Abstract
Background
American Academy of Orthopaedic Surgeons (AAOS) has provided the guidelines for diagnosing a patient with periprosthetic joint infection including the use of positron emission tomography/computed tomography (PET/CT). Systematic evidence focussing on periprosthetic joint infection (PJI) of hip is limited, which also contains limited number of studies. Hence, the current study aims to perform a pooled analysis of all studies that have assessed the diagnostic accuracy of PET/CT for PJI of hip.
Methods
Searches were done in PubMed Central, EMBASE, MEDLINE, SCOPUS and Cochrane library until December 2022. Meta-analysis was carried out using random-effects model. With 95% confidence intervals (CIs), pooled sensitivity and specificity were reported.
Results
Twenty-six studies met the inclusion criteria. The pooled sensitivity of PET/CT was 89% (95% CI 84–93%), while the pooled specificity was 86% (95% CI 79–91%). The AUROC was 0.94 (95% CI 0.72–0.99). There was statistically significant heterogeneity (p < 0.001) with I2 value of 96%. The diagnostic odds ratio was 52 (95% CI 26–106). Likelihood ratio positive was 6.5 (95% CI 4.1–10.3) and negative was 0.13 (95% CI 0.08–0.19).
Conclusion
Our study found that PET/CT was found to have higher level of accuracy in terms of sensitivity and specificity. Further large-scale research can help to find answers for such questions and provide final conclusive evidence on the inclusion of the imaging modality into the routine clinical practice guidelines for suspected periprosthetic joint infection patients.
Similar content being viewed by others
Introduction
A large number of patients worldwide have hip prosthetics. The prevalence of patients with any prosthesis is nearly 3% amongst middle aged and older adults and it seems to double by 80 years [1]. With an ageing population, the number of hip joint arthroplasty procedures has risen in recent decades. By 2060, the number of hip arthroplasty procedures is expected to rise by nearly 40% [2]. However, there is a limitation in that a significant portion of these prosthetics require revision, with the rate rising to nearly 15% after ten years [3]. The commonest cause of this revision is mainly aseptic or septic loosening, which contribute to about two-third of total revisions followed by dislocations and fractures [4]. This shows the importance of differentiating the aseptic and septic loosening, which is necessary to plan the treatment for the patients [5]. However, differentiating these conditions can be difficult with the existing clinical procedures.
The American Academy of Orthopaedic Surgeons (AAOS) has provided the guidelines for diagnosing a patient with periprosthetic joint infection, which recommends testing such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), as well as the use of positron emission tomography/computed tomography (PET/CT) in certain cases [6]. Amongst these procedures, role of PET-CT is particularly important, given its higher level of accuracy compared to rest of the parameters.7 PET-CT also has several advantages in terms of convenience to the patients, no requirement for the cell labelling (unlike white blood cell scintigraphy), and the entire diagnostic procedure takes not more than two hours [7].
Though several primary studies and fewer secondary meta-analyses are available on this topic [8,9,10], systematic evidence focussing on periprosthetic joint infection of hip is limited, which also contains limited number of studies. Specifically focussing on periprosthetic joint infection of hip will provide guidance and frame guidelines for specific procedure and site of infection. Hence, the current study aims to search for and perform a pooled analysis of all studies that have assessed the diagnostic accuracy of PET/CT for periprosthetic joint infection.
Objective
The objective of the present investigation is to conduct a comprehensive search and meta-analysis of all relevant studies that have evaluated the diagnostic precision of PET/CT in the context of periprosthetic joint infection.
Materials and methods
Inclusion criteria
Type of studies
We included research articles that looked at how well PET/CT works for detecting periprosthetic joint infection at hip, regardless of the design of the study, contrast material used. We included studies that were published as full text or grey literature (i.e. unpublished data) in the form of thesis, conference abstracts, etc. We did not include case reports, or case series or traditional review articles.
Index test
Studies utilizing PET/CT as the index test for diagnosing the periprosthetic joint infection of the hip joint.
Reference standards
We only included studies that compared the accuracy of PET/CT for detecting periprosthetic joint infection with an intraoperative or postoperative confirmation of infection using standard microbiological/histopathological/clinical procedures.
