Abstract
Background
The spleen is the second most commonly injured organ in cases of abdominal trauma. Management of splenic injury depends on the clinical status of the patient and can include nonoperative management (NOM), splenic artery embolization (SAE), surgery (operative splenic salvage or splenectomy), or a combination of these treatments. In nonoperatively managed cases, SAE is sometimes used to control haemorrhage. However, the indications for SAE have not been clearly defined and, in some cases, the potential complications of the procedure may outweigh its benefits.
Review of the literature
Through review of the literature we address the question of when SAE is indicated in combination with NOM of splenic injury, and whether SAE may delay needed surgical treatment in some cases. This systematic review highlighted the use of imperfect and inconsistent scoring systems in the diagnosis of splenic injury, the lack of consensus regarding indications for SAE, and the potential for severe morbidities associated with this procedure. Based on current literature and evidence we provide a new, non-verified, decision algorithm.
Conclusions
NOM+ SAE involves potential risks and operative management may be preferable to SAE for certain patients. To clarify current literature, we propose a new algorithm for blunt abdominal trauma that should be validated prospectively. New evidence-based protocols should be developed to guide diagnosis and management of patients with splenic trauma.
Similar content being viewed by others
Background
Abdominal injury occurs in approximately 20–30 % of all trauma patients. The spleen is the second most commonly injured organ in both blunt and penetrating abdominal trauma [1, 2].
Raza et al. reviewed 1285 cases of abdominal trauma over a ten-year period; 26 % of these suffered a splenic injury. Of the patients in the initial study group, 89.91 % were managed without surgery and 30 % of these had a splenic injury. The initial presentation of splenic injury can be variable and depends on the severity of the associated injuries, the amount of blood lost, and the mechanism of trauma. Routine diagnostic workup of suspected splenic injury includes chest radiographs, abdominal ultrasound, a focused assessment with sonography for trauma (FAST) scan, or CT imaging. Abdominal CT imaging with intravenous contrast is the preferred imaging method in hemodynamically stable patients; when the patient is in an unstable condition, a FAST scan that shows the presence of free within the abdomen can indicate that emergency surgery is necessary. Physicians and surgeons should remain alert for concomitant injuries to the liver (the organ most frequently injured by blunt abdominal trauma) and other intra-abdominal organs.
Splenic artery embolization (SAE) is increasingly being used in medical practice. This trend started in the 1970s when Maddison reported the first successful SAE in a patient with esophageal varices, hepatic cirrhosis, and recurrent gastrointestinal bleeding [3]. In 1975, Chuang and Reuter reported successful SAE after splenic injury in ten dogs [4]. In 1985, Sclafani et al. reported that embolization of 107 arterial injuries yielded an 82.2 % success rate [5]. There was a further evolution towards proximal SAE or more distal and selective embolization of the branches of the splenic artery.
Until the 1990s splenectomy remained the treatment of choice for splenic injury, but nonoperative management (NOM) became increasingly popular in the pediatric setting around 1992 when Haller et al. reported on the safety of NOM of solid organ injuries in children [6]. Sclafani reported in 1995 a study of 172 patients and the use angiography with subsequent use of proximal embolization of the splenic artery when extravasation was present [7]. In his study NOM was used in stable patients with no extravasation on angiography, splenectomy or splenorrhaphy was performed in unstable patients or in patients with associated injuries or disease. Overall splenic salvage rate was 88 % with a splenic salvage rate of 97 % in the patients managed non-operatively.
The first large multi-institutional study was published in 2000 by Peitzman et al. [8]. In this EAST study 1488 patients with blunt splenic injury were reviewed. The authors report operative management in 38,5 % of the patients and immediate operative management was proportional to the grade of injury. In patient groups with a larger hemoperitoneum, more laparotomies were performed. They further report a NOM failure rate of 10,8 % of which 60,9 % within the first 24 h of admittance. 54,8 % of the patients were successfully managed nonoperatively.
In 2005 Haan reported on 648 patients in a single institution study with splenic salvage rates of 90 % after SAE and 100 % after planned NOM [9]. Failure of NOM increased with higher injury grades but 80 % of grade IV and V injuries were successfully managed nonoperatively. Interestingly, a 40 % failure rate was reported when an arteriovenous fistula was present, even after embolization.
Currently, between 60 and 80 % of splenic injuries are managed without surgery and the reported success rates for NOM range between 85 and 94 %. NOM can be combined with SAE when certain conditions are met, and retrospective studies have reported higher success rates and higher splenic salvage rates when NOM is combined with SAE [10–12]. However, no consensus has been reached on the correct indications for combining NOM and SAE, especially in higher grade splenic injuries. In the current literature, the use of NOM in combination with SAE for treatment of blunt splenic injury is dependent on multiple factors, which are: the grade of the splenic injury, the injury severity score (ISS), patient age, the presence of contrast blush on CT, active extravasation on angiography, need for transfusion, the presence of significant hemoperitoneum, and the presence of splenic artery pseudoaneurysms. Most trauma protocols consider hemodynamic instability or a high-grade splenic lesion (IV–V) to be indications for emergency laparotomy. Operative splenic salvage (OSS) or splenectomy can then be attempted. However, based on the currently available literature the use of NOM, SAE, or OSS is controversial. Retrospective review of data, small study groups, and changes in protocols or in standard practice make it difficult to draw conclusions regarding the optimal management of splenic injuries.
