Abstract
Background
We report the first ante-mortem diagnosis of hemorrhagic pericardial effusion in hereditary hemorrhagic telangiectasia resulting in constriction; the case also demonstrates the unusual but well-described complication of right-sided heart failure requiring extracorporeal membrane oxygenation (ECMO) support after pericardiectomy.
Case presentation
A previously healthy 48 year old man with a strong family history of Osler–Weber–Rendu disease presented to our institution with signs and symptoms of advance heart failure. His workup demonstrated a thickened pericardium and constrictive physiology. He was brought to the operating room where old clot and inflamed tissue were appreciated in the pericardial space and he underwent complete pericardiectomy under cardiopulmonary bypass. Separation from bypass, hampered by the development of right ventricular dysfunction and profound vasoplegia, required significant pressor and inotropic support. The right heart dysfunction and vasoplegia worsened in the early postoperative period requiring a week of ECMO after which his right ventricle recovered and he was successfully de-cannulated.
Conclusion
Given the poor outcome of severe postoperative right ventricular failure after pericardiectomy, with high central venous pressure, a low gradient between central venous and pulmonary artery pressures and high vasopressor requirements, ECMO should be instituted promptly.
Similar content being viewed by others
Background
Originally labeled Osler–Weber–Rendu disease after the clinicians who first described the condition, hereditary hemorrhagic telangiectasia (HHT) is characterized by the primarily-dominant, autosomal transmission of dermal, mucosal and visceral telangiectasias and visceral arteriovenous malformations [1]. Spontaneous hemorrhage into the pericardium in the context of HHT is an unusual cause of pericardial constriction with only one reported case where the diagnosis was made post-mortem [2]. We report the first ante-mortem diagnosis of hemorrhagic pericardial effusion in HHT resulting in constriction; the case also demonstrates the unusual but well-described [3] complication of right-sided heart failure requiring extracorporeal membrane oxygenation (ECMO) support after pericardiectomy.
Case presentation
A previously healthy 48-year-old male presented to our Emergency Department with dyspnea. Over the previous six months he had gained 60 pounds. He was unable to ambulate more than twenty-feet without resting. Although he had no history of epistaxis, mucocutaneous telangiectasia or documented visceral arteriovenous malformations, his family history was notable for a mother, two brothers and a daughter with genetically-confirmed HHT.
He was afebrile and hemodynamically stable. He had a rapid, regular heart rate, diminished breath-sounds bilaterally, pitting edema to his chest wall, a normal creatinine (1.0 mg/dL) and elevated total bilirubin (2.2 mg/dL). Viral and antibody testing for COVID-19 were negative. His chest roentgenogram demonstrated an enlarged cardiac silhouette, pulmonary interstitial edema and moderate-sized pleural effusions. Computed tomography demonstrated thickened pericardium and bilateral pleural effusions (Fig. 1a). An echocardiogram demonstrated normal biventricular function, thickened pericardium, severely elevated right atrial pressure with a dilated and non-collapsible inferior vena cava, elevated medial e’ tissue velocity of 12.6 cm/s (Fig. 1b) and pronounced ventricular septal bounce (Fig. 1c, d). Simultaneous pressure-tracings of the left ventricle (LV) and right ventricle (RV) and of the LV and wedge-pressure were pathognomonic of constrictive physiology. His coronary anatomy was normal. He was optimized on the medical service before going to the operating room for radical pericardiectomy.
a Computed tomography demonstrating thickened pericardium (yellow arrow), pleural effusions and lung consolidation. Transthoracic apical four-chamber echocardiogram demonstrating elevated medial E’ velocity (b), septal movement towards LV on inspiration (yellow arrow) (c) and toward RV on expiration (red arrow) (d)
Through a median sternotomy hemorrhagic inflammation and tenacious adhesions were evident between the thickened pericardium and heart (Fig. 2a, b) requiring initiation of cardiopulmonary bypass using the femoral vessels. The pericardium was resected anteriorly and posteriorly from phrenic nerve to phrenic nerve. Separation from bypass, hampered by the development of RV dysfunction and profound vasoplegia, required significant pressor and inotropic support. Total bypass time was 144 min. He required plasma and platelets to obtain hemostasis. His central venous pressure dropped from 32 to 18 mmHg, the pulmonary artery systolic pressure was in the mid 20’s mmHg, his LV was vigorous and cardiac output remained 7–9 L/min.
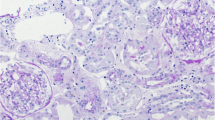
a, b Thickened pericardium in anterior–posterior (a) and lateral views (b). Black arrow identifies hemorrhage in pericardial space. White arrow points towards markedly thickened pericardium. c–f Hematoxylin and eosin stained histomicrographs of pericardium. c Scattered hemosiderin deposits are present within thickened and fibrotic pericardium consistent with prior hemorrhage (yellow arrows). d Diffuse, dense collagen deposition. e Extensive pericardial fibrosis resulting in markedly thickened and rough pericardial surface with adhesion formation. f Focus of normal-thickness pericardium shown for comparison
Over the next forty-eight hours, the vasoplegia worsened despite escalating pressor support. A transesophageal echocardiogram demonstrated akinesis of the RV (Fig. 3a). He developed renal failure requiring continuous renal replacement therapy. The next morning he was placed on femoral veno-arterial ECMO. Over the next week his pressor and inotropic support were weaned dramatically. He was decannulated after seven days support, extubated postoperative day 13 and transitioned to intermittent hemodialysis. His total bilirubin peaked at 32 mg/dL.