Outcome measure
We only included studies that reported the sensitivity and specificity of this diagnostic method, or that provided information that could be used to calculate these rates (like true positives, true negatives, false negatives and false positives).
Search strategy
A thorough and methodical search of multiple electronic databases such as PubMed Central, EMBASE, MEDLINE, SCOPUS and Cochrane library were conducted. The keywords and search terms were determined during the planning stage. Both medical subject headings and free-text words were utilized to search the databases, and truncations, wildcards, and proximity searching were employed with the keywords and their synonyms. The same terms were also used to search for published studies in the Cochrane library, Scopus, and Embase. The search also included key concepts and corresponding subject headings in each database. The final search was a combination of the individual search results using appropriate Boolean operators. The search was limited to studies published in English and from the inception of the databases up to December 2022. Detailed search strategy is available in Additional file 1.
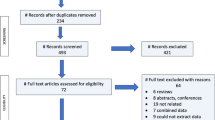
Study selection
Two authors were responsible for the initial screening process, which involved evaluating the titles and abstracts of the literature search. Citations, along with their titles and abstracts, were added to a designated endnote library and duplicates were removed to create a final list of studies to be reviewed. The full text of these studies was then retrieved and evaluated by the same two authors against the inclusion criteria of the study. Studies that did not meet the criteria were excluded and the reasons for exclusion were recorded. The screening and selection process was illustrated using a PRISMA flow chart [11].
Data extraction
Using a pre-designed data extraction form, information was gathered from the studies, including details such as the study design, setting, index test, reference standards, type of contrast agent used in PET/CT, sample size, average age, inclusion and exclusion criteria, test results and negatives. The data were then entered into STATA software and a third investigator reviewed the entered data to ensure accuracy against the original study reports.
Risk of bias assessment
Two independent authors have assessed the risk of bias in the studies by using the "Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool" [12]. The following areas were evaluated: patient selection, index tests, reference standards, and the flow and timing of assessments. The authors assigned a grade of high, low, or unclear for the potential source of bias in each of the included studies.
Statistical analysis
To get the pooled values of sensitivity, specificity, likelihood ratio positive, negative, and summary diagnostic odds ratio for PET/CT, a meta-analysis was carried out using STATA 14.2 ("StataCorp, College Station, TX, USA"). It was used to create "Summary Receiver Operator Characteristic curves (sROC)" and the outcome was reported as area under ROC (AUROC). A forest plot was used to graphically display study-specific and combined estimations. Chi square test for heterogeneity, and I2 statistics to measure the inconsistency was performed. Publication bias was evaluated, graphically displayed, and tested using Deek's test for asymmetry in the funnel plot. Meta-regression was performed with the factors such as contrast agent, study design, study region, sample size and risk of bias assessment.
Results
Study selection
The systematic literature search yielded 1578 records, and 121 of those studies were determined to be pertinent for full-text retrieval. Four publications were found by manually examining the bibliographies of the retrieved studies. Finally, 26 studies satisfied all the inclusion criteria during the second round of screening and were incorporated in the analysis (Fig. 1) [8,9,10, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35].
Characteristics of included studies
Table 1 shows the characteristics of the included studies. Majority (22 studies) were prospective studies. Most studies were done in USA (6 studies), Germany (4 studies), China (2 studies), The Netherlands (2 studies), Taiwan (2 studies) and India (2). Histopathological, microbiological and clinical findings were most commonly used as reference standard amongst the included studies. The sample size ranged from 10 to 134. Majority studies (21 studies) had lower risk of bias (Table 1).
Diagnostic accuracy of PET/CT for periprosthetic joint infection
The pooled sensitivity of PET/CT was 89% (95% CI 84–93%), while the pooled specificity was 86% (95% CI 79–91%) (Fig. 2). The AUROC was 0.94 (95% CI 0.72–0.99) (Fig. 3). There was statistically significant heterogeneity (p < 0.001) with I2 value of 96%. The diagnostic odds ratio was 52 (95% CI 26–106). Likelihood ratio positive was 6.5 (95% CI 4.1–10.3) and negative was 0.13 (95% CI 0.08–0.19). The likelihood ratio scattergram (Fig. 4) was generated to identify whether the imaging can be used for either confirmation or exclusion or both confirmation and exclusion. Both the likelihood ratios were placed in the right lower quadrant of the scattergram, indicating that the imaging cannot be used as a confirmatory test or to rule out the condition.
