). A.1 - The time course of the membrane current. The holding current at Vhp in control (beginning of the blue traces - label C) and during stretching (beginning of the red traces - label S). A pulse from − 45 to 0 mV induces ICa,L, which decreases during stretching (indicated by a negative blue current wave compared to a negative red wave). A.2 – I/V curve of IL before (blue triangles) and during (red triangles) stretching, as well as ICa,L before (blue circles) and during (red circles) stretching. B: (8 μm stretch). B.1 - The time course of the membrane current before and during stretching, which results in a greater reduction of ICa,L compared to A.1. Notations as in A.1. B.2 – I/V curves of IL and ICa,L before and during stretching. Notations as in A.2. C: (10 μm stretch). C.1 – The time course of the membrane current in control and during stretching. ICa,L decreases with increasing stretching. Notations as in A.1. C.2 – I/V curves of IL and ICa,L before and during stretching. Notations as in A.2
In K+ in/K+ out solutions, Gd3+ eliminates stretch-induced reduction in ICa,L at all levels of cell stretch, as previously demonstrated [5, 6].
The comparison of the mean values of differential currents ΔSIhc, ΔSIL(−45), ΔSIL(−80), ΔSItcCa,L and ΔSICa,L during cell stretch at 6, 8, and 10 μm is presented in Fig. 4. It should be noted that ΔSIhc, ΔSIL(−45), and ΔSIL(−80) are mechanosensitive and are based on the activation of stretch-activated channels (SAC).
Local stretch increased current through nonselective cation channels I ns and, at the same time, reduced I Ca,L in Cs + in /Cs + out solutions (time course and voltage dependence).
In Fig. 5A.1, the effect of 6 μm stretch on time-dependent membrane currents in Cs+ in/Cs+ out solutions is presented. At the control stage, the holding current was 0 nA (labeled as C, Fig. 5A.1), while stretch resulted in negative holding current values (labeled as S, Fig. 5A.1). The difference in the holding current induced by stretch was (-) 0.12 nA (0.09 ± 0.01 nA, n = 7) at − 45 mV. The pulse to 0 mV resulted in an L-type Ca2+ current of − 1.49 nA (− 1.62 ± 0.13 nA, n = 18), or − 7.3 pA/pF (− 7.1 ± 0.2 pA/pF, n = 18). The stretch of 6 μm reduced the L-type Ca2+ current, SICa,L (as shown by the negative current wave in Fig. 5A.1, from blue to red). During the recording of the time course, the stretch-induced difference of L-type Ca2+ current in control and during the stretch (ΔSItcCa,L) was (+) 0.41 nA ((+) 0.35 ± 0.05 nA, n = 7).
Figure 5 A.2 displays the voltage dependence of Lns, ICa,L and its modulation by a 6 μm stretch, as shown in the I/V curves. Before stretching, the I/V curve of Ins was linear and intersected the voltage axis (zero current potential V0) at − 40 mV (− 38 ± 3 mV, n = 7). After a modest 6-µm stretch, Ins shifted to more negative values, and the resulting ISAC = SIns - CIns (in Cs+ in/Cs+ out solutions) was (-) 0.10 nA ((-) 0.09 ± 0.02 nA, n = 7) at − 45 mV and (-) 0.14 nA ((-) 0.12 ± 0.01 nA, n = 7) at -80 mV, while V0 changed to − 5 mV (− 6 ± 3 mV, n = 7). At potentials close to 0 mV, the I/V curves recorded before and during the stretch intersected, while at positive potentials, Ins exhibited an increase due to the stretch. Furthermore, the I/V curve of SICa,L during the stretch decreased from − 1.27 nA in the control to − 1.00 nA, resulting in a ΔSICa,L of (+) 0.27 nA ((+) 0.34 ± 0.06 nA, n = 7) when compared to the control values.
When subjected to an 8 μm stretch, the difference in the holding current at − 45 mV changed to values close to (-) 0.17 nA ((-) 0.16 ± 0.301 nA, n = 7; labeled S, Fig. 5B.1, compared to label Cin the figure). The pulse from − 45 to 0 mV induced ICa,L, but the 8 μm stretch attenuated SICa,L (as seen in Fig. 5B.1, where the negative current wave shifts from blue to red during the stretch), from − 1.49 nA in the control to − 0.86 nA. When the time course was registered, ΔSItcCa,L was calculated to be (+) 0.63 nA ((+) 0.64 ± 0.06 nA, n = 7).
The 8 μm stretch caused a shift in the I/V relation to more negative currents compared to the 6 μm stretch (as seen in Fig. 5B.2): ISAC(−45) was (-) 0.16 nA ((-) 0.16 ± 0.02 nA, n = 7) at − 45 mV, and ISAC(−80) was (-) 0.25 nA ((-) 0.18 ± 0.04 nA, n = 7) at − 80 mV. During this stretch, the I/V curve of ICa,L further decreased SICa,L from − 1.27 to − 0.54 nA, resulting in an increase in differential current ΔSICa,L to (+) 0.73 nA ((+) 0.62 ± 0.09 nA, n = 7) compared to control values.
The longest 10 μm stretch caused a shift of the holding current to the negative region (label S, Fig. 5C.1, compared to label C). The stretch-induced difference in the holding current was (-) 0.35 nA ((-) 0.34 ± 0.02 nA, n = 7) at − 45 mV. Furthermore, this stretch reduced SICa,L even more (Fig. 5C.1), from − 1.49 nA in the control to − 0.74 nA. In the case of time course registration, ΔSItcCa,L equals (+) 0.75 nA ((+) 0.75 ± 0.05 nA, n = 7).
Reduction of ICa,L in Cs+ in/Cs+ out solutions with K+ currents suppressed during local stretching of cardiomyocytes by 6, 8, and 10 μm. Vhp = − 45 mV. A: (6 μm stretch). A.1 – The time course of the membrane current. The holding current at Vhp in control (beginning of the blue traces - label C) and during stretching (beginning of the red traces – label S). A pulse from − 45 to 0 mV induces ICa,L, which decreases during stretching (indicated by a negative blue current wave compared to a negative red wave). A.2 – I/V curve of Ins before (blue triangles) and during (red triangles) stretching, as well as ICa,L before (blue circles) and during (red circles) stretching. B: (8 μm stretch). B.1 - The time course of the membrane current before and during stretching, which results in a greater reduction of ICa,L compared to A.1. Notations as in A.1. B.2 – I/V curves of Ins and ICa,L before and during stretching. Notations as in A.2. C: (10 μm stretch). C.1 – The time course of the membrane current in control and during stretching. ICa,L decreases with increasing stretching. Notations as in A.1. C.2 – I/V curves of Ins and ICa,L before and during stretching. Notations as in A.2
Stretching by 10 μm shifted the I/V relation to more negative currents than an 8 μm stretch (Fig. 5C.2). Specifically, ISAC(−45) was (-) 0.32 nA ((-) 0.34 ± 0.05 nA, n = 7) and ISAC(−80) was (-) 0.53 nA ((-) 0.48 ± 0.10 nA, n = 7). The 10-µm stretch further reduced SICa,L to − 0.38 nA (Fig. 5C.2, red circles), resulting in an increase in differential current ΔSICa,L to (+) 0.89 nA ((+) 0.79 ± 0.09 nA, n = 7).
