Abstract
Background
To retrospectively analyze the efficacy and safety of concurrent chemoradiotherapy (CCRT) plus recombinant human endostatin (Endostar, CCRT + E) versus CCRT alone in locally advanced nasopharyngeal carcinoma (LANPC).
Methods
A retrospective analysis of patients initially treated for LANPC from November 2016 to March 2019 was performed: trial group received CCRT + E and control group received CCRT. Prognoses and adverse effects were evaluated.
Results
Eighty-eight patients were included: 43 received CCRT + E and 45 received CCRT. The median follow-up time was 54.0 (range: 8.0–64.0) months. The survival data of the CCRT + E and CCRT groups were as follows: 3-year progression-free survival (PFS) rates, 81.4% and 63.6% (hazard ratio [HR] 0.418, 95%CI 0.181–0.963, P = 0.034); 3-year distant metastasis-free survival (DMFS) rates, 88.3% and 77.3% (HR 0.370, 95%CI 0.132–1.039, P = 0.049); 3-year overall survival rates, 88.2% and 81.9% (HR 0.437, 95%CI 0.151–1.260, P = 0.114); and 3-year locoregional failure-free survival rates, 87.8% and 86.9% (HR 0.795, 95%CI 0.242–2.616, P = 0.705). Three months after radiotherapy, the complete response (CR) rates of cervical lymph node regression were 97.7% and 82.2% for the CCRT + E and CCRT groups (P = 0.041). The corresponding CR rates were 100% and 80.0% for lymph node necrosis (P = 0.001) and 100% and 85.2% for extranodal extension (P = 0.041). The CCRT + E group had higher incidence of grade 3/4 leukopenia (32.6% vs. 13.3%, P = 0.031), with similar results for late toxicity.
Conclusions
CCRT + E significantly prolonged 3-year PFS and DMFS in LANPC, and patients had better lymph node regression.
Similar content being viewed by others
Introduction
Cases of nasopharyngeal carcinoma (NPC) are reported throughout Southeast Asia and are common in China's Guangxi and Guangdong provinces. The annual incidence of NPC in Guangxi is 10–30 per 100,000 people, with an increased mortality rate [1, 2]. The wide use of intensity-modulated radiation therapy (IMRT) has led to an effective improvement in survival rates of patients with NPC compared with previous two-dimensional radiotherapies, with 5-year overall survival rates reaching 86.6–93.2% in stages I–II and 63.2–80.5% in stages III–IVB [3]. Currently, concurrent chemoradiotherapy (CCRT) is the standard of care for locally advanced nasopharyngeal carcinoma (LANPC), but distant metastases remain a significant cause of treatment failure [3,4,5]. Therefore, new therapies are needed to lower the distant metastatic rate and improve treatment efficacy in sufferers with LANPC.
Endostar, a recombinant human vascular endothelial inhibitor, is a multi-targeted tumor cell inhibitor developed in China [6]. Endostar directly inhibits vascular endothelial cell multiplication and suppresses tumor development through multiple targets, including vascular endothelial growth factor (VEGF), VEGF receptor-2 (VEGFR-2), and platelet-derived growth factor receptor [7]. It can also normalize tumor blood vessels and exert antitumor effects [7, Concurrent chemoradiotherapy In both groups, the target area and dose design of IMRT for NPC, according to reports 50 and 62 of the International Radiation Unit and Measurement Organization (ICRU) and the expert consensus of the Radiation Treatment Oncology Organization (RTOG) 0225. GTVnx includes primary NPC foci and enlarged retropharyngeal lymph nodes, whereas GTVnd includes imaging and palpation findings of enlarged cervical lymph nodes. The high-risk clinical target volume (CTV1) was a 5–10 mm outward expansion of the GTVnx (or 1–3 mm if close to the brainstem or spinal cord) to cover the submicroscopic increase in the high-risk site and entire nasopharynx. The low-risk clinical target volume (CTV2) was a 5–10 mm outward expansion of CTV1 to include the