Fagan nomogram (Fig. 5) was generated to identify the clinical application of the imaging technique. The nomograms showed very good clinical application with significant increase in the post-test probabilities compared to the pre-test probabilities. Meta-regression results did not find any factors significantly associated with the sensitivity or specificity model, but the type of contrast material and mean age showed significant association in the joint model (p < 0.001) (Fig. 6). Publication bias assessment showed a symmetrical plot with deek’s test showing a p value of 0.33 (Fig. 7).
Subgroup analysis based on the type of PET revealed that use of fluoride/gallium (Fig. 8) had higher sensitivity (93%; 95% CI 84–98%) and specificity (94%; 95% CI 89–97%) with AUC of 0.97 (95% CI 0.89–0.99) when compared to FDG-PET (sensitivity = 87%, 95% CI 81–92%; specificity = 83%, 95% CI 73–89%; AUC = 0.92; 95% CI 0.69–0.98) (Fig. 9).
Discussion
PET/CT is a powerful imaging tool that can provide important information for the diagnosis and management of periprosthetic infections of the hip joint. PET/CT has several advantages over traditional imaging modalities such as X-ray and MRI in the evaluation of periprosthetic infections. Synthesizing the evidence showing its accuracy will help to inform the clinicians and decision makers to add the imaging technique to the guidelines and make it a standard protocol for these patients. Hence, this review was done to find the accuracy of PET/CT for diagnosing the periprosthetic infection of the hip.
In total, 26 of the identified studies were included in the review and analysis. Most studies were prospective and had lower risk of bias. PET/CT was found to have higher level of accuracy in terms of sensitivity (89%) and specificity (86%) with AUROC of 0.94. This finding was in line with the previous similar reviews on this topic [36,37,38]. However, the previous reviews have included studies irrespective of the site of infection and had limited number of studies when compared to the current review.
In addition to these general findings, our review further differentiated the accuracy based on the type of PET tracer used. The subgroup analysis revealed that the use of fluoride/gallium in PET/CT scanning yielded even higher accuracy than FDG-PET. Specifically, the sensitivity and specificity rates for fluoride/gallium were 93% (95% CI 84–98%) and 94% (95% CI 89–97%), respectively, with an AUC of 0.97 (95% CI 0.89–0.99). In comparison, FDG-PET demonstrated a slightly lower sensitivity of 87% (95% CI 81–92%) and specificity of 83% (95% CI 73–89%), with an AUC of 0.92 (95% CI 0.69–0.98). These results suggest that the choice of PET tracer can have significant implications for the diagnostic accuracy of PET/CT in the evaluation of periprosthetic infections of the hip joint. Particularly, the use of fluoride/gallium tracers seems to present a more effective option for diagnosing these infections, and it might be beneficial to update imaging protocols to preferentially use these tracers when available and appropriate.
The clinical application of PET/CT was also found to be appropriate, given the significant increase in the post-test probability in the nomogram compared to the pre-test probability. However, it did not satisfy the criteria to be used as either a confirmatory test or as a test to rule out the condition as per the LR scattergram. Nonetheless, the use of a radiotracer, such as 18F-fluorodeoxyglucose (18F-FDG), allows for the identification of increased metabolic activity, which is a characteristic of infected tissues [39]. This can be useful in detecting early or subtle signs of infection that may not be visible on other imaging modalities. Additionally, PET/CT provides functional and anatomic information in a single examination, which can be useful in the evaluation of complex cases where the distinction between infection and postoperative changes can be challenging [7]. By combining the functional information provided by the PET scan with the anatomic information provided by the CT scan, PET/CT scan aid in the localization and characterization of the infection.
Furthermore, PET/CT can be used to monitor the response to treatment, as it can detect resolution of the metabolic activity, which is an indication of the elimination of the infection. This can help in the management of periprosthetic infections of the hip joint by monitoring the treatment effectiveness. It is vital to highlight another recent clinical investigation which provides valuable context to our findings. This study conducted at the RWTH University Medical Centre of Aachen, Germany, revealed that the pathogens most frequently cultured were S. epidermidis, S. aureus, E. faecalis, and Methicillin-resistant Staph aureus (MRSA) in patients undergoing revision surgery for PJI of THA and TKA. Interestingly, the study reported that preoperative synovial fluid aspiration was positive in 37% of cases, intraoperative microbiology was positive in 85%, and bacteraemia was present in 17% of patients. These findings underscore the persistent challenge of PJIs, necessitating efficient diagnostic methods [40].