In Cs+ in/Cs+ out solutions, Gd3+ eliminates the reduction of stretch-induced ICa,L as well as ΔSIL(−45), ΔSIL(−80), as previously demonstrated in our studies [5, 6] (not shown in Fig. 5).
Figure 6 compares the mean values of ISAC(hc), ISAC(−45), ISAC(−80), SICa,L, and ΔSICa,L during cell stretching at 6, 8, and 10 μm in Cs+ in/Cs+ out solutions. ISAC(hc), ISAC(−45), and ISAC(−80) are also mechanosensitive currents based on the work of SAC. Additionally, ICa,L is likely to be conducted through CaV1.2 channels and is also mechanosensitive in ventricular rat cardiomyocytes.
Gd 3+ eliminates the L-type Ca 2+ current via Ca V 1.2 channels in K + in /K + out, Cs + in /K + out, K + in /Cs + out and Cs + in /Cs + out solutions
Effect of 5 µM Gd3+ on IL and ICa,L in K+ in/K+ out (A), Cs+ in/K+ out (B), K+ in/Cs+ out (C), and Cs+ in/Cs+ out (D) solutions. Control curves in blue: IL – triangles and ICa,L – circles. Curves in the presence of Gd3+ in red: IL – triangles and ICa,L – circles. Note: C: Switching cell perfusion from K+ in/K+ out solution (IL – black triangles and ICa,L – black circles) to K+ in/Cs+ out solution (IL – blue triangles and ICa,L – blue circles), followed by the application of Gd3+ (IL – red triangles and ICa,L – red circles). While Gd3+ exerts only a minor effect on IL, it eliminates ICa,L in all solutions tested
Figure 7. A, B, C, and D illustrate that ICa,L values remained constant (1.48 ± 0.06 nA, n = 24) under all experimental conditions tested, including K+ in/K+ out, Cs+ in/K+ out, K+ in/Cs+ out, and Cs+ in/Cs+ out solutions. Furthermore, during the transition of cell perfusion from K+ in/K+ out to K+ in/Cs+ out solutions (Fig. 7C), ICa,L values did not change (n = 6). The ICa,L values were determined by calculating the maximum calcium peak current at a given potential at the point on the late current curve that corresponds to that potential. For Cs+ in/Cs+ out solutions, two variants of ICa,L values were presented (Fig. 7B): (1) up to zero and (2) up to a characteristic point on the late current curve. Typically, only the value (1) is used for calculations in the literature.
It has been shown that, on the background of cell stretch, Gd3+ at a concentration of 5 µM blocks ISAC [6]. The addition of Gd3+ abolished the dependence of ISAC on all local stretch values. Our experiments revealed that Gd3+ also had a minor inhibitory effect on the IL current at − 45 and − 80 mV, suggesting that ISAC may have contributed to the net currents of the non-stretched cells. This is depicted in Fig. 7, where the blue triangles indicate the control and the red triangles indicate the application of the blocker (n = 6). Additionally, Gd3+ did not affect the background current, IK1 (Fig. 7A).
To investigate potential changes in L-type Ca2+ current through CaV1.2 channels, we applied Gd3+, which is known to be a nonspecific blocker of the mechanically gated channel’s current ISAC. Our results indicated that the addition of 5 µM of Gd3+ eliminated L-type Ca2+ current in K+ in/K+ out (n = 6), Cs+ in/K+ out (n = 6), K+ in/Cs+ out (n = 6), and Cs+ in/Cs+ out (n = 6) solutions (blue circles in the control compared to red circles after application of the blocker).
Discussion
Channel transcripts and their mechanosensitivity
In ventricular cardiomyocytes, mechanosensitive channels are believed to play a role in the regulation of the contractile properties of the heart [5]. In our experiments, we found significant amounts of transcripts for the mechanosensitive channels TRPM7, TRPC1, and TRPM4 (Table 1).
TRPM7 is a nonselective cation channel that is permeable to both Ca2+ and Mg2+ [102]. It has been shown to contribute to the stretch-induced current in ventricular cardiomyocytes by mediating a Ca2+ influx in response to mechanical stretch [103, 104]. This influx of Ca2+ is believed to activate downstream signaling pathways that regulate contractility [103]. TRPC1 was shown to contribute to the stretch-induced current in ventricular cardiomyocytes by mediating a non-selective cation influx in response to mechanical stretch, which influx is believed to depolarize the cell membrane and contribute to the regulation of contractility [104]. TRPM4 is a Ca2+-activated non-selective cation channel that has been shown to contribute to the stretch-induced current in ventricular cardiomyocytes [45]. It is believed to be activated by Ca2+ influx through other channels such as TRPC1 and TRPM7 [37, 42, 105]. TRPM4 activation is believed to contribute to contractility regulation by modulating the duration of AP [106].
Studies on mechanosensitivity in murine ventricular myocytes have shown a link between stretch-activated TRPC6 channels as well as stretch-deactivated GK1 and especially Kir2.3 channels [22]. GK1 channels are formed by Kir2.1, Kir2.2, and Kir2.3 proteins [107, 108]. In our experiments, we found multiple transcripts of Kir2.1 and Kir2.2 in isolated ventricular myocytes from rats, while Kir2.3 was absent. Therefore, in K+ in/K+ out solutions, the mechanosensitivity of ventricular myocytes is probably determined by the stretch-activated TRPM7, TRPC1, and TRPM4 channels and the stretch-deactivated GK1 (Kir2.1 and Kir2.2) channels. Our findings are consistent with other studies [109], which have shown that ventricular IK1 is based primarily on the heteromeric assembly of the Kir2.1 and Kir2.2 channels, while the Kir2.3 channels are more relevant in the atrium.
The local stretch of cells modulates I Ca,L, probably through Ca V 1.2 channels
One of the main questions of the study was to determine the cause of changes in ICa,L. Our observations showed a decrease in SICa,L with discrete cell stretching, while there was a corresponding increase in ΔSItcCa,L and ΔSICa,L during cell stretching at 6, 8, and 10 μm.
