Abstract
Background
Epidemiological studies have demonstrated that individuals with preexisting conditions, including diabetes mellitus (DM), are more susceptible to air pollution. However, the underlying mechanisms remain unclear. In this study, we proposed that a high glucose setting enhances ambient fine particulate matter (PM2.5)-induced macrophage activation and secretion of the proinflammatory cytokine, IL-1β, through activation of the NLRP3 inflammasome, altering the balance between matrix metalloproteinases (MMPs) and tissue inhibitors of MMPs (TIMPs).
Results
Exposure of mouse alveolar macrophages to non-cytotoxic doses of PM2.5 led to upregulation of IL-1β, activation of the NLRP3 inflammasome, increased nuclear translocation of the transcription factor NF-κB, increased generation of reactive oxygen species (ROS), and increased expression and enzymatic activity of MMP-9; these effects were enhanced when cells were pretreated with high glucose. However, pretreatment in a high glucose setting alone did not induce significant changes. ROS generation following PM2.5 exposure was abolished when cells were pretreated with ROS scavengers such as Trolox and superoxide dismutase (SOD), or with an NADPH oxidase inhibitor, DPI. Pretreatment of cells with DPI attenuated the effects of a high glucose setting on PM2.5-induced upregulation of IL-1β, activation of the NLRP3 inflammasome, and nuclear translocation of NF-κB. In addition, enhancement of PM2.5-induced expression and enzymatic activity of MMP-9 following high glucose pretreatment was not observed in primary alveolar macrophages obtained from NLRP3 or IL-1R1 knockout (KO) mice, where pro-IL-1β cannot be cleaved to IL-1β or cells are insensitive to IL-1β, respectively.
Conclusions
This study demonstrated that exposure of mouse alveolar macrophages to PM2.5 in a high glucose setting enhanced PM2.5-induced production of IL-1β through activation of the NLRP3 inflammasome and nuclear translocation of NF-κB due to PM2.5-induced oxidative stress, leading to MMP-9 upregulation. The key role of NADPH oxidase in PM2.5-induced ROS generation and activation of the IL-1β secretion pathway and the importance of IL-1β secretion and signaling in PM2.5-induced increases in MMP-9 enzymatic activity were also demonstrated. This study provides a further understanding of the potential mechanisms underlying the susceptibility of individuals with DM to air pollution and suggests potential therapeutic targets.
Similar content being viewed by others
Background
Air pollution, composed of particulate matter (PM) and gases such as sulfur and nitrogen dioxide, is a serious public health issue. Fine ambient PM of diameter less than or equal to 2.5 µm (PM2.5) can penetrate from the mouth and throat deep into the lungs, posing serious health problems [1]. Epidemiological studies suggest a link between particulate air pollution and increased morbidity and mortality from respiratory and cardiovascular diseases [2,3,4,5]. In addition, epidemiological studies and animal experiments have shown that individuals with preexisting conditions, such as diabetes mellitus, chronic obstructive pulmonary disease (COPD), asthma, fatty liver disease, sepsis, etc., are more susceptible to air pollution [6,7,8,9,10]. However, the mechanisms underlying this susceptibility are still not clarified.
Diabetes mellitus (DM) is the most common endocrine disorder in humans. DM is principally characterized by hyperglycemia, resulting in microvascular and macrovascular complications, such as diabetic retinopathy, coronary artery disease, etc., that increase mortality and reduce the quality of life. Diabetes can increase the severity and clinical course of several pulmonary diseases including asthma, COPD, fibrosis, pulmonary hypertension, lung cancer, etc., which is mainly associated with the pro-inflammatory and proliferative properties of diabetes [11]. Several epidemiological studies have shown that people with DM are especially sensitive to the effects of PM on daily mortality and pulmonary and cardiovascular disease hospitalizations [9]. However, a biological mechanism linking PM exposure to exacerbated impairment of pulmonary and cardiovascular function in people with DM is still unknown.
The first step of PM-induced pulmonary injury is the inflammatory response, where immune cells such as macrophages, neutrophils, etc. are excessively activated. A variety of cytokines have been implicated in the pathogenesis of PM-induced lung inflammation and injury [12]. IL-1β is one of a family of pro-inflammatory cytokines thought to be involved in the initiation of the inflammatory process, contributing to acute and chronic inflammation [13, 14]. Excessive pro-inflammatory activity driven by IL-1β is a major pathophysiological event in several autoimmune, neurodegenerative, and metabolic diseases. IL-1β is released by a highly regulated process, in which caspase-1-mediated cleavage of pro-IL-β is the rate-limiting step [14]. Previous studies have shown that exposure to either PM or high glucose causes IL-1β secretion in macrophages or monocytes [15,16,17]. Though the detailed mechanisms by which IL-1β is induced are unknown, previous studies have shown that activation of the NLRP3 inflammasome and/or toll-like receptors (TLRs), oxidative stress, nuclear translocation of transcription factor NF-κB, etc., may be involved in PM or high glucose-induced IL-1β secretion [15,16,17].
Although several studies have addressed the modulation of the macrophage response to PM, few studies have focused on the combined effects of PM and high glucose on macrophages, especially concerning the production of IL-1β and the underlying mechanisms responsible. Hence, the purpose of this study was to evaluate the effects of PM2.5 on mouse alveolar macrophages with and without high glucose pretreatment and to identify the potential mechanisms involved in the enhanced susceptibility of macrophages to PM2.5 in a high glucose environment. The hypothesis was that exposure of alveolar macrophages to PM2.5 in the setting of high glucose would result in enhanced activation of alveolar macrophages, leading to increased production of IL-1β through activation of NLRP3 inflammasome and/or TLRs and increased nuclear translocation of transcription factor NF-κB by PM2.5-induced oxidative stress, finally resulting in MMPs/TIMPs imbalance.
Methods
Fine ambient particulate matter (PM2.5)
Fine ambient particulate matter (PM2.5), a Standard Reference Material® (SRM 2786) with a mean diameter of approximately 2.8 μm, was purchased from the National Institute of Standards and Technology (NIST) (Gaithersburg, MD, USA). Its certificate of analysis is available online (https://tsapps.nist.gov/srmext/certificates/2786.pdf). In this study, PM2.5 was prepared at a concentration of 5 mg/mL in physiological saline and diluted with physiological saline if necessary. The PM2.5 was vortexed thoroughly before each experiment.
Chemicals and reagents
Primary antibodies including anti-IL-1β (D6D6T) (cat. no. 31202, 1:500), anti-cleaved IL-1β (E7V2A) (cat. no. 63124, 1:1000), anti-NLRP3 (D4D8T) (cat. no. 15101, 1:1000), anti-TLR2 (E1J2W) (cat. no. 13744, 1:1000), anti-Histone H3 (cat. no. 9715, 1:2000), and anti-β-actin (E4D9Z) (cat. no. 58169, 1:2000) antibodies, and secondary antibodies including HRP-conjugated goat anti-rabbit IgG (cat. no. 7074, 1:2000) and horse anti-mouse IgG (cat. no. 7076, 1:2000) were purchased from the Cell Signaling Technology (Beverly, MA, USA). Anti-NF-κB p65 (F-6) (cat. no. sc-8008, 1:200) was obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Cell culture and PM2.5 and/or high glucose treatment
Immortalized mouse alveolar macrophages MH-S were purchased from American Type Culture Collection (ATCC, cat. no. CRL-2019, Manassas, VA, USA) and cultured in an incubator with a humidified atmosphere of 5% CO2 at 37 °C. The complete cell culture medium contained RPMI 1640 medium (cat. no. 10–043-CV, without glucose, Corning, Manassas, VA, USA) supplemented with 10% FBS, 100 IU/mL penicillin, 100 μg/mL streptomycin (Corning), 0.05 mM 2-mercaptoethanol (Gibco, Grand Island, NY, USA), and 5 mM glucose (Acros Organics, NJ, USA).
