Abstract
Backgrounds
Despite publication of international guidelines, there are notable controversial points of clinical target volume (CTV) delineation in nasopharyngeal carcinoma (NPC). Recently, scholars proposed a novel way of delineation of CTV in NPC—individualization of CTV delineation based on T classification and spread patterns, which yielded excellent long-term local control with limited late toxicities. The aim of this study was to clarify the anatomic patterns and pathways of local recurrence of NPC and provide a clinical reference for the delineation of CTV.
Methods
A total of 869 patients with non-metastatic NPC were treated with intensity-modulated radiation therapy (IMRT) at our institution between 2009 and 2010. Among the 57 cases of local/locoregional recurrence, 52 cases with traceable radiotherapy plans and magnetic resonance imaging at the time of the first diagnosis of recurrence were included. Anatomical structures and gross tumor volume of local recurrence were contoured. The incidence of relapse of each anatomic structure, route of local recurrence, and their correlation were analyzed.
Results
Locally advanced disease had a significantly increased risk of recurrence in the posterior nasal cavity and a trend towards higher risk of recurrence in the clivus, lateral pterygoid muscle, and hypoglossal canal. Based on the incidence of local recurrence, we constructed a high-risk map for the early and locally advanced stages. Local recurrences were classified into five routes, where anterior extension accounted for the majority (30.8%), and caudal tumor extension pathway had the lowest incidence (5.8%). There was a significant correlation between the local recurrences of neural foramina and neighboring anatomical structures along each pathway. All cases relapsed at unilateral cavernous sinus, most at the same side of primary tumor. Based on our findings, we proposed some suggestions on delineations of CTV, based on T classification and local extension pattern.
Conclusions
Local recurrence of NPC varied according to T classification, followed a stepwise pattern, spread via neural foramina, and recurred at ipsilateral cavernous sinus. This provides meaningful clinical evidence for delineation of CTV, especially individualized delineation.
Similar content being viewed by others
Introduction
Radiotherapy is the primary treatment modality for nasopharyngeal carcinoma (NPC). Given the neighboring relationship between the primary tumor and critical normal organs, target delineation in NPC remains a challenge for radiation oncologists. Even in the era of intensity-modulated radiation therapy (IMRT), inadequate coverage of the target volume or inadequate dosimetry remains one of the most important reasons for local failure [1, 2].
The fundamental step is accurate delineation of the gross tumor volume (GTV). Given the application of multimodal radiology techniques, the contouring of GTV has become increasingly consistent. The high-risk clinical target volume (CTV) is generated by the expansion of 8–10 mm of the GTV, with anatomic edition according to different intra-institutional practice, clinical protocols, or regional guidelines [3,4,5,6,7,8]. Adequate delineation of high-risk CTV is important for local control. However, there are still notable differences in the delineation of the CTV between various institutions [9]. The recent publication of international guidelines for delineation of the CTV for NPC [10] has provided a practical reference for radiation oncologists; however, most recommendations were the consensus of experts, which were based on the risk of involvement of primary tumor and traditional bony landmarks of 2-dimensional (2D) radiotherapy. According to the guidelines, there were a few controversial points of delineation, which had reached a low degree of agreement and lacked clinical validation.
There are a few studies on the local extension patterns of primary tumors in NPC [11, 12]. However, to our knowledge, there is a paucity of research focusing on concrete analysis of local recurrences of NPC in the era of IMRT. Most studies classified local relapses as in-field, marginal, or out-of-field failures [13,14,15], yet did not assess the anatomic distributions of local recurrence. We believe that a comprehensive analysis of patterns of local recurrence helps to validate the delineation of CTV and thus provide hints for future modifications. Hence, we collected local recurrence cases in a large consecutive cohort of patients treated by IMRT with long-term follow-up, aiming to perform an in-depth analysis of the local recurrence patterns of NPC.