In general, membrane channels (including voltage-gated) are expected to respond to mechanical stimuli because mechanical energy can affect the energy barriers between different conformational states of a channel protein [110]. For example, longitudinal stretching has been shown to modify the gating mechanism of; NaV channels [111], such as NaV1.5 [81, 82] and NaV1.6 [83], CaV channels such as CaV1.2 [84], CaV1.3 [85], and CaV2.2 channels [86], as well as KV channels such as KV1.2 [67], KV1.5, and KV3.2 [87, 112]. In addition, mechanical energy can affect the conformation of proteins associated with cytoskeletal elements [113, 114], such as F-actin [114] and integrins [115]. This can also activate stretch-sensitive kinases (Src, MAP) or phosphatases, which can, in turn, modulate the channel protein by phosphorylation and dephosphorylation [109]. Finally, mechanical stretch can also impact the production rate of reactive oxygen species, or NO, which can modify channel gating through oxidative or nitrosative mechanisms [116], which in turn can play a role in stretch-induced effects on Ca2+ release from the sarcoplasmic reticulum (SR) [116, 117].
The L-type Ca2+ current is responsible for generating the negative current wave observed at the start of the depolarizing clamp step (Fig. 3A.1, B.1, and C.1), as well as the long-lasting plateau of the AP. Interestingly, the local mechanical stretch has been shown to decrease ICa,L, with the reduction being observed across the entire range of clamp potentials. In particular, the voltage dependence of ICa,L appears to remain unchanged under these conditions (see Fig. 3A.2, B.3, and C.4).
In ventricular myocytes, some nonselective channels are known to be activated by an increase in cytosolic calcium concentration ([Ca2+]C) [118]. To investigate whether stretch-induced changes in [Ca2+]C might play a role in these effects, Gannier et al. (1996) conducted experiments in which they prevented possible stretch-induced increments in [Ca2+]C [119]. Interestingly, they have found that chelation of the [Ca2+]C does not have a significant effect on ISAC. However, we observed significant effects of BAPTA on the stretching effects on ICa,L. Specifically, while ISAC in Cs+ in/Cs+ out solutions was found to be insensitive to chelation of [Ca2+]C, the stretch-induced reduction of ICa,L disappeared after dialyzing the cell with 5 mM BAPTA in the patch pipette [6].
Since stretch has been shown to increase [Ca2+]C and BAPTA can chelate cytosolic Ca2+, it is likely that the stretch-induced reduction of SICa,L results from the stretch-induced increase in [Ca2+]C followed by Ca2+-mediated inactivation of the Ca2+ channel (Ca2+-calmodulin interaction with the Ca2+ channel α subunit) [12]. We propose that the primary effect of stretch is to increase [Ca2+]C via an increase in Ca2+ influx through SACs or via Ca2+ release from the SR in the vicinity of the L-type Ca2+ channel. Previous research has suggested that ICa,L can be reduced by an increase in [Ca2+]C and by stimulation of IP (current due to electrogenic sodium pum**) by an increase in [Na+]C. The concept of indirect activation by stretch should also be applied to the current generated by Na+/Ca2+-exchange if [Na+] is elevated by Na+ influx due to ISAC [120] and to K+ channels activated by Ca2+ or Na+ ions [121]. Alternatively, the stretch may increase [Ca2+]C by Ca2+ release from the SR [117].
Cytoskeletal F-actin fibers were found to be involved specifically in ISAC activation and regulation of the CaV1.2 channel gating mechanism. In the context of cell stretch, which has been shown to increase ISAC and decrease ICa,L, treatment with cytochalasin D, a toxin known to depolymerize F-actin, blocks the effects of stretch on late currents and leads to further reduction of ICa,L [8], which also corroborates the effect of cell stretch, probably on the CaV1.2 channel.
We make such an assumption based on the analysis of the transcript quantities for Ca2+ ion channel genes. As we have demonstrated, the transcript counts for the CaV1.2 channel gene are exceptionally high, measuring 1336.66 ± 71.8. In contrary, for CaV1.3, this count is quite low at 17.33 ± 2.03, and for CaV1.1, it is minimal at 0.33 ± 0.33. We did not detect other channels involved in the whole L-type Ca2+ current. Based on these numerical values, we can infer the primary role of the CaV1.2 channel in the formation of the L-type Ca2+ current that we observed.
Voltage-gated current modulation or mechanosensitivity of the (CaV1.2) channel
It is now well established that Gd3+ blocks a range of ion channels, including SACs (mechanically gated non-selective cation channels, MGCns, and mechanically gated potassium channels, MGCK), which was previously assumed in the study by Yang et al. (1989) [122]. In addition, Gd3+ has been found to block several other ion channels, such as BKCa channels cloned from chick ventricular myocytes [123] and delayed rectifier current (IK) in guinea pig single ventricular myocytes, including both IKR (rapidly activated) and IKS (slowly activated), while the background current IK1, was not affected by Gd3+ [124]. Moreover, Gd3+ was a potent INa blocker near the threshold potential for Na+ channels in rabbit ventricular myocytes [122]. It has been demonstrated that Gd3+ is also a potent blocker of L-type Ca2+ channels in isolated guinea pig ventricular myocytes [125].
In our experiments, treatment with the nonspecific inhibitor of ISAC, Gd3+, on the background of cell stretching eliminated both ISAC and ICa,L at all stretching magnitudes and voltage steps relative to the Vhp. This response to Gd3+ was maintained in Cs+ in/Cs+ out solutions, indicating that voltage-gated channels, apparently CaV1.2 in adult rat ventricular myocytes, have additional mechanosensitive properties.
Conclusion
Our analysis revealed the presence of transcripts for the TRPM7, TRPC1, and TRPM4 channels that are known to exhibit mechanosensitivity. Furthermore, we detected mechanosensitive transcripts of the Kir6.2 and Kir6.1 channels, as well as transcripts of GK1 channels formed by the Kir2.1 and Kir2.2 proteins. Although the detection of the TREK-1/K2P2.1 transcript was limited, indirect data from other studies supports its presence [77]. The highest number of RNA reads among all CaV channels was detected for CaV1.2 channels, which themselves exhibit mechanosensitivity.
Cell stretching at various magnitudes discretely increased ISAC and decreased ICa,L probably through CaV1.2 channels in K+ in/K+ out, Cs+ in/K+ out, K+ in/Cs+ out, and Cs+ in/Cs+ out solutions. However, treatment with the nonspecific blocker of ISAC, Gd3+, on the background of cell stretching eliminated both ISAC and ICa,L at all stretching magnitudes and voltage steps relative to Vhp. The study suggests that voltage-gated CaV1.2 channels in adult rat ventricular myocytes have additional mechanosensitive properties, as evidenced by the maintained response to Gd3+ in the Cs+ in/Cs+ out solution.
Data Availability
The datasets generated during and/or analyzed during the current study are available in the following repository [https://disk.yandex.ru/d/40Xg_q8soUg7AA].
References
Kaufmann R, Theophile U. Autonomously promoted extension effect in Purkinje fibers, papillary muscles and trabeculae carneae of rhesus monkeys. Pflugers Arch Gesamte Physiol Menschen Tiere. 1967;297:174–89.
Nazir SA, Lab MJ. Mechanoelectric feedback and atrial arrhythmias. Cardiovasc Res. 1996;32:52–61.