To determine the mRNA or protein expression levels of pro-inflammatory cytokines (IL-1β and IL-18), components of NLRP3 inflammasome (NLRP3 and caspase-1), Toll-like receptors (TLR2 and TLR4), NF-κB p65 (nuclear and cytoplasmic), MMPs (MMP-2 and MMP-9), and TIMPs (TIMP-1 and TIMP-2) in MH-S macrophages after PM2.5 exposure, the cells were treated with 25 or 50 μg/mL of PM2.5 for 1, 3, 6, 12, or 24 h (time-response study), or with 25, 50, and 100 μg/mL of PM2.5 for 6 h (dose–response study). To determine whether the effects of PM2.5 were enhanced at a high glucose setting, the MH-S cells were cultured in complete medium containing 30 mM glucose. The control cells were cultured in complete medium only. Mannitol was used as an osmolality control. 3 × 106 cells in 20 mL medium were seeded in each 75 cm2 flask (day 0). The medium was refreshed on day 4 and day 7. On day 9, the cells were split, and 3 × 106 cells were seeded for another cycle. After 2 cycles (18 days), the cells were collected and 1 × 106 cells in 2 mL medium were seeded in each well of 6-well plates. After overnight culture, the medium was refreshed, and the cells were treated with 25 or 50 μg/mL of PM2.5 (20 μL of 2.5 or 5 mg/mL of PM2.5) for 3 h (for IL-1β, NLRP3, or TLR2 mRNA), 6 h (for IL-1β, NLRP3, or TLR2 protein by Western blot), or 24 h (for MMPs and TIMPs). The cells treated with physiological saline (20 μL) were used as a control.
Cytotoxicity of PM2.5 and/or glucose on mouse alveolar macrophages MH-S
The cells were seeded in 96-well plates. After overnight culture, the cells were treated with 0, 25, 50, 100, 200, and 400 μg/mL of PM2.5 or 5, 10, 20, 30, 40, and 50 mM of glucose for 24 h. The cytotoxicity of PM2.5 or glucose in MH-S cells was determined by two different methods: CellTiter 96 AQueous Non-Radioactive Cell Proliferation Assay (MTS assay) (Promega, Madison, WI, USA) and alamarBlue™ assay (Invitrogen, Eugene, OR, USA) according to the manufacturer’s instructions. To observe whether there was cytotoxicity with PM2.5 treatment in a high glucose environment, the cells were pretreated with 30 mM glucose for 18 days followed by 25 or 50 μg/mL of PM2.5 treatment for another 24 h. Mannitol was used as an osmolality control.
Total RNA isolation and RT-qPCR
Total RNA was isolated from the cells by using TRIzol® reagent (Sigma-Aldrich, St. Louis, MO, USA), and RT-qPCR was performed as described previously [18, 19]. 2 µg total RNA was reverse-transcribed into cDNA by using M-MLV reverse transcriptase (Promega, Madison, WI, USA). qPCR was performed by using iTaq™ Universal SYBR® Green Supermix (Bio-Rad, Hercules, CA, USA) on a BioRad iQ5 Multicolor Real-Time PCR Detection System (Bio-Rad). The PCR reaction was performed as follows: 40 cycles at 94 °C for 10 s, at 58 °C for 45 s, and at 72 °C for 45 s. Data were quantified by using the 2−ΔΔCt (Livak) method [20]. β-actin was used as an internal control. All the primers used were listed in Table 1.
Protein extraction and Western blot
Total protein was isolated from the cells by RIPA lysis buffer (Santa Cruz Biotechnology, Santa Cruz, CA, USA) while nuclear and cytoplasmic proteins were extracted by using NE-PER™ Nuclear and Cytoplasmic Extraction Reagent (Thermo Scientific, Rockford, IL, USA) according to the manufacturer’s instructions. Western blot was performed as described previously [18, 21]. The expression of β-actin was used as an internal reference for cytoplasmic or total protein, and histone H3 was for nuclear protein. Immunoreactive bands were quantified by using NIH ImageJ software (http://imagej.nih.gov/ij/). Uncropped versions of Western blots were shown in Additional file 5.
Measurement of ROS
ROS generation in mouse alveolar macrophages MH-S after PM2.5 and/or high glucose exposure was determined by using 2', 7'-dichlorodihydrofluorescein diacetate (H2DCF-DA, Molecular Probes, Eugene, OR, USA). The cells seeded in 96-well plates were pretreated with 5 µM of H2DCF-DA for 2 h before the cells were exposed to 0, 6.3, 12.5, 25, and 50 μg/mL of PM2.5 for 12 h, or to 50 μg/mL of PM2.5 for 3, 6, 12, and 24 h. To determine the effects of PM2.5 on ROS generation in MH-S cells with high glucose pretreatment, the cells were pretreated with 30 mM of glucose for 18 days. Then the cells were seeded and pretreated with 5 µM of H2DCF-DA for 2 h, followed by treatment with 50 μg/mL of PM2.5 for another 12 h. The cells treated with physiological saline were used as the control, and mannitol was used as an osmolality control. The DCF fluorescence was measured by using a Synergy HT microreader (BioTek, Winooski, VT, USA) at λex485/ λem528.
To observe the effects of ROS scavenges or inhibitors on ROS generation in MH-S cells after PM2.5 exposure, the following reagents were used: (1) 100 μM of Trolox (Sigma-Aldrich, St. Louis, MO, USA), a water-soluble analog of vitamin E which has an antioxidant effect; (2) 10 μM of diphenyleneiodonium chloride (DPI) (Alexis, San Diego, CA, USA), a specific inhibitor of NADPH oxidase; and (3) 300 U/mL of superoxide dismutase (SOD) (Sigma-Aldrich), an enzyme that catalyzes the dismutation of the superoxide radical into oxygen and hydrogen peroxide. The cells were pre-treated with ROS scavenges or inhibitors for 2 h and 5 μM of H2-DCFDA for another 2 h, followed by 25 or 50 μg/mL of PM2.5 treatment for 12 h. The fluorescence values were measured as described above.
MitoSOX™ Red Mitochondrial Superoxide Indicator (Invitrogen, Eugene, OR, USA) was used to detect mitochondrial ROS generation in MHS cells after PM2.5 exposure according to the manufacturer’s instructions. Briefly, the cells were pretreated with 5 µM of MitoSOX™ for one hour before 0, 6.3, 12.5, 25, and 50 μg/mL of PM2.5 exposure for another 12 h. The fluorescence at λex530/ λem590 was recorded by a Synergy HT microreader (BioTek, Winooski, VT, USA).
Measurement of cytokines and MMP-2/9 by ELISA
The levels of IL-1β in the cell culture media were determined by Mouse IL-1beta ELISA kit (cat. no. BMS6002, Invitrogen by Thermo Fisher Scientific, Vienna, Austria) while the MMP-2 and MMP-9 protein levels were analyzed by Mouse MMP-2 or MMP-9 PicoKine™ ELISA Kit (cat. no. EK0460 or EK0466, Boster Biological Technology, Pleasanton, CA, USA) according to the manufacturer’s instructions.
Gelatin zymography assay
The enzymatic activities of MMP-2 and MMP-9 were determined by gelatin zymography assay as described in our previous studies [19, 22]. Briefly, the cells were cultured in FBS-free media for 24 h prior to PM2.5 exposure. At the end of exposure, the cell culture media were collected, and an equal volume of media was loaded in each lane of 10% SDS-PAGE copolymerized with 0.5 mg/mL gelatin, which was used as the substrate under nonreducing conditions. After washing 4 times (15 min each) with renaturing buffer [50 mM Tris–HCl buffer (pH 7.5), 2.5% Triton X-100] at room temperature, the gels were incubated in calcium assay buffer [50 mM Tris–HCl buffer (pH 7.5), 0.2 M NaCl, 7.55 mM CaCl2, 1 μM ZnCl2, and 1% Triton X-100] at 37 °C overnight. After briefly washing with ddH2O, the gel was stained with 0.1% Coomassie Brilliant Blue R-250 (Bio-Rad, Hercules, CA, USA) at room temperature for one hour, then destained with 10% acetic acid until the clear bands were observed.
Isolation of alveolar macrophages from mice
Animal use was reviewed and approved by the University of Louisville Institutional Animal Care and Use Committee. Wild-type C57BL/6J (JAX stock no. 000664), NLRP3 knockout (KO) (B6.129S6-Nlrp3tm1Bhk/J, JAX stock no. 021302), and IL-1R1 KO (B6.129S7-Il1r1tm1Imx/J, JAX stock no. 003245) mice were purchased from The Jackson Laboratory (Bar Harbor, ME, USA), and both strains of homozygous KO mice are viable, fertile, and bred in our university animal facility. The mice were housed in an air-conditioned room (temperature of 20 ± 2 °C, relative humidity of 60 ± 10%) with a 12 h light and 12 h dark cycle environment and with free access to food and water.
