Abstract
Background
Phelan-McDermid syndrome (PHMDS) is a rare genetic disorder mostly caused by haploinsufficincy of SHANK3 gene, and characterized by neonatal hypotonia, developmental delay, minor dysmorphic features, seizures and behavior problems. Literature of this syndrome is scanty and confusing, and represents a challenge for pediatricians, in terms of finding the correct diagnoses.
Case presentation
In a postnatal case with hypotonia and dysmorphic features a de novo ring chromosome r(22) leading to in parallel microdeletion and micro duplication in 22q13 was diagnosed by banding cytogenetics, and further characterized in detail by molecular cytogenetic and chromosomal microarray.
Conclusion
Here a rare PHMDS case caused by a r(22) is presented. Less than 10 comparable cases are reported in the literature. The present case highlights the importance of conducting genetic counseling and appropriate genetic tests for newborns with mild dysmorphic features.
Similar content being viewed by others
Background
Ring chromosome 22/r(22) syndrome [ORPHA: 1446] is a rare chromosomal aberration with a prevalence of 1/1,000,000 and usually a de novo event; however, there are some familial cases reported. Especially familial r(22) cases may be without phenotypic effects, as in those no crucial genetic material was lost or gained. Clinical manifestations in deleterious r(22) cases may include developmental and speech delay, global intellectual disability, growth retardation, microcephaly, hypotonia and mild to prominent facial dysmorphic features, such as large ears and bulbous nose [1,2,3,4]. Psychological and behavioral problems including aggressive behavior, as well as hyperactivity, bipolar affective disorder, self-injurious behavior, and autistic spectrum disorders are relatively common among patients with this chromosomal abnormality [5,6,7,8]. Seizures of different types including febrile, generalized tonic–clonic, focal, absence seizures and peculiar features can be present in about 25% of the cases with 22q13 deletion [9, 10].
Skin disorders and pigmentation abnormalities were observed in a few number of cases with constitutional mosaicism of r[22] chromosome, such as hypomelanosis, hypochromic maculae and patchy depigmentation in different part of the body [11, 12].
Speech delay is one of the common features among individuals with 22q13 deletion, this region could be a candidate genomic segment to carry genes involved in speech development and autistic spectrum in childhood [13].
Besides copy number variants (CNVs) due to ring chromosome formation, a common mechanism how ring chromosomes may lead to clinical problems is, that they tend to lead to be lost or duplicated as a whole in part of the patient’s cells. Thus, mosaics like mos 46,XX/46,XX,r(22)/45,XX, − 21/47,XX,r(22),+r(22) can be observed. According to the mosaic status in different tissues, various phenotypic deviations may be observed in basically similar r(22) cases [14]. According to [15] r(22) has been seen to be associated with PHMDS in at least 5 cases, yet. Here we report another such case, which was not suspected to be PHMDS, before a r(22) was observed in banding cytogenetics.
Case presentation
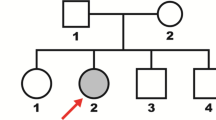
A full-term female infant was born by lower segment caesarian section after breech presentation. Clinical examination indicated mild neonatal hypotonia, feeding difficulties, mild facial dysmorphism expressed as small rounded face and microcephaly (head circumference at birth was 33 cm), synophrys, and a birth weight of 3.0 kg. After one month, she was admitted to the general pediatric ward with short history of cough, fever, cyanosis and change of voice particularly during crying. Otherwise, she was active, with normal heart rate and blood pressure, and no seizure or abnormal movements. Her weight was 2.66 kg, with head circumference of 34 cm being below 3rd percentile. Respiratory examination showed mild stridor, otherwise, auscultation of the chest revealed equal bilateral breath sounds with scattered rhonchi. Respiratory panel indicated human rhinovirus. Her cardiovascular and central nervous systems were unremarkable, abdomen was soft with no distension, palpable masses or organomegaly. She was treated symptomatically as a case of bronchiolitis and at the same time metabolic and chromosomal analysis were requested to investigate the causes of her failure to thrive. Karyotype revealed heterozygous ring chromosome 22 with a karyotype of 46,XX,r(22) (Fig. 1). The patient was discharged home in a stable condition after she started to gain weight in the hospital, and a clinical dietician was involved in treatment protocol. Two weeks later, she was readmitted to the pediatric ward with history of cough, fever and shortness of breath. At examination she showed mild respiratory distress as intercostal and subcostal retraction, and X-ray evidenced of bronchopneumia. Fiber optic study confirmed diagnosis of laryngomalacia.