skull base, alveolus, cavernous sinus, parapharyngeal space, pterygopalatine fossa, posterior nasal cavity, and the lymph node drainage area in the neck. For the planned target regions derived from GTVnx, GTVnd, CTV1, and CTV2, the administered doses were 70–72, 64–72, 62–64, and 54–56 Gy, respectively, 30–33 f, five times a week for 6–7 weeks; concurrent chemotherapy regimens included cisplatin (80 mg/m2), nedaplatin (80 mg/m2), and docetaxel plus cisplatin (DOC 75 mg/m2, DDP 80 mg/m2). A cycle included 21 days. After the completion of radiotherapy, assessments were performed every 3 months for 1–3 years, every 6 months for 4–5 years, and annually thereafter. The review included head and neck enhanced MRI or enhanced CT (for patients for whom MRI was prohibited), chest CT, liver imaging (abdominal ultrasound or CT), bone imaging, nasopharyngoscopy, and laboratory examination. PET/CT was optional. Efficacy was evaluated according to solid tumor version 1.1 (RECIST1.1), and efficacy indicators included complete response (CR), partial response, stable disease, and progressive disease. Toxic reactions were evaluated according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE v4.0). Statistical analyses were performed using SPSS Statistics (version 25.0; IBM Corp., Armonk, NY, USA) and GraphPad Prism 6.0. P < 0.05 was considered statistically significant. The χ2 test or Fisher's exact test was used to detect qualitative variables and adverse effects, and differences in continuous variables were assessed using the Mann–Whitney U test. Survival curves were analyzed using the Kaplan–Meier method. The hazard ratios (HRs) were analyzed using the Cox proportional hazard model.Follow-up
Statistical analysis
Results
Patient characteristics
Our study included 88 patients with initially treated LANPC, of whom 61 (69.3%) were men. The mean age of patients in both groups was 44.2 years (range: 24–66). The number of patients with clinical stages III, IVa, and IVb was 31, 46, and 11, respectively. The number of patients with lymph node stages of N1, N2, and N3 was 45, 26, and 11, respectively. The sex, tumor (T) stage, clinical stage, lymph node (N) stage, and age were similar in the two groups (P > 0.05) (Table 1).
During concurrent chemoradiotherapy, all 43 (100%) patients in the CCRT + E group completed three processes of Endostar. After radiotherapy, 37 (86.0%) patients received two cycles of Endostar, and four (9.3%) received one cycle of Endostar. Two (4.7%) patients did not continue Endostar maintenance treatment. All 43 (100%) patients received ≥ 2 cycles of concurrent chemotherapy, of whom 40 (93.0%) were on single-agent cisplatin regimens, and three (7.0%) received both single-agent cisplatin and single-agent nedaplatin regimens. In the CCRT group, 43 patients (95.6%) received ≥ 2 cycles of chemotherapy and two (4.4%) received one cycle. Of them, 39 (86.7%) patients were treated with cisplatin alone, one (2.2%) received only docetaxel plus cisplatin, and four (8.9%) received both single-agent cisplatin and docetaxel plus cisplatin, and one (2.2%) received all three regimens. Cisplatin dose was reduced in four CCRT + E and three CCRT patients due to hematological toxicity reactions and gastrointestinal reactions, respectively. In the CCRT + E group, one patient was suspended from radiotherapy for 12 days due to infectious shock, and the dose of radiotherapy was increased to GTVnx 77 Gy/35 f. The remaining patients completed the radiotherapy program according to the original protocol.
Tumour response and survival analysis
Three months after radiotherapy, the CR rates of nasopharyngeal lesions were 53.5% (23/43) and 60.0% (27/45) in the CCRT + E and CCRT groups, respectively. The recent outcomes of nasopharyngeal lesions were similar in both groups (P = 0.538) (Table 2).