Over the next ten days his inotropic and pressor support were weaned off and his total bilirubin trended downwards. Repeat echocardiogram on day #23 showed mild to moderate RV hypokinesis. He was discharged to acute rehabilitation on day #25 and home ten days later. Pathologic examination (Fig. 2c–f) revealed a markedly thickened, fibrotic pericardium with chronic inflammation, fresh hemorrhage, old blood and significant adhesions.
Two months later his total bilirubin, renal function and weight had normalized. Four months after the original operation an echocardiogram showed mild RV dysfunction (Fig. 3b). One year later the patient felt well with no symptoms of heart failure but had persistent, unexplained lower extremity weakness. Of note, genetic testing subsequent to discharge confirmed the suspected diagnosis of HHT. The patient gave his permission for publication of this report.
Discussion and conclusions
The impact of HHT on the management of constriction in this patient was most profound regarding the resulting bleeding diathesis likely compounded by the heparinization required for a longer than anticipated cardiopulmonary bypass run. The high transfusion requirement in theory could contribute to pulmonary congestion and high right ventricular afterload leading to RV failure but in this case the pulmonary pressures were normal. Right ventricular failure is a well-described cause of early morbidity and mortality after pericardiectomy [4]. Right ventricular deconditioning occurs over time due to myocardial atrophy from chronic under-filling of the chamber. The RV is supported by the pericardium that acts as an inelastic truss preventing dilatation. When the stiffened pericardium is removed the impaired RV has no further mechanical support, and abrupt increases in venous return can lead to volume overload, chamber dilation and RV failure.
In our patient ECMO was instituted on the second postoperative day, it allowed for de-escalation of pressor support and recovery of significant RV function. In retrospect, however, institution of ECMO more promptly may have allowed for a less prolonged recovery. Given the poor outcome of severe postoperative RV failure after pericardiectomy, we agree with previous recommendations [3] that with high central venous pressure, a low gradient between central venous and pulmonary artery pressures and high vasopressor requirements, that ECMO be instituted as soon as possible.
Availability of data and materials
Not applicable.
Abbreviations
- HHT:
-
Hereditary hemorrhagic telangiectasia
- ECMO:
-
Extra-corporeal membrane oxygenation
- LV:
-
Left ventricle
- RV:
-
Right ventricle
References
Rendu M. Épistaxis répétées chez un sujet porteur de petits angiomes cutanés et muqueux. Bull Mem Soc Med Hop Paris. 1896;13:731–3.
Higuchi M, Ohnishi T, Arita N, Hayakawa T, Ikeda T, Mogami H. A case of Osler–Weber–Rendu disease with brain abscess; the mechanism of the formation of brain abscess and its treatment in Osler–Weber–Rendu disease. No Shinkei Geka. 1991;19(10):969–74.
Beckmann E, Ismail I, Cebotari S, et al. Right-sided heart failure and extracorporeal life support in patients undergoing pericardiectomy for constrictive pericarditis: a risk factor analysis for adverse outcome. Thorac Cardiovasc Surg. 2017;65:662–70.
Yu HT, Ha JW, Lee S, et al. Transient right ventricular dysfunction after pericardiectomy in patients with constrictive pericarditis. Korean Cir J. 2011;41(5):283–6.
Acknowledgements
Not applicable.
Funding
There was no funding for this project.
Author information
Authors and Affiliations
Contributions
JSC: engaged in the management of the patient, writing of manuscript and editing process. RB: engaged in the management of the patient, writing of manuscript and editing process. LJD: processed the histology, wrote that section of the manuscript and was involved in the editing process. HH: engaged in the management of the patient both in the operating room and in the postoperative period and with the writing of the manuscript. AB: engaged in the diagnostic workup and in selecting images for presentation in the manuscript as well as with editing the paper. NM: engaged in the diagnostic workup and in selecting images for presentation in the manuscript as well as with editing the paper. DGR: engaged in all aspects of the clinical management of the patient and the writing of the case report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our institutional IRB waived the need for approval because this was an anonymous case report and no experimental intervention or interaction was performed.
Consent for publication
We obtained consent from the patient for publication of the report and it is available upon request.
Competing interests
None of the authors on this paper have any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chung, J.S., Bylsma, R., Denham, L.J. et al. Hemorrhagic pericardial effusion resulting in constriction in hereditary hemorrhagic telangiectasia. J Cardiothorac Surg 17, 44 (2022). https://doi.org/10.1186/s13019-022-01782-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01782-1