Methods & results
We reviewed the literature and used critical interpretive synthesis methodology in the following discussion. A search of the following databases was conducted during October 2015: Medline database, Trip database, EMBASE, Web of Science, Cochrane Library, and Scopus. We also manually searched the reference lists of the retrieved articles. Our search terms included: splenic injury, embolization, operative, management.
We included original research articles that reported on splenic injury in combination with embolization therapy, operative, and nonoperative management. Papers were excluded if they focused specifically on adolescent, pediatric, or neonatal populations and if they included specific diagnostic groups. Guidelines, surveys, and meta-analyses were also excluded. The search was executed sequentially and is documented in Table 1. All articles were assessed for relevance by reading the abstract and, where needed, the entire paper using the above criteria.
Duplicates were excluded and the final selection of articles was based on their relevance and quality. Papers were excluded if no full text could be obtained. To select high-quality studies, we assessed all articles following the Critical Review Form for Quantitative Studies and guidelines from Law et al. [13]. An overview of the selected articles is presented in Table 2. Excluded articles are also presented in Table 2 for reference. Despite the large amount of articles retrieved, we were not able to carry out a meta-analysis because of the heterogeneity of study methods, data and quality of articles.
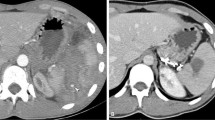
In order to further support the literature review we propose a new, non-verified, algorithm for blunt abdominal trauma, based on existing algorithms presented in the literature and modified according to our findings (Fig. 1).
Algorithm for management of splenic trauma modified from Ekeh and Tugnoli [8, 28]. Abbreviations: HD: hemodynamically; BP: blood pressure; FAST: Focused Assessment with Sonography for Trauma; ICU: Intensive Care Unit; SAE: splenic artery embolization; MDCT: Multidetector CT grading (Table 4); NOM: non operative management; CE: contrast extravasation; IV: intravenous
Discussion
Hemodynamically unstable patients
Abdominal trauma with hemodynamic instability is an absolute indication for operative management in most protocols. However, in cases of splenic injury, SAE and NOM is increasingly being performed even in patients that are hemodynamically unstable. The use of NOM or SAE in hemodynamically unstable patients is highly controversial and should be further studied. Delays in diagnostic testing and inappropriate selection of hemodynamically unstable patients for this treatment protocol could increase morbidity and mortality rates, as some authors have suggested [14–16]. Importantly, there has been little research on managing patients with transient hemodynamic stability, although Hagiwara et al. did report successful SAE in 15 patients with transient responses to fluid administration [17].
Most studies in the literature are retrospective case series that describe the immediate technical success of SAE without comparisons with surgical treatment or a purely conservative approach. Operative intervention by means of splenectomy is thought to increase morbidity and mortality rates, but this is biased by higher injury severity scores in patients that are surgically managed. A large study of 11,793 patients by Zarzaur et al. (2011) could not confirm a correlation between splenectomy and in-hospital mortality when the data were corrected for demographic, physiologic, and injury-related factors [18]. The risk of overwhelming post-splenectomy sepsis has been advocated as a concern and relative contraindication for splenectomy; however, this rare complication occurs in only approximately 0.9 % of splenectomy cases and is preventable by immunization [19]. A recent, large, population-based study classified 9719 patients with splenic injuries into two groups, splenectomy or non-splenectomy, and compared these against a control group of 30,413 patients with other abdominal injuries. This study warned of a two-fold increased risk of develo** type II diabetes post-splenectomy [20]. In contrast, some authors have reported higher morbidity after SAE than after surgical intervention [21]. In addition, there is evidence of splenic functional alterations after SAE, although research suggests that no immunizations are necessary after NOM combined with SAE [22]. In a 2010 paper, Shih and colleagues demonstrated a cytokine hyporesponse after SAE [23] therefore, SAE should not be considered definitively safer than splenectomy.
Hemodynamically stable patients
SAE, as opposed to pure conservative management, is even more difficult to advocate in hemodynamically stable patients. In a 2015 study, Olthoff et al. looked at the management of 253 patients with splenic injury in Dutch trauma centers taking into account hemodynamic instability on admission, high-grade injury, and ISS [24]. Although the rate of NOM was comparable between the five trauma centers reviewed, the use of SAE for splenic injuries was highly variable between the centers, illustrating the lack of consensus that exists regarding the management of blunt splenic injury.