The lymph node CR rates were 97.7% (42/43) and 82.2% (37/45) in the CCRT + E and CCRT groups, respectively (P = 0.041) (Table 2), and the result suggested that patients in the CCRT + E group had better overall lymph node regression than the CCRT group. There were 104 and 113 measurable regional lymph nodes in the two groups, respectively. The CR rates of retropharyngeal lymph nodes in patients in the CCRT + E and CCRT groups were 95.5% (42/44) and 84.4% (38/45), respectively (P = 0.170). The CR rates of lymph node necrosis were 100% (47/47) and 80.0% (40/50), respectively (P = 0.001). The CR rates of extranodal extension of the lymph nodes were 100% (31/31) and 85.2% (23/27), respectively (P = 0.041). Lymph node necrosis and extranodal extension of the lymph nodes were associated with better outcomes in the CCRT + E group. The CR rates of lymph nodes in the CCRT + E and CCRT groups were 97.8% (89/91) and 88.9% (88/99) in the subgroup of lymph nodes with the shortest diameter ≤ 3 cm, respectively (P = 0.015), and 100% (13/13) versus 71.4% (10/14) in the subgroup of lymph nodes with the shortest diameter > 3 cm, respectively (P = 0.098) (Table 3).
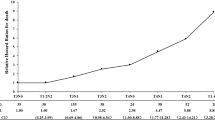
There were 88 patients in both groups, with a median follow-up time of 54.0 (range: 8.0–64.0) months. There were five (11.6%) deaths in the CCRT + E group and 10 (22.2%) in the CCRT group (Table 4), all of which were nasopharyngeal cancer-related deaths. In the CCRT + E group, five (11.6%) patients had distant metastases: four in the lungs, two in the liver, and four in the bone. Four of these patients presented with ≥ 2 organ metastases. Thirteen (28.9%) patients in the CCRT group had distant metastases: six cases of lung metastasis, three of liver metastasis, seven of bone metastasis, and two of other sites. Six of these patients presented with ≥ 2 organ metastases (Table 4). Locoregional recurrence occurred in five (11.6%) patients in the CCRT + E group and six (13.3%) patients in the CCRT group (Table 4). The 3-year overall survival (OS), progression-free survival (PFS), distant metastasis-free survival (DMFS), and locoregional failure-free survival (LRFFS) in CCRT + E and CCRT were 88.2% versus 81.9% (hazard ratio [HR] 0.437, 95% CI 0.151–1.260; log-rank P = 0.114), 81.4% versus 63.6% (HR 0.418, 95% CI 0.181–0.963; log-rank P = 0.034), 88.3% versus 77.3% (HR 0.370, 95% CI 0.132–1.039; log-rank P = 0.049), and 87.8% versus 86.9% (HR 0.795, 95%CI 0.242–2.616; log-rank P = 0.705), respectively (Fig. 1).
Cumulative survival curves after treatment with concurrent chemoradiotherapy plus Endostar compared with concurrent chemoradiotherapy. a Overall survival; b Progression-free survival; c Distant metastasis-free survival; d Locoregional failure -free survival. HR, hazard ratio; CI, confidence interval
Adverse effects
Acute adverse events during treatment in the CCRT + E and CCRT groups are shown in Table 5. Grade 3 or 4 adverse reactions were mainly focused on leukopenia, thrombocytopenia, decreased hemoglobin, nausea, vomiting, dry mouth, oral mucositis, and radiation dermatitis. The incidence of grade 3 or 4 leukopenia was significantly higher in the CCRT + E group (14/43, 32.6%) than in the CCRT group (6/45, 13.3%) (P = 0.031), which improved after symptomatic treatment without treatment interruption or cessation. The incidence of other grade 3 or 4 adverse reactions was similar in both groups (P > 0.05). The negative effects of grade 1 or 2 in both groups were leukopenia, decreased hemoglobin, weight loss, nausea, vomiting, dry mouth, oral mucositis, liver dysfunction, renal dysfunction, and skin reactions; these events were not significantly different between the groups (P > 0.05).
