Abstract
Background
Rehabilitation in iNPH is suggested to be an important factor to improve patients’ functions but there are lack of clinical trials evaluating the effect of rehabilitation interventions after shunt surgery in iNPH. The objective of this study was to evaluate the effect of a physical exercise programme and goal attainment for patients with idiopathic normal pressure hydrocephalus (iNPH) after surgery compared to a control group.
Methods
This was a dual centre randomised controlled trial with assessor blinding, intention-to-treat (ITT) and per protocol (PP) analysis. Individuals diagnosed with iNPH scheduled to undergo shunt surgery at the Linkö** University Hospital in Linkö** and Sahlgrenska University Hospital in Gothenburg, Sweden were consecutively eligible for inclusion. Inclusion was conducted between January 2016 and June 2018. The patients were randomised 1:1 using sequentially numbered sealed envelopes to receive either written exercise information (control group) or written information and an additional supervised high-intensity, functional exercise programme (HIFE) executed twice weekly over 12 weeks (exercise group). Preoperatively, the patients set individual goals. The primary outcome was change from baseline in the total iNPH scale score at the post-intervention follow-up. Secondary outcomes were goal attainment, and change in the separate scores of gait, balance, neuropsychology and continence and in the total score after 6 months.
Results
In total, 127 participants were randomised to the exercise group (n = 62) and to the control group (n = 65). In the ITT population (exercise group, n = 50; control group, n = 59), there were no between-group differences in the primary outcome, but the attrition rate in the exercise group was high. The exercise group improved more than the control group in the balance domain scores after 6 months. Post-intervention, the PP exercise population achieved their set goals to a greater extent than the controls.
Conclusions
An additional effect of the 12-week HIFE-programme on the overall improvement according to the iNPH-scale after shunt surgery in iNPH was not shown. This could be due to high attrition rate. However, the long-term effect on balance and higher goal achievement indicate beneficial influences of supervised physical exercise.
Trial registration clinicaltrials.gov, NCT02659111. Registered 20 January 2016, https://clinicaltrials.gov/ct2/show/NCT02659111
Similar content being viewed by others
Introduction
The core clinical symptoms in idiopathic normal pressure hydrocephalus (iNPH) are impaired gait in combination with a disturbed balance [1,2,3] often in conjunction with cognitive impairment and incontinence [4]. The iNPH scale is a calibrated, norm-based grading scale assessing postoperative outcome in iNPH and previously used in the European multi-centre study [5]. The scale covers four symptom domains and a total score is calculated [6]. Approximately 80% of the patients are reported to benefit from shunt surgery [5, 7]. However, patients with iNPH are more sedentary in comparison with healthy controls of the same age. Despite the alleviation of symptoms, the patients’ overall physical activity does not increase after surgery [8].
In Parkinson’s disease with a symptomatology similar to iNPH, physical exercise is an essential part of the treatment [9, 10]. Goal-oriented aerobic exercise has been suggested to promote neuroplasticity, motor and cognitive improvements [11]. Exercise programmes lasting for more than 12 weeks have long-term effects [12]. Rehabilitation in iNPH is emphasised to be an important factor to improve patients’ functions [13, 14]. A recently published non-randomised clinical trial evaluating home exercise in iNPH concluded that home exercise was easy to implement and accepted by the patients [15]. However, no randomised clinical trial has explored the effectiveness of rehabilitation in iNPH.
The aim of this study was to evaluate the effect on outcome and goal achievement of an added physical exercise programme for patients with iNPH after shunt surgery, compared to a control group of iNPH patients. We hypothesised that the high-intensity functional exercise programme (HIFE) [16] would have positive effects on the main symptom domains in iNPH evaluated with the iNPH scale [6].
Methods
Participants
Consecutive patients diagnosed with iNPH according to the international guidelines [4] and waiting for shunt surgery were eligible for inclusion. Exclusion criteria were Mini Mental State Examination (MMSE) [17] < 16, inability to walk with or without walking aids for > 10 m or suffering from other diseases making intensive exercise impossible. After the decision on surgery, eligible patients were included and randomised. All patients had a ventriculo-peritoneal shunt with either a Strata™ Valve, n = 71 (Medtronic PS Medical, Santa Barbara, USA), a Codman® Medos® Hakim Valve, n = 49, or a Codman® Certas® Plus, n = 7 (Integra LifeSciences Corporation). Participants were recruited from two Swedish Hydrocephalus centres at Linkö** University hospital (Linkö**) and Sahlgrenska University hospital (Gothenburg).
The study conforms with Declaration of Helsinki guidelines and the medical ethical committee of Linkö** approved the study, Approval Number: 2015/250-31. The study protocol was published in advance at clinicaltrials.gov, Id: NCT02659111. Eligible patients received oral and written information and gave written informed consent of acceptance.