Primary alveolar macrophages were isolated from C57BL/6J, NLRP3 KO, and IL-1R1 KO mice by bronchoalveolar lavage (BAL) as described previously [23, 24]. 0.8 mL of ice-cold FBS- and glucose-free RPMI 1640 medium supplemented with 100 IU/mL penicillin, 100 μg/mL streptomycin, and 0.4 mM EDTA was used to lavage the lungs. Each mouse was lavaged six times, and approximately 1 × 105 macrophages were obtained from each mouse. The lavage fluid from the same strain of mice was combined and centrifugated at 200 × g and 4 °C for 10 min. After centrifugation, the cells were resuspended at 2 × 105 or 6 × 105 cells/mL in RPMI 1640 medium supplemented with 10% FBS, 100 IU/mL penicillin, 100 μg/mL streptomycin, 0.05 mM 2-mercaptoethanol, and 5 mM glucose. Then, 1 × 105 (for IL-1β and NLRP3 mRNA) or 3 × 105 (for MMP-2/9 protein and activity) cells were seeded into each well of a 24-well plate. The cells were treated with 50 μg/mL of PM2.5 for 3 h (for IL-1β and NLRP3 mRNA) or 24 h (for MMP-2/9 protein and activity) with/without 30 mM glucose pretreatment for 24 h. After treatment, the cells or the cell culture media were collected. If the cell culture media would be used for the determination of MMP-2 and MMP-9 protein levels by ELISA or their activities by gelatin zymography assay, FBS-free medium was used to culture the cells. The above procedures were repeated three times.
Statistical analysis
Data were expressed as the mean ± SEM, and the differences were analyzed by one-way analysis of variance (ANOVA) followed by Dunnett (for comparison with the control) or Bonferroni (for all pairwise comparisons) post-hoc test or two-way ANOVA followed by the Holm-Sidak test by using SigmaPlot 13.0 software (Systat Software, Inc., San Jose, CA, USA). A difference was considered statistically significant when a p-value was less than 0.05.
Results
Cytotoxicity of PM2.5 and/or glucose on mouse alveolar macrophages MH-S
To find the appropriate non-cytotoxic doses for the following mechanism study, the cytotoxicity of PM2.5 or glucose in mouse alveolar macrophages MH-S was at first determined. The results showed that exposure of MH-S cells to 50 μg/mL or less of PM2.5 for 24 h did not cause significant cytotoxicity although exposure to 100 μg/mL or above of PM2.5 did by using MTS assay (Fig. 1a), which was further confirmed by using alamarBlue™ assay (Additional file 1). On the other hand, treatment with as high as 50 mM glucose did not result in any cytotoxicity in MH-S cells (Fig. 1b). Therefore, in the subsequent experiments, non-cytotoxic doses of PM2.5 (≤ 50 µg/mL) and glucose (30 mM) were chosen to observe the effects of PM2.5 with/without high glucose pretreatment on mouse alveolar macrophages. When the cells were pretreated with 30 mM glucose or mannitol (as an osmolality control) for 18 days followed by 25 or 50 µg/mL of PM2.5 treatment for another 24 h, no cytotoxicity was observed (Fig. 1c).
Cytotoxicity of PM2.5 and/or glucose on MH-S cells. a and b The cells were treated with PM2.5 or glucose for 24 h. c The cells were pretreated with 30 mM of glucose for 18 days, followed by treatment with PM2.5 for 24 h. Mannitol was used as an osmolality control. The cells treated with physiological saline were used as control. Cytotoxicity was determined by MTS assay (Promega). Data are shown as mean ± SEM (n = 6). * p < 0.05 vs. control
Exposure to PM2.5 caused upregulation of IL-1β, NLRP3, and TLR2 in MH-S cells
The expression levels of pro-inflammatory cytokines (IL-1β and IL-18), components of NLRP3 inflammasome (NLRP3 and caspase-1), and TLRs (TLR2 and TLR4) in mouse alveolar macrophages MH-S were determined at both mRNA level by RT-qPCR and protein level by Western blot. For RT-qPCR, the cells were exposed to 25 or 50 μg/mL of PM2.5 for 1, 3, 6, 12, and 24 h. The results showed that 50 μg/mL of PM2.5 exposure caused significantly increased IL-1β mRNA expression as early as 1 h after exposure. Exposure of the cells to both 25 and 50 μg/mL of PM2.5 for 3 h caused near 25-fold increase in IL-1β mRNA, which maintained an increase at 6, 12, and 24 h after PM2.5 exposure (Fig. 2a). However, only 50 μg/mL of PM2.5 exposure for 6 h caused a twofold increase in IL-18 mRNA, which returned to baseline level at 12 and 24 h after PM2.5 exposure (Fig. 2a). In addition, 25 and 50 μg/mL of PM2.5 exposure also caused significant upregulation of NLRP3 and TLR2, but not caspase-1 and TLR4, at the similar pattern as IL-1β mRNA expression (Fig. 2b, c).
mRNA expression levels of pro-inflammatory cytokines (a), components of NLRP3 inflammasome (b), and TLRs (c) in MH-S cells exposed to PM2.5 (dose- and time-response studies). The cells were treated with 25 or 50 μg/mL of PM2.5 for 1, 3, 6, 12, and 24 h. The cells treated with physiological saline were used as control. The mRNA expression of the gene was determined by RT-qPCR and normalized to the β-actin expression in the same sample. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control
The upregulation of IL-1β, NLRP3, and TLR2 after PM2.5 exposure was further confirmed at the protein level by Western blot. The results of the dose–response study revealed that exposure of MH-S cells to 25, 50, and 100 μg/mL of PM2.5 for 6 h caused significant upregulation of pro-IL-1β, cleaved IL-1β, NLRP3, and TLR2 (Fig. 3a, b). The time-response study showed that both pro-IL-1β and cleaved IL-1β were significantly increased in MH-S cells exposed to 50 μg/mL of PM2.5 for 3 h and 6 h after exposure (Fig. 4a, b). Then the pro-IL-1β level decreased to near baseline level after 50 μg/mL of PM2.5 treatment for 12 h while the cleaved IL-1β level was still significantly increased (Fig. 4a, b). NLRP3 protein expression level had a similar trend as pro-IL-1β; increased at 3 and 6 h after 50 μg/mL of PM2.5 treatment and decreased at 12 h after treatment (Fig. 4a, b). The TLR2 protein level was significantly increased in MH-S cells exposed to 50 μg/mL of PM2.5 for 3, 6, and 12 h (Fig. 4a, b).
Dose–response study of protein expression of IL-1β, NLRP3, and TLR2 in MH-S cells exposed to PM2.5. The cells were treated with 25, 50, and 100 μg/mL of PM2.5 for 6 h. The cells treated with physiological saline were used as control. a is the Western blot result of a single experiment while b is the normalized results of Western blots. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control
Time-response study of protein expression of IL-1β, NLRP3, and TLR2 in MH-S cells exposed to PM2.5. The cells were treated with 50 μg/mL of PM2.5 for 3, 6, and 12 h. The cells treated with physiological saline were used as control. a is the Western blot result of a single experiment while b is the normalized results of Western blots. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control
High glucose pretreatment enhanced PM2.5-induced upregulation of IL-1β and NLRP3, but not TLR2
At first, the mRNA expression levels of IL-1β, NLRP3, and TLR2 were determined by RT-qPCR after MH-S cells were pretreated with 30 mM of glucose for 9 days followed by treatment with 50 μg/mL of PM2.5 for 3 h. The results showed that although PM2.5 exposure significantly upregulated IL-1β, NLRP3, and TLR2 in control cells (5 mM glucose), no enhanced expression was observed in the cells with high glucose pretreatment (data not shown). Then the cells were maintained in 30 mM of glucose environment for 18 days followed by treatment with 50 μg/mL of PM2.5 for 3 h. Our results showed that PM2.5 exposure caused significantly increased mRNA expression levels of IL-1β, NLRP3, and TLR2 (Fig. 5), which were consistent with the results of dose- and time-dependent studies (Fig. 2). Moreover, the mRNA levels of both IL-1β and NLRP3, but not TLR2, were enhanced in MH-S cells with high glucose, but not osmolarity control mannitol, pretreatment (Fig. 5a-c). Thus, a time point of 18 days of high glucose pretreatment was selected. The enhanced mRNA expression of IL-1β and NLRP3 by PM2.5 exposure with high glucose pretreatment was also observed in primary alveolar macrophages obtained from C57BL/6J mice by bronchoalveolar lavage (BAL) (Additional file 2).
