Abstract
Purpose
The objective of the study was to explore the effect of periodontally accelerated osteogenic orthodontics (PAOO) in orthodontic patients with bone dehiscence and fenestration in the anterior alveolar region of the mandible.
Methods
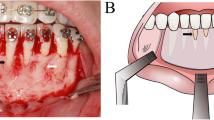
A retrospective study was performed in 42 patients with bone dehiscence and fenestrations in the anterior alveolar region of the mandible who underwent the PAOO technique. The bleeding index (BI), probing depth (PD), keratinized gingiva width (KGW), gingival recession level (GRL), and gingival phenotype were recorded and assessed at baseline and 6 and 12 months postoperatively. Cone-beam computerized tomography was used to measure bone volume in terms of root length (RL), horizontal bone thickness at different levels, and vertical bone height at baseline and 6 months and 12 months after surgery.
Results
The sample was composed of 42 patients (22 males and 20 females; mean age, aged 25.6 ± 4.8 years) with 81 teeth showing dehiscence/fenestrations and 36 sites presenting gingival recessions. There was no significant difference in BI, PD, or KGW (between baseline and 6 or 12 months postoperatively) based on the clinical evaluations (P > 0.05). Gingival recession sites demonstrated a significant reduction in the GRL after surgery (P < 0.05). Furthermore, the proportion of teeth with a thick gingival phenotype increased from 33.61% at baseline to 53.13% at the end of the follow-up. In addition, the bone thickness measurements at the mid-root and crestal levels were markedly increased compared with the baseline values (P < 0.05), although the increase in thickness at the apical level was not statistically significant (P > 0.05).
Conclusions
Within the limitations of the study, the results show that the PAOO technique is beneficial to periodontal conditions in terms of soft and hard tissue augmentation. The PAOO procedure may represent a safe and efficient treatment for orthodontic patients with bone dehiscence and fenestration.
Trial registration
This study was approved by the ethics committee of the stomatological hospital affiliated with **'an Jiaotong University (xjkqll [2019] No. 016) and registered in the Chinese Clinical Trial Registry (ChiCTR2100053092).
Similar content being viewed by others
Background
At present, the considerable number of adult orthodontic patients is driving demand for aesthetics-centred, function-oriented and fast-paced treatment, which poses a great challenge in clinical practice [1,9]. An accumulating body of research has indicated that PAOO has advantages over traditional orthodontic methods in terms of accelerated tooth movement up to 3 to 4 times, increased scope of orthodontic therapy, abridged treatment duration, sustainable alveolar bone augmentation, increased range of tooth movement, reduced root resorption and enhanced stability of the postorthodontic mandibular irregularity index for at least 10 years [8, 10,11,12]. To our knowledge, although the research to date has indicated that PAOO is a safe, time-consuming and effective treatment, most of the studies were case reports, [13,14,15] and there is a lack of systematic studies to ascertain whether PAOO is safe or detrimental to the periodontal tissues of adults, especially in patients with bone dehiscence and fenestration.
Bone dehiscence (a defect that extends to the cervical surface of the root, leading to marginal alveolar bone loss) and fenestration (a window that affects the root surface but is still bordered by bone along its coronal aspect) are the most common alveolar bone defects [16, 17]. A previous study noted that Class II and Class III subjects showed a high prevalence of bone defects surrounding the anterior mandibular teeth, with rates of up to 41.11% and 45.02%, respectively [18]. These defects usually lead to root exposure, gingival recession and even treatment relapse or failure, which pose challenges in orthodontic treatment [19, 20]. Therefore, shortening the duration of orthodontic treatment and decreasing severe sequelae are of great significance for orthodontic patients, especially adults with bone fenestration and dehiscence, which are also aesthetically significant issues that are time consuming to treat. PAOO has been regarded as a promising therapeutic strategy with minimal side effects in terms of root resorption and bone defect risks [16].
Therefore, the present study was designed to examine the clinical efficacy of PAOO in adult patients with bone fenestration and dehiscence. Periodontal status was evaluated by the bleeding index (BI), probing depth (PD), keratinized gingiva width (KGW), gingival recession level (GRL) and gingival phenotype at baseline and 3, 6 and 12 months postoperatively. Bone volume was also measured during the follow-up period, with the aim of providing guidance for the clinical application of PAOO therapy.