None of the grade 3 or 4 late toxic reactions occurred in the CCRT + E group. In the CCRT group, two patients had grade 3 hearing impairment; however, no grade 4 adverse reactions occurred. Limitation of mouth opening, decreased vision, hearing loss, temporal lobe damage, subcutaneous fibrosis, cranial nerve palsy, and dry mouth were the major adverse effects of grade 1 or 2, with similar incidence in both groups (P > 0.05) (Table 6).
Discussion
This retrospective study showed that CCRT + E is effective in reducing the rate of distant metastases and promoting lymph node regression in patients with LANPC. Specifically, CCRT + E significantly improved 3-year DMFS and PFS in patients with LANPC and improved CR rates in cervical lymph nodes, including lymph node necrosis and extranodal extension.
Currently, distant metastasis remains the leading cause of treatment failure in NPC [3,4,5, 16], and a similar result was found in this study, with 17% of patients experiencing distant metastasis at 3 years. This result implies that reducing the rate of distant metastasis is the key to improving the outcome of NPC. Previous studies have shown that blood and lymphatic vessels influence the oncogenesis, development, and metastasis of neoplasms, indicating that inhibiting the production of tumor blood and lymphatic vessels can impede the development and metastasis of neoplasms [17, 18]. VEGF is a tumor-inducing factor that contributes to angiogenesis [19, 20] and is an adverse prognostic factor in patients with NPC [21, 22]. Endostar restrains tumor development and lymph node metastasis by suppressing VEGF expression, inhibiting tumor vascular and lymphatic vessel production, and reducing the entry of tumor cells into circulation [7]. As confirmed in this study, CCRT + E significantly improved 3-year DMFS and PFS in patients with LANPC. In the study by Li et al. [15], the CR rates of cervical lymph nodes in the CCRT + E and CCRT groups were 91.1% and 71.4%, respectively, with a significant difference (P = 0.048), consistent with the result of the present study (97.7% vs. 82.2%, P = 0.041).
The 3-year PFS of patients in the CCRT group in this study was 63.6%, and 3-year DMFS was 77.3%, which was similar to the results of previous studies [23, 24]. In a phase II clinical study by Fountzilas et al. [23], the 3-year PFS rate in LANPC patients receiving CCRT was 63.5%. A phase II–III randomized clinical study by Tan et al. [24] reported 3-year DFS and DMFS rates of 67.4% and 79.9%, respectively. In a study by Li et al. [25] in which sequential Endostar plus induction chemotherapy and concurrent chemoradiotherapy were compared with sequential induction chemotherapy and concurrent chemoradiotherapy for LANPC, the 2-year OS, PFS, and DMFS rates in the trial group were 82.3%, 77.2%, and 82.2%, respectively. Here, the 3-year OS, PFS, and DMFS (88.2%, 81.4%, and 88.3%, respectively) were higher than the 2-year survival rates reported by Li et al. [25], wherein the trial group received only one cycle of Endostar in concurrent chemoradiotherapy. In contrast, in this study, the trial group (of 43 patients) received three cycles of Endostar during concurrent chemoradiotherapy—this could explain the observed differences in survival. It has been shown that Endostar is effective in inducing vascular normalization 5–7 days after administration, and when administered in combination, two consecutive cycles of treatment are required to assess efficacy [26,27,28]. Endostar increases radiotherapy sensitivity [12, 29], and increasing the dosing cycle of Endostar during concurrent chemoradiotherapy improves radiotherapy sensitivity and thus its efficacy.
Approximately 85% of patients initially diagnosed with nasopharyngeal carcinoma have cervical lymph node metastases [30]. Cervical lymph node metastases are closely related to patient survival prognosis, and lymph node necrosis and extranodal extension are independent prognostic factors of NPC [31,32,33]. Hence, improving lymph node outcomes is crucial. The results of this study showed that 3 months after radiotherapy, the CCRT + E group had better outcomes for lymph node necrosis (P = 0.001), lymph nodes of extranodal extension (P = 0.041), and lymph nodes with the shortest diameter ≤ 3 cm (P = 0.015). The reason for the enhanced therapeutic effect of the CCRT + E regimen could be that Endostar inhibits the production of tumor blood vessels and lymphatic vessels and induces the normalization of tumor blood vessels, thereby improving tumor cell hypoxia and enhancing the radiosensitivity of hypoxic cells. The CR rate of lymph nodes with the shortest diameters of > 3 cm was significantly better in the CCRT + E group than that in the CCRT group (100% vs. 71.4%). Nevertheless, the difference was not statistically significant (P = 0.098), possibly because the sample size of this study was limited. Therefore, a study with a larger sample is needed to further clarify the efficacy of CCRT + E on lymph nodes with the shortest diameters > 3 cm.