Enhanced mRNA expression of IL-1β (a) and NLRP3 (b), but not TLR2 (c) in MH-S cells exposed to PM2.5 at high glucose setting. The cells were treated with 50 μg/mL of PM2.5 for 3 h with/without 30 mM of glucose pretreatment for 18 days. Mannitol was used as an osmolality control. The cells treated with physiological saline were used as control. The mRNA expression of the gene was determined by RT-qPCR and normalized to the β-actin expression in the same sample. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with PM2.5 treatment only
The mRNA expression results were further confirmed at protein levels by Western blot; the protein expression levels of pro-IL-1β, cleaved IL-1β, and NLRP3, but not TLR2, were enhanced in MH-S cells exposed to 50 μg/mL of PM2.5 for 6 h with high glucose pretreatment for 18 days (Fig. 6a, b). Moreover, the IL-1β protein levels in the cell culture media, determined by ELISA, were increased in a time-dependent manner when MH-S cells were exposed to 50 μg/mL of PM2.5 for 6, 12, and 24 h, with significant increase at 24 h after PM2.5 exposure (Fig. 6c). And this effect was enhanced in the cells with 30 mM glucose pretreatment for 18 days (Fig. 6d). These results suggest that in a high glucose environment, PM2.5 exposure caused enhanced production of pro-inflammatory cytokine IL-1β and activation of NLRP3 inflammasome.
High glucose pretreatment enhanced the effects of PM2.5 on the activation of NLRP3 inflammasome, but not TLR2, in MH-S cells. The cells were treated with 50 μg/mL of PM2.5 for 6 h (a and b) or 24 h (d) with/without 30 mM of glucose pretreatment for 18 days. c The cells were treated with 50 μg/mL of PM2.5 for 6, 12, and 24 h. The cells treated with physiological saline were used as control. a is the Western blot result of a single experiment while b is the normalized results of Western blots. c and d The cell culture media were collected for ELISA by Mouse IL-1beta ELISA kit (Invitrogen). Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with PM2.5 treatment only. n.s., not specific
Enhanced NF-κB nuclear translocation in MH-S cells exposed to PM2.5 in a high glucose environment
NF-κB binding sites have been identified in the promoter region of both human and mouse IL-1β [25,26,27] and NLRP3 [28, 29]. Therefore, we next determined whether PM2.5 exposure caused NF-κB nuclear translocation by detection of both nuclear and cytoplasmic NF-κB p65 protein levels by Western blot. The results of both dose- and time-response studies showed that exposure of MH-S cells to PM2.5 caused significantly increased expression of NF-κB p65 in the nuclei but decreased expression in the cytoplasm, indicating that PM2.5 exposure caused NF-κB nuclear translocation (Fig. 7a-d). After MH-S cells were pretreated with 30 mM of glucose for 18 days, 50 μg/mL of PM2.5 treatment caused an even higher level of nuclear and lower level of cytoplasmic NF-κB p65 protein expression (Fig. 7e, f), indicating PM2.5 exposure caused enhanced nuclear translocation of NF-κB in a high glucose environment.
Enhanced NF-κB nuclear translocation in MH-S cells exposed to PM2.5 in a high glucose environment. The cells were treated with 25, 50, and 100 μg/mL of PM2.5 for 6 h (a and b) or with 50 μg/mL of PM2.5 for 3, 6, and 12 h (c and d). e and f The cells were treated with 50 μg/mL of PM2.5 for 6 h with/without 30 mM glucose pretreatment for 18 days. The cells treated with physiological saline were used as control. Nuclear and cytoplasmic proteins were extracted from the cells by using NE-PER™ Nuclear and Cytoplasmic Extraction Reagent (Thermo Scientific). The expression of β-actin was used as an internal reference for cytoplasmic protein while histone H3 was for nuclear protein. a, c, e are Western blot results of a single experiment while b, d, f are normalized results of Western blots. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with PM2.5 treatment only. Nuc, nuclear protein; Cyt, cytoplasmic protein
Enhanced ROS generation in MH-S cells exposed to PM2.5 at high glucose setting and the possible source of ROS
ROS generation in mouse alveolar macrophages MH-S after exposure to PM2.5 with/without high glucose pretreatment was determined by measurement of DCF fluorescence intensity. PM2.5 exposure caused a dose-and a time-dependent increase in DCF fluorescence when the cells were exposed to 6.3, 12.5, 25, and 50 μg/mL of PM2.5 for 12 h (Fig. 8a) or to 50 μg/mL of PM2.5 for 3, 6, 12, and 24 h (Fig. 8b). When the cells were pretreated with 30 mM of glucose for 18 days, 50 μg/mL of PM2.5 exposure induced an enhanced ROS generation (Fig. 8c). However, 30 mM glucose treatment alone did not cause any increase in ROS generation, and the osmolality control mannitol did not cause any enhanced ROS generation induced by PM2.5 exposure (Fig. 8c). These results indicated that PM2.5 exposure could induce enhanced oxidative stress on alveolar macrophages in a high glucose environment.
Enhanced ROS generation in MH-S cells exposed to PM2.5 with high glucose pretreatment. The cells were pretreated with 5 µM of H2DCF-DA for 2 h, followed by treatment with PM2.5 for 12 h (a) or with 50 μg/mL of PM2.5 for 3, 6, 12, and 24 h (b). c The cells were pretreated with 30 mM of glucose for 18 days and 5 µM of H2DCF-DA for 2 h, followed by treatment with PM2.5 for 12 h. Mannitol was used as an osmolality control. d The cells were pretreated with ROS inhibitors or scavengers for 2 h, followed by treatment with 5 µM of H2DCF-DA for 2 h and PM2.5 for 12 h. e The cells were pretreated with 30 mM of glucose for 18 days and DPI for 2 h, followed by treatment with 5 µM of H2DCF-DA for 2 h and PM2.5 for 12 h. The cells treated with physiological saline were used as control. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with the same dose of PM2.5 treatment only; $ p < 0.05 vs. group with the same PM2.5 and glucose treatments, but without DPI pretreatment
To determine the possible source of ROS in MH-S cells exposed to PM2.5 with/without high glucose pretreatment, ROS inhibitors or scavengers were used to pretreat the cells prior to 25 and 50 μg/mL of PM2.5 exposure. The results showed that pretreatment of the cells with 10 μM of DPI (a specific NADPH oxidase inhibitor), 100 μM of Trolox (an antioxidant), or 300 U/mL of superoxide dismutase (SOD, an enzyme that catalyzes the dismutation of the superoxide radical into oxygen and hydrogen peroxide) significantly inhibited PM2.5-induced ROS generation (Fig. 8d). However, the production of superoxide by mitochondria was not increased after PM2.5 exposure by using MitoSOX™ Red Mitochondrial Superoxide Indicator (Additional file 3). In addition, pretreatment of the cells with 10 μM of DPI also abolished PM2.5-induced ROS generation in the cells in a high glucose environment (Fig. 8e). All these results suggest that NADPH oxidase, rather than mitochondria, may be responsible for PM2.5-induced enhanced ROS generation in alveolar macrophages with high glucose pretreatment.
In addition, to determine the role of activation of NADPH oxidase in NF-κB nuclear translocation, NLRP3 inflammasome activation, and IL-1β production induced by PM2.5 exposure in a high glucose environment, the cells with/without high glucose pretreatment were treated with 10 μM of DPI for 2 h followed by treatment with 50 μg/mL of PM2.5 for 6 h. The results showed that DPI pretreatment significantly attenuated PM2.5-induced NF-κB nuclear translocation and increased expression of NLRP3, pro-IL-1β, and cleaved IL-1β in MH-S cells with/without high glucose pretreatment (Fig. 9a-c), suggesting ROS generated by NADPH oxidase is responsible for PM2.5-induced NF-κB nuclear translocation, NLRP3 inflammasome activation, and IL-1β production in alveolar macrophages.