Methods
Study design
The present single-centre, retrospective study included 54 recruited subjects who were prescribed PAOO surgery by the Department of Periodontology, School of Stomatology, ** Sutures for Stabilization of Osseous Grafts With Resorbable Membranes for Buccal Ridge Augmentation: A Technique Report. J Oral Implantol. 2017;43(4):283–90." href="/article/10.1186/s13005-022-00344-z#ref-CR38" id="ref-link-section-d41782544e1688">38, 39]. Most studies have demonstrated periodontal regeneration following the combination approach. A systematic review showed histologically superior healing following the combination of barrier membranes and grafting materials when compared with barrier membranes alone or grafting materials alone [40]. Additionally, to avoid more invasive and less predictable regenerative procedures, stem cells of different origins, such as induced pluripotent stem cells (iPSCs), have been proposed as possible alternatives. IPSCs have the potential to proliferate and differentiate into all cell types derived from the three primary germ layers (ectoderm, endoderm and mesoderm), making them a potential alternative resource for the regeneration of either mineralized tooth components or supporting tissue. In addition, to avoid more invasive and less predictable regenerative procedures, Stem cells of different origins such as induced pluripotent stem cells (iPSCs) were proposed as possible alternative. IPSCs have potential for proliferation and differentiate into all derivatives of the three primary germ layers: ectoderm, endoderm and mesoderm, which could be proposed as alternative in regeneration either of mineralized tooth components or supporting tissue [41].
Root resorption, an undesirable sequela of traditional orthodontic treatment with a long treatment. Thus, the average orthodontic treatment time for adults is 18.7 to 31 months duration, is usually attributed to hyalinizing necrosis of the periodontal ligament and commonly identified in adults [6]. However, significant root resorption was not identified in the current study, which was in accordance with previous findings [28]. Based on the current understanding, after PAOO surgery is performed, cortical incision initiates the RAP to reduce the resistance to tooth movement, leading to a decrease in the orthodontic treatment time and a reduction in root resorption.
The present study, combined with previously published data show that, as a technology combines corticotomy-facilitated orthodontics, alveolar augmentation, and periodontal treatment, PAOO treatment facilitates the management of pre-existing bone fenestration and dehiscence, further improving the periodontal stability. PAOO differs from prior techniques by the additional step of alveolar bone grafting. It is this additional step that is believed to be responsible for the increased postoperative alveolar bone amount, which enhances the long-term orthodontic stability. All of the surgeries in our study were done on the buccal side. The surgery would done on the lingual/palatal side sometimes when patients undergoing lingual orthodontics or the need of lingual inclination of the anterior incisors. However, there lack of the study about lingual PAOO may due to the risk of violating important lingual anatomic structures. Nahm et.al showed that augmented corticotomy on the palate was beneficial for bodily movement in a bialveolar patient with an extremely thin alveolar bone housing [42].
The present study, combined with previously published data, shows that PAOO treatment, as a technology that combines corticotomy-facilitated orthodontics, alveolar augmentation, and periodontal treatment, improves periodontal stability by facilitating the management of pre-existing bone fenestration and dehiscence. However, although the present study demonstrated favourable results based on the outcomes obtained, there still exist some limitations, and the long-term clinical efficacy of PAOO in adult patients with bone fenestration and dehiscence remains unknown. In addition, although the quantity of new bone was ascertained, the quality of the newly formed bone also needs to be measured and analysed. In future studies, we will expand the dataset and continue the study along with histologic analysis to strengthen the basic theory and clinical basis for the proper use of PAOO.
Finally, suitable protective measures must be identified with regard to clothing, operating protocols, disinfection of environments, and management of waiting rooms and front offices under the circumstances of the COVID-19 pandemic [43].