Dobrev D, Ravens U. Remodeling of cardiomyocyte ion channels in human atrial fibrillation. Basic Res Cardiol. 2003;98:137–48. https://doi.org/10.1007/s00395-003-0409-8.
Craelius W, Chen V, el-Sherif N. Stretch activated ion channels in ventricular myocytes. Biosci Rep. 1988;8:407–14. https://doi.org/10.1007/BF01121637.
Kamkin A, Kiseleva I, Isenberg G. Stretch-activated currents in ventricular myocytes: amplitude and arrhythmogenic effects increase with hypertrophy. Cardiovascular Res. 2000;48:409–20. https://doi.org/10.1016/S0008-6363(00)00208-X.
Kamkin A, Kiseleva I, Isenberg G. Ion selectivity of stretch-activated cation currents in mouse ventricular myocytes. Pflugers Arch - Eur J Physiol. 2003;446:220–31. https://doi.org/10.1007/s00424-003-1018-y.
Zeng T, Bett GCL, Sachs F. Stretch-activated whole cell currents in adult rat cardiac myocytes. Am J Physiol Heart Circ Physiol. 2000;278:548–57. https://doi.org/10.1152/ajpheart.2000.278.2.H548.
Kamkin A, Kiseleva I, Wagner K-D, Bohm J, Theres H, Günther J, et al. Characterization of stretch-activated ion currents in isolated atrial myocytes from human hearts. Pflugers Arch - Eur J Physiol. 2003;446:339–46. https://doi.org/10.1007/s00424-002-0948-0.
Bustamante JO, Ruknudin A, Sachs F. Stretch-activated channels in heart cells: relevance to cardiac hypertrophy. J Cardiovasc Pharmacol. 1991;17(Suppl 2):110–3. https://doi.org/10.1097/00005344-199117002-00024.
Kim D. Novel cation-selective mechanosensitive ion channel in the atrial cell membrane. Circ Res. 1993;72:225–31. https://doi.org/10.1161/01.res.72.1.225.
Ruknudin A, Sachs F, Bustamante JO. Stretch-activated ion channels in tissue-cultured chick heart. Am J Physiol. 1993;264. https://doi.org/10.1152/ajpheart.1993.264.3.H960. :H960-972.
Sigurdson W, Ruknudin A, Sachs F. Calcium imaging of mechanically induced fluxes in tissue-cultured chick heart: role of stretch-activated ion channels. Am J Physiol. 1992;262:H1110–1115. https://doi.org/10.1152/ajpheart.1992.262.4.H1110.
None FGEW, Jy G. LG. A possible mechanism for large stretch-induced increase in [Ca2+]i in isolated guinea-pig ventricular myocytes. Cardiovascular research [Internet]. 1996 [cited 2023 Sep 29];32. https://pubmed.ncbi.nlm.nih.gov/8776413/.
Youm JB, Han J, Kim N, Zhang Y-H, Kim E, Leem CH, et al. Role of Stretch-activated channels in the heart: action potential and Ca2+ transients. In: Kamkin A, Kiseleva I, editors. Mechanosensitivity in cells and tissues. Moscow: Academia; 2005. http://www.ncbi.nlm.nih.gov/books/NBK7490/.
Youm JB, Han J, Kim N, Zhang Y-H, Kim E, Joo H, et al. Role of stretch-activated channels on the stretch-induced changes of rat atrial myocytes. Prog Biophys Mol Biol. 2006;90:186–206. https://doi.org/10.1016/j.pbiomolbio.2005.06.003.
Belus A, White E. Streptomycin and intracellular calcium modulate the response of single guinea-pig ventricular myocytes to axial stretch. J Physiol. 2003;546:501–9. https://doi.org/10.1113/jphysiol.2002.027573.
Hongo K, White E, Le Guennec JY, Orchard CH. Changes in [Ca2+]i, [Na+]i and Ca2+ current in isolated rat ventricular myocytes following an increase in cell length. J Physiol. 1996;491(Pt 3):609–19.
Sasaki N, Mitsuiye T, Noma A. Effects of mechanical stretch on membrane currents of single ventricular myocytes of guinea-pig heart. Jpn J Physiol. 1992;42:957–70. https://doi.org/10.2170/jjphysiol.42.957.
White E, Boyett MR, Orchard CH. The effects of mechanical loading and changes of length on single guinea-pig ventricular myocytes. J Physiol. 1995;482:93–107. https://doi.org/10.1113/jphysiol.1995.sp020502.
Calaghan SC, Belus A, White E. Do stretch-induced changes in intracellular calcium modify the electrical activity of cardiac muscle? Progress in Biophysics and Molecular Biology. 2003;82:81–95. https://doi.org/10.1016/s0079-6107(03)00007-5.
Isenberg G, Klöckner U. Calcium currents of isolated bovine ventricular myocytes are fast and of large amplitude. Pflugers Arch. 1982;395:30–41. https://doi.org/10.1007/BF00584965.
Dyachenko V, Husse B, Rueckschloss U, Isenberg G. Mechanical deformation of ventricular myocytes modulates both TRPC6 and Kir2.3 channels. Cell Calcium. 2009;45:38–54. https://doi.org/10.1016/j.ceca.2008.06.003.
Babraham Bioinformatics -. FastQC A Quality Control tool for High Throughput Sequence Data. https://www.bioinformatics.babraham.ac.uk/projects/fastqc/.
Bolger AM, Lohse M, Usadel B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics. 2014;30:2114–20. https://doi.org/10.1093/bioinformatics/btu170.
Chen S, Zhou Y, Chen Y, Gu J. Fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics. 2018;34:i884–90. https://doi.org/10.1093/bioinformatics/bty560.
Kim D, Langmead B, Salzberg SL. HISAT: a fast spliced aligner with low memory requirements. Nat Methods. 2015;12:357–60. https://doi.org/10.1038/nmeth.3317.
Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence Alignment/Map format and SAMtools. Bioinformatics. 2009;25:2078–9. https://doi.org/10.1093/bioinformatics/btp352.
Anders S, Pyl PT, Huber W. HTSeq—a Python framework to work with high-throughput sequencing data. Bioinformatics. 2015;31:166–9. https://doi.org/10.1093/bioinformatics/btu638.
Verheijck EE, van Ginneken AC, Wilders R, Bouman LN. Contribution of L-type Ca2+ current to electrical activity in sinoatrial nodal myocytes of rabbits. Am J Physiol. 1999;276:1064–77. https://doi.org/10.1152/ajpheart.1999.276.3.H1064.
Galli GLJ, Taylor EW, Shiels HA. Calcium flux in turtle ventricular myocytes. Am J Physiol Regul Integr Comp Physiol. 2006;291:1781–9. https://doi.org/10.1152/ajpregu.00421.2006.