Subsequent single nucleotide polymorphism (SNP)-array analysis (HumanCytoSNP-12v2.1, Illumina) identified two adjacent CNVs in chromosome 22:
-
an interstitial duplication of the long arm of chromosome 22 (arr[GRCh37] 22q13.2q13.31(43682699_46704243) × 3) of approximately three megabases (Mb). This region is not polymorphic (DGV, gnomAD) and includes 24 OMIM genes (3 of them are classified as disease causing: ATXN10, FBLN1 and PPARA; see Table 1). Duplications 22q13.2q13.31 were not described in the Achropuce, Decipher, Clingen and Pubmed databases. Thus, this copy number variant (CNV) is of uncertain significance.
-
The adjacent distal heterozygous deletion of the long arm of chromosome 22 (arr[GRCh37] 22q13.31q13.33(46722256_51169045) × 1) was approximately 4.4 Mb in size. This region is not polymorphic (DGV, gnomAD) and includes 37 OMIM genes (12 of them are classified as disease causing including: TRMU, CELSR1, ALG12, MLC1, MOV10L1, TUBGCP6, SCO2, TYMP, CHKB, SBF1, ARSA, and SHANK3; see Table 2) [16,17,18]. Deletion of SHANK3 and the terminal region of the long arm of chromosome 22 are responsible for autosomal dominant inherited PHMDS [OMIM #606,232, ORPHA: 48652] [19,20,21]. This deletion is pathogenic due to haploinsufficiency of the included autosomal dominant genes or damasking recessive mutations on the second allele and contributes to the patient’s phenotype.
To confirm the SNP-array results, fluorescence in situ hybridization (FISH) studies were carried out. Centromeric probe D14/22Z1 (Zytovison, Bremerhaven, Germany), a probe for all acrocentric short arms (midi54) [22], and as locus specific probes the subtelomeric probe D22S163 (Abbott/Vysis, Wiesbaden, Germany in 22q13.33), RP3-388M5 (in 22q13.-2 ~ 13.31; chr22:44,142,192–44,319,759) and RP3-398C22 (in 22q13.31; chr22:46,075,907–46,165,234) were used to further characterize the r(22). A whole chromosome paint (wcp) for chromosome 22 was applied as control probe [23]. It could be shown that almost the whole short arm of chromosome 22 was lost on the ring chromosome and one breakpoint of r(22) is in 22p11.1, covered by probe D14/22Z1. Besides by application of the three locus specific probes it could be confirmed that the subtelomeric region was deleted in the r(22) and it was revealed that the region being duplicated according to SNP-array results is inverted duplicated (see Fig. 1). Therefore, the karyotype of the case according to ISCN 2020 nomenclature [24] is 46,XX,r(22)(::p11.1- > q13.31::q13.31- > q13.2::).ish r(22)(wcp22 + ,midi54-,D14/22Z1dim,RP3-388M5 + + ,RP3-398C22 + + ,D22S163-).arr[GRCh37] 22q13.2q13.31(43682699_46704243) × 3),22q13.31q13.33(46722256_51169045) × 1).
Currently, the patient is one year and eight months old, active, cheerful, playful, growing well, and still rely on commercial infant milk formula. She was born with two small hemangiomas; one of them was on the front head which gradually faded, and the other on the sacral area which is regressing in size with age; so far hemangiomas are no specific features of PHMDS and are common among newborns. Her weight is 10.9 kg on the 50th percentile, length is 80 cm on the 50th percentile, and head circumference is 44 cm on 5th percentile. She is achieving her developmental milestones as she can stand and started walking.
Discussion and conclusion
PHMDS is characterized by wide range of phenotypic and clinical features due to the highly diverse deletion sizes and different genes involved. The case presented here has a r(22) which was present in each studied cell of the patient. There was no evidence for a mosaic karyotype as reported for other r(22) cases in the literature [12, 25]. In the 22q13.31q13.33 deletion identified in the proband there are 12 genes involved, one of the important genes in this region related to the early speech development is SHANK3 located at 22q13.3, its expression plays a pivotal role in the development of the cerebral cortex and the cerebellum, and therefore, it is a strong candidate gene for neurobehavioral disorders [26], dysmorphic features, autism spectrum disorders, bipolar disorders, hyperactivity, gastrointestinal symptoms, retinopathy, and cardia malformations [27]. Although [28] reported that clinical features of patients without SHANK3 deletion were similar to that of patients having the SHANK3 deletion which may suggest that other genes within this region may play a role in the phenotypes of PHMDS.