In summary, PET/CT can provide crucial information in the diagnosis and management of periprosthetic infections of the hip joint, due to its high sensitivity and specificity, its ability to provide functional and anatomic information in a single examination and its ability to monitor the treatment effectiveness [41].
The current study evidence has several strengths compared to previous reviews. First, this review contains the maximum number of studies on this research question. Second, most studies in our review were higher quality studies, enhancing the credibility of the available evidence. Third, there was no significant publication bias, further enhancing the reliability of the evidence. Finally, additional analysis to check the clinical utility, applicability and meta-regression was performed.
Limitations
Our review also has certain limitations. There was significant heterogeneity in the study analysis, which was explored by means of meta-regression. Influence of various factors that might influence the accuracy parameters could not be explored, due to limitations of the study under each of the subcategories.
Conclusions
Nonetheless, the current review findings are essential for the clinicians and surgeons involved in the management of patients with periprosthetic joint infection. PET/CT is a good enough diagnostic method and can be applied in patients suspected of having periprosthetic infection of the hip. To the already existing advantages in terms of time and cost reduction, the evidence of high level of accuracy can be added as another major advantage to be included in the standard protocol of these patients. Utilizing this imaging modality will help to start the treatment early leading to better patient outcomes. More prospective studies can be performed to check whether this can be used as confirmatory test, as it has not reached such levels as per the current review findings. Further large-scale research can help to find answers for such questions and provide final conclusive evidence on the inclusion of the imaging modality into the routine clinical practice guidelines for suspected periprosthetic joint infection patients.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
14 November 2023
A Correction to this paper has been published: https://doi.org/10.1186/s13018-023-04345-9
References
MaraditKremers H, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–97.
Matharu GS, Culliford DJ, Blom AW, Judge A. Projections for primary hip and knee replacement surgery up to the year 2060: an analysis based on data from The National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Ann R Coll Surg Engl. 2022;104(6):443–8. https://doi.org/10.1308/rcsann.2021.0206.
Labek G, Thaler M, Janda W, et al. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–7.
Kapadia BH, Berg RA, Daley JA, et al. Periprosthetic joint infection. Lancet. 2016;387:386–94.
Charette RS, Melnic CM. Two-stage revision arthroplasty for the treatment of prosthetic joint infection. Curr Rev Musculoskelet Med. 2018;11:332–40.
Tubb CC, Polkowksi GG, Krause B. Diagnosis and Prevention of Periprosthetic Joint Infections. J Am Acad Orthop Surg. 2020;28(8):e340–8. https://doi.org/10.5435/JAAOS-D-19-00405.
Romanò CL, Petrosillo N, Argento G, Sconfienza LM, Treglia G, Alavi A, et al. The role of imaging techniques to define a peri-prosthetic hip and knee joint infection: multidisciplinary consensus statements. J Clin Med. 2020;9(8):2548. https://doi.org/10.3390/jcm9082548.
Basu S, Kwee TC, Saboury B, et al. FDG PET for diagnosing infection in hip and knee prostheses: prospective study in 221 prostheses and subgroup comparison with combined (111) In-labeled leukocyte/(99m)Tc-sulfur colloid bone marrow imaging in 88 prostheses. Clin Nucl Med. 2014;39:609–15.
Kwee RM, Broos WA, Brans B, et al. Added value of 18F-FDG PET/CT in diagnosing infected hip prosthesis. Acta Radiol. 2018;59:569–76.
García-Barrecheguren E, Rodríguez Fraile M, Toledo Santana G, ValentíNín JR, Richter Echevarría JA. 18FDG-PET: a new diagnostic approach in hip prosthesis infection. Revista Española de Medicina Nuclear (English edition). 2007;26(4):208–20.
Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22(1):128.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Int Med. 2011;155(8):529–36.