Inhibition of NADPH oxidase by DPI abolished PM2.5-induced NF-κB nuclear translocation, NLRP3 inflammasome activation, and IL-1β production. The MH-S cells were treated with 10 μM DPI for 2 h, followed by 50 μg/mL of PM2.5 for 6 h with/without 30 mM glucose pretreatment for 18 days. The cells treated with physiological saline were used as control. Nuclear and cytoplasmic proteins were extracted from the cells by using NE-PER™ Nuclear and Cytoplasmic Extraction Reagent (Thermo Scientific). The expression of β-actin was used as an internal reference for cytoplasmic protein while histone H3 was for nuclear protein. a is the Western blot result of a single experiment while b and c are the normalized results of Western blots. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with PM2.5 treatment only; $ p < 0.05 vs. group with the same PM2.5 and glucose treatments, but without DPI pretreatment. Nuc, nuclear protein; Cyt, cytoplasmic protein; n.s., not specific
Enhanced MMP-9 production by IL-1β in alveolar macrophages exposed to PM2.5 in a high glucose environment
At first, MMP-2 and MMP-9 mRNA expression levels were determined by RT-qPCR in MH-S cells exposed to 25 or 50 μg/mL of PM2.5 for 3, 6, 12, and 24 h. The results showed that exposure of MH-S cells to PM2.5 caused a time-dependent and significant increase in MMP-9 mRNA expression (Fig. 10a). However, PM2.5 exposure only caused a slight, but not significant, upregulation of MMP-2 (Fig. 10b), TIMP-1, and TIMP-2 (Additional file 4). Since significantly increased IL-1β protein was detected in the cell culture medium after 24 h of PM2.5 treatment (Fig. 6c), and previous studies demonstrated that IL-1β can induce MMP-9 upregulation [30,31,32,33], a time point of 24 h was selected for MMPs assessment. When the cells were pretreated with 30 mM of glucose for 18 days followed by PM2.5 exposure for 24 h, the mRNA expression level of MMP-9, but not MMP-2, was significantly enhanced (Fig. 10c, d). MMP-2 and MMP-9 protein levels were determined in the cell culture media by ELISA. The results showed that 50 μg/mL of PM2.5 exposure for 24 h caused a significant increase in MMP-9, but not MMP-2, protein level in the cell culture media, and pretreatment with high glucose enhanced this effect (Fig. 10e, f). The results of MMP-9 enzymatic activity determined by gelatin zymography assay had a similar trend as MMP-9 mRNA and protein expression (Fig. 10g, h).
The expression levels and enzymatic activities of MMP-2 and MMP-9 in MH-S cells exposed to PM2.5 with/without high glucose pretreatment. The cells were treated with 25 or 50 μg/mL of PM2.5 for 3, 6, 12, and 24 h (a, b, g) or 24 h (c-f, h) with/without 30 mM of glucose pretreatment for 18 days. The cells treated with physiological saline were used as control. a-d The mRNA expressions of MMP-2 and MMP-9 were determined by RT-qPCR and normalized to the β-actin expression in the same sample. e, f The protein levels of MMP-2 and MMP-9 in cell culture media were determined by ELISA. Data are shown as mean ± SEM (n = 3). * p < 0.05 vs. control; # p < 0.05 vs. group with the same dose of PM2.5 treatment only. g, h The enzymatic activities of MMP-2 and MMP-9 in the cell culture media were determined by gelatin zymography assay
To determine whether enhanced MMP-9 expression and enzymatic activity in alveolar macrophages exposed to PM2.5 with high glucose pretreatment was induced by enhanced IL-1β level with PM2.5 and high glucose exposure, primary alveolar macrophages isolated from NLRP3 KO and IL-1R1 KO mice were used. Knocking out of NLRP3 results in malfunction of NLRP3 inflammasome, thus preventing the cleavage of pro-IL-1β from producing mature IL-1β [52,53]. In newly diagnosed T1D patients, IL-1β is increased and likely acts as an early inflammatory signal in T1D progression [54]. In the present study, increased expression of both pro-IL-1β and cleaved IL-1β was observed in alveolar macrophages exposed to PM2.5, which was enhanced when cells were pretreated with high glucose prior to PM2.5 exposure, suggesting that individuals with diabetes may be more vulnerable to PM-induced pulmonary and systemic inflammation and other PM-related health problems.
Many factors may cause IL-1β upregulation, including activation of NLRP3 inflammasome and/or toll-like receptors (TLRs), oxidative stress, etc. [15,16,17]. NLRP3 inflammasome is a cytoplasmic multiprotein complex that is currently the most extensively studied inflammasome, and is assembled by the recruitment of adapter protein ASC and pro-caspase-1 by NLRP3 protein when cells sense intracellular danger signals [14, 15]. NLRP3 inflammasome mediates the cleavage and activation of caspase-1, which cleaves pro-IL-1β to active IL-1β [14, 15]. In this study, both mRNA and protein expression levels of NLRP3 in MH-S cells exposed to PM2.5 with/without high glucose pre-treatment were assessed. The results showed that both mRNA and protein expressions of NLRP3 were upregulated by PM2.5 exposure, with enhanced expression when cells were pre-treated with high glucose, suggesting that the activation of NLRP3 inflammasome may be involved in enhanced production of IL-1β in alveolar macrophages in a high glucose environment after PM2.5 exposure.
In addition to NLRP3 upregulation, increased mRNA expression of IL-1β and increased protein expression of pro-IL-1β were also observed in alveolar macrophages with PM2.5 exposure with/without high glucose pretreatment. NF-κB could be responsible for the upregulation of IL-1β and NLRP3 [25, 26, 28, 29]. NF-κB binding sites have been identified in the promoter regions of both human and mouse IL-1β [25,26,27] and NLRP3 [28, 29]. NF-κB signaling is involved in a large array of immune and inflammatory responses and diseases [55]. The best-studied and most important NF-κB family member is RelA (also named p65). In this study, NF-κB p65 was found to be translocated from the cytoplasm to the nucleus upon PM2.5 exposure, and this effect was enhanced when the cells were pretreated with high glucose, indicating NF-κB was involved in the upregulation of IL-1β and NLRP3 after PM2.5 exposure in the high glucose environment. Many factors including TLRs [29], oxidative stress [56, 57], pro-inflammatory cytokines such as IL-1β [58], etc. can activate NF-κB. TLR2, but not TLR4, was observed to be activated by PM2.5 exposure, but no enhanced activation of TLR2 was observed after cells were pretreated with high glucose. However, ROS was enhanced when cells were treated with PM2.5 in a high glucose environment, indicating NF-κB activation mediated by ROS, not TLRs, is responsible for enhanced PM2.5-induced upregulation of NLRP3 and IL-1β in a high glucose environment.
Oxidative stress is considered an important mechanism underlying PM-induced health effects. Increased ROS generation in cells exposed to PM and activation of ROS-responsive transcription factors such as NF-κB and AP-1, which, together with the depletion of antioxidant defenses, can lead to the release of pro-inflammatory cytokines such as IL-1β [56, 57]. Here, ROS generation in MH-S cells exposed to PM2.5 with/without high glucose pre-treatment was determined. The results showed that ROS generation was increased by PM2.5 exposure, which was enhanced when cells were in a high glucose environment. Pretreatment of alveolar macrophages with an NADPH oxidase inhibitor, DPI, inhibited PM2.5-induced ROS generation, but mitochondria superoxide specific detector, MitoSOX, failed to detect significant superoxide generation after PM2.5 exposure, suggesting that the ROS induced by PM2.5 exposure were mainly generated by NADPH oxidase rather than through the mitochondria. Moreover, pretreatment of alveolar macrophages with DPI attenuated NF-κB nuclear translocation and upregulation of NLRP3 and IL-1β induced by PM2.5 exposure in a high glucose environment, confirming that enhanced IL-1β production upon PM2.5 exposure is through NLRP3 inflammasome activation and NF-κB nuclear translocation caused by NADPH oxidase-generated ROS.