In hemodynamically stable patients, retrospective studies have shown that NOM has a reduced failure rate when combined with SAE [12, 25–30], but prospective studies and certain retrospective studies have failed to confirm these findings [11, 15]. Several studies have been published that show increased numbers of both minor and major complications, leading to an increase in time spent in the hospital, with the use of SAE [15, 31–33]. Moreover, there is no consensus on the follow-up management and imaging of patients with splenic injuries. Given the lack of evidence in the literature, Olthof et al. published a study in 2013 using the Delphi method to reach an expert opinion on the optimal management and follow-up protocol for blunt splenic injury [28]. In several questionnaires, trauma surgeons and interventional radiologists have tried to reach consensus on the indications for, and optimal follow-up management and imaging to use with, NOM combined with SAE. Almost all of the experts used the American Association for the Surgery of Trauma (AAST) scoring system to grade splenic injuries (Table 3). They all agreed on the use of NOM with or without SAE in small graded injuries (I–II) with no or only a small hemoperitoneum. In high-grade injuries (III–V) with a large hemoperitoneum and active contrast extravasation half of the experts would still attempt NOM + SAE, but most of them would not make a second attempt if the initial SAE failed. Most importantly, they all agreed that rapid intervention is needed for SAE to succeed. Current recommendations are that intervention should be performed within 60 min of admission in stable patients with active contrast extravasation and within 15 to 30 min when a large hemoperitoneum is present. No consensus was reached on management after failure of the initial NOM, or on the appropriate length of stay (LOS) in the hospital.
In search of better criteria for determining the need for intervention, Koca et al. correlated the results of NOM with the American Association for the Surgery of Trauma (AAST) splenic injury grade (see below) [34]. They found that hemodynamically stable patients can safely be treated with NOM, including patients with multi-organ injuries and higher grade splenic injuries. Most injuries are lower grade injuries (I–III), and not surprisingly transfusion is correlated with the injury grade. A 2008 article by Gonzalez et al. added the degree of hemoperitoneum and associated injuries as predictive factors for NOM failure [35]. In 2004, Wahl and colleagues retrospectively analyzed 164 patients with blunt splenic injuries; [36] after univariate analysis they found that lower blood pressure, higher ISS, lower pH, and more packed RBC transfusions are the best indicators of the need for operative intervention. Age, heart rate, splenic abbreviated injury scale score, and GCS did not significantly correlate with the need for operative management. Similarly, Tugnoli et al. (2014) presented the algorithm used in the Bologna-Maggiore Hospital; in 293 patients with splenic injuries admitted between 2009 and 2013 [37] they reported a NOM success rate of 95.8 %. All hemodynamically stable cases with active contrast extravasation or grade V injuries were embolized, preferably proximally within the splenic artery.
In a 2015 AAST prospective observational study, Zarzaur et al. investigated the risk of delayed splenectomy after NOM with or without SAE [38]. They found that the only risk factor for delayed splenectomy was the finding of active extravasation at presentation; thus calling for closer observation of patients with this finding irrespective of whether SAE was performed. Patients with grade I injury had no risk for delayed splenectomy. In cases with higher grade (II to V) injuries, the authors advocated close observation for 10–14 days. In the 2005 study of Haan et al. the presence of arteriovenous fistula on CT imaging was predictive for 40 % of failure rates in nonoperatively managed patients [9]. The presence of vascular lesions (arteriovenous fistulas, pseudoaneurysms) and impact on NOM success rates was further investigated by several authors. In a 2014 study, the Wake Forest University investigated failure rates after angiography with subsequent embolization, ignoring presence or absence of any vascular lesion, for all grade III to V splenic injuries in stable patients in a protocolized manner and comparing this to a historic control group [39]. From 168 patients 67 % were managed nonoperatively with an overall NOM failure rate of 5 %. In the patient group where protocol was violated the failure rate was 25 % compared to 3 % in the protocol group (P = 0.03). Comparing this to a historic control group, 52 % patients underwent NOM with a significant higher failure rate of 15 % (P = 0.04). For each injury grade they reported lower failure rates in the study group compared to the control group and when protocol was followed. However, they did not reach statistical significance when comparing patients treated according to protocol or patients deviating from protocol in injury grades IV and V. The authors did not report on complications or on splenic function after embolization in their study group, no data is available whether proximal or distal embolization was used.
Another prospective study from Parihar et al. [40] found a shorter LOS in SAE patients (5.4 days compared with 6.6 days for NOM patients without SAE), as well as higher hemoglobin concentrations and systolic blood pressures. A recent study, which used propensity score analysis, found no statistically significant difference between observation and embolization in the subsequent splenectomy rate [41].
Scoring systems
Many scoring systems have been developed to grade splenic injuries, among which the AAST grading system for splenic injury (Table 3) is the most popular. Two separate studies have correlated CT findings with the AAST injury grade and subsequent need for intervention. In the study by Barquist et al. [42], four radiologists retrospectively reviewed 200 CT images of patients who had undergone splenectomy; the operative grading of the splenic injuries was used as a gold standard. The weighted kappa score for intrarater reproducibility was 0.15–0.77 and the interrater kappa score was 0–0.84 (mean 0.23). In the study by Cohn et al. [43], five radiologists reviewed CT scans of 300 patients with liver and splenic injuries using the AAST grading system. Twenty-one percent of the patients with splenic injuries visible on CT images required intervention. Cohn et al. reached the same conclusion as Barquist et al.; the sensitivity of the AAST injury grade for predicting the need for intervention is poor and interrater variability, even among experienced radiologists, is high. Both thus concluded that the AAST scoring system is unreliable because even experienced radiologists often underestimate the magnitude of the injury, and other factors should also be considered when evaluating indications for surgery or angiography. The authors also evaluated kappa scores for the reporting of contrast blush on CT imaging and found that they were similarly variable, although contrast blush on CT imaging is considered a major indication that intervention is needed.