Methods
Patients
From January 2009 to December 2010, 869 patients with primary non-metastatic, pathologically confirmed NPC were treated with IMRT at Fudan University Shanghai Cancer Center. All patients were re-staged using the 8th edition of the American Joint Committee on Cancer (AJCC) [16]. The details of pretreatment evaluation, treatment, and long-term survival were described in a previous publication [17]. In brief, the 5-year local recurrence-free survival was 89.7% with a median follow-up of 54.3 months [17]. In this study, only patients with solitary local recurrence as well as local and regional recurrence (57 cases) were included. All cases with local recurrence in our study were confirmed by re-biopsy. The primary IMRT plans were recovered. Magnetic resonance imaging (MRI) at the time of the first diagnosis of local/locoregional recurrence was traced and imported into the MIM system (7.1.2; MIM Software, Beachwood, OH). This MRI was fused and aligned with the primary computed tomography (CT) of the IMRT plans. The original IMRT plan or MRI of local recurrence was unavailable in five patients because of failure of recovery of IMRT plans and MRI and diagnosis of local relapse in other hospitals. In total, 52 patients with traceable primary radiotherapy plans and MRI for local recurrence were included in this study. A flow diagram of the enrolled patients is shown in Additional file 1: Fig. A.1. The study protocol was approved by the Institutional Review Board (IRB) of Fudan University Shanghai Cancer Center (2208258-14) according to the principles of the Declaration of Helsinki. The informed consent was waived by the IRB due to the retrospective nature, minimal risk to participants and secondary analysis of previous project. The clinical characteristics of the 52 patients are shown in Additional file 1: Table A.1. The median disease-free interval was 35.3 (range 8.9–60.0) months.
Radiotherapy techniques
Patients were immobilized in the supine position with a thermoplastic mask. CT was performed after immobilization, obtaining 3-mm slices from the calvarium to the hyoid bone and 5-mm slices from the hyoid bone to 2 cm below the sternoclavicular joint. According to the definitions of the ICRU50 and ICRU62 (International Commission on Radiation Units and Measurements), the target volumes were outlined on each layer of the CT images on an IMRT workstation (Pinnacle 3; Philips Healthcare, Best, Netherlands). GTVp included primary tumors and metastatic lymph nodes. The high-risk CTV should cover at least the GTVp with an 8-mm expansion, the entire nasopharynx, parapharyngeal space, at least the anterior two-third of the clivus, the base of the skull, pterygoid fossa, pterygopalatine fossa, inferior sphenoid sinus, and posterior edge of the nasal cavity and maxillary sinuses (at least 5 mm of the posterior part). If the tumor is T3–T4, the entire sphenoid sinus, entire clivus, and bilateral cavernous sinus should be included. The details are outlined in Table 1. The delineation of high-risk CTV of cervical nodes was depicted in our previous publication [18].
A margin of 3–5 mm around the GTV and CTV should be added to account for patient motion and setup error. A smaller margin (at least 1–2 mm and 2–3 mm) will be used for the GTV and CTV, which is adjacent to a critical neurological structure.
Radiation was delivered using a simultaneous integrated boost technique. The total dose to the primary tumor was 66 Gy in 30 fractions for T1 or T2 disease, and 70.4 Gy in 32 fractions for T3 or T4 lesions. The total dose delivered to the metastatic lymph nodes was 66 Gy in 30–32 fractions. High- and low-risk CTV received 60 Gy and 54 Gy in 30–32 fractions, respectively. Inverse IMRT plans were optimized using the Pinnacle treatment planning system. Normal tissue contouring, constraints and plan evaluation were in accordance with the Radiation Therapy Oncology Group 0225 protocol [5].
Contouring anatomic structures and GTVr
Primary MRI was fused with primary CT of the IMRT plan using automated rigid alignment with MIM software. An experienced radiation oncologist contoured normal anatomic structures with the guidance of MRI (Additional file 1: Fig. A.2). The anatomical structures were selected based on the risk assessment of primary tumor extensions, according to the literature [11, 12]. The nomenclature of the anatomic structures is listed in Additional file 1: Table A.2.
Then, MRI of local recurrence was co-registered with primary CT sets of the IMRT plan using automated rigid alignment by MIM software. The delineation of the GTV of the recurrent tumor (GTVr) was first performed with the help of fused recurrent MRI, after which minor manual modification was permitted, considering the anatomic changes between primary CT and recurrent MRI (Additional file 1: Fig. A.2).