MMP-2 and MMP-9 are gelatinases, belonging to a large group of proteins called extracellular matrix metalloproteinases (MMPs), and cleave elastin, type IV collagen, and several other ECM molecules [59]. Activation of MMP-2 and/or MMP-9 has been found to play an important role in the pathogenesis of diabetic retinopathy [60, 61], nephropathy [62], neuropathy [63], vascular complications [64], skin complications [65], etc. In this study, MMP-9 expression and enzymatic activity were found to be increased upon PM2.5 exposure in mouse alveolar macrophages and this effect was enhanced in cells with high glucose pretreatment. PM2.5 exposure also caused enhanced IL-1β production in alveolar macrophages with high glucose pretreatment, but there was a delay in MMP-9 upregulation as compared to IL-1β. This raised the intriguing possibility that IL-1β might regulate MMP-9 production in alveolar macrophages. To explore this possibility, cells from NLRP3 KO and IL-1R1 KO mice were used. In NLRP3 KO mice, pro-IL-1β cannot be cleaved to form mature IL-1β [34] while IL-1R1 KO mice fail to respond to IL-1β [35]. No increased expression and enzymatic activity of MMP-9 were observed in primary alveolar macrophages obtained from both NLRP3 KO and IL-1R1 KO mice, suggesting the important role of IL-1β in the regulation of MMP-9 production in cells exposed to PM2.5 with and without high glucose pretreatment. Previous studies have demonstrated that IL-1β can induce MMP-9 upregulation in multiple cells including human alveolar epithelial carcinoma cells A549 [30], human fetal neurons [31], rat glomerular mesangial cells [32], mouse cochlear cells HEI-OC1 [33], etc. IL-1β was also able to upregulate MMP-2 expression in rat cardiac microvascular endothelial cells [66]. Although the precise mechanisms that how IL-1β regulates MMP-9 expression remain unclear, several possible pathways have been explored including signaling cascades leading to the activation of AP-1 and NF-κB [32], c-Src-dependent transactivation of EGFR/PDGFR/PI3K/Akt linking to the NF-κB pathway [30], activation of ERKs and p38 MAPK signaling pathways [32, 33], etc.
Conclusions
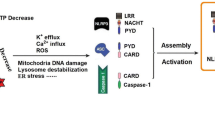
Pretreatment of mouse alveolar macrophages with high glucose enhanced PM2.5-induced production of pro-inflammatory cytokine IL-1β through activation of the NLRP3 inflammasome and increased nuclear translocation of transcription factor NF-κB due to PM2.5-induced oxidative stress, finally leading to MMP-9 upregulation (Fig. 12). This study provides a further understanding of the potential mechanisms underlying the susceptibility of individuals with diabetes to air pollution. The pro-inflammatory cytokine IL-1β may lead to acute and chronic pulmonary inflammation and contribute to other PM2.5-related health problems. Thus, the steps in the IL-1β synthesis and secretion pathway may act as potential therapeutic targets. Development of new drugs targeting the NLRP3 inflammasome, IL-1 receptor antagonists, agents that can remove IL-1β from the circulation, etc., may reduce the susceptibility of diabetics to air pollution. Antidiabetic medications that also inhibit IL-1β secretion may offer considerable therapeutic promise in regions with high PM pollution. For example, pioglitazone can reduce IL-1β secretion [67] and glyburide can inhibit the activation of the NLRP3 inflammasome [68]. In addition, to reduce PM-induced oxidative stress, a daily supplement of antioxidants such as vitamins C and E as well as fresh vegetables and fruits may also be recommended for individuals with diabetes. These findings may also inform PM regulations for susceptible populations, such as individuals with diabetes. To further confirm the susceptibility of individuals with diabetes to air pollution and the underlying mechanisms, in vivo studies involving obese or diabetic animal models may be performed.
Availability of data and materials
All data and materials are included in the manuscript.
Code availability
Not applicable.
Abbreviations
- cDNA:
-
Complementary DNA
- DM:
-
Diabetes mellitus
- DPI:
-
Diphenyleneiodonium chloride
- H2DCF-DA:
-
2′, 7′-Dichlorodihydrofluorescein diacetate
- IL-1β:
-
Interleukin 1 beta
- IL-1R1:
-
Interleukin 1 receptor, type I
- KO:
-
Knock out
- MMP-2:
-
Matrix metalloproteinase-2
- MMP-9:
-
Matrix metalloproteinase-9
- NF-κB:
-
Nuclear factor-kappa B
- NLRP3:
-
NOD-, LRR- and pyrin domain-containing protein 3
- PM2.5 :
-
Ambient fine particulate matter (diameter less than 2.5 µM)
- PVDF:
-
Polyvinylidene difluoride
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- TIMP-1:
-
Tissue inhibitor of metalloproteinases 1
- TIMP-2:
-
Tissue inhibitor of metalloproteinases 2
- TLRs:
-
Toll-like receptors
References
U.S. Environmental Protection Agency: Particulate Matter (PM) Basics. (2022).
Hayes RB, Lim C, Zhang Y, Cromar K, Shao Y, Reynolds HR, et al. PM2.5 air pollution and cause-specific cardiovascular disease mortality. Int J Epidemiol. 2020;49(1):25–35. https://doi.org/10.1093/ije/dyz114.
Lux H, Baur X, Budnik LT, Heutelbeck A, Teixeira JP, Neumann E, et al. Outdoor air pollution from industrial chemicals causing new onset of asthma or COPD: a systematic review protocol. J Occup Med Toxicol. 2020;15(1):38. https://doi.org/10.1186/s12995-020-00289-6.
Pope CA 3rd, Coleman N, Pond ZA, Burnett RT. Fine particulate air pollution and human mortality: 25+ years of cohort studies. Environ Res. 2020;183:108924. https://doi.org/10.1016/j.envres.2019.108924.
Abed Al Ahad M, Sullivan F, Demsar U, Melhem M, Kulu H. The effect of air-pollution and weather exposure on mortality and hospital admission and implications for further research: A systematic sco** review. PLoS ONE. 2020;15(10):e0241415. https://doi.org/10.1371/journal.pone.0241415.
Rush B, Wiskar K, Fruhstorfer C, Celi LA, Walley KR. The impact of chronic ozone and particulate air pollution on mortality in patients with sepsis across the United States. J Intensive Care Med. 2020;35(10):1002–7. https://doi.org/10.1177/0885066618804497.
Tarantino G, Capone D, Finelli C. Exposure to ambient air particulate matter and non-alcoholic fatty liver disease. World J Gastroenterol. 2013;19(25):3951–6. https://doi.org/10.3748/wjg.v19.i25.3951.
Wang J, Li Y, Zhao P, Tian Y, Liu X, He H, et al. Exposure to Air Pollution Exacerbates Inflammation in Rats with Preexisting COPD. Mediators Inflamm. 2020;2020:4260204. https://doi.org/10.1155/2020/4260204.
Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH, et al. Ambient air pollution and diabetes: A systematic review and meta-analysis. Environ Res. 2020;180:108817. https://doi.org/10.1016/j.envres.2019.108817.
Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, Steiropoulos P, et al. Impact of Air Pollution on Asthma Outcomes. Int J Environ Res Public Health. 2020. https://doi.org/10.3390/ijerph17176212.
Khateeb J, Fuchs E, Khamaisi M. Diabetes and lung disease: a neglected Relationship. Rev Diabet Stud. 2019;15:1–15. https://doi.org/10.1900/RDS.2019.15.1.
Vogel CF, Sciullo E, Wong P, Kuzmicky P, Kado N, Matsumura F. Induction of proinflammatory cytokines and C-reactive protein in human macrophage cell line U937 exposed to air pollution particulates. Environ Health Perspect. 2005;113(11):1536–41. https://doi.org/10.1289/ehp.8094.
Abbate A, Toldo S, Marchetti C, Kron J, Van Tassell BW, Dinarello CA. Interleukin-1 and the Inflammasome as Therapeutic Targets in Cardiovascular Disease. Circ Res. 2020;126(9):1260–80. https://doi.org/10.1161/CIRCRESAHA.120.315937.
Chan AH, Schroder K. Inflammasome signaling and regulation of interleukin-1 family cytokines. J Exp Med. 2020. https://doi.org/10.1084/jem.20190314.
Gora IM, Ciechanowska A, Ladyzynski P. NLRP3 inflammasome at the interface of inflammation, endothelial dysfunction, and type 2 diabetes. Cells. 2021. https://doi.org/10.3390/cells10020314.
Grishman EK, White PC, Savani RC. Toll-like receptors, the NLRP3 inflammasome, and interleukin-1beta in the development and progression of type 1 diabetes. Pediatr Res. 2012;71(6):626–32. https://doi.org/10.1038/pr.2012.24.