In 2001, Protetch et al. reported that the incidence of contrast blush was related to the grade of injury, with 3.2 % of grade I/II injuries and up to 37.6 % of grade IV and V injuries showing a contrast blush in CT images [44]. Interventions were more frequent when a contrast blush was present, but multivariate regression analysis showed no correlation between finding a contrast blush and splenic intervention. This was confirmed by both Thompson et al. and Michailidou et al.; both also reported that the size of the contrast blush was correlated with the need for intervention [45, 46]. They both found that similar cut-off values (1 cm and 1.5 cm) indicated the need for intervention. Other factors that also correlated with the need for intervention in splenic injury were injury grade, hypotension on admission to the emergency department, and age. The findings of these studies support the need for better protocols and parameters to allow proper assessment of the need for intervention in cases of splenic trauma.
In 2007, Marmery et al. suggested a new grading system for splenic injury that takes into account active bleeding or splenic vascular injury (including splenic pseudoaneurysms and arteriovenous fistulas) [47]. Their new grading system was statistically significantly better than the AAST grading system in terms of its ability to predict the need for splenic arteriography (P = 0.0036) or the combination of arteriography and surgery (P = 0.0006). Table 4 presents the proposed new grading system.
Complications
There has been much research published, and work is still ongoing, to understand the complications after SAE compared with those after surgery and NOM. All of the treatment modalities for splenic injury are associated with high morbidity rates. Specific morbidities associated with SAE include pancreatitis, splenic infarction, post-embolization syndrome, and intestinal perforation.
Two retrospective studies examined the complications that occur after SAE [32, 33]. Ekeh et al. reviewed 1383 patients with blunt splenic injury over an 11-year period; 78.5 % were treated nonoperatively, and of this group 8.1 % underwent SAE. Major complications including splenic infarction, splenic abscess, contrast-induced renal insufficiency, and splenic cysts occurred in 14 % of the patients who underwent SAE. Wu et al. reported that 28.5 % of patients who underwent SAE experienced major complications. Distal embolization was associated with more major complications than proximal SAE. Minor complications (pleural effusion, coil migration, and fever) occurred in 34 % and 61.9 % of the patients in the SAE groups in the studies by Ekeh et al. and Wu et al., respectively.
In 2004, Haan et al. reported SAE complication rates in 140 patients and reported a splenic salvage rate of 87 % [31]. This rate indirectly correlated with injury severity scores. More than 80 % of the grade IV and V injuries in their study were successfully managed nonoperatively. No significant difference was noted in patients older than 55 years of age. The presence of a significant hemoperitoneum did not alter success rates; however, the presence of arteriovenous fistulas did. They concluded that complications after SAE are common, but do not seem to influence outcomes.
In 2008, Wei et al. published a retrospective study showing lower complication rates after SAE even with higher splenic Abbreviated Injury Scores in this group compared with the operatively managed group (6 % vs. 36 %, P < 0.01) [30]. They found that the introduction of SAE reduced operative interventions by 16 % between 2000 and 2006 in their Level 1 center. A French prospective multicenter study investigated complication rates in 91 patients [21]. Twenty percent underwent splenectomy with a post-surgical morbidity of 15 %. Fifteen patients (16 %) underwent embolization and 67 were initially managed nonoperatively. In the embolization group with severe injury (grade III–V), the morbidity was 73 %. The splenectomy group with severe injury had a total morbidity of 70 %. The NOM group had a morbidity of 58 %. Specific morbidities after NOM, surgery, and SAE were 10, 15, and 47 % (P = 0.02), respectively. The study concluded that embolization should not be used as a prophylactic measure, but should only be used in cases with active bleeding. We could not find well-designed studies comparing complication rates between the three treatment modalities.
Other factors to be considered
-
Need for transfusion
In their 2015 study of 253 patients, Olthoff et al. found a very large variation but no significant difference in the need for transfusion between patients treated with SAE and those treated with NOM [24]. The mean number of transfused blood products was 5.5 units (±9.9) in the NOM group versus 9.1 units (±17.2) in embolized patients (P = 0.75). Rosati et al. reported on the need for transfusion in patients requiring immediate splenectomy (70 %), embolization (46.5 %), and NOM (25.9 %), but failed to adjust these data for injury severity and confounders [12]. They found that the need for transfusion was a major risk factor for mortality (adjusted OR = 2.63; CI 1.27 – 5.42, P = 0.009). Dent et al. compared transfusion rates between NOM, early embolization, and operative management [25]. They reported a 2.1-unit difference in the transfusion rate (P < 0.01) of the NOM group versus the operative management group, and found no statistically significant difference between transfusion rates in the early embolization and operative management groups without correcting for confounders. They also found no difference in transfusion rates when they compared patients who underwent early embolization versus late embolization.