Conclusion
The data obtained in the present study show that PAOO may represent a promising, safe, and effective treatment for adults with bone fenestration and dehiscence; it can result in improved periodontal health and simultaneously facilitate the repair of bone dehiscence and fenestration on the labial aspect of the mandibular anterior area, which can also be beneficial to soft tissue. However, further clinical investigations should be performed over a long follow-up period to evaluate long-term stability after PAOO.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- PAOO:
-
Periodontally accelerated osteogenic orthodontics
- RAP:
-
Regional acceleratory phenomenon
- BI:
-
Bleeding index
- PD:
-
Probing depth
- KGW:
-
Keratinized gingiva width
- GRL:
-
Gingival recession level
- CEJ:
-
Cemento-enamel junction
- RL:
-
Root length
- ABT:
-
Bone thickness at the apical level
- MBT:
-
Bone thickness at the mid-root level
- CBT:
-
Bone thickness at the crestal level
- VBH:
-
Vertical bone height
References
Hou HY, Li CH, Chen MC, Lin PY, Liu WC, Cathy Tsai YW, Huang RY. A novel 3D-printed computer-assisted piezocision guide for surgically facilitated orthodontics. Am J Orthod Dentofacial Orthop. 2019;155(4):584–91.
Yi J, **ao J, Li Y, Li X, Zhao Z. Efficacy of piezocision on accelerating orthodontic tooth movement: A systematic review. Angle Orthod. 2017;87(4):491–8.
Johal A, Joury E. What factors predict the uptake of orthodontic treatment among adults? Am J Orthod Dentofacial Orthop. 2015;147(6):704–10.
Amit G, Jps K, Pankaj B, Suchinder S, Parul B. Periodontally accelerated osteogenic orthodontics (PAOO) - a review. J Clin Exp Dent. 2012;4(5):e292–6.
Ong MM, Wang HL. Periodontic and orthodontic treatment in adults. Am J Orthod Dentofacial Orthop. 2002;122(4):420–8.
Hatrom AA, Howait MS, Zawawi KH, Al-Turki GA, Alansari RA, Almehayawi NF, Alammari SH, Mohammed RA, Hassan AH. Pulp volume changes after piezocision-assisted tooth movement: a randomized clinical trial. BMC Oral Health. 2021;21(1):28.
Moresca R. Orthodontic treatment time: can it be shortened? Dental Press J Orthod. 2018;23(6):90–105.
Ferguson DJ, Wilcko MT, Wilcko WM, Makki L. Scope of treatment with periodontally accelerated osteogenic orthodontics therapy. Semin Orthod. 2015;21(3):176e186.
Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar resha**: two case reports of decrowding. Int J Periodontics Restorative Dent. 2001;21(1):9–19.
Singh S, Jayan B. Comparative Evaluation of Periodontally Accelerated Osteogenic Orthodontics (PAOO) Versus Conventional Orthodontic Tooth Movement in Adult Patients with Bimaxillary Dentoalveolar Protrusion. Int J Periodontics Restorative Dent. 2019;39(4):571–7.
Farina R, Salinas F, Zurbuchen A, Hinojosa A, Barreda M. Corticotomy-assisted Le ~ Fort I osteotomy: an alternative to segmentation of the maxilla in orthognathic surgery. J Craniofac Surg. 2015;26(4):1316e1320.
Makki L, Ferguson DJ, Wilcko MT, Wilcko WM, Bjerklin K, Stapelberg R, Al-Mulla A. Mandibular irregularity index stability following alveolar corticotomy and grafting: A 10 year preliminary study. Angle Orthod. 2015;85:743–9.
AlHammadi HA, Wilcko MT, Ferguson DJ. Severe Mandibular Crowding Treated with Nonextraction Periodontally Accelerated Osteogenic Orthodontics. Int J Periodontics Restorative Dent. 2019;39(5):e188–94.
Muñoz F, Wilcko T, Acuña S, Gracia B, Sanhueza V, Palacios S, O’Ryan JA. Periodontally Accelerated Osteogenic Orthodontics (PAOO) technique in cleft patients: A complement to orthognathic surgery in dentoalveolar expansion. A case series report. J Craniomaxillofac Surg. 2020;48(11):1028–34.
Soltani L, Loomer PM, Chaar EE. A Novel Approach in Periodontally Accelerated Osteogenic Orthodontics (PAOO): A Case Report. Clin Adv Periodontics. 2019;9(3):110–4.