Sagawa H, Hoshino S, Yoshioka K, Ding W-G, Omatsu-Kanbe M, Nakagawa M, et al. Postnatal developmental changes in the sensitivity of L-type Ca2 + channel to inhibition by verapamil in a mouse heart model. Pediatr Res. 2018;83:1207–17. https://doi.org/10.1038/pr.2018.46.
Dyachenko V, Rueckschloss U, Isenberg G. Modulation of cardiac mechanosensitive ion channels involves superoxide, nitric oxide and peroxynitrite. Cell Calcium. 2009;45:55–64. https://doi.org/10.1016/j.ceca.2008.06.002.
Boycott HE, Barbier CSM, Eichel CA, Costa KD, Martins RP, Louault F, et al. Shear stress triggers insertion of voltage-gated potassium channels from intracellular compartments in atrial myocytes. Proc Natl Acad Sci U S A. 2013;110:3955–64. https://doi.org/10.1073/pnas.1309896110.
Kamkin A, Kiseleva I, Wagner K-D, Scholz H. Mechano-Electric Feedback in the heart: evidence from intracellular microelectrode recordings on multicellular preparations and single cells from healthy and diseased tissue. In: Kamkin A, Kiseleva I, editors. Mechanosensitivity in cells and tissues. Moscow: Academia; 2005. http://www.ncbi.nlm.nih.gov/books/NBK7502/.
Lozinsky I, Kamkin A. Mechanosensitive alterations of action potentials and membrane currents in healthy and diseased cardiomyocytes: Cardiac tissue and isolated cell. In: Kamkin A, Kiseleva I, editors. Mechanosensitivity of the heart. Dordrecht: Springer Netherlands; 2010. pp. 185–238. https://doi.org/10.1007/978-90-481-2850-1_8.
Andriulė I, Pangonytė D, Gwanyanya A, Karčiauskas D, Mubagwa K, Mačianskienė R. Detection of TRPM6 and TRPM7 proteins in normal and diseased Cardiac Atrial tissue and isolated cardiomyocytes. Int J Mol Sci. 2022;23:14860. https://doi.org/10.3390/ijms232314860.
Numata T, Shimizu T, Okada Y. TRPM7 is a stretch- and swelling-activated cation channel involved in volume regulation in human epithelial cells. Am J Physiol Cell Physiol. 2007;292:C460–467. https://doi.org/10.1152/ajpcell.00367.2006.
Bessac BF, Fleig A. TRPM7 channel is sensitive to osmotic gradients in human kidney cells. J Physiol. 2007;582:1073–86. https://doi.org/10.1113/jphysiol.2007.130534.
Oancea E, Wolfe JT, Clapham DE. Functional TRPM7 channels accumulate at the plasma membrane in response to fluid flow. Circ Res. 2006;98:245–53. https://doi.org/10.1161/01.RES.0000200179.29375.cc.
Riccio A, Medhurst AD, Mattei C, Kelsell RE, Calver AR, Randall AD, et al. mRNA distribution analysis of human TRPC family in CNS and peripheral tissues. Brain Res Mol Brain Res. 2002;109:95–104. https://doi.org/10.1016/s0169-328x(02)00527-2.
Huang H, Liang L, Liu P, Wei H, Sachs F, Niu W, et al. Mechanical effects on KATP Channel Gating in Rat Ventricular myocytes. PLoS ONE. 2013;8:e63337. https://doi.org/10.1371/journal.pone.0063337.
Maroto R, Raso A, Wood TG, Kurosky A, Martinac B, Hamill OP. TRPC1 forms the stretch-activated cation channel in vertebrate cells. Nat Cell Biol. 2005;7:179–85. https://doi.org/10.1038/ncb1218.
Barritt G, Rychkov G. TRPs as mechanosensitive channels. Nat Cell Biol. 2005;7:105–7. https://doi.org/10.1038/ncb0205-105.
Liu H, El Zein L, Kruse M, Guinamard R, Beckmann A, Bozio A, et al. Gain-of-function mutations in TRPM4 cause autosomal dominant isolated cardiac conduction Disease. Circ Cardiovasc Genet. 2010;3:374–85. https://doi.org/10.1161/CIRCGENETICS.109.930867.
Guinamard R, Demion M, Magaud C, Potreau D, Bois P. Functional expression of the TRPM4 cationic current in ventricular cardiomyocytes from spontaneously hypertensive rats. Hypertension. 2006;48:587–94. https://doi.org/10.1161/01.HYP.0000237864.65019.a5.
Morita H, Honda A, Inoue R, Ito Y, Abe K, Nelson MT, et al. Membrane stretch-induced activation of a TRPM4-like nonselective cation channel in cerebral artery myocytes. J Pharmacol Sci. 2007;103:417–26. https://doi.org/10.1254/jphs.fp0061332.
Brayden JE, Earley S, Nelson MT, Reading S. Transient receptor potential (TRP) channels, vascular tone and autoregulation of cerebral blood flow. Clin Exp Pharmacol Physiol. 2008;35:1116–20. https://doi.org/10.1111/j.1440-1681.2007.04855.x.
Koch SE, Gao X, Haar L, Jiang M, Lasko VM, Robbins N, et al. Probenecid: novel use as a non-injurious positive inotrope acting via cardiac TRPV2 stimulation. J Mol Cell Cardiol. 2012;53:134–44. https://doi.org/10.1016/j.yjmcc.2012.04.011.
Muraki K, Iwata Y, Katanosaka Y, Ito T, Ohya S, Shigekawa M, et al. TRPV2 is a component of osmotically sensitive cation channels in murine aortic myocytes. Circ Res. 2003;93:829–38. https://doi.org/10.1161/01.RES.0000097263.10220.0C.
Fauconnier J, Lanner JT, Sultan A, Zhang S-J, Katz A, Bruton JD, et al. Insulin potentiates TRPC3-mediated cation currents in normal but not in insulin-resistant mouse cardiomyocytes. Cardiovasc Res. 2007;73:376–85. https://doi.org/10.1016/j.cardiores.2006.10.018.
Goel M, Zuo C-D, Sinkins WG, Schilling WP. TRPC3 channels colocalize with Na+/Ca2+ exchanger and Na+ pump in axial component of transverse-axial tubular system of rat ventricle. Am J Physiol Heart Circ Physiol. 2007;292:874–83. https://doi.org/10.1152/ajpheart.00785.2006.
Kojima A, Kitagawa H, Omatsu-Kanbe M, Matsuura H, Nosaka S. Ca2+ paradox injury mediated through TRPC channels in mouse ventricular myocytes. Br J Pharmacol. 2010;161:1734–50. https://doi.org/10.1111/j.1476-5381.2010.00986.x.
Yamaguchi Y, Iribe G, Nishida M, Naruse K. Role of TRPC3 and TRPC6 channels in the myocardial response to stretch: linking physiology and pathophysiology. Prog Biophys Mol Biol. 2017;130:264–72. https://doi.org/10.1016/j.pbiomolbio.2017.06.010.