-
Impact of direct supervision
A retrospective review in 2011 investigated the impact of direct supervision (DS) or indirect supervision (IS) on the management of splenic injuries [48]. Using data from 506 cases the authors found significant differences in compliance with protocols (DS, 95 % vs. IS, 82 %, P < 0.001), operation rates (DS 16 %, vs. IS, 8 %, P = 0.016), ICU use (IS, 84.1 % vs. DS, 73.0 %, P = 0.029), hospital costs (IS, $142.956 ± $36.219 vs. DS, $62.981 ± $8.784, P = 0.048), and use of SAE without indication (IS, 8 vs. DS, 0). Interestingly, there were no reported differences in mortality or splenectomy rates.
-
Time to intervention and volume of the centers.
In 2014, Olthof et al. retrospectively examined the time to intervention in patients undergoing SAE and patients undergoing surgery in a cohort of 96 adults [49]. In hemodynamically stable patients, the median time to intervention for patients in the SAE group was 117 min compared with 105 min for patients in the surgery group. The differences in time to intervention or re-intervention, and the complication rates were not significantly different between the two patient groups. There was a higher transfusion rate for patients in the splenic surgery group; the median number of transfused units of packed RBCs was eight for hemodynamically unstable patients undergoing SAE versus 24 for patients undergoing splenic surgery (P = 0.09). A report published in 2015 reviewed 10,405 records in the National Trauma Data Bank to find a correlation between high and low angio centers and to investigate any relationship between angiography use and its timing or splenectomy after angiography [50]. They concluded that early angiography is associated with higher splenic salvage rates but found no statistically significant difference in splenectomy rates between the high and low angiography volume centers.
We could not find any articles comparing the relationship between time to intervention and success or complication rates between patients undergoing NOM, SAE, or splenic surgery.
-
Costs & Length of stay
Different authors have investigated the costs of SAE versus surgical management. Wahl et al. reported no significant cost differences between these two treatment modalities (SAE, $49.300 ± $40.460 vs. OM, $54.590 ± $34.760) [36]. This was confirmed by Wei et al., who found the costs associated with SAE to be $47,000 ± $31,000 and the costs associated with OM to be $40,000 ± $34,000 [30]. Both authors assessed the LOS and differences in LOS in patients who received different treatments. Wahl et al. found an average LOS of 45 ± 26 days for patients who went directly to the operating theatre, compared with 14 ± 15 days for patients who underwent SAE (P < 0.02). Wei et al. found that the average LOS in the surgical group was 14 ± 10 days and in the SAE group was 12 ± 12 days (P > 0.05). Bruce et al. also came to the same conclusion in their 2011 study; [51] in that study the median total hospital charges were $41,269 (± $31,128) for the NOM + SAE group compared with $46,356 (± $11,334) for the OM group (P = 0.545). They did report higher procedure-related charges for OM patients compared with patients undergoing NOM + SAE ($28,709 ± $6941 vs. $19,062 ± $14,025; P = 0.16); however, this was offset by more charges for a greater number of radiological evaluations in the other group.
Summary
Based on the literature review we propose a new, non-verified, decision algorithm for splenic trauma. We hope this can further serve as a tree of order in the vast amount of publications concerning this topic. We stress that this algorithm is not verified and should be further verified in well designed, prospective studies, is it to be used in daily practice.
The term hemodynamically unstable is not clearly defined in most literature and it is often unclear if authors included or excluded transient responders. The nature of the patient’s response to fluid therapy is important and should be considered in all splenic trauma protocols. Most authors agree that surgical intervention is indicated when the patient is hemodynamically unstable. In close relation with response to fluid resuscitation is time to intervention, which is an important factor to consider from the start. Higher splenic salvage rates are achieved when earlier intervention is possible and expert opinion states that intervention is recommended within one hour of admittance. In prospect, when the time to intervention will be several hours OM or NOM may be better options than SAE, depending on the clinical presentation. Clinicians and surgeons should always keep in mind that pre- and post-intervention delays make it increasingly difficult to operate because of the several surgical and nonsurgical issues that can develop (e.g., clotting of the intraperitoneal hemorrhage, infection, and development of comorbidities). Non responders should be triaged promptly with a minimal delay towards surgical intervention.
There is a distinction between major and minor complications and treatment-specific morbidities. While it is difficult to correlate complications with the embolization procedure, especially in small studies, it is interesting to look at treatment-specific complications and associated risk-benefit ratios; however, no well-designed studies compare NOM, NOM + SAE, and OM for the treatment of splenic trauma. Until such studies are available, we should look at the clinical value and possible risks of an intervention on a patient-specific level while considering all factors, and kee** in mind the relatively high complication rate after SAE. It is important to avoid the bias of expecting operative interventions to have higher complication rates than SAE, which seems like a less invasive procedure. Increased use of NOM with or without SAE should not erode clinical judgment and surgical skills.