Two experienced radiology experts (with more than 15 years of practice) reviewed the contouring of the GTVr and anatomic structures. Any disagreement was resolved by discussion and recontouring.
Analysis of anatomic distribution of local recurrence and pathways
The delineation of the GTVr and anatomic structures were exported from MIM with DICOM format. A python script was used to calculate the overlap volume between anatomic structures and GTVr. Then the overlap data for each patient were exported to R project (version 4.0.5; R Foundation, Vienna, Austria) for statistics analysis. The anatomic structure was marked as local recurrence if a certain percentage of the volume overlapped with the GTVr. To select the appropriate threshold to define local recurrence, we compared the proportion of cases with certain anatomic structures involved under various thresholds of volume overlapped with GTVr. As shown in Additional file 1: Fig. A.3 and Table A.3, the pattern under the threshold of ≥ 1% was consistent with that of ≥ 2–5%, whereas the threshold of > 0% seemed to be much more sensitive than the other thresholds. To balance the sensitivity and specificity, we selected a threshold of ≥ 1%; that is, if ≥ 1% of the volume of a certain anatomic structure overlapped with the GTVr, then this structure was defined as local recurrence in this case.
Sanford et al. [19] summarized the local extension patterns of primary tumor into five common routes. We adopted this classification as the pathway of local recurrence and classified each case into a certain pathway manually if at least two neighboring anatomic structures along this pathway were involved in local recurrence.
Dosimetric analysis
The dose coverage of the entire cohort is presented in Additional file 1: Table A.4. The dosimetric parameters of patients with and without local recurrence are compared in Additional file 1: Table A.5. The dose coverage of T1, T2 was generally better than that of T3,4. However, there were no significant differences in V100, V99, V95,Footnote 1 and D98Footnote 2 of planning tumor volume (PTV) of primary tumor (PTV-G) and V95 and V99 of PTV of high-risk CTV between patients with and without local recurrence in this study.
Statistical analysis
All analyses were performed using R project. The χ2 test or Fisher’s exact test was used to compare categorical variables, and the independent Student’s t-test was used to compare the means of continuous variables. Spearman or Pearson correlation was used to analyze the relationship between the two variables. In all cases, a two-sided p < 0.05 was considered statistically significant.
Results
Risk of local recurrence of various anatomic structures
The cumulative incidence of local recurrence at different anatomical structures varied from 1.9 to 76.9% (Additional file 1: Table A.6). T classification is an important factor that influences the risk of local recurrence. Locally advanced disease (T3–T4) had a significantly higher risk of recurrence at the posterior part of the nasal cavity (52.6% vs. 21.2%, p = 0.020) and showed a trend towards a higher risk of recurrence at the clivus (42.1% vs. 18.2%, p = 0.061), lateral pterygoid muscle (21.1% vs. 3.0%, p = 0.054), and hypoglossal canal (21.1% vs. 3.0%, p = 0.054).
According to the cumulative incidence or local recurrence, we classified anatomical structures into three risk grades: high risk (≥ 30%), median risk (≥ 15–30%), and low risk (< 15%), as shown in Table 2. In locally advanced cases (T3–T4), these anatomical structures had a median risk of local recurrence and were recommended being covered by CTV, including the posterior ethmoid sinus (21.1%), lateral pterygoid muscle (21.1%), hypoglossal canal (21.1%), inferior orbital fissure (15.8%), and cavernous sinus (15.8%).
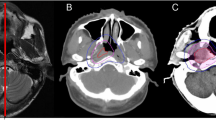
However, in early-stage disease (T1–T2), these structures may not be routinely included in the delineation of the CTV, given the low risk of local recurrence: posterior ethmoid sinus (9.1%), inferior orbital fissure (9.1%), lateral pterygoid muscle (3.0%), hypoglossal canal (3.0%), and cavernous sinus (3.0%). Based on the differences in local recurrence risk, our team generated high-risk maps of local recurrence for early-stage and locally advanced cases using a python script (Fig. 1).
