Abstract
Background
Previous research indicated outcomes among refractory out-of-hospital cardiac arrest (OHCA) patients with initial shockable rhythm were different in Singapore and Osaka, Japan, possibly due to the differences in access to extracorporeal cardiopulmonary resuscitation. However, this previous study had a risk of selection bias. To address this concern, this study aimed to evaluate the outcomes between Singapore and Osaka for OHCA patients with initial shockable rhythm using only population-based databases.
Methods
This was a secondary analysis of two OHCA population-based databases in Osaka and Singapore, including adult OHCA patients with initial shockable rhythm. A machine-learning-based prediction model was derived from the Osaka data (n = 3088) and applied to the PAROS-SG data (n = 2905). We calculated the observed-expected ratio (OE ratio) for good neurological outcomes observed in Singapore and the expected derived from the data in Osaka by dividing subgroups with or without prehospital ROSC.
Results
The one-month good neurological outcomes in Osaka and Singapore among patients with prehospital ROSC were 70% (791/1,125) and 57% (440/773), and among patients without prehospital ROSC were 10% (196/1963) and 2.8% (60/2,132). After adjusting patient characteristics, the outcome in Singapore was slightly better than expected from Osaka in patients with ROSC (OE ratio, 1.067 [95%CI 1.012 to 1.125]), conversely, it was worse than expected in patients without prehospital ROSC (OE ratio, 0.238 [95%CI 0.173 to 0.294]).
Conclusion
This study showed the outcomes of OHCA patients without prehospital ROSC in Singapore were worse than expected derived from Osaka data even using population-based databases.
(249/250 words).
Similar content being viewed by others
Introduction
Extracorporeal cardiopulmonary resuscitation (ECPR), which utilizes extracorporeal membrane oxygenation (ECMO) during cardiopulmonary resuscitation, is an advanced procedure designed for OHCA patients who are unresponsive to standard resuscitation, especially those presenting with initial shockable rhythms like ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) [1,2,3,4]. Our previous research indicated the frequency of ECPR differs greatly between Osaka, Japan, and Singapore for refractory OHCA patients with initial shockable rhythm, and, among such patients, observed neurologically favorable outcomes and survival in Singapore was less than expected compared to Osaka [2]. However, this previous study had a substantial risk of selection bias, as the reference population in Osaka included only patients who were selected and transferred to tertiary care hospitals. To address concerns about selection bias and to confirm the robustness of previous results, we investigated the reproducibility and validity using population-based data. We also estimated the additional number of patients, using population-based data, who might obtain favorable outcomes if the resuscitation strategy in Osaka was implemented in Singapore. This study aimed to evaluate the validity of the previous results indicating outcome differences among OHCA patients with initial shockable rhythm in Singapore and Osaka using population-based data.
Methods
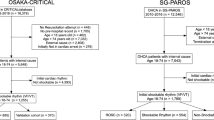
This was a secondary analysis of two population-based OHCA databases in Singapore and Osaka, Japan, which were the All-Japan Utstein Registry and the Singapore Pan-Asian Resuscitation Outcomes Study (SG-PAROS) [5, 6]. Detailed information about these databases can be found in the Additional file 1 (S-Method 1). We extracted data on the Osaka Prefecture from this nationwide registry, with the aim of addressing the limitations of our previous study as mentioned in the background section. Similar to the previous study, [2] we included adult OHCA patients aged 18–74 with initial shockable rhythms, and excluded those without prehospital records, those who didn't receive resuscitation, had external causes or weren't in arrest when paramedics arrived. A machine-learning-based prediction model derived and validated as mentioned below using data from the Osaka data (derivation data 2010–2018, validation data 2019), was applied to the PAROS-SG data (2010–2019). The primary outcome of this study was one-month survival with favorable neurological outcomes defined as Cerebral Performance Category (CPC) 1 or 2. The secondary outcome of this study was one-month survival [7].