Nowzari H, Yorita FK, Chang HC. Periodontally accelerated osteogenic orthodontics combined with autogenous bone grafting. Compend Contin Educ Dent. 2008;29(4):200–6 quiz 207, 218.
Koke U, Sander C, Heinecke A, Müller HP. A possible influence of gingival dimensions on attachment loss and gingival recession following placement of artificial crowns. Int J Periodontics Restorative Dent. 2003;23(5):439–45.
Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S109–19.
Yagci A, Veli I, Uysal T, Ucar FI, Ozer T, Enhos S. Dehiscence and fenestration in skeletal Class I, II, and III malocclusions assessed with cone-beam computed tomography. Angle Orthod. 2012;82(1):67–74.
Enhos S, Uysal T, Yagci A, Veli İ, Ucar FI, Ozer T. Dehiscence and fenestration in patients with different vertical growth patterns assessed with cone-beam computed tomography. Angle Orthod. 2012;82(5):868–74.
Lucchese A, Matarese G, Manuelli M, Ciuffreda C, Bassani L, Isola G, Cordasco G, Gherlone E. Reliability and efficacy of palifermin in prevention and management of oral mucositis in patients with acute lymphoblastic leukemia: a randomized, double-blind controlled clinical trial. Minerva Stomatol. 2016;65(1):43–50.
Rothe LE, Bollen AM, Little RM, Herring SW, Chaison JB, Chen CS, Hollender LG. Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod Dentofacial Orthop. 2006;130(4):476–84.
Bahammam MA. Effectiveness of bovine-derived xenograft versus bioactive glass with periodontally accelerated osteogenic orthodontics in adults: a randomized, controlled clinical trial. BMC Oral Health. 2016;16(1):126.
Wang B, Shen G, Fang B, Yu H, Wu Y, Sun L. Augmented corticotomy-assisted surgical orthodontics decompensates lower incisors in Class III malocclusion patients. J Oral Maxillofac Surg. 2014;72(3):596–602.
Mazza JE, Newman MG, Sims TN. Clinical and antimicrobial effect of stannous fluoride on periodontitis. J Clin Periodontol. 1981;8(3):203–12.
Alkan Ö, Kaya Y, Tunca M, Keskin S. Changes in the gingival thickness and keratinized gingival width of maxillary and mandibular anterior teeth after orthodontic treatment. Angle Orthod. 2021;91(4):459–67.
Xu X, Wu JQ, Jiang JH, Liang C, Wang XE, **g WD, Xu L. Periodontal Effect of Periodontally Accelerated Osteogenic Orthodontics in Skeletal Angle Class III: A Nonrandomized, Controlled Trial. Int J Periodontics Restorative Dent. 2020;40(4):e169–77.
Miyamoto T, Lang M, Khan S, Kumagai K, Nunn ME. The clinical efficacy of deproteinized bovine bone mineral with 10% collagen in conjunction with localized piezosurgical decortication enhanced orthodontics: A prospective observational study. J Periodontol. 2019;90(10):1106–15.
Wilcko MT, Ferguson DJ, Makki L, Wilcko WM. Keratinized Gingiva Height Increases After Alveolar Corticotomy and Augmentation Bone Grafting. J Periodontol. 2015;86(10):1107–15.
Wang B, ** W, Chen H, Shao J, Song A, Zhang F. Periodontal effect of augmented corticotomy-assisted orthodontics versus conventional orthodontics in treatment of adult patients with bialveolar protrusion. BMC Oral Health. 2022;22(1):81.
Mattingly JA, Sauer GJ, Yancey JM, Arnold RR. Enhancement of Streptococcus mutans colonization by direct bonded orthodontic appliances. J Dent Res. 1983;62(12):1209–11.
Younes F, Eghbali A, Raes M, De Bruyckere T, Cosyn J, De Bruyn H. Relationship between buccal bone and gingival thickness revisited using non-invasive registration methods. Clin Oral Implants Res. 2016;27(5):523–8.
Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127(5):552–61 quiz 625.
Liu X, Fan B, Abdelrehem A, Ma Z, Yang C. Membrane fixation for osseous graft stabilization in periodontally accelerated osteogenic orthodontics: a comparative study. BMC Oral Health. 2020;20(1):22.