Xu T, Zeng Y, Yang X, Liu G, Lv T, Yang H, et al. Application of 68 Ga-citrate PET/CT for differentiating periprosthetic joint infection from aseptic loosening after joint replacement surgery. Bone Joint Res. 2022;11(6):398–408.
Kumar R, Kumar R, Kumar V, Malhotra R. Comparative analysis of dual-phase 18F-fluoride PET/CT and three phase bone scintigraphy in the evaluation of septic (or painful) hip prostheses: A prospective study. J Orthop Sci. 2016;21(2):205–10.
Pill SG, Parvizi J, Tang PH, Garino JP, Nelson C, Zhuang H, et al. Comparison of fluorodeoxyglucose positron emission tomography and 111indium–white blood cell imaging in the diagnosis of periprosthetic infection of the hip. J Arthroplasty. 2006;21(6):91–7.
Chen SH, Ho KC, Hsieh PH, Lee MSS, Yen TC. Potential clinical role of 18F FDG-PET/CT in detecting hip prosthesis infection: a study in patients undergoing two-stage revision arthroplasty with an interim spacer. Q J Nucl Med Mol Imaging. 2010;54:429–35.
Teiler J. Leukocyte scintigraphy, SPECT/CT and PET/CT in the diagnosis of prosthetic joint infection. 2021. Thesis. Available from: https://openarchive.ki.se/xmlui/handle/10616/47709
Love C, Marwin SE, Tomas MB, Krauss ES, Bhargava KK, Nichols KJ, et al. Diagnosing infection in the failed joint replacement: a comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J Nucl Med. 2004;45:1864–71.
Wang Y, Wang R, Zhang X, Li L, Liu H, Chang Y, et al. Diagnostic performance of [68Ga]Ga-DOTA-FAPI-04 for periprosthetic hip joint infection. In Review; 2022. Available from: https://www.researchsquare.com/article/rs-2330193/v1
Kiran M, Donnelly TD, Armstrong C, Kapoor B, Kumar G, Peter V. Diagnostic utility of fluorodeoxyglucose positron emission tomography in prosthetic joint infection based on MSIS criteria. Bone Joint J. 2019;101-B(8):910–4.
Mumme T, Reinartz P, Alfer J, Müller-Rath R, Buell U, Wirtz DC. Diagnostic values of positron emission tomography versus triple-phase bone scan in hip arthroplasty loosening. Arch Orthop Trauma Surg. 2005;125(5):322–9.
Aksoy SY, Asa S, Ozhan M, Ocak M, Sager MS, Erkan ME, et al. FDG and FDG-labelled leucocyte PET/CT in the imaging of prosthetic joint infection. Eur J Nucl Med Mol Imaging. 2014;41(3):556–64.
Stumpe KDM, Nötzli HP, Zanetti M, Kamel EM, Hany TF, Görres GW, et al. FDG PET for differentiation of infection and aseptic loosening in total hip replacements: comparison with conventional radiography and three-phase bone scintigraphy. Radiology. 2004;231(2):333–41.
Chryssikos T, Parvizi J, Ghanem E, Newberg A, Zhuang H, Alavi A. FDG-PET imaging can diagnose periprosthetic infection of the hip. Clin Orthop Related Res. 2008;466(6):1338–42.
Verberne SJ, Temmerman OPP, Vuong BH, Raijmakers PG. Fluorodeoxyglucose positron emission tomography imaging for diagnosing periprosthetic hip infection: the importance of diagnostic criteria. Int Orthop. 2018;42(9):2025–34.
Kumar R, Kumar R, Kumar V, Malhotra R. Potential clinical implication of 18 F-FDG PET/CT in diagnosis of periprosthetic infection and its comparison with 18 F-Fluoride PET/CT. J Med Imaging Radiat Oncol. 2016;60(3):315–22.
Tseng JR, Chang YH, Yang LY, Wu CT, Chen SY, Wan CH, et al. Potential usefulness of 68Ga-citrate PET/CT in detecting infected lower limb prostheses. EJNMMI Res. 2019;9(1):2.
Reinartz P, Mumme T, Hermanns B, Cremerius U, Wirtz DC, Schaefer WM, et al. Radionuclide imaging of the painful hip arthroplasty: positron-emission tomography versus triple-phase bone scanning. J Bone Joint Surg British. 2005;87(4):465–70.