Recommended clinical target volume according to the percentage of local recurrence in cases of early and locally advanced stage of nasopharyngeal carcinoma. A–H Demonstrated the risk of local recurrence of each anatomic structure and recommended delineation of clinical target volume (CTV) in T1–T2 case with nasopharyngeal carcinoma, at the level of cranial border of C2, midpoint of C1, hard palate, midpoint of maxillary sinus, foramen lacerum, great wing of sphenoid bone, inferior orbital fissure and midpoint of orbit. I–P Demonstrated the risk of local recurrence of each anatomic structure and recommended delineation of clinical target volume (CTV) in T3–T4 case with nasopharyngeal carcinoma, at the level of cranial border of C2, midpoint of C1, hard palate, midpoint of maxillary sinus, foramen lacerum, great wing of sphenoid bone, inferior orbital fissure and midpoint of orbit. The color bar showed the risk of local recurrence. The pink and red line showed the iso-risk line of 15% and 30% of local recurrence. In our study, the iso-risk line of 15% was selected as the recommended contouring of CTV. It was noteworthy that lateral pterygoid muscle, posterior ethmoid sinus, inferior orbital fissure and cavernous sinus were not included in the delineation of CTV in early-stage disease, but were encompassed by CTV in locally advanced disease
Pathways of local recurrence
We classified each case of local relapse into five routes (Table 3; Fig. 2) according to the suggestion by Sanford et al. [19]. Cases with local recurrence at the nasopharynx and retropharyngeal lymph nodes were classified as in situ relapse, which was not included in the pathway analysis. Except in situ relapse, all the remaining cases of recurrence fell into the five routes mentioned above.
The stepwise pattern and pathways of local recurrence of nasopharyngeal carcinoma. The incidence of recurrence of each anatomic site was listed in the schema. It was noteworthy that most of the recurrence of nasopharyngeal carcinoma followed a stepwise, orderly pattern, with decreased incidence of relapse as the distance from nasopharynx increased. Of note, the cases of in-situ recurrence were excluded from analysis. LVPM, Levator veli palatine muscle; TVPM, Tensor veli palatine muscle
The most common route of local recurrence was anterior tumor extension (30.8%), in which local relapse mainly occurred through the pterygopalatine fossa. The caudal tumor extension pathway had the lowest incidence of local relapse (5.8%).
Within each pathway, there was a significant correlation between the neural foramina and other anatomic structures (Spearman correlation test, p < 0.05, Table 4), and the incidence of recurrence gradually decreased as the distance from the nasopharynx increased (Fig. 2). This indicated that recurrent tumors are likely to spread through neural foramina in a stepwise fashion.
In addition, we evaluated the correlation between neighboring structures and anatomic structures with notably different risks of relapse among various T classifications (Table 4). For example, invasion of the inferior orbital fissure was associated with recurrence in the posterior nasal cavity, pterygoid process, pterygopalatine fossa, foramen rotundum, and cavernous sinus. Relapse of the hypoglossal canal was associated with the clivus and jugular foramen. In addition, there were significant correlations between relapse in posterior ethmoid sinus and posterior nasal cavity/ sphenoid sinus, relapse in lateral pterygoid muscle and medial pterygoid muscle. This indicated that certain anatomic structure should be included by CTV in case of the involvement of neighboring structures.
The unilateral recurrence of cavernous sinus
There were four cases with recurrence of cavernous sinus (Table 5). All four cases relapsed at unilateral cavernous sinus. Among them, three cases were primarily diagnosed as locally advanced disease, and recurred at the same side of the primary tumor. One case had primary T1 disease involving bilateral roof of nasopharynx, however, developed extensive recurrence to cavernous sinus.
Suggestions on delineations of clinical target volumes
As mentioned above, we have depicted high risk maps of local recurrence of various T classifications, evaluated the correlations of local recurrence between key anatomic structure and neighboring structures, and clarified the recurrence pattern at cavernous sinus. Based on current findings, we propose some suggestions on delineation of CTV, which are summarized in Table 1.