Currently there is no evidence of reduced transfusion rates when SAE is used in conjunction with NOM compared with NOM alone. Transfusion rates are higher in patients who undergo an operative intervention and are a risk factor for mortality; however, no studies are available that compare similar patient groups and their corresponding transfusion rates.
Multiple studies have reported on the cost effectiveness of splenic injury management: operative intervention brings the costs of surgery and of higher transfusion rates; however, conversely NOM + SAE requires higher imaging costs and there is ultimately no significant difference between the costs of the two interventions.
We reviewed the different scoring systems and the use of imaging for diagnosing splenic injuries. As imaging modalities improve smaller bleeds are increasingly being visualized. It is known that these bleeds can be self-limiting; however, no studies have shown the clinical significance of these small bleeds and other radiological findings such as pseudoaneurysms and arteriovenous fistulas. Additional studies will be needed to assess whether embolization is superior to NOM in these cases. Studies have shown important interrater and intrarater differences in image evaluation in cases of splenic injury, and more specifically in the assessment of a contrast blush on CT imaging. Contrast blush is considered an important parameter for assessment of the need for intervention but recent studies have shown that the size of the contrast blush is what matters. Though whether a cut-off value of 1 cm or 1.5 cm is more suitable for determining the optimal treatment is not yet known. According to the literature, the presence of a hemoperitoneum does not alter the success rates of SAE.
The MDCT grading system proposed by Marmery et al. has shown a better correlation with the need for intervention than the conventionally used AAST grading system. Currently, there is no consensus on the use of one grading system that correlates well with the need for intervention, and most published studies have used the AAST grading system. Lack of standardized grading makes it difficult to compare older studies with recent and future studies. Interpreting CT images and grading the splenic injury is difficult and should be performed by experienced radiologists using the proposed grading system with a consistent technique. We propose the use of specific image analysis protocols to achieve a consistent approach and improve future studies. We propose the use of the MDCT grading system in our decision algorithm.
The treatment plan should be managed by experienced trauma surgeons or interventional radiologists using a multidisciplinary approach when possible. It should be clear who is responsible for assessing the indications for SAE, NOM, or OM. The literature has shown better results when protocols are in place; and ideally there should be consensus on who is responsible for initiating treatment.
Conclusions
The current literature is unclear on the correct indications for NOM ± SAE versus surgery for splenic trauma. To further clarify current evidence we propose, a non-verified, decision algorithm for blunt abdominal trauma. A prospective well designed study is needed to validate our decision algorithm. Consensus on the management of blunt splenic injury between radiologists, trauma surgeons and emergency medicine physicians could reduce conflicting data, improve current protocols, and avoid harm to patients. More prospective data and well-designed studies, taking into account other factors including long term results and morbidity, on the management of splenic trauma are needed.
Abbreviations
- AAST:
-
American Association for the Surgery of Trauma
- BP:
-
Blood pressure
- CE:
-
Contrast extravasation
- DS:
-
Direct supervision
- FAST scan:
-
Focused assessment with sonography for trauma
- GCS:
-
Glasgow coma scale
- HD:
-
Hemodynamically
- ICU:
-
Intensive care unit
- IS:
-
Indirect supervision
- ISS:
-
Injury severity score
- IV:
-
Intravenous
- LOS:
-
Length of stay
- MDCT:
-
Multidetector computer tomography
- NOM:
-
Nonoperative management
- OM:
-
Operative management
- OR:
-
Operating room
- OSS:
-
Operative splenic salvage
- RBCs:
-
Red blood cells
- SAE:
-
Splenic artery embolization
References
Raza M, Abbas Y, Devi V, Prasad KV, Rizk KN, Nair PP. Nonoperative management of abdominal trauma -- a 10 years review. World J Emerg Surg. 2013;8(1):14.
Søreide K. Epidemiology of major trauma. Br J Surg. 2009;96(7):697–8.
Maddison FE. Embolic therapy of hypersplenism. Invest Radiol. 1973;8(4):280–1.
Chuang VP, Reuter SR. Selective arterial embolization for the control of traumatic splenic bleeding. Invest Radiol. 1975;10(1):18–24.
Panetta T, Sclafani SJA, Goldstein AS, Phillips TF. Percutaneous transcatheter embolization for arterial trauma. J Vasc Surg. 1985;2(1):54–64.
Haller Jr JA, Papa P, Drugas G, Colombani P. Nonoperative management of solid organ injuries in children. Is it safe? Ann Surg. 1994;219(6):625–8. discussion 628–631.
Sclafani S, Shafan GW, Scalea TM, et al. Nonoperative salvage of computed tomography--diagnosed splenic injuries : utilization of angiography for triage and embolization for hemostasis. J Trauma Injury Infect Crit Care. 1995;39(5):818–27.