Rabolli V, Lison D, Huaux F. The complex cascade of cellular events governing inflammasome activation and IL-1beta processing in response to inhaled particles. Part Fibre Toxicol. 2016;13(1):40. https://doi.org/10.1186/s12989-016-0150-8.
Mo Y, Zhang Y, Wan R, Jiang M, Xu Y, Zhang Q. miR-21 mediates nickel nanoparticle-induced pulmonary injury and fibrosis. Nanotoxicology. 2020;14(9):1175–97. https://doi.org/10.1080/17435390.2020.1808727.
Mo Y, Zhang Y, Mo L, Wan R, Jiang M, Zhang Q. The role of miR-21 in nickel nanoparticle-induced MMP-2 and MMP-9 production in mouse primary monocytes: In vitro and in vivo studies. Environ Pollut. 2020;267:115597. https://doi.org/10.1016/j.envpol.2020.115597.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25(4):402–8. https://doi.org/10.1006/meth.2001.1262.
Mo Y, Zhang Y, Zhang Y, Yuan J, Mo L, Zhang Q. Nickel nanoparticle-induced cell transformation: involvement of DNA damage and DNA repair defect through HIF-1alpha/miR-210/Rad52 pathway. J Nanobiotechnology. 2021;19(1):370. https://doi.org/10.1186/s12951-021-01117-7.
Zhang Y, Wan R, Zhang Q, Mo Y. Application of Gelatin Zymography in Nanotoxicity Research. Methods Mol Biol. 2019;1894:133–43. https://doi.org/10.1007/978-1-4939-8916-4_8.
Mo Y, Zhang Y, Zhang Q. Evaluation of pulmonary toxicity of nanoparticles by bronchoalveolar lavage. Methods Mol Biol. 2019;1894:313–22. https://doi.org/10.1007/978-1-4939-8916-4_18.
Mo Y, Jiang M, Zhang Y, Wan R, Li J, Zhong CJ, et al. Comparative mouse lung injury by nickel nanoparticles with differential surface modification. J Nanobiotechnology. 2019;17(1):2. https://doi.org/10.1186/s12951-018-0436-0.
Hiscott J, Marois J, Garoufalis J, D’Addario M, Roulston A, Kwan I, et al. Characterization of a functional NF-kappa B site in the human interleukin 1 beta promoter: evidence for a positive autoregulatory loop. Mol Cell Biol. 1993;13(10):6231–40. https://doi.org/10.1128/mcb.13.10.6231-6240.1993.
Chan C, Li L, McCall CE, Yoza BK. Endotoxin tolerance disrupts chromatin remodeling and NF-kappaB transactivation at the IL-1beta promoter. J Immunol. 2005;175(1):461–8. https://doi.org/10.4049/jimmunol.175.1.461.
Zhang Y, Saccani S, Shin H, Nikolajczyk BS. Dynamic protein associations define two phases of IL-1beta transcriptional activation. J Immunol. 2008;181(1):503–12. https://doi.org/10.4049/jimmunol.181.1.503.
Boaru SG, Borkham-Kamphorst E, Van de Leur E, Lehnen E, Liedtke C, Weiskirchen R. NLRP3 inflammasome expression is driven by NF-kappaB in cultured hepatocytes. Biochem Biophys Res Commun. 2015;458(3):700–6. https://doi.org/10.1016/j.bbrc.2015.02.029.
Qiao Y, Wang P, Qi J, Zhang L, Gao C. TLR-induced NF-kappaB activation regulates NLRP3 expression in murine macrophages. FEBS Lett. 2012;586(7):1022–6. https://doi.org/10.1016/j.febslet.2012.02.045.
Cheng CY, Kuo CT, Lin CC, Hsieh HL, Yang CM. IL-1beta induces expression of matrix metalloproteinase-9 and cell migration via a c-Src-dependent, growth factor receptor transactivation in A549 cells. Br J Pharmacol. 2010;160(7):1595–610. https://doi.org/10.1111/j.1476-5381.2010.00858.x.
Vecil GG, Larsen PH, Corley SM, Herx LM, Besson A, Goodyer CG, et al. Interleukin-1 is a key regulator of matrix metalloproteinase-9 expression in human neurons in culture and following mouse brain trauma in vivo. J Neurosci Res. 2000;61(2):212–24.
Eberhardt W, Huwiler A, Beck KF, Walpen S, Pfeilschifter J. Amplification of IL-1 beta-induced matrix metalloproteinase-9 expression by superoxide in rat glomerular mesangial cells is mediated by increased activities of NF-kappa B and activating protein-1 and involves activation of the mitogen-activated protein kinase pathways. J Immunol. 2000;165(10):5788–97. https://doi.org/10.4049/jimmunol.165.10.5788.
Nam SI, Kwon TK. Dexamethasone inhibits interleukin-1beta-induced matrix metalloproteinase-9 expression in cochlear cells. Clin Exp Otorhinolaryngol. 2014;7(3):175–80. https://doi.org/10.3342/ceo.2014.7.3.175.
Kovarova M, Hesker PR, Jania L, Nguyen M, Snouwaert JN, **ang Z, et al. NLRP1-dependent pyroptosis leads to acute lung injury and morbidity in mice. J Immunol. 2012;189(4):2006–16. https://doi.org/10.4049/jimmunol.1201065.
Glaccum MB, Stocking KL, Charrier K, Smith JL, Willis CR, Maliszewski C, et al. Phenotypic and functional characterization of mice that lack the type I receptor for IL-1. J Immunol. 1997;159(7):3364–71.
U.S. Environmental Protection Agency: National Ambient Air Quality Standards (NAAQS) for PM. (2021).
IQAir: 2021 World Air Quality Report. (2021).
Fajardo RJ, Karim L, Calley VI, Bouxsein ML. A review of rodent models of type 2 diabetic skeletal fragility. J Bone Miner Res. 2014;29(5):1025–40. https://doi.org/10.1002/jbmr.2210.
Baker EH, Clark N, Brennan AL, Fisher DA, Gyi KM, Hodson ME, et al. Hyperglycemia and cystic fibrosis alter respiratory fluid glucose concentrations estimated by breath condensate analysis. J Appl Physiol. 2007;102(5):1969–75. https://doi.org/10.1152/japplphysiol.01425.2006.
Astrand A, Wingren C, Benjamin A, Tregoning JS, Garnett JP, Groves H, et al. Dapagliflozin-lowered blood glucose reduces respiratory Pseudomonas aeruginosa infection in diabetic mice. Br J Pharmacol. 2017;174(9):836–47. https://doi.org/10.1111/bph.13741.
Hunt WR, Zughaier SM, Guentert DE, Shenep MA, Koval M, McCarty NA, et al. Hyperglycemia impedes lung bacterial clearance in a murine model of cystic fibrosis-related diabetes. Am J Physiol Lung Cell Mol Physiol. 2014;306(1):L43–9. https://doi.org/10.1152/ajplung.00224.2013.
Gill SK, Hui K, Farne H, Garnett JP, Baines DL, Moore LS, et al. Increased airway glucose increases airway bacterial load in hyperglycaemia. Sci Rep. 2016;6:27636. https://doi.org/10.1038/srep27636.
Oliveira TL, Candeia-Medeiros N, Cavalcante-Araujo PM, Melo IS, Favaro-Pipi E, Fatima LA, et al. SGLT1 activity in lung alveolar cells of diabetic rats modulates airway surface liquid glucose concentration and bacterial proliferation. Sci Rep. 2016;6:21752. https://doi.org/10.1038/srep21752.
Evren E, Ringqvist E, Willinger T. Origin and ontogeny of lung macrophages: from mice to humans. Immunology. 2020;160(2):126–38. https://doi.org/10.1111/imm.13154.
Machiels B, Dourcy M, **ao X, Javaux J, Mesnil C, Sabatel C, et al. A gammaherpesvirus provides protection against allergic asthma by inducing the replacement of resident alveolar macrophages with regulatory monocytes. Nat Immunol. 2017;18(12):1310–20. https://doi.org/10.1038/ni.3857.
Brunekreef B, Holgate ST. Air pollution and health. Lancet. 2002;360(9341):1233–42. https://doi.org/10.1016/S0140-6736(02)11274-8.
Mo Y, Wan R, Chien S, Tollerud DJ, Zhang Q. Activation of endothelial cells after exposure to ambient ultrafine particles: the role of NADPH oxidase. Toxicol Appl Pharmacol. 2009;236(2):183–93. https://doi.org/10.1016/j.taap.2009.01.017.