For T1–T2 disease, we suggest including medial pterygoid muscle in CTV laterally, given the median risk of local relapse (18.2%) at this structure. Our data demonstrated the low risk of recurrence at posterior ethmoid sinus, so we suggest encompassing the vomer and surrounding ethmoid sinus in CTV to ensure coverage of superior border of nasopharynx, per recommendation of international guideline [10]. Our data showed that the risk of local recurrence at hypoglossal canal in T1–T2 cases was low (3.0%), and the risk of recurrence of this structure correlated with that of clivus and jugular foramen. In addition, the risk of recurrence of jugular foramen correlated with that of levator veli palatine muscle, retropharyngeal nodes and parapharyngeal space. Hence, we recommend sparing the jugular foramen and hypoglossal canal unless there is extensive posterior-lateral infiltration of primary tumor or high jugular lymphadenopathy. We recommend sparing cavernous sinus by CTV in early-stage disease, due to the low incidence of relapse in cavernous sinus.
In T3–T4 disease, local recurrence risk of lateral pterygoid muscle was demonstrated to be marginally higher, and this was significantly associated with invasion of medial pterygoid muscle. Hence, we suggest including lateral pterygoid muscle in CTV in case of the involvement of medial pterygoid muscle in locally advanced disease. Similarly, we advocate including posterior part of ethmoid sinus in case of invasion of posterior nasal cavity or sphenoid sinus, and recommend coverage of inferior orbital fissure in case of involvement of pterygopalatine fossa, given the high risk of local relapse of these anatomic structures and their close relationships in locally advanced cases. Considering the unilateral recurrence of cavernous sinus and the median risk of relapse in T3–T4 disease, we recommend coverage of cavernous sinus of the involved side by CTV.
Of note, these were merely suggestions derived from retrospective data of our institutional practice. The further interpretation of these suggestions should be based on full consideration of individual patient’s factors and the experience of individual center.
Discussion
The current recommendations of delineation of CTV are generally based on the understanding of the natural behavior of tumor invasion, the experience of 2D/3D radiotherapy, as well as the patterns of local recurrence in the era of IMRT. In this study, we collected local recurrence cases in a large consecutive cohort of patients with uniform intra-institutional protocol and a long-term follow-up, which is one of the few attempts to perform an in-depth analysis of the local recurrence patterns of NPC and provided validations for delineation of CTV.
When IMRT was introduced into the treatment of NPC in early 2000s, the delineation of CTV was universal, irrespective of T classification [5, 7]. Gradually, scholars began to modify the delineation according to T classification. For example, cavernous sinus was included merely in cases of T3–T4 disease, as mentioned in the protocol of RTOG 0615 [20]. Similarly, our study demonstrated that the recurrence risk of anatomic sites varied between various T subgroups. Lateral pterygoid muscle and hypoglossal canal, tended to have a higher incidence of relapse in T3–T4 disease than in T1–T2. The risk of recurrence of cavernous sinus was numerically higher in locally advanced disease, albeit did not reach statistical significance (T3–T4 15.8% vs. T1–T2 3.0%).
In addition, our data showed that certain anatomic structure were exposed to a high risk of local recurrence in case of the involvement of neighboring structures. For example, relapse in the jugular foramen correlated with the levator veli palatini muscle, retropharyngeal node, and parapharyngeal space. Recurrence in the hypoglossal canal was associated with the clivus and jugular foramen. Both supported the practice to cover jugular foramen and hypoglossal canal in case of postero-lateral extension of primary tumor and retropharyngeal lymph nodes, which was consistent with the recommendations of international guidelines of delineation of CTV [10]. Likewise, we propose covering the posterior ethmoid sinus in T3–T4 cases, especially in cases of invasion into the posterior nasal cavity and sphenoid sinus. We suggest encompassing the inferior orbital fissure when primary tumor involved the pterygopalatine fossa and foramen rotundum. Of note, the criteria to cover inferior orbital fissure has not been discussed in the international guidelines before [10].