Peitzman AB, Heil B, Rivera L, et al. Blunt splenic injury in adults: multi-institutional study of the Eastern association for the surgery of trauma. J Trauma. 2000;49(2):177–87. discussion 187–189.
Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma. 2005;58(3):492–8.
Fu C-Y, Wu S-C, Chen R-J, et al. Evaluation of need for operative intervention in blunt splenic injury: intraperitoneal contrast extravasation has an increased probability of requiring operative intervention. World J Surg. 2010;34(11):2745–51.
Ekeh AP, Izu B, Ryan M, McCarthy M. The impact of splenic artery embolization on the management of splenic trauma: an 8-year review. Am J Surg. 2009;197(3):337–41.
Rosati C, Ata A, Siskin GP, et al. Management of splenic trauma: a single institution’s 8-year experience. Am J Surg. 2015;209(2):308–14.
Law M, Stewart D, Letts L, Pollock N, Bosch J, Westmorland M. Guidelines for critical review form : qualitative studies. McMaster Univ Occup Ther Evidence-Based Pract Res Gr. 2007;1–12.
Cooney R, Ku J, Cherry R, et al. Limitations of splenic angioembolization in treating blunt splenic injury. J Trauma. 2005;59(4):926–32.
Peitzman AB, Harbrecht BG, Rivera L, Heil B. Eastern Association for the Surgery of Trauma Multi institutional Trials Workgroup. Failure of observation of blunt splenic injury in adults: variability in practice and adverse consequences. J Am Coll Surg. 2005;201(2):179–87.
Peitzman AB, Ferrada P, Puyana JC. Nonoperative management of blunt trauma: have we gone too far? Surg Infect. 2009;10(5):427–33.
Hagiwara A, Fukushima H, Murata A, Matsuda H, Shimazaki S. Blunt splenic injury: usefulness of transcatheter arterial embolization in patients with a transient response to fluid resuscitation. Radiology. 2005;235(1):57–64.
Zarzaur BL, Croce MA, Fabian TC. Variation in the use of urgent splenectomy after blunt splenic injury in adults. J Trauma. 2011;71(5):1333–9.
Holdsworth R, Irving A, Cuschieri A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br J Surg. 1991;78(9):1031–8.
Wu S-C, Fu C-Y, Muo C-H, Chang Y-J. Splenectomy in trauma patients is associated with an increased risk of postoperative type II diabetes: a nationwide population-based study. Am J Surg. 2014;208(5):811–6.
Chastang L, Bège T, Prudhomme M, et al. Is non-operative management of severe blunt splenic injury safer than embolization or surgery? Results from a French prospective multicenter study. J Visc Surg. 2015;152(2):85–91.
Skattum J, Titze TL, Dormagen JB, et al. Preserved splenic function after angioembolisation of high grade injury. Injury. 2012;43(1):62–6.
Shih H-C, Wang C-Y, Wen Y-S, et al. Spleen artery embolization aggravates endotoxin hyporesponse of peripheral blood mononuclear cells in patients with spleen injury. J Trauma. 2010;68(3):532–7.
Olthoff DC, Luitse JSK, de Rooij PP, et al. Variation in treatment of blunt splenic injury in Dutch academic trauma centers. J Surg Res. 2015;194(1):233–8.
Dent D, Alsabrook G, Erickson BA, et al. Blunt splenic injuries: high nonoperative management rate can be achieved with selective embolization. J Trauma. 2004;56(5):1063–7.
Dehli T, Bagenholm A, Trasti NC, et al. The treatment of spleen injuries: a retrospective study. Scand J Trauma Resusc Emerg Med. 2015;23(1):85.
Gaarder C, Dormagen JB, Eken T, et al. Nonoperative management of splenic injuries: improved results with angioembolization. J Trauma. 2006;61(1):192–8.
Olthof DC, van der Vlies CHCH, van der Vlies CHCH, et al. Consensus strategies for the nonoperative management of patients with blunt splenic injury: a Delphi study. J Trauma Acute Care Surg. 2013;74(6):1567–74.
Sabe AA, Claridge JA, Rosenblum DI, Lie K, Malangoni MA. The effects of splenic artery embolization on nonoperative management of blunt splenic injury: a 16-year experience. J Trauma. 2009;67(3):565.
Wei B, Hemmila MR, Arbabi S, et al. Angioembolization reduces operative intervention for blunt splenic injury. J Trauma. 2008;64(6):1472–7.
Haan JM, Biffl W, Knudson MM, et al. Splenic embolization revisited: a multicenter review. J Trauma. 2004;56(3):542–7.
Ekeh AP, Khalaf S, Ilyas S, et al. Complications arising from splenic artery embolization: a review of an 11-year experience. Am J Surg. 2013;205(3):250–4.
Wu S-C, Chen R-J, Yang AD, et al. Complications associated with embolization in the treatment of blunt splenic injury. World J Surg. 2008;32(3):476–82.
Koca B, Topgul K, Yuruker SS, Cinar H, Kuru B. Non-operative treatment approach for blunt splenic injury: is grade the unique criterion? J Trauma Emerg Surg. 2013;19(4):337–42.