Chacko TK, Zhuang H, Stevenson K, Moussavian B, Alavi A. The importance of the location of fluorodeoxyglucose uptake in periprosthetic infection in painful hip prostheses. Nucl Med Commun. 2002;23(9):851–5.
Zhuang H, Duarte PS, Pourdehnad M, Maes A, Acker FV, Shnier D, et al. The promising role of 18F-FDG PET in detecting infected lower limb prosthesis implants. J Nucl Med. 2001;42:44–8.
Aleksyniene R, Iyer V, Bertelsen HC, Nilsson MF, Khalid V, Schønheyder HC, et al. The role of nuclear medicine imaging with 18F-FDG PET/CT, combined 111In-WBC/99mTc-Nanocoll, and 99mTc-HDP SPECT/CT in the evaluation of patients with chronic problems after TKA or THA in a prospective study. Diagnostics. 2022;12(3):681.
Manthey N, Reinhard P, Moog F, Knesewitsch P, Hahn K, Tatsch K. The use of [18F]fluorodeoxyglucose positron emission tomography to differentiate between synovitis, loosening and infection of hip and knee prostheses. Nucl Med Commun. 2002;23(7):645–53.
Vanquickenborne B, Maes A, Nuyts J, Acker F, Stuyck J, Mulier M, et al. The value of 18FDG-PET for the detection of infected hip prosthesis. Eur J Nucl Med Mol Imaging. 2003;30(5):705–15.
Mayer-Wagner S, Mayer W, Maegerlein S, Linke R, Jansson V, Müller PE. Use of 18F-FDG-PET in the diagnosis of endoprosthetic loosening of knee and hip implants. Arch Orthop Trauma Surg. 2010;130(10):1231–8.
Kobayashi N, Inaba Y, Choe H, Ike H, Fujimaki H, Tezuka T, et al. Use of F-18 fluoride PET to differentiate septic from aseptic loosening in total hip arthroplasty patients. Clin Nuclear Med. 2011;36(11):e156–61.
Verberne SJ, Raijmakers PG, Temmerman OP. The accuracy of imaging techniques in the assessment of periprosthetic hip infection: a systematic review and meta-analysis. JBJS. 2016;98(19):1638–45.
Hu M, Chen G, Luo L, Shang L. A systematic review and meta-analysis on the accuracy of fluorodeoxyglucose positron emission tomography/computerized tomography for diagnosing periprosthetic joint infections. Front Surg. 2022;9:698781. https://doi.org/10.3389/fsurg.2022.698781.
Verberne SJ, Sonnega RJ, Temmerman OP, Raijmakers PG. What is the accuracy of nuclear imaging in the assessment of periprosthetic knee infection? A meta-analysis. Clin Orthop Related Res. 2017;475(5):1395–410.
Hao R, Yuan L, Kan Y, Yang J. 18F-FDG PET for diagnosing painful arthroplasty/prosthetic joint infection. Clin Transl Imaging. 2017;5(4):315–22.
Migliorini F, Weber CD, Bell A, Betsch M, Maffulli N, Poth V, et al. Bacterial pathogens and in-hospital mortality in revision surgery for periprosthetic joint infection of the hip and knee: analysis of 346 patients. Eur J Med Res. 2023;28(1):177. https://doi.org/10.1186/s40001-023-01138-y.
Kung BT, Seraj SM, Zadeh MZ, Rojulpote C, Kothekar E, Ayubcha C, et al. An update on the role of 18F-FDG-PET/CT in major infectious and inflammatory diseases. Am J Nucl Med Mol Imaging. 2019;9(6):255–73.
Acknowledgements
None declared.
Funding
No Funding was received.
Author information
Authors and Affiliations
Contributions
HH: Concept and designed the study, and analysed data; JL: Collected the data and helped in data analysis and drafting of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee of the **an Central Hospital Affiliated to Shandong First Medical University. Furthermore, comply with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Furthermore, the written informed consent was taken from all the patients.
Consent to publish
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search Strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hua, H., Liu, J. Diagnostic accuracy of positron emission tomography/computerized tomography for periprosthetic joint infection of hip: systematic review and meta-analysis. J Orthop Surg Res 18, 640 (2023). https://doi.org/10.1186/s13018-023-04061-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04061-4