Moreover, the ATXN10 and FBLN1 genes which are involved in the 22q13.2q13.31 duplication, and CELSR1 gene encode proteins that are involved in neurodevelopmental features, and their copy number variation may contribute to the clinical phenotypes of PHMDS as well [28, 29], while the deletion of ARSA may cause remarkable loss of myelin in the central nervous system, resulting in different neurological problems [12]. In addition to the role of SHANK3, the deletion of the ALG12, MLC1, TUBGCP6, SCO2 and CHKB genes located in the 22q13.31q13.33 region may have contributed in the mild dysmorphic features in the proband, whereas the deletion of the TRMU, ARSA genes may be involved in the mild hypotonia (https://www.omim.org/). The PPARA gene which is known to play a role in lipid metabolism pathways, and contributes to the susceptibility to hyperapobetalipoproteinemia and some other chronic disease [30]. However, although this gene is duplicated in the proband but all lipids profile are within the normal ranges.
While it is still early to evaluate our case regarding possible psychological and behavioral and other chronic disorders, we may conclude that the clinical characteristics including dysmorphic features like small head, small rounded face and mild hypotonia are a consequence of her chromosomal imbalance. And the level of the mild dysmorphic features in the proband might be a result of phenotypic overlay with the adjacent duplication including the ATXN10 duplication, which might be in turn neuroprotective and modifies the severity of PHMDS features.
In this case report we describe the molecular cytogenetic and clinical characteristics of a one year and eight months female diagnosed with PHMDS involving deletion of SHANK3 gene, and 22q13 duplication syndrome with mild hypotonia and dysmorphic features. This case sheds lights on the importance of offering genetic counseling and genetic testing for newborns with mild dysmorphic features, which could be due to genetic factors. It is highly recommended to follow up the children in order to diagnose any possible behavioral or psychological disorders, which may appear in the future, since the patient harbors a duplication of 22q13, which may increase the risk of developmental delay as well as for learning and intellectual difficulties. Taking into account that early diagnosis of such disorders might be helpful in patient’s management and treatment.
Availability of data and materials
Please contact the corresponding author for data requests.
References
Stoll C, Roth MP. Segregation of a 22 ring chromosome in three generations. Hum Genet. 1983;63(3):294–6.
Teyssier M, Moreau N. Familial transmission of deleted chromosome 22 [r(22)p0?] in two normal women. Ann Genet. 1985;28(2):116–8.
Crusi A, Engel E. Prenatal diagnosis of 3 cases of ring G chromosomes: one 21 and two 22, one of which was de novo. Ann Genet. 1986;29(4):253–60.
Wenger SL, Boone LY, Cummins JH, Del Vecchio MA, Bay CA, Hummel M, et al. Newborn infant with inherited ring and de novo interstitial deletion on homologous chromosome 22s. Am J Med Genet. 2000;91(5):351–4.
Sovner R, Stone A, Fox C. Ring chromosome 22 and mood disorders. J Intellect Disabil Res. 1996;40(Pt 1):82–6.
MacLean JE, Teshima IE, Szatmari P, Nowaczyk MJ. Ring chromosome 22 and autism: report and review. Am J Med Genet. 2000;90(5):382–5.
Sarasua SM, Dwivedi A, Boccuto L, Rollins JD, Chen CF, Rogers RC, et al. Association between deletion size and important phenotypes expands the genomic region of interest in Phelan-McDermid syndrome (22q13 deletion syndrome). J Med Genet. 2011;48(11):761–6.
Sarasua SM, Dwivedi A, Boccuto L, Chen CF, Sharp JL, Rollins JD, et al. 22q13.2q13.32 genomic regions associated with severity of speech delay, developmental delay, and physical features in Phelan-McDermid syndrome. Genet Med. 2014;16(4):318–28.
Phelan K, McDermid HE. The 22q13.3 Deletion Syndrome (Phelan-McDermid Syndrome). Mol Syndromol. 2012;2(3–5):186–201.
Figura MG, Coppola A, Bottitta M, Calabrese G, Grillo L, Luciano D, et al. Seizures and EEG pattern in the 22q13.3 deletion syndrome: clinical report of six Italian cases. Seizure. 2014;23(9):774–9.
Ritter CL, Steele MW, Wenger SL, Cohen BA. Chromosome mosaicism in hypomelanosis of Ito. Am J Med Genet. 1990;35(1):14–7.
Guilherme RS, Soares KC, Simioni M, Vieira TP, Gil-da-Silva-Lopes VL, Kim CA, et al. Clinical, cytogenetic, and molecular characterization of six patients with ring chromosomes 22, including one with concomitant 22q11.2 deletion. Am J Med Genet A. 2014;164A(7):1659–65.
Goizet C, Excoffier E, Taine L, Taupiac E, El Moneim AA, Arveiler B, et al. Case with autistic syndrome and chromosome 22q13.3 deletion detected by FISH. Am J Med Genet. 2000;96(6):839–44.