Dasu MR, Devaraj S, Jialal I. High glucose induces IL-1beta expression in human monocytes: mechanistic insights. Am J Physiol Endocrinol Metab. 2007;293(1):E337–46. https://doi.org/10.1152/ajpendo.00718.2006.
Cornut M, Bourdonnay E, Henry T. Transcriptional Regulation of Inflammasomes. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21218087.
Donath MY, Boni-Schnetzler M. IL-1beta activation as a response to metabolic disturbances. Cell Metab. 2010;12(5):427–8. https://doi.org/10.1016/j.cmet.2010.10.002.
Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nat Rev Immunol. 2011;11(2):98–107. https://doi.org/10.1038/nri2925.
Pradhan AD, Manson JE, Rifai N, Buring JE, Ridker PM. C-reactive protein, interleukin 6, and risk of develo** type 2 diabetes mellitus. JAMA. 2001;286(3):327–34. https://doi.org/10.1001/jama.286.3.327.
Spranger J, Kroke A, Mohlig M, Hoffmann K, Bergmann MM, Ristow M, et al. Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam Study. Diabetes. 2003;52(3):812–7. https://doi.org/10.2337/diabetes.52.3.812.
Kaizer EC, Glaser CL, Chaussabel D, Banchereau J, Pascual V, White PC. Gene expression in peripheral blood mononuclear cells from children with diabetes. J Clin Endocrinol Metab. 2007;92(9):3705–11. https://doi.org/10.1210/jc.2007-0979.
Liu T, Zhang L, Joo D, Sun SC. NF-kappaB signaling in inflammation. Signal Transduct Target Ther. 2017. https://doi.org/10.1038/sigtrans.2017.23.
Donaldson K, Stone V, Borm PJ, Jimenez LA, Gilmour PS, Schins RP, et al. Oxidative stress and calcium signaling in the adverse effects of environmental particles (PM10). Free Radic Biol Med. 2003;34(11):1369–82.
Miller MR. The role of oxidative stress in the cardiovascular actions of particulate air pollution. Biochem Soc Trans. 2014;42(4):1006–11. https://doi.org/10.1042/BST20140090.
El Kasmi KC, Vue PM, Anderson AL, Devereaux MW, Ghosh S, Balasubramaniyan N, et al. Macrophage-derived IL-1beta/NF-kappaB signaling mediates parenteral nutrition-associated cholestasis. Nat Commun. 2018;9(1):1393. https://doi.org/10.1038/s41467-018-03764-1.
Nagase H, Visse R, Murphy G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc Res. 2006;69(3):562–73. https://doi.org/10.1016/j.cardiores.2005.12.002.
Kowluru RA. Role of matrix metalloproteinase-9 in the development of diabetic retinopathy and its regulation by H-Ras. Invest Ophthalmol Vis Sci. 2010;51(8):4320–6. https://doi.org/10.1167/iovs.09-4851.
Unal A, Baykal O, Ozturk N. Comparison of matrix metalloproteinase 9 and 14 levels in vitreous samples in diabetic and non-diabetic patients: a case control study. Int J Retina Vitreous. 2022;8(1):44. https://doi.org/10.1186/s40942-022-00394-0.
Li SY, Huang PH, Yang AH, Tarng DC, Yang WC, Lin CC, et al. Matrix metalloproteinase-9 deficiency attenuates diabetic nephropathy by modulation of podocyte functions and dedifferentiation. Kidney Int. 2014;86(2):358–69. https://doi.org/10.1038/ki.2014.67.
Deng X, Ma P, Wu M, Liao H, Song XJ. Role of matrix metalloproteinases in myelin abnormalities and mechanical allodynia in rodents with diabetic neuropathy. Aging Dis. 2021;12(7):1808–20. https://doi.org/10.14336/AD.2021.0126.
Uemura S, Matsushita H, Li W, Glassford AJ, Asagami T, Lee KH, et al. Diabetes mellitus enhances vascular matrix metalloproteinase activity: role of oxidative stress. Circ Res. 2001;88(12):1291–8. https://doi.org/10.1161/hh1201.092042.
Zhou P, Yang C, Zhang S, Ke ZX, Chen DX, Li YQ, et al. The imbalance of MMP-2/TIMP-2 and MMP-9/TIMP-1 contributes to collagen deposition disorder in diabetic non-injured skin. Front Endocrinol (Lausanne). 2021;12:734485. https://doi.org/10.3389/fendo.2021.734485.
Mountain DJ, Singh M, Menon B, Singh K. Interleukin-1beta increases expression and activity of matrix metalloproteinase-2 in cardiac microvascular endothelial cells: role of PKCalpha/beta1 and MAPKs. Am J Physiol Cell Physiol. 2007;292(2):C867–75. https://doi.org/10.1152/ajpcell.00161.2006.
Glatz T, Stock I, Nguyen-Ngoc M, Gohlke P, Herdegen T, Culman J, et al. Peroxisome-proliferator-activated receptors gamma and peroxisome-proliferator-activated receptors beta/delta and the regulation of interleukin 1 receptor antagonist expression by pioglitazone in ischaemic brain. J Hypertens. 2010;28(7):1488–97. https://doi.org/10.1097/HJH.0b013e3283396e4e.
Lamkanfi M, Mueller JL, Vitari AC, Misaghi S, Fedorova A, Deshayes K, et al. Glyburide inhibits the Cryopyrin/Nalp3 inflammasome. J Cell Biol. 2009;187(1):61–70. https://doi.org/10.1083/jcb.200903124.
Acknowledgements
Not applicable.
Funding
This work was partly supported by NIH (ES023693, ES028911, and HL147856), KSEF-148-RED-502–16-381, and Kentucky Lung Cancer Research Program to Dr. Qunwei Zhang. This work was also partly supported by P30ES030283 from the National Institute for Environmental Health Sciences.
Author information
Authors and Affiliations
Contributions
YM, LM, YZ, YBZ, and JY designed and performed the experiments, analyzed the data, and/or interpreted the results of the experiments. QZ conceived and supervised the study. The manuscript was written by YM, LM, and YZ and revised critically by QZ. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocols and the use of animals were approved by and in accordance with the University of Louisville Animal Care and Use Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Cytotoxicity of PM2.5 on MH-S cells. The cells were treated with PM2.5 for 24 h. The cells treated with physiological saline were used as control. Cytotoxicity was determined by alamarBlueTM assay (Invitrogen). Data are shown as mean ± SEM (n = 6). * p < 0.05 vs. control.
Additional file 2
: Enhanced expression of IL-1β and NLRP3 in primary mouse alveolar macrophages exposed to PM2.5 at high glucose setting. Primary alveolar macrophages were obtained from C57BL/6J mice by bronchoalveolar lavage (BAL) and pretreated with 30 mM of glucose for 24 h, followed by treatment with 50 μg/mL of PM2.5 for 3 h. The cells treated with physiological saline were used as control. The mRNA expressions of IL-1β and NLRP3 were determined by RT-qPCR and normalized to the β-actin expression in the same sample. Data are shown as mean ± SEM of three independent experiments. * p < 0.05 vs. control; # p < 0.05 vs. group with PM2.5 treatment only.
Additional file 3
: Mitochondrial superoxide was not increased in MH-S cells exposed to PM2.5. The cells were pretreated with 5 µM of MitoSOXTM for 1 h, followed by treatment with PM2.5 for 12 h. The cells treated with physiological saline were used as control. Data are shown as mean ± SEM (n = 3).
Additional file 4
: The expression of TIMP-1 and TIMP-2 in MH-S cells exposed to PM2.5. The cells were treated with 25 or 50 µg/mL of PM2.5 for 3, 6, 12, and 24 h. The cells treated with physiological saline were used as control. The mRNA expression of TIMP-1 or TIMP-2 was determined by RT-qPCR and normalized to the β-actin expression in the same sample. Data are shown as mean ± SEM (n = 3).
Additional file 5
: Uncropped versions of Western blots.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mo, Y., Mo, L., Zhang, Y. et al. High glucose enhances the activation of NLRP3 inflammasome by ambient fine particulate matter in alveolar macrophages. Part Fibre Toxicol 20, 41 (2023). https://doi.org/10.1186/s12989-023-00552-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12989-023-00552-8