Han L, Li J. Canonical transient receptor potential 3 channels in atrial fibrillation. Eur J Pharmacol. 2018;837:1–7. https://doi.org/10.1016/j.ejphar.2018.08.030.
Quick K, Zhao J, Eijkelkamp N, Linley JE, Rugiero F, Cox JJ, et al. TRPC3 and TRPC6 are essential for normal mechanotransduction in subsets of sensory neurons and cochlear hair cells. Open Biol. 2012;2:120068. https://doi.org/10.1098/rsob.120068.
Zhao Y, Huang H, Jiang Y, Wei H, Liu P, Wang W, et al. Unusual localization and translocation of TRPV4 protein in cultured ventricular myocytes of the neonatal rat. Eur J Histochem. 2012;56:e32. https://doi.org/10.4081/ejh.2012.e32.
Loukin S, Zhou X, Su Z, Saimi Y, Kung C. Wild-type and brachyolmia-causing mutant TRPV4 channels respond directly to stretch force. J Biol Chem. 2010;285:27176–81. https://doi.org/10.1074/jbc.M110.143370.
Suzuki M, Mizuno A, Kodaira K, Imai M. Impaired pressure sensation in mice lacking TRPV4. J Biol Chem. 2003;278:22664–8. https://doi.org/10.1074/jbc.M302561200.
Suzuki M, Sato J, Kutsuwada K, Ooki G, Imai M. Cloning of a stretch-inhibitable nonselective cation channel. J Biol Chem. 1999;274:6330–5. https://doi.org/10.1074/jbc.274.10.6330.
Birder LA, Nakamura Y, Kiss S, Nealen ML, Barrick S, Kanai AJ, et al. Altered urinary bladder function in mice lacking the vanilloid receptor TRPV1. Nat Neurosci. 2002;5:856–60. https://doi.org/10.1038/nn902.
Grimm C, Kraft R, Sauerbruch S, Schultz G, Harteneck C. Molecular and functional characterization of the melastatin-related cation channel TRPM3. J Biol Chem. 2003;278:21493–501. https://doi.org/10.1074/jbc.M300945200.
Gomis A, Soriano S, Belmonte C, Viana F. Hypoosmotic- and pressure-induced membrane stretch activate TRPC5 channels. J Physiol. 2008;586:5633–49. https://doi.org/10.1113/jphysiol.2008.161257.
Sénatore S, Rami Reddy V, Sémériva M, Perrin L, Lalevée N. Response to mechanical stress is mediated by the TRPA channel painless in the Drosophila heart. PLoS Genet. 2010;6:e1001088. https://doi.org/10.1371/journal.pgen.1001088.
Corey DP, García-Añoveros J, Holt JR, Kwan KY, Lin S-Y, Vollrath MA, et al. TRPA1 is a candidate for the mechanosensitive transduction channel of vertebrate hair cells. Nature. 2004;432:723–30. https://doi.org/10.1038/nature03066.
Kindt KS, Viswanath V, Macpherson L, Quast K, Hu H, Patapoutian A, et al. Caenorhabditis elegans TRPA-1 functions in mechanosensation. Nat Neurosci. 2007;10:568–77. https://doi.org/10.1038/nn1886.
Spassova MA, Hewavitharana T, Xu W, Soboloff J, Gill DL. A common mechanism underlies stretch activation and receptor activation of TRPC6 channels. Proc Natl Acad Sci U S A. 2006;103:16586–91. https://doi.org/10.1073/pnas.0606894103.
Takahashi K, Kakimoto Y, Toda K, Naruse K. Mechanobiology in cardiac physiology and Diseases. J Cell Mol Med. 2013;17:225–32. https://doi.org/10.1111/jcmm.12027.
Sharif-Naeini R, Folgering JHA, Bichet D, Duprat F, Lauritzen I, Arhatte M, et al. Polycystin-1 and – 2 dosage regulates pressure sensing. Cell. 2009;139:587–96. https://doi.org/10.1016/j.cell.2009.08.045.
Foster DB, Gu J-M, Kim EH, Wolfson DW, O’Meally R, Cole RN, et al. Tbx18 orchestrates Cytostructural Transdifferentiation of Cardiomyocytes to Pacemaker cells by recruiting the epithelial-mesenchymal transition program. J Proteome Res. 2022;21:2277–92. https://doi.org/10.1021/acs.jproteome.2c00133.
Watanabe H, Murakami M, Ohba T, Ono K, Ito H. The pathological role of transient receptor potential channels in Heart Disease. Circ J. 2009;73:419–27. https://doi.org/10.1253/circj.cj-08-1153.
Gottlieb PA, Bae C, Sachs F. Gating the mechanical channel Piezo1: a comparison between whole-cell and patch recording. Channels (Austin). 2012;6:282–9. https://doi.org/10.4161/chan.21064.
Wong T-Y, Juang WC, Tsai CT, Tseng CJ, Lee WH, Chang SN, et al. Mechanical stretching simulates Cardiac Physiology and Pathology through Mechanosensor Piezo1. J Clin Med. 2018;7:410. https://doi.org/10.3390/jcm7110410.
Copp SW, Kim JS, Ruiz-Velasco V, Kaufman MP. The mechano-gated channel inhibitor GsMTx4 reduces the exercise pressor reflex in decerebrate rats. J Physiol. 2016;594:641–55. https://doi.org/10.1113/JP271714.
Zeng W-Z, Marshall KL, Min S, Daou I, Chapleau MW, Abboud FM, et al. PIEZOs mediate neuronal sensing of blood pressure and the Baroreceptor Reflex. Science. 2018;362:464–7. https://doi.org/10.1126/science.aau6324.
Tan JHC, Liu W, Saint DA. Differential expression of the mechanosensitive potassium channel TREK-1 in epicardial and endocardial myocytes in rat ventricle. Exp Physiol. 2004;89:237–42. https://doi.org/10.1113/expphysiol.2003.027052.
Schmidt C, Wiedmann F, Kallenberger SM, Ratte A, Schulte JS, Scholz B, et al. Stretch-activated two-pore-domain (K2P) potassium channels in the heart: focus on atrial fibrillation and Heart Failure. Prog Biophys Mol Biol. 2017;130:233–43. https://doi.org/10.1016/j.pbiomolbio.2017.05.004.
Maingret F, Patel AJ, Lesage F, Lazdunski M, Honoré E. Mechano- or acid stimulation, two interactive modes of activation of the TREK-1 potassium channel. J Biol Chem. 1999;274:26691–6. https://doi.org/10.1074/jbc.274.38.26691.
Takahashi K, Naruse K. Stretch-activated BK channel and heart function. Prog Biophys Mol Biol. 2012;110:239–44. https://doi.org/10.1016/j.pbiomolbio.2012.08.001.
Sokabe M, Naruse K, Qiong-Yao T. A new mechanosensitive channel SAKCA and a new MS channel blocker GsTMx-4. Nihon Yakurigaku Zasshi. 2004;124:301–10. https://doi.org/10.1254/fpj.124.301.