The incidence of grade 3 or 4 leukopenia in CCRT + E is highly variable across studies, ranging from 5.3 to 44.8% [15, 34,35,36], which may be related to different chemotherapy regimens and cycles, Endostar cycles, and radiotherapy doses. In this study, the incidence of grade 3/4 leukopenia in the CCRT + E group was 32.6%, but all patients recovered with symptomatic management, and no patient interrupted or discontinued treatment, and no patient died of acute toxic events. The late toxic reactions were similar in both groups (P > 0.05), indicating that CCRT + E was safe and feasible for the treatment of LANPC.
Our study had some limitations. This study was retrospective in nature, with a follow-up period of only 3 years and a limited number of patient cases. Therefore, a large prospective study observing the long-term prognosis is needed for further validation.
Conclusions
This study showed that CCRT + E improved 3-year PFS and DMFS in patients with LANPC compared with CCRT and that patients treated with CCRT + E had better cervical lymph node regression with a manageable safety profile.
Data availability
All data generated and analyzed during this study are included in this published article.
Abbreviations
- CCRT:
-
Concurrent chemoradiotherapy
- E:
-
Endostar
- NPC:
-
Nasopharyngeal carcinoma
- LANPC:
-
Locally advanced nasopharyngeal carcinoma
- IMRT:
-
Intensity-modulated radiation therapy
- HR:
-
Hazard ratio
- T:
-
Tumor
- N:
-
Lymph node
- CR:
-
Complete response
- VEGF:
-
Vascular endothelial growth factor
- UICC:
-
Union for International Cancer Control
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- PET/CT:
-
Positron emission tomography CT
- ICRU:
-
International Radiation Unit and Measurement Organization
- RTOG:
-
Radiation treatment oncology organization
- CTV:
-
Clinical target volume
- RECIST1.1:
-
Response evaluation criteria in solid tumours 1.1
- NCI-CTCAE:
-
National Cancer Institute Common Terminology Criteria for Adverse Events
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- DMFS:
-
Distant metastasis-free survival
- LRFFS:
-
Locoregional failure-free survival
References
Chen Y, Chan A, Le Q, et al. Nasopharyngeal carcinoma. Lancet (London, England). 2019;394(10192):64–80.
Wei K, Zheng R, Zhang S, et al. Nasopharyngeal carcinoma incidence and mortality in China, 2013. Chin J Cancer. 2017;36(1):90.
Au K, Ngan R, Ng A, et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: a report of 3328 patients (HKNPCSG 1301 study). Oral Oncol. 2018;77:16–21.
Zhang L, Huang Y, Hong S, et al. Gemcitabine plus cisplatin versus fluorouracil plus cisplatin in recurrent or metastatic nasopharyngeal carcinoma: a multicentre, randomised, open-label, phase 3 trial. Lancet (London, England). 2016;388(10054):1883–92.
Chen L, Hu C, Chen X, et al. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2012;13(2):163–71.
Wang J, Sun Y, Liu Y, et al. Results of randomized, multicenter, double-blind phase III trial of rh-endostatin (YH-16) in treatment of advanced non-small cell lung cancer patients. Chin J Lung Cancer. 2005;8(4):283–90.
Ling Y, Yang Y, Lu N, et al. Endostar, a novel recombinant human endostatin, exerts antiangiogenic effect via blocking VEGF-induced tyrosine phosphorylation of KDR/Flk-1 of endothelial cells. Biochem Biophys Res Commun. 2007;361(1):79–84.