As for cavernous sinus, Liang et al. [11] reported the risk of bilateral invasion of cavernous sinus was low (1.5%). Sanford et al. [19] advocated covering the Meckel’s cave and cavernous sinus ipsilaterally for lateralized tumors. Wu et al. [21] recently characterized the locoregional extension patterns of unilateral NPC and demonstrated that contralateral skull base was not invaded in this case. In accordance with these, our study showed all cases relapsed at unilateral cavernous sinus, most cases at the same side of the primary tumor. The risk of recurrence of cavernous sinus was higher in locally advanced disease. This supported the recommendations of international guidelines—to spare the cavernous sinus in T1–T2 disease and cover the whole ipsilateral cavernous sinus in T3–T4 disease [10].
Furthermore, our study showed that local recurrence followed similar routes with primary invasions. Sanford et al. [19] summarized local invasions routes into five pathways. Our study showed all local recurrence except in situ relapse could be classified into these five pathways as well. Among five routes, anterior tumor extension (30.8%) accounted for the majority, in which local relapse mainly occurred through the pterygopalatine fossa. This may be partially attributed to the extensive communications of pterygopalatine fossa with various cranial nerves and anatomic structures.
Recently, scholars proposed a novel way of delineation of CTV in NPC—individualization of CTV delineation based on stepwise spread patterns. Li et al. [22] and Sanford et al. [19] adopted different individualized delineations based on T classification and spread patterns, both attained excellent long-termed local control and low late toxicities. **e et al. [23] reported individualized CTV delineation in unilateral NPC yielded excellent long-term local control with limited out-of-field recurrences. In this cohort, unilateral NPC was defined as a nasopharyngeal mass confined to one side of the nasopharynx and did not exceed the midline [23]. The CTVs were determined based on the distance from the gross tumor, and the contralateral para-pharyngeal space and skull base orifices were spared from irradiation [23]. Our study proved that local recurrence differed among various primary T classifications, followed a stepwise pattern, and shared similar routes with primary invasion, which supported the rationale of individualization of CTV delineation based on T classification and spread patterns. Taken together, individualized CTV delineation is a promising treatment de-escalation strategy that maintains local control and meanwhile spares unnecessary irradiation, which deserves further optimization and validation by prospective clinical studies.
Conclusions
Collectively, our study demonstrated that local recurrence of NPC varied according to T classification, followed a stepwise pattern, shared similar routes with primary invasions, and usually recurred at ipsilateral cavernous sinus. Despite the retrospective and single-institutional analysis, our study provides a meaningful clinical reference for delineation of high-risk CTV in NPC and supports the rationale of individualized delineation based on T classification and spread patterns. Given the limitations of sample size and retrospective nature, our findings should be further evaluated using external data or prospective clinical studies.
Availability of data materials
The data in our study have been deposited on the Mendeley Data (data.mendeley.com). After publication of the study findings, our data are available from the corresponding author and database administrator on reasonable request.
Notes
V95: volume of PTV that received at least 95% of the prescription dose.
D98: dose received by 98% of PTV.
Abbreviations
- NPC:
-
Nasopharyngeal carcinoma
- GTV:
-
Gross tumor volume
- CTV:
-
Clinical tumor volume
- IMRT:
-
Intensity-modulated radiation therapy
- 2D:
-
2-Dimensional
- 3D:
-
3-Dimensional
- AJCC:
-
American Joint Committee of Cancer
- ICRU:
-
International Commission on Radiation Units and Measurements
- GTVp:
-
Gross tumor volume of primary tumor
- GTVr:
-
Gross tumor volume of local recurrence
- PTV:
-
Planning tumor volume
- PTV-G:
-
Planning tumor volume of primary tumor
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- IRB:
-
Institutional Review Board
References
Ng WT, Lee MC, Chang AT, Chan OS, Chan LL, Cheung FY, et al. The impact of dosimetric inadequacy on treatment outcome of nasopharyngeal carcinoma with IMRT. Oral Oncol. 2014;50(5):506–12. https://doi.org/10.1016/j.oraloncology.2014.01.017.