Van Wagoner DR. Mechanosensitive gating of atrial ATP-sensitive potassium channels. Circ Res. 1993;72:973–83. https://.
Beyder A, Rae JL, Bernard C, Strege PR, Sachs F, Farrugia G. Mechanosensitivity of Nav1.5, a voltage-sensitive sodium channel. J Physiol. 2010;588:4969–85. https://doi.org/10.1113/jphysiol.2010.199034.
Morris CE, Juranka PF. Nav Channel Mechanosensitivity: activation and inactivation accelerate reversibly with Stretch. Biophys J. 2007;93:822–33. https://doi.org/10.1529/biophysj.106.101246.
Wang JA, Lin W, Morris T, Banderali U, Juranka PF, Morris CE. Membrane trauma and Na+ leak from Nav1.6 channels. Am J Physiol Cell Physiol. 2009;297:C823–834. https://doi.org/10.1152/ajpcell.00505.2008.
Lyford GL, Strege PR, Shepard A, Ou Y, Ermilov L, Miller SM, et al. Alpha (1 C) (ca(V)1.2) L-type calcium channel mediates mechanosensitive calcium regulation. Am J Physiol Cell Physiol. 2002;283:C1001–1008. https://doi.org/10.1152/ajpcell.00140.2002.
Vincent PF, Bouleau Y, Petit C, Dulon D. A synaptic F-actin network controls otoferlin-dependent exocytosis in auditory inner hair cells. Elife. 2015;4:e10988. https://doi.org/10.7554/eLife.10988.
Calabrese B, Tabarean IV, Juranka P, Morris CE. Mechanosensitivity of N-type calcium channel currents. Biophys J. 2002;83:2560–74. https://doi.org/10.1016/S0006-3495(02)75267-3.
Laitko U, Morris CE. Membrane tension accelerates rate-limiting voltage-dependent activation and slow inactivation steps in a Shaker channel. J Gen Physiol. 2004;123:135–54. https://doi.org/10.1085/jgp.200308965.
Hammami S, Willumsen NJ, Olsen HL, Morera FJ, Latorre R, Klaerke DA. Cell volume and membrane stretch independently control K + channel activity. J Physiol. 2009;587:2225–31. https://doi.org/10.1113/jphysiol.2008.163550.
Grunnet M, Jespersen T, MacAulay N, Jørgensen NK, Schmitt N, Pongs O, et al. KCNQ1 channels sense small changes in cell volume. J Physiol. 2003;549:419–27. https://doi.org/10.1113/jphysiol.2003.038455.
Otway R, Vandenberg JI, Guo G, Varghese A, Castro ML, Liu J, et al. Stretch-sensitive KCNQ1 mutation A link between genetic and environmental factors in the pathogenesis of atrial fibrillation? J Am Coll Cardiol. 2007;49:578–86. https://doi.org/10.1016/j.jacc.2006.09.044.
Fatehi M, Carter CC, Youssef N, Light PE. The mechano-sensitivity of cardiac ATP-sensitive potassium channels is mediated by intrinsic MgATPase activity. J Mol Cell Cardiol. 2017;108:34–41. https://doi.org/10.1016/j.yjmcc.2017.05.004.
Al-Shammari H, Latif N, Sarathchandra P, McCormack A, Rog-Zielinska EA, Raja S, et al. Expression and function of mechanosensitive ion channels in human valve interstitial cells. PLoS ONE. 2020;15:e0240532. https://doi.org/10.1371/journal.pone.0240532.
Maingret F, Patel AJ, Lesage F, Lazdunski M, Honoré E. Lysophospholipids open the two-pore domain mechano-gated K(+) channels TREK-1 and TRAAK. J Biol Chem. 2000;275:10128–33. https://doi.org/10.1074/jbc.275.14.10128.
Numata T, Shimizu T, Okada Y. Direct mechano-stress sensitivity of TRPM7 channel. Cell Physiol Biochem. 2007;19:1–8. https://doi.org/10.1159/000099187.
Earley S, Waldron BJ, Brayden JE. Critical role for transient receptor potential channel TRPM4 in myogenic constriction of cerebral arteries. Circ Res. 2004;95:922–9. https://doi.org/10.1161/01.RES.0000147311.54833.03.
Yamaguchi Y, Iribe G, Kaneko T, Takahashi K, Numaga-Tomita T, Nishida M, et al. TRPC3 participates in angiotensin II type 1 receptor-dependent stress-induced slow increase in intracellular Ca2+ concentration in mouse cardiomyocytes. J Physiol Sci. 2018;68:153–64. https://doi.org/10.1007/s12576-016-0519-3.
Christensen AP, Corey DP. TRP channels in mechanosensation: direct or indirect activation? Nat Rev Neurosci. 2007;8:510–21. https://doi.org/10.1038/nrn2149.
Bae C, Sachs F, Gottlieb PA. The mechanosensitive ion channel Piezo1 is inhibited by the peptide GsMTx4. Biochemistry. 2011;50:6295–300. https://doi.org/10.1021/bi200770q.
Bae C, Gottlieb PA, Sachs F. Human PIEZO1: removing inactivation. Biophys J. 2013;105:880–6. https://doi.org/10.1016/j.bpj.2013.07.019.
Josephson I, Sperelakis N. On the ionic mechanism underlying adrenergic-cholinergic antagonism in ventricular muscle. J Gen Physiol. 1982;79:69–86. https://doi.org/10.1085/jgp.79.1.69.
Kamkin A, Kiseleva I, Theres H, Eulert-Grehn J-J, Wagner KD, Scholz H, et al. Enhanced L-type calcium currents in cardiomyocytes from transgenic rats overexpressing SERCA2a. Exp Clin Cardiol. 2010;15:e109–15.
Monteilh-Zoller MK, Hermosura MC, Nadler MJS, Scharenberg AM, Penner R, Fleig A. TRPM7 provides an ion channel mechanism for cellular entry of trace metal ions. J Gen Physiol. 2003;121:49–60. https://doi.org/10.1085/jgp.20028740.
Nadler MJ, Hermosura MC, Inabe K, Perraud AL, Zhu Q, Stokes AJ, et al. LTRPC7 is a Mg.ATP-regulated divalent cation channel required for cell viability. Nature. 2001;411:590–5. https://doi.org/10.1038/35079092.
Zitt C, Zobel A, Obukhov AG, Harteneck C, Kalkbrenner F, Lückhoff A, et al. Cloning and functional expression of a human Ca2+-permeable cation channel activated by calcium store depletion. Neuron. 1996;16:1189–96. https://doi.org/10.1016/s0896-6273(00)80145-2.
Dienes C, Hézső T, Kiss DZ, Baranyai D, Kovács ZM, Szabó L, et al. Electrophysiological effects of the Transient Receptor Potential Melastatin 4 Channel Inhibitor (4-Chloro-2-(2-chlorophenoxy)acetamido) Benzoic Acid (CBA) in Canine Left Ventricular cardiomyocytes. Int J Mol Sci. 2021;22:9499. https://doi.org/10.3390/ijms22179499.