Randomisation and blinding
One person at each centre, neither participating in the assessments nor in the data analysis, randomly assigned eligible patients 1:1 using sequentially sealed envelopes, to the added intervention (exercise group) or to usual care (control group) without stratification. The sealed envelopes were randomly computer generated and the sequential management ensured the randomisation. The assessors at the two centres were blinded after assignment to the interventions and in order to keep the randomisation, the patients were asked to keep their intervention confidential. The randomisation key was opened after the last six-month follow-up.
Intervention
In the usual care routine both groups received the same written and oral information about physical activity and eight standardised low-intensity home-based exercises (Additional File 1). All participants in both groups set individual goals, comprising concrete descriptions of what they were ho** to accomplish following treatment, such as being able to walk a specified distance, e.g. to the supermarket. The goals were set with a physiotherapist (in Gothenburg) or an occupational therapist (in Linkö**), in conjunction with hospital visits for preoperative assessments.
Following surgery, the exercise group underwent an individual high-intensity functional exercise programme, the HIFE programme(™) [16, 18] for one hour, twice a week, for 12 weeks. The HIFE programme is a battery of functional weight-bearing exercises focusing on balance and gait. The exercises are based on everyday movements, e.g. standing up from a sitting position or walking over obstacles performed at high physical intensity. In order to increase the effort during progress, a weight belt is used. The programme is described in detail elsewhere [18]. After the 12-week intervention period the patients were motivated to continue with the physical activity.
The HIFE programme was performed under the supervision of local physiotherapists in outpatient clinics. The supervising physiotherapists discussed the patients’ goal settings and encouraged activity. A coordinator from one of the centres contacted the patient and the local physiotherapist to initiate the intervention. A standardised exercise manual [18], a weight belt and a protocol were sent to the physiotherapist and the coordinator maintained contact with the physiotherapist during the intervention.
Outcome measures
The follow-up occasions were after the 12-week intervention and 6 months postoperatively. The iNPH scale introduced by Hellström et al. [6] consists of four domains; gait, balance, neuropsychology and continence. Different ordinal scales and continuous measures are used to quantify symptoms in each domain and raw scores are converted to a min–max range from 0 to 100 for all domains separately as well as for the total scale (Additional File 2). The primary efficacy variable was change in the total iNPH scale score from baseline to the follow-up at the end of intervention. Secondary efficacy variables were changes in the four separate domain scores and goal attainment at the end of the intervention and at the six-month follow-up and change in the total iNPH scale score at the six-month follow-up.
To assess goal attainment, we used a modified version of the goal attainment scaling (GAS) [19]. In the analysis we created a simplified dichotomous scale: 0, 1 or 2 = goal is achieved or exceeded, − 1 or − 2 = goal is not achieved. The patients answered the question: “What would you like to achieve after the shunt surgery?” To make the desired goal evaluable, the first question was followed by questions to specify the goal e.g. walking distance and/or frequency.
In the preparing study period, the research group met repeatedly in order to strengthen the reliability of the assessments, and the occupational therapist and the physiotherapists from the two centres co-evaluated a pilot patient.
Statistical analysis
A sample size analysis according to the score of the total iNPH scale was performed prior to the study start. We assumed that we would find a difference in improvement of five points, with an expected improvement in the control group of 16 points and a hypothesised improvement in the exercise group of 21 points, with the same SD in both groups of 10 points and a significance level of 5%. With 80% power and a two-sided T-test/Fisher’s non-parametric permutation test, 63 participants were needed in each group.
According to the statistical analysis plan, primary and secondary analyses were carried out with the intention-to-treat (ITT) population defined as all randomly assigned patients with at least one follow-up assessment. Missing data were not replaced. A complementary analysis was performed on the per protocol (PP) population. To be included in the PP population the participants in both groups must have completed all the follow-up assessments and the participants in the exercise group attended at least 18 of the 24 intervention sessions within 4 months postoperatively.
For comparison within groups, Fisher’s non-parametric permutation test for matched pairs was used. The confidence interval for dichotomous variables was the unconditional exact confidence limits. If no exact limits could be computed, the asymptotic Wald confidence limits with continuity correction were calculated instead. The confidence interval for the mean difference between groups was based on Fisher’s non-parametric permutation test. For comparison between groups, Fisher’s non-parametric permutation test was used for continuous variables, Fisher’s exact test for dichotomous variables, and a Chi-square test for non-ordered categorical variables. The main results are presented as the mean difference between the two randomised groups with 95% CI. All statistical tests were two-tailed and conducted at the 0.05 significance level.
For variables with significant differences at baseline, a mixed model was used with the explanatory variables; baseline variable, treatment group and the interaction between them. For each model, the F test was used to test the significance of interaction between a baseline variable and treatment group.