Wang J, Qing G, Ou X, Hu W, Hu C, Zhang Z. The impact of target dosimetry on patients’ locoregional recurrence in nasopharyngeal carcinoma: a propensity score-matched analysis. Radiother Oncol. 2019;141:67–71. https://doi.org/10.1016/j.radonc.2019.09.001.
Lee N, **a P, Quivey JM, Sultanem K, Poon I, Akazawa C, et al. Intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys. 2002;53(1):12–22. https://doi.org/10.1016/s0360-3016(02)02724-4.
Ng WT, Lee MC, Hung WM, Choi CW, Lee KC, Chan OS, et al. Clinical outcomes and patterns of failure after intensity-modulated radiotherapy for nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2011;79(2):420–8. https://doi.org/10.1016/j.ijrobp.2009.11.024.
Lee N, Harris J, Garden AS, Straube W, Glisson B, **a P, et al. Intensity-modulated radiation therapy with or without chemotherapy for nasopharyngeal carcinoma: radiation therapy oncology group phase II trial 0225. J Clin Oncol. 2009;27(22):3684–90. https://doi.org/10.1200/JCO.2008.19.9109.
NRG-HN001: Randomized phase II and phase III studies of individualized treatment for nasopharyngeal carcinoma based on biomarker Epstein Barr Virus (EBV) Deoxyribonucleic Acid (DNA). https://www.nrgoncology.org/Clinical-Trials/Protocol/nrg-hn001?filter=nrg-hn001. Published April 21, 2014. Updated June 28, 2021. Accessed May 11, 2022.
The Chinese Committee of staging modification of nasopharyngeal carcinoma. 2010 Nasopharyngeal carcinoma intensity-modulated radiotherapy target and dose design guidelines: expert consensus. Chin J Radiat Oncol 2011;20:267–9 (in Chinese). https://doi.org/10.3760/cma.j.issn.1004-4221.2011.04.001.
Lin S, Pan J, Han L, Zhang X, Liao X, Lu JJ. Nasopharyngeal carcinoma treated with reduced-volume intensity-modulated radiation therapy: report on the 3-year outcome of a prospective series. Int J Radiat Oncol Biol Phys. 2009;75(4):1071–8. https://doi.org/10.1016/j.ijrobp.2008.12.015.
Zhang S, Yang S, Xu P, Xu Y, Zhou G, Ou X, et al. Variations of clinical target volume delineation for primary site of nasopharyngeal cancer among five centers in China. Front Oncol. 2020;10:1572. https://doi.org/10.3389/fonc.2020.01572.
Lee AW, Ng WT, Pan JJ, Poh SS, Ahn YC, AlHussain H, et al. International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiother Oncol. 2018;126(1):25–36. https://doi.org/10.1016/j.radonc.2017.10.032.
Liang SB, Sun Y, Liu LZ, Chen Y, Chen L, Mao YP, et al. Extension of local disease in nasopharyngeal carcinoma detected by magnetic resonance imaging: improvement of clinical target volume delineation. Int J Radiat Oncol Biol Phys. 2009;75(3):742–50. https://doi.org/10.1016/j.ijrobp.2008.11.053.
Li WF, Sun Y, Chen M, Tang LL, Liu LZ, Mao YP, et al. Locoregional extension patterns of nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Chin J Cancer. 2012;31(12):579–87. https://doi.org/10.5732/cjc.012.10095.
Cao C, Jiang F, ** Q, ** T, Huang S, Hu Q, et al. Locoregional extension and patterns of failure for nasopharyngeal carcinoma with intracranial extension. Oral Oncol. 2018;79:27–32. https://doi.org/10.1016/j.oraloncology.2018.02.004.
Li JX, Huang SM, Jiang XH, Ouyang B, Han F, Liu S, Wen BX, Lu TX. Local failure patterns for patients with nasopharyngeal carcinoma after intensity-modulated radiotherapy. Radiat Oncol. 2014;9:87. https://doi.org/10.1186/1748-717X-9-87.
Kong F, Ying H, Du C, Huang S, Zhou J, Chen J, et al. Patterns of local-regional failure after primary intensity modulated radiotherapy for nasopharyngeal carcinoma. Radiat Oncol. 2014;9:60. https://doi.org/10.1186/1748-717X-9-60.
Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. 8th ed. New York: Springer; 2017.
Ou X, Zhou X, Shi Q, **ng X, Yang Y, Xu T, et al. Treatment outcomes and late toxicities of 869 patients with nasopharyngeal carcinoma treated with definitive intensity modulated radiation therapy: new insight into the value of total dose of cisplatin and radiation boost. Oncotarget. 2015;6(35):38381–97. https://doi.org/10.18632/oncotarget.5420.
Ou XM, Miao YB, Wang XS, Ding JH, He XY, Hu CS. The feasibility analysis of omission of elective irradiation to level IB lymph nodes in low-risk nasopharyngeal carcinoma based on the 2013 updated consensus guideline for neck nodal levels. Radiat Oncol. 2017;12:137. https://doi.org/10.1186/s13014-017-0869-x.
Sanford NN, Lau J, Lam MB, Juliano AF, Adams JA, Goldberg SI, et al. Individualization of clinical target volume delineation based on stepwise spread of nasopharyngeal carcinoma: outcome of more than a decade of clinical experience. Int J Radiat Oncol Biol Phys. 2019;103(3):654–68. https://doi.org/10.1016/j.ijrobp.2018.10.006.
Lee NY, Zhang Q, Pfister DG, Kim J, Garden AS, Mechalakos J, et al. Addition of bevacizumab to standard chemoradiation for locoregionally advanced nasopharyngeal carcinoma (RTOG 0615): a phase 2 multi-institutional trial. Lancet Oncol. 2012;13(2):172–80. https://doi.org/10.1016/S1470-2045(11)70303-5.
Wu Z, Zhang L, He Q, Li F, Ma H, Zhou Y, et al. Characteristics of locoregional extension of unilateral nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Radiat Oncol. 2022;17(1):52. https://doi.org/10.1186/s13014-022-02017-2.
Lin L, Yao JJ, Zhou GQ, Guo R, Zhang F, Zhang Y, et al. The efficacy and toxicity of individualized intensity-modulated radiotherapy based on the tumor extension patterns of nasopharyngeal carcinoma. Oncotarget. 2016;7(15):20680–90. https://doi.org/10.18632/oncotarget.8004.
**e DH, Wu Z, Li WZ, Cheng WQ, Tao YL, Wang L, et al. Individualized clinical target volume delineation and efficacy analysis in unilateral nasopharyngeal carcinoma treated with intensity-modulated radiotherapy (IMRT): 10-year summary. J Cancer Res Clin Oncol. 2022;148(8):1931–42. https://doi.org/10.1007/s00432-022-03974-7.
Acknowledgements
We acknowledge the support of the Department of Radiation Oncology, Fudan University Shanghai Cancer Center. The views expressed in this publication are those of the authors.
Funding
This project was supported by the National Natural Science Foundation of China (Grant No. 81602372), the CSCO-Young Research Fund of Chinese Society of Clinical Oncology (Grant No. Y-Young2021-0127) and the Key Clinical Specialty Project of Shanghai. The funders had no role in the study design, data collection and analysis, the interpretation of the results, the preparation of the manuscript, or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Study concept: XO, JW, CH. Study design: XO, WY. Data acquisition: XO, YH, BW, HZ. Quality control of data and algorithms: XO, JW. Data analysis and interpretations: XO, WY. Statistic analysis: XO, JW. Manuscript preparations: XO, WY. Manuscript editing: XO, WY. Manuscript review: JW, CH, XH, HY, XL. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Institutional Review Board (IRB) of Fudan University Shanghai Cancer Center (2208258-14) according to the principles of the Declaration of Helsinki. The informed consent was waived by the IRB due to the retrospective nature, minimal risk to participants and secondary analysis of previous project.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Tables and Figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ou, X., Yan, W., Huang, Y. et al. Unraveling the patterns and pathways of local recurrence of nasopharyngeal carcinoma: evidence for individualized clinical target volume delineation. Radiat Oncol 18, 55 (2023). https://doi.org/10.1186/s13014-023-02199-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-023-02199-3