Gonzalez M, Bucher P, Ris F, Andereggen E, Morel P. Splenic trauma: predictive factors for failure of non-operative management. J Chir (Paris). 2008;145(6):561–7.
Wahl WL, Ahrns KS, Chen S, et al. Blunt splenic injury: Operation versus angiographic embolization. Surgery. 2004;136(4):891–9.
Tugnoli G, Bianchi E, Biscardi A, et al. Nonoperative management of blunt splenic injury in adults: there is (still) a long way to go. The results of the Bologna-Maggiore Hospital trauma center experience and development of a clinical algorithm. Surg Today. 2015;45(10):1210–7.
Zarzaur BL, Kozar R, Myers JG, et al. The splenic injury outcomes trial. J Trauma Acute Care Surg. 2015;79(3):335–42.
Miller PR, Chang MC, Requarth JA, et al. Prospective Trial of Angiography and Embolization for All Grade III to V Blunt Splenic Injuries: nonoperative management success rate is significantly improved. J Am Coll Surg. 2014;218(4):644–8.
Parihar ML, Kumar A, Gamanagatti S, et al. Role of splenic artery embolization in management of traumatic splenic injuries: a prospective study. Indian J Surg. 2013;75(5):361–7.
Olthof DC, Joosse P, Bossuyt PMM, et al. Observation versus embolization in patients with blunt splenic injury after trauma: a propensity score analysis. World J Surg. 2016;40(5):1264–71.
Barquist ES, Pizano LR, Feuer W, et al. Inter- and intrarater reliability in computed axial tomographic grading of splenic injury: why so many grading scales? J Trauma. 2004;56(2):334–8.
Cohn SM, Arango JI, Myers JG, et al. Computed tomography grading systems poorly predict the need for intervention after spleen and liver injuries. Am Surg. 2009;75(2):133–9.
Omert LA, Salyer D, Dunham CM, Porter J, Silva A, Protetch J. Implications of the “contrast blush” finding on computed tomographic scan of the spleen in trauma. J Trauma. 2001;51(2):272–8.
Thompson BE, Munera F, Cohn SM, MacLean AA, Cameron J, Rivas L, et al. Novel computed tomography scan scoring system predicts the need for intervention after splenic injury. J Trauma. 2006;60(5):1083–6.
Michailidou M, Velmahos GC, van der Wilden G, Alam HB, de Moya M, Chang Y. “Blush” on trauma computed tomography: not as bad as we think! J Trauma Acute Care Surg. 2012;73(3):580–4.
Marmery H, Shanmuganathan K, Alexander MT, Mirvis SE. Optimization of selection for nonoperative management of blunt splenic injury: Comparison of MDCT grading systems. Am J Roentgenol. 2007;189(6):1421–7.
Claridge JA, Carter JW, McCoy AM, Malangoni MA. In-house direct supervision by an attending is associated with differences in the care of patients with a blunt splenic injury. Surgery. 2011;150(4):718–25.
Olthof DC, Sierink JC, van Delden OM, Luitse JSK, Goslings JC. Time to intervention in patients with splenic injury in a Dutch level 1 trauma centre. Injury. 2014;45(1):95–100.
Zarzaur BL, Savage SA, Croce MA, Fabian TC. Trauma center angiography use in high-grade blunt splenic injuries: timing is everything. J Trauma Acute Care Surg. 2014;77(5):666–71.
Bruce PJP, Helmer SD, Harrison PB, Sirico T, Haan JM. Nonsurgical management of blunt splenic injury: Is it cost effective? Am J Surg. 2011;202(6):810–6. doi:10.1016/j.amjsurg.2011.06.041.
Acknowledgements
None.
Funding
None.
Availability of data and materials
All datasets and figures supporting the conclusions of this article are included within the article and its Additional file 1.
Authors’ contributions
FvdC and AM were responsible for the study concept and design. FvdC carried out the literature search. Both authors critically reviewed the manuscript for important intellectual content. AM was the study supervisor. Both authors read and approved the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written consent was obtained from both patients.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table 1.
Search results and number of articles retrieved after applying the selection criteria.After the initial search, all articles were entered in a reference database (Mendeley). Table 2. Summary table of articles that met inclusion criteria after initial selection. Articles marked in grey were excluded. Table 3. Traditionally used American Association for the Surgery of Trauma (AAST) scoring system for splenic injuries. Figure 1. Algorithm for management of splenic trauma modified from Ekeh and Tugnoli.8, 32 Abbreviations: HD: hemodynamically; BP: blood pressure; FAST: Focused Assessment with Sonography for Trauma; ICU: Intensive Care Unit; SAE: splenic artery embolization; MDCT: Multidetector CT grading (Table 4); NOM: non operative management; CE: contrast extravasation; IV: intravenous. (ZIP 126 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Van der Cruyssen, F., Manzelli, A. Splenic artery embolization: technically feasible but not necessarily advantageous. World J Emerg Surg 11, 47 (2016). https://doi.org/10.1186/s13017-016-0100-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13017-016-0100-7