Hof T, Simard C, Rouet R, Sallé L, Guinamard R. Implication of the TRPM4 nonselective cation channel in mammalian sinus rhythm. Heart Rhythm. 2013;10:1683–9. https://doi.org/10.1016/j.hrthm.2013.08.014.
Zaritsky JJ, Redell JB, Tempel BL, Schwarz TL. The consequences of disrupting cardiac inwardly rectifying K+ current (IK1) as revealed by the targeted deletion of the murine Kir2.1 and Kir2.2 genes. J Physiol. 2001;533:697–710. https://doi.org/10.1111/j.1469-7793.2001.t01-1-00697.x.
Clark RB, Tremblay A, Melnyk P, Allen BG, Giles WR, Fiset C. T-tubule localization of the inward-rectifier K+ channel in mouse ventricular myocytes: a role in K+ accumulation. J Physiol. 2001;537:979–92. https://doi.org/10.1111/j.1469-7793.2001.00979.x.
Scherer D, Seyler C, Xynogalos P, Scholz EP, Thomas D, Backs J, et al. Inhibition of Cardiac Kir Current (IK1) by protein kinase C critically depends on PKCβ and Kir2.2. PLoS ONE. 2016;11:e0156181. https://doi.org/10.1371/journal.pone.0156181.
Isenberg G, Kondratev D, Dyachenko V, Kazanski V, Gallitelli MF. Isolated cardiomyocytes: Mechanosensitivity of Action potential, membrane current and Ion Concentration. In: Kamkin A, Kiseleva I, editors. Mechanosensitivity in cells and tissues. Moscow: Academia; 2005. http://www.ncbi.nlm.nih.gov/books/NBK7515/.
Tabarean IV, Juranka P, Morris CE. Membrane stretch affects gating modes of a skeletal muscle sodium channel. Biophys J. 1999;77:758–74. https://doi.org/10.1016/S0006-3495(99)76930-4.
Laitko U, Juranka PF, Morris CE. Membrane stretch slows the concerted step prior to opening in a kv channel. J Gen Physiol. 2006;127:687–701. https://doi.org/10.1085/jgp.200509394.
Lab MJ. Mechanosensitive-mediated interaction, integration, and cardiac control. Ann N Y Acad Sci. 2006;1080:282–300. https://doi.org/10.1196/annals.1380.022.
Janmey PA. The cytoskeleton and cell signaling: component localization and mechanical coupling. Physiol Rev. 1998;78:763–81. https://doi.org/10.1152/physrev.1998.78.3.763.
Dabiri BE, Lee H, Parker KK. A potential role for integrin signaling in mechanoelectrical feedback. Prog Biophys Mol Biol. 2012;110:196–203. https://doi.org/10.1016/j.pbiomolbio.2012.07.002.
Kamkin AG, Kamkina OV, Shim AL, Bilichenko A, Mitrokhin VM, Kazansky VE, et al. The role of activation of two different sGC binding sites by NO-dependent and NO-independent mechanisms in the regulation of SACs in rat ventricular cardiomyocytes. Physiol Rep. 2022;10:e15246. https://doi.org/10.14814/phy2.15246.
Petroff MG, Kim SH, Pepe S, Dessy C, Marbán E, Balligand JL, et al. Endogenous nitric oxide mechanisms mediate the stretch dependence of Ca2+ release in cardiomyocytes. Nat Cell Biol. 2001;3:867–73. https://doi.org/10.1038/ncb1001-867.
Ehara T, Noma A, Ono K. Calcium-activated non-selective cation channel in ventricular cells isolated from adult guinea-pig hearts. J Physiol. 1988;403:117–33.
Gannier F, White E, Le Garnier null JY. A possible mechanism for large stretch-induced increase in [Ca2+]i in isolated guinea-pig ventricular myocytes. Cardiovasc Res. 1996;32:158–67.
Isenberg G, Kazanski V, Kondratev D, Gallitelli MF, Kiseleva I, Kamkin A. Differential effects of stretch and compression on membrane currents and [Na+]c in ventricular myocytes. Prog Biophys Mol Biol. 2003;82:43–56. https://doi.org/10.1016/s0079-6107(03)00004-x.
Wendt-Gallitelli MF, Voigt T, Isenberg G. Microheterogeneity of subsarcolemmal sodium gradients. Electron probe microanalysis in guinea-pig ventricular myocytes. J Physiol. 1993;472:33–44. https://doi.org/10.1113/jphysiol.1993.sp019934.
Yang XC, Sachs F. Block of stretch-activated ion channels in Xenopus oocytes by gadolinium and calcium ions. Science. 1989;243:1068–71. https://doi.org/10.1126/science.2466333.
Tang QY, Qi Z, Naruse K, Sokabe M. Characterization of a functionally expressed stretch-activated BKCa channel cloned from chick ventricular myocytes. J Membr Biol. 2003;196:185–200. https://doi.org/10.1007/s00232-003-0637-8.
Hongo K, Pascarel C, Cazorla O, Gannier F, Le Guennec JY, White E. Gadolinium blocks the delayed rectifier potassium current in isolated guinea-pig ventricular myocytes. Exp Physiol. 1997;82:647–56. https://doi.org/10.1113/expphysiol.1997.sp004053.
Lacampagne A, Gannier F, Argibay J, Garnier D, Le Guennec JY. The stretch-activated ion channel blocker gadolinium also blocks L-type calcium channels in isolated ventricular myocytes of the guinea-pig. Biochim Biophys Acta. 1994;1191:205–8. https://doi.org/10.1016/0005-2736(94)90250-x.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work: A.G.K., O.V.K., and V.E.K. Substantial contributions to the acquisition, analysis, or interpretation of data for the work: A.G.K., V.E.K., O.V.K., V.M.M., A.B., A.S.R., A.D.Z., V.I.Z., E.A.N., S.A.S., P.V.S. and M.I.M. Drafting the work or revising it critically for important intellectual content: A.G.K. Final approval of the version to be published: A.G.K., O.V.K., V.E.K., V.M.M., A.B., A.S.R., A.D.Z., V.I.Z., E.A.N., S.A.S., P.V.S., and M.I.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All experiments in this study were approved by the Ethics Committee of the Russian National Research Medical University according to the guidelines issued by the Guide for Care and Use of Laboratory Animals (8th edition, 2011) published by the US National Institutes of Health and ARRIVE guidelines.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kamkin, A.G., Kamkina, O.V., Kazansky, V.E. et al. Identification of RNA reads encoding different channels in isolated rat ventricular myocytes and the effect of cell stretching on L-type Ca2+current. Biol Direct 18, 70 (2023). https://doi.org/10.1186/s13062-023-00427-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13062-023-00427-0