Guilherme RS, Meloni VF, Kim CA, Pellegrino R, Takeno SS, Spinner NB, et al. Mechanisms of ring chromosome formation, ring instability and clinical consequences. BMC Med Genet. 2011;12:171.
Crocco M, Panciroli M, Milanaccio C, Morerio C, Verrico A, Garre ML, et al. Case report: the emerging role of ring chromosome 22 in Phelan-McDermid syndrome with atypical teratoid/rhabdoid tumor: the first child treated with growth hormone. Front Neurol. 2021;12: 741062.
Phelan MC, Rogers RC, Saul RA, Stapleton GA, Sweet K, McDermid H, et al. 22q13 deletion syndrome. Am J Med Genet. 2001;101(2):91–9.
Soorya L, Kolevzon A, Zweifach J, Lim T, Dobry Y, Schwartz L, et al. Prospective investigation of autism and genotype-phenotype correlations in 22q13 deletion syndrome and SHANK3 deficiency. Mol Autism. 2013;4(1):18.
Yi F, Danko T, Botelho SC, Patzke C, Pak C, Wernig M, et al. Autism-associated SHANK3 haploinsufficiency causes Ih channelopathy in human neurons. Science. 2016;352(6286):aaf2669.
Phelan K, Rogers RC, Boccuto L. Phelan-McDermid Syndrome. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, et al., editors. GeneReviews(R). Seattle (WA); 1993.
Phelan MC. Deletion 22q13.3 syndrome. Orphanet J Rare Dis. 2008;3:14.
Harony-Nicolas H, De Rubeis S, Kolevzon A, Buxbaum JD. Phelan McDermid syndrome: from genetic discoveries to animal models and treatment. J Child Neurol. 2015;30(14):1861–70.
Mrasek K, Heller A, Rubtsov N, Trifonov V, Starke H, Rocchi M, et al. Reconstruction of the female Gorilla gorilla karyotype using 25-color FISH and multicolor banding (MCB). Cytogenet Cell Genet. 2001;93(3–4):242–8.
Liehr T, Claussen U. Current developments in human molecular cytogenetic techniques. Curr Mol Med. 2002;2(3):283–97.
International Standing Committee on Human Cytogenomic Nomenclature, McGowan-Jordan J, Hastings RJ, Moore S. ISCN 2020: an international system for human cytogenomic nomenclature (2020). Basel; Hartford: Karger (2020)
Kosho T, Matsushima K, Sahashi T, Mitsui N, Fukushima Y, Sobajima H, et al. “Ring syndrome” involving chromosome 2 confirmed by FISH analysis using chromosome-specific subtelomeric probes. Genet Couns. 2005;16(1):65–70.
Delahaye A, Toutain A, Aboura A, Dupont C, Tabet AC, Benzacken B, et al. Chromosome 22q13.3 deletion syndrome with a de novo interstitial 22q13.3 cryptic deletion disrupting SHANK3. Eur J Med Genet. 2009;52(5):328–32.
Ricciardello A, Tomaiuolo P, Persico AM. Genotype-phenotype correlation in Phelan-McDermid syndrome: a comprehensive review of chromosome 22q13 deleted genes. Am J Med Genet A. 2021;185(7):2211–33.
Li S, ** KW, Liu T, Zhang Y, Zhang M, Zeng LD, et al. Fraternal twins with Phelan-McDermid syndrome not involving the SHANK3 gene: case report and literature review. BMC Med Genomics. 2020;13(1):146.
Jeffries AR, Curran S, Elmslie F, Sharma A, Wenger S, Hummel M, et al. Molecular and phenotypic characterization of ring chromosome 22. Am J Med Genet A. 2005;137(2):139–47.
Duval C, Fruchart JC, Staels B. PPAR alpha, fibrates, lipid metabolism and inflammation. Arch Mal Coeur Vaiss. 2004;97(6):665–72.
Acknowledgements
We thank the family for its participation in this study.
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no funding for this study.
Author information
Authors and Affiliations
Contributions
YK and HA carried out the clinical evaluation and collected the clinical data from the family. HYH conducted the genetic counseling. HYH, AW, TL performed the genetic testing and interpretation of the results. HYH drafted the manuscript. All authors read and revised the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study has been approved by the research ethical committee of the Bahrain Defence Force Hospital, Royal Medical Services.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Khalifa, Y., Hassan, H.Y., Weise, A. et al. Molecular cytogenetic and phenotypic characterization of Phelan McDermid and 22q13 duplication syndrome: a case report. Mol Cytogenet 15, 52 (2022). https://doi.org/10.1186/s13039-022-00629-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-022-00629-7