In the statistical analysis, patient characteristics, pre-hospital information, in-hospital procedures, and outcomes were described as continuous variables with median and interquartile range (IQR), while categorical variables were reported as numbers and percentages. In the main analysis, similar to the previous study, [2] we developed and validated machine-learning predictive models (random forest) of outcomes using the Osaka derivation data. The prediction models incorporated the following covariates: sex, age, witnessed events, bystander CPR, bystander automated external defibrillator, prehospital advanced airway management, prehospital adrenaline administration, and time from call to the hospital. We assessed the model's performance using the Osaka validation data. Then, we applied the prediction model to the SG-PAROS data in order to calculate the expected probability of outcomes. Subsequently, we computed the observed-expected ratio (OE ratio) and the observed-expected difference (OE difference) between the observed outcomes and the expected probability derived from the Osaka data with 95% confidence intervals (CI). Moreover, we estimated the incremental number of patients with the outcome by multiplying the OE difference by the number of cases. We calculated these values separately for patients with and without prehospital ROSC, to evaluate the potential impact of resuscitation strategies such as ECPR after hospital arrival but before ROSC. All statistical analyses were performed using R software, version 4.1.2 (R Foundation for Statistical Computing). The other details of the methods are described in the Additional file 1 (S-Method 2–4).
Results
Patient characteristics
For the Osaka Utstein Registry database, 3414 OHCA patients with an initial shockable rhythm were included in the analysis [the derivation cohort (n = 3,088) and the validation cohort (n = 326)]. Of the SG-PAROS database, 2905 patients with initial shockable rhythm were included in the analysis. The study flowchart is described in the Additional file 1 (S-Results 1). The median [IQR] age was 62 [51, 68] in the derivation cohort in Osaka, and 58 [50, 65] in the SG-PAROS. Good neurological outcomes were 32% (987/3,088) in Osaka and 17% (500/2,905) in Singapore. The prehospital ROSC were 36% (1,125/3,088) in Osaka and 27% (773/2,905) in Singapore, and among them, one-month good neurological outcomes were 70% (791/1,125) in Osaka and 57% (440/773), respectively. In comparison, among the patients without prehospital ROSC, good neurological outcomes were 10.0% (196/1,963) and 2.8% (60/2,132), respectively. The other details of characteristics, in-hospital information, and outcomes are described in Table 1 and the Additional file 1: (S-Results 2–5). ECMO was rarely performed in both populations of Singapore (with prehospital ROSC, 0.9% and without 0.5%). The prediction model derived from the Osaka derivation data performed well in the validation data. The details of the prediction model are described in the Additional file 1 (S-Results 6–7).
The observed expected ratio, difference, and incremental number of patients
The one-month good neurological outcome in patients with prehospital ROSC in Singapore was the same or slightly better than expected compared to Osaka (OE ratio, 1.067 [95%CI 1.012 to 1.125] and OE difference, 0.036 [95%CI 0.006 to 0.066]). Conversely, the neurological outcome in patients without prehospital ROSC in Singapore was worse than expected compared to Osaka (OE ratio, 0.238 [95%CI 0.173 to 0.294] and OE difference, − 0.09 [95%CI − 0.096 to -0.083]), (Fig. 1). Similarly, for one-month survival, the result was consistent as follows: with prehospital ROSC, OE ratio, 0.97 [95%CI 0.925 to 1.012] and OE difference, − 0.021 [95%CI − 0.051 to 0.008], and without prehospital ROSC, OE ratio 0.297 [95%CI 0.242 to 0.345] and OE difference, -0.128 [95%CI -0.138 to -0.119], (Fig. 1).
OE difference and the incremental number of patients with or without Prehospital ROSC. (Left) The Observed-Expected ratio and 95% confidence interval (CI). (Right) The Observed-Expected difference and 95% confidence interval (CI). Good Neuro One-month good neurological outcome, Survival One-month survival, ROSC, Return of spontaneous circulation
The incremental one-month good neurological outcome in patients with prehospital ROSC was better than expected (27.8 [95% CI 4.9 to 50.7]), but was fewer than expected (− 191.9 [95% CI −205.6 to − 177.6]) in patients without prehospital ROSC) between 2010 and 2019. The incremental number of one-month survival cases had a similar trend to neurological outcomes (patients with pre-hospital ROSC: − 16.3 [95%CI − 39.1 to 5.9], patients without prehospital ROSC: − 272.7 [95%CI − 293.2 to − 253.8]). The incremental one-month good neurological outcome in each year is described in the Additional file 1 (S-Results 8).