Guan Y, Li A, **ao W, et al. The efficacy and safety of endostar combined with chemoradiotherapy for patients with advanced, locally recurrent nasopharyngeal carcinoma. Oncotarget. 2015;6(32):33926–34.
Cao Y. Opinion: emerging mechanisms of tumour lymphangiogenesis and lymphatic metastasis. Nat Rev Cancer. 2005;5(9):735–43.
Gao P, Zhou G, Zhang Q, et al. Lymphangiogenesis in gastric carcinoma correlates with prognosis. J Pathol. 2009;218(2):192–200.
Shang L, Zhao J, Wang W, et al. Inhibitory effect of endostar on lymphangiogenesis in non-small cell lung cancer and its effect on circulating tumor cells. Chin J Lung Cancer. 2014;17(10):722–9.
Zhou J, Wang L, Xu X, et al. Antitumor activity of Endostar combined with radiation against human nasopharyngeal carcinoma in mouse xenograft models. Oncol Lett. 2012;4(5):976–80.
** T, Li B, Chen X. A phase II trial of Endostar combined with gemcitabine and cisplatin chemotherapy in patients with metastatic nasopharyngeal carcinoma (NCT01612286). Oncol Res. 2013;21(6):317–23.
Ye W, Liu R, Pan C, et al. Multicenter randomized phase 2 clinical trial of a recombinant human endostatin adenovirus in patients with advanced head and neck carcinoma. Mol Ther. 2014;22(6):1221–9.
Li Y, Tian Y, ** F, et al. A phase II multicenter randomized controlled trial to compare standard chemoradiation with or without recombinant human endostatin injection (Endostar) therapy for the treatment of locally advanced nasopharyngeal carcinoma: long-term outcomes update. Curr Probl Cancer. 2020;44(1):100492.
Tang LL, Chen YP, Chen CB, et al. The Chinese Society of Clinical Oncology (CSCO) clinical guidelines for the diagnosis and treatment of nasopharyngeal carcinoma. Cancer Commun (Lond, Engl). 2021;41(11):1195–227.
Folkman J. Antiangiogenesis in cancer therapy–endostatin and its mechanisms of action. Exp Cell Res. 2006;312(5):594–607.
Kerbel R. Tumor angiogenesis: past, present and the near future. Carcinogenesis. 2000;21(3):505–15.
Fujita K, Sano D, Kimura M, et al. Anti-tumor effects of bevacizumab in combination with paclitaxel on head and neck squamous cell carcinoma. Oncol Rep. 2007;18(1):47–51.
Tan J, Jiang L, Cheng X, et al. Association between VEGF-460T/C gene polymorphism and clinical outcomes of nasopharyngeal carcinoma treated with intensity-modulated radiation therapy. Onco Targets Ther. 2017;10:909–18.
Li Y, Hu C, Shao Q, et al. Elevated expressions of survivin and VEGF protein are strong independent predictors of survival in advanced nasopharyngeal carcinoma. J Transl Med. 2008;6:1.
Chua D, Nicholls J, Sham J, et al. Prognostic value of epidermal growth factor receptor expression in patients with advanced stage nasopharyngeal carcinoma treated with induction chemotherapy and radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59(1):11–20.
Fountzilas G, Ciuleanu E, Bobos M, et al. Induction chemotherapy followed by concomitant radiotherapy and weekly cisplatin versus the same concomitant chemoradiotherapy in patients with nasopharyngeal carcinoma: a randomized phase II study conducted by the Hellenic Cooperative Oncology Group (HeCOG) with biomarker evaluation. Ann Oncol. 2012;23(2):427–35.
Tan T, Lim W, Fong K, et al. Concurrent chemo-radiation with or without induction gemcitabine, Carboplatin, and Paclitaxel: a randomized, phase 2/3 trial in locally advanced nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2015;91(5):952–60.
Li Y, ** F, Wu W, et al. Clinical results of recombinant human endostatin combined with chemoradiotherapy for locally advanced nasopharyngeal carcinoma. Chin J Oncol. 2015;37(2):128–32.