Coscia G, Coscia V, Peluso V, Addabbo F. Augmented corticotomy combined with accelerated orthodontic forces in class III orthognathic patients: morphologic aspects of the mandibular anterior ridge with cone-beam computed tomography. J Oral Maxillofac Surg. 2013;71(10):1760.e1-9.
Bhattacharya P, Bhattacharya H, Anjum A, Bhandari R, Agarwal DK, Gupta A, Ansar J. Assessment of Corticotomy Facilitated Tooth Movement and Changes in Alveolar Bone Thickness - A CT Scan Study. J Clin Diagn Res. 2014;8(10):ZC26-30.
Ma Z, Zheng J, Yang C, **e Q, Liu X, Abdelrehem A. A new modified bone grafting technique for periodontally accelerated osteogenic orthodontics. Medicine (Baltimore). 2018;97(37):e12047.
Shalev TH, Kurtzman GM, Shalev AH, Johnson DK, Kersten MEM. Continuous Periosteal Strap** Sutures for Stabilization of Osseous Grafts With Resorbable Membranes for Buccal Ridge Augmentation: A Technique Report. J Oral Implantol. 2017;43(4):283–90.
Behring J, Junker R, Walboomers XF, Chessnut B, Jansen JA. Towards guided tissue and bone regeneration: morphology, attachment, proliferation, and migration of cells cultured on collagen barrier membranes. Syst Rev Odontology. 2008;96(1):1–11.
Sculean A, Nikolidakis D, Schwarz F. Regeneration of periodontal tissues: combinations of barrier membranes and grafting materials - biological foundation and preclinical evidence: a systematic review. J Clin Periodontol. 2008;35(8 Suppl):106–16.
Tetè G, D’Orto B, Nagni M, Agostinacchio M, Polizzi E, Agliardi E. Role of induced pluripotent stem cells (IPSCS) in bone tissue regeneration in dentistry: a narrative review. J Biol Regul Homeost Agents. 2020;34(6 Suppl. 3):1–10.
Nahm KY, Shin SY, Ahn HW, Kim SH, Nelson G. Gummy Smile Correction Using Lingual Orthodontics and Augmented Corticotomy in Extremely Thin Alveolar Housing. J Craniofac Surg. 2017;28(7):e599–603.
Gherlone E, Polizzi E, Tetè G, Capparè P. Dentistry and Covid-19 pandemic: operative indications post-lockdown. New Microbiol. 2021;44(1):1–11.
Acknowledgements
The authors would like to acknowledge the statistical analysis of the research reported in this publication, which was supported by the Department of Statistics, School of Public Health, **'an Jiaotong University.
Funding
1. Medical research project of the 2018 "Science and Technology plus" Action Plan.
Number: 201805100YX8SF34 (1).
2. Natural Science Fund basic research programme of Shaanxi Province
Number: 2022JQ-772.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ziling Chen, Huan Zhou, Kaili Zhang, Yue Chen.
Formal Analysis: Ziling Chen, Kaili Zhang, Xu Wang.
Investigation: Ziling Chen, Xu Wang.
Methodology: Ziling Chen, Kaili Zhang, Xu Wang, Liangqiuyue Zhong.
Project Administration: Yue Chen, Yuxia Hou.
Writing – Original Draft: Ziling Chen, Huan Zhou, Xu Wang.
Writing – Review & Editing: Yue Chen, Huan Zhou, Yuxia Hou.
Corresponding author
Ethics declarations
Consent for publication
The authors have no competing interests that might be perceived to influence the results or discussion reported in this paper.
Ethics approval and consent to participate
This study was approved by the ethics committee of Stomatological Hospital affiliated with **'an Jiaotong University (xjkqll [2019] No. 016) and registered in the Chinese Clinical Trial Registry (ChiCTR2100053092).
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Z., Zhou, H., Zhang, K. et al. The clinical efficacy of periodontally accelerated osteogenic orthodontics in patients with bone fenestration and dehiscence: a retrospective study. Head Face Med 18, 40 (2022). https://doi.org/10.1186/s13005-022-00344-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13005-022-00344-z