Discussion
This population-based observational study showed that the outcomes of OHCA patients without prehospital ROSC in Singapore were worse than expected derived from Osaka data even using population-based databases. These results were consistent with our previous research, mitigating previous selection bias concerns.
Similar to the previous study, we speculated that the outcome difference among patients without ROSC between Singapore and Osaka was related to the different availability of ECPR. First, outcomes were similar among patients with ROSC after adjusting the patients’ characteristics, which suggests the quality of post-resuscitation care after ROSC was comparable between Singapore and Osaka. In contrast, for patients without prehospital ROSC, ECMO was rarely performed (0.5%, 11/2,132) and hospital admission was considerably low (20%, 435/2,132) in Singapore while the percentage of ECPR cases was 30–60% and hospital admission was reported around 60–80% in the tertiary care hospitals in Osaka. [2] Considering the reports from RCTs that the hospital admission of the patients treated with ECPR were remarkably higher than the conventional group [e.g., INCEPTION trial, ECPR group 81% (57/70) vs 36% (23/64)], we suggested that the difference of hospital admission may be mainly caused by the difference of frequency of ECPR. [8, 9] In addition, the OE differences in neurological outcomes among patients without ROSC was approximately 9–10%, which is comparable to the effect magnitude of the ECPR strategy observed in a previous study in Japan (SAVE-J study) [12.3% (32/260) and 1.5% (3/194), with a risk difference of 10.8%], or the RCT in Prague, which also reported a risk difference of approximately 9.5%. [10, 11] Therefore, considering that the OE difference in our study closely aligns with the effect estimates from previous studies investigating aggressive ECPR strategies, we think it is reasonable to attribute the difference to ECPR strategies.
Several limitations should be acknowledged in this study, similar to the previous study. It didn't directly examine the link between ECPR policies and outcomes but instead highlighted potential differences in in-hospital care before ROSC between Osaka and Singapore. Outcomes might also be influenced by unmeasured factors like past medical history, frailty, and quality of resuscitation. A lack of detailed data limited our comparison of resuscitation specifics. Moreover, there are risks associated with the prediction model, such as overfitting and regularization bias. [12, 13].
Conclusion
This study using two population-based databases indicated that the outcomes of OHCA patients without prehospital ROSC in Singapore were worse than expected compared to Osaka. The results are consistent with our previous research. We speculate that the outcome difference among patients without ROSC between Singapore and Osaka was due to different availability of ECPR.
(1455/1500 words).
Availability of data and materials
This study's datasets and/or analyses are not publicly available because the ethics committee did not permit it.
References
Inoue A, Hifumi T, Sakamoto T, Kuroda Y. Extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest in adult patients. J Am Heart Assoc. 2020;9(7):e015291.
Okada Y, Shahidah N, Ng YY, Chia MYC, Gan HN, Leong BSH, et al. Outcome assessment for out-of-hospital cardiac arrest patients in Singapore and Japan with initial shockable rhythm. Crit Care. 2023;27(1):351.
Okada Y, Kiguchi T, Irisawa T, Yamada T, Yoshiya K, Park C, et al. Development and validation of a clinical score to predict neurological outcomes in patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation. JAMA Netw Open. 2020;3(11):e2022920.
Okada Y, Komukai S, Kitamura T, Kiguchi T, Irisawa T, Yamada T, et al. Clinical phenoty** of out-of-hospital cardiac arrest patients with shockable rhythm–machine learning-based unsupervised cluster analysis. Circ J. 2022;86(4):668–76.
Okada Y, Irisawa T, Yamada T, Yoshiya K, Park C, Nishimura T, et al. Clinical outcomes among out-of-hospital cardiac arrest patients treated by extracorporeal cardiopulmonary resuscitation: The CRITICAL study in Osaka. Resuscitation. 2022; Ireland: Elsevier.
Doctor NE, Ahmad NS, Pek PP, Yap S, Ong ME. The Pan–Asian resuscitation outcomes study (PAROS) clinical research network: what, where, why and how. Singapore Med J. 2017;58(7):456–8.
Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein style. A statement for health professionals from a task force of the American heart association, the European resuscitation council, the heart and stroke foundation of Canada, and the Australian resuscitation council. Circulation. 1991;84(2):960–75.
Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, et al. Early Extracorporeal CPR for refractory out-of-hospital cardiac arrest. New Eng J Med 2023; 388(4): 299–309.
Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. The Lancet. 2020;396(10265):1807–16.
Sakamoto T, Morimura N, Nagao K, Asai Y, Yokota H, Nara S, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2014;85(6):762–8.
Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2022;327(8):737–47.
Kühl N, Schemmer M, Goutier M, Satzger G. Artificial intelligence and machine learning. Electron Mark. 2022;32(4):2235–44.
James G, Witten D, Hastie T, Tibshirani R, Service S. An Introduction to Statistical Learning: with Applications in R. New York: Springer; 2013.
Acknowledgements
The authors are deeply grateful to all EMS personnel for collecting the Utstein data. The authors would also like to thank Ms. Maeve Pek and the late Ms. Susan Yap from the Department of Emergency Medicine, Singapore General Hospital; Ms Noor Azuin and Ms. Nurul Asyikin from Unit for Prehospital Emergency Care, Singapore General Hospital; Ms Woo Kai Lee from National University Heart Centre Singapore for their contributions and support to the Singapore PAROS registry, and all other Singapore PAROS investigators (Ling Tiah, Changi General Hospital, Singapore; Si Oon Cheah, Urgent Care Clinic International, Singapore; Shun Yee Low, Sengkang General Hospital, Singapore; Wei Ling Tay, Ng Teng Fong General Hospital, Singapore; Shir Lynn Lim, National University Heart Centre Singapore, Singapore) that contributed to the study. The authors thank the JSPS Overseas Research Fellowships, the FUKUDA Foundation for Medical Technology, and the International Medical Research Foundation for their support.
Funding
This study was supported by a scientific research grant from the JSPS KAKENHI of Japan (JP22K21143 to YO), the ZOLL Foundation (YO), National Medical Research Council, Clinician Scientist Award, Singapore (NMRC/CSA/024/2010, NMRC/CSA/0049/2013 and NMRC/CSASI/014/2017) to MEHO, and Ministry of Health, Health Services Research Grant, Singapore (HSRG/0021/2012) to MEHO. These organizations have no role in conducting this research.
Author information
Authors and Affiliations
Contributions
Conceptualization, YO, MO. Data curation, NS, YYN, MYCC, HNG, BSHL, DRM, NED, WMN, TK, TI, MEHO. Methodology, YO, MO. Analysis, YO, MO. Writing–original draft, YO, MO. Writing–review & editing, NS, YYN, BSHL, TK, NN, TK, TI. Project administration, NS, TK. Funding Acquisition, YO, MEHO. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethical approval and consent participate
This study was conducted according to the Declaration of Helsinki. This study was approved by the Centralized Institutional Review Board and Domain Specific Review Board in Singapore granted approval for the SG-PAROS database (ref no: 2013/604/C, 2013/00929 and 2018/2937) and Domain Specific Review Board (ref no: C/10/545 and 2013/00929) and the ethics committee of Kyoto University (R-1538). Informed consent was waived due to the nature of the observational study. Informed consent was waived due to the nature of the observational study.
Consent for publication
Not applicable.
Competing interests
YO has received a research grant from the ZOLL Foundation and an overseas scholarship from the FUKUDA Foundation for Medical Technology and the International Medical Research Foundation. MEHO reports grants from the Laerdal Foundation, Laerdal Medical, and Ramsey Social Justice Foundation for funding of the Pan-Asian Resuscitation Outcomes Study an advisory relationship with Global Healthcare SG, a commercial entity that manufactures cooling devices; and funding from Laerdal Medical on an observation program to their Community CPR Training Centre Research Program in Norway. MEHO is a Scientific Advisor to TIIM Healthcare SG and Global Healthcare SG. These organizations have no role in conducting this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Okada, Y., Shahidah, N., Ng, Y.Y. et al. Comparing outcomes of out-of-hospital cardiac arrest patients with initial shockable rhythm in Singapore and Osaka using population-based databases. Crit Care 27, 479 (2023). https://doi.org/10.1186/s13054-023-04771-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04771-5