Jiang X, Dai P, Wu J, et al. Effect of recombinant human endostatin on radiosensitivity in patients with non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;83(4):1272–7.
Jiang X, Dai P, Qiao Y, et al. Clinical study on the recombinant human endostatin regarding improving the blood perfusion and hypoxia of non-small-cell lung cancer. Clin Transl Oncol. 2012;14(6):437–43.
Yao J, Fan L, Peng C, et al. Clinical efficacy of endostar combined with chemotherapy in the treatment of peritoneal carcinomatosis in gastric cancer: results from a retrospective study. Oncotarget. 2017;8(41):70788–97.
Zhang K, Yang S, Zhu Y, et al. Protection against acute radiation-induced lung injury: a novel role for the anti-angiogenic agent Endostar. Mol Med Rep. 2012;6(2):309–15.
Wang X, Hu C, Ying H, et al. Patterns of lymph node metastasis from nasopharyngeal carcinoma based on the 2013 updated consensus guidelines for neck node levels. Radiother Oncol. 2015;115(1):41–5.
Feng Y, Cao C, Hu Q, et al. Prognostic value and staging classification of lymph nodal necrosis in nasopharyngeal carcinoma after intensity-modulated radiotherapy. Cancer Res Treat. 2019;51(3):1222–30.
Liang S, Chen L, Yang X, et al. Influence of tumor necrosis on treatment sensitivity and long-term survival in nasopharyngeal carcinoma. Radiother Oncol. 2021;155:219–25.
Karakurt Eryılmaz M, Kadıyoran C. Prognostic significance of radiologic extranodal extension in nasopharyngeal cancer. Otolaryng Head Neck. 2022;166(2):321–6.
Lu H, Wu Y, Liu X, et al. Endostar, an antiangiogenesis inhibitor, combined with chemoradiotherapy for locally advanced cervical cancer. Oncol Res. 2022;28(9):929–44.
Zhai Y, Ma H, Hui Z, et al. HELPER study: A phase II trial of continuous infusion of endostar combined with concurrent etoposide plus cisplatin and radiotherapy for treatment of unresectable stage III non-small-cell lung cancer. Radiother Oncol. 2019;131:27–34.
Zhang S, Han C, Sun L, et al. Efficacy and safety of recombinant human endostatin combined with radiotherapy or chemoradiotherapy in patients with locally advanced non-small cell lung cancer: a pooled analysis. Radiat Oncol. 2020;15(1):205.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 71964003, 81460460, 81760542, 82160467), the Natural Science Foundation of Guangxi Zhuang Autonomous Region (No. 2018JJA141048), the Research Foundation of the Science and Technology Department of Guangxi Province, China (Grant Nos. 2016GXNSFAA380252, 2018AB61001 and 2014GXNSFBA118114), the Research Foundation of the Health Department of Guangxi Province, China (No. S2018087), Guangxi Medical University Training Program for Distinguished Young Scholars (2017), Medical Excellence Award Funded by the Creative Research Development Grant from the First Affiliated Hospital of Guangxi Medical University (2016).Guangxi Medical High-level Talents Training Program. The central government guide local science and technology development projects (ZY18057006).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. MK and YXY edited the manuscript. Material preparation and analysis were performed by YXY, ZYZ and ZRL. MJS, YTQ and CLY collected datas. YXY interpreted data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki. All methods were performed in accordance with the relevant guidelines and regulations. The study was approved by the Research Ethics Committee of Guangxi Medical University (NO. 2022-KY-E-(170)). Individual consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
All authors declared that they have no competing interests with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yin, Y., Zhou, Z., Li, Z. et al. Efficacy of concurrent chemoradiotherapy plus Endostar compared with concurrent chemoradiotherapy in the treatment of locally advanced nasopharyngeal carcinoma: a retrospective study. Radiat Oncol 17, 135 (2022). https://doi.org/10.1186/s13014-022-02104-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-022-02104-4