Exploratory interaction analyses between treatment group and baseline variables were performed for primary efficacy variables and for selected secondary variables. Baseline variables with interaction p < 0.10 were further investigated with sub-group analyses. A professional statistician conducted the statistical analyses with SAS® v9.2 (Cary, NC).
Results
Participant’s flow and dropouts
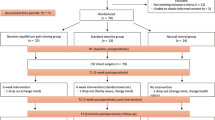
Participants were recruited from January 2016 until June 2018 and the last six-month follow-up was completed in May 2019. The inclusion stopped when the calculated sample size was achieved and 131 patients were allocated for randomisation. Four patients were excluded because of incorrect randomisation: two were diagnosed with secondary NPH and two did not undergo surgery. Of the remaining 127 participants, 62 were randomised to the exercise group and 65 to the control group.
Fifty individuals in the exercise group and 59 in the control group were available for the ITT follow-up analysis at the end of the intervention. Twelve participants in the exercise group were lost to the follow-up assessment; two died due to a subdural haematoma, one moved abroad, four had subdural haematomas treated with an elevated valve opening pressure setting, one had a distal shunt catheter dysfunction, one had a shunt infection and three participants withdrew their consent. In the control group, six participants were lost at the end of intervention follow-up; one died due to cardiac arrest approximately 3 months after surgery, four had subdural haematomas treated with an elevated valve opening pressure, and one had an intra-cerebral haemorrhage.
Twenty-eight participants in the exercise group and 58 in the control group were available for the PP analysis at the end of the intervention. In addition to the dropouts in the ITT population, four participants declined to participate in the intervention or withdrew consent, nine could not start the intervention due to logistic reasons and nine participants had fewer than 18 intervention sessions. In the control group, one participant was lost due to headache caused by shunt over-drainage.
At the six-month follow-up, 43 participants in the exercise group and 51 in the control group were available for the ITT analysis and 27 participants in the exercise group and 50 in the control group for the PP analysis (Fig. 1). If it was necessary to confirm a working shunt at the follow-up, radiological control followed by either CSF-dynamic testing or radionuclide shuntography was performed.
CONSORT flowchart of included patients in the intention-to-treat (ITT) and per protocol (PP) analyses. ITT was defined as all randomised participants with at least one follow-up assessment. PP was defined as all randomised participants with complete follow-up assessments and in the exercise group at least 18 exercise sessions
Background characteristics
The background characteristics and medical history of the ITT population are presented in Table 1. All characteristics were balanced except for age, which was higher in the control group. The same unbalanced age was seen in the PP population. There were no interaction effects of age on the primary or the secondary variables in the iNPH scale.
Effects of intervention
No harms or negative effects because of the intervention were reported.
Change in iNPH scale score
At the post-intervention follow-up, 88/127 patients (80.7%) improved ≥ 5 points on the total iNPH scale score. Compared to baseline, both the exercise group and the control group improved at the post-intervention follow-up and after 6 months. There were no between-group differences regarding change in the total iNPH scale scores from baseline at any of the follow-up sessions. In the secondary ITT analysis of each iNPH scale domain, the exercise group had higher balance domain scores than the control group at 6 months. For all other domains there were no between-group differences, both the exercise group and the control group significantly improved in all separate domains compared to baseline at the two follow-up sessions (Fig. 2, Additional File 3).
The total iNPH scale score and the separate domain scores (0–100) at baseline, at the post-intervention follow-up and at the 6-month follow-up in the intention-to-treat population (exercise group n = 50; control group n = 59). Line in box is median and the marker shows the mean. All values at the post-intervention follow-up and the six-month follow-up in both exercise group and control group are significantly changed from baseline (p ≤ 0.05). Significant differences between the groups are presented with p-value in the figure
In an exploratory interaction analysis, sex appeared to be an interacting factor and a sub-group analysis by sex was conducted. At baseline, females had lower gait domain scores than males but without significant differences (females n = 53; median 43.7, min–max 9.7–100; mean 46.0, SD 21.5 vs males n = 74, median 54.7, min–max 9.7–100; mean 55.6, SD 24.5); p = 0.06. At the post-intervention follow-up females in the exercise group had greater improvements in the gait domain scores from baseline (n = 20; median 25, min–max 0–54.7; mean 24.7, SD 13.6) compared to females in the control group (n = 24; median 10.8, min–max – 10 to 48.3; mean 14.6, SD 15.4), p = 0.026; mean 10.2 (95% CI 1.3; 19.3).
Similar results for the total iNPH scale score were seen in the PP population as in the ITT population. For the secondary outcome measures there were no between-group differences in changes from baseline for any of the separate iNPH scale domains at the post-intervention follow-up. After 6 months, the exercise group had improved more than the control group in the balance domain scores compared to baseline but showed similar improvements in the other domains (Fig. 3, Additional File 4).
The total iNPH scale score and the separate domain scores (0–100) at baseline, at the post-intervention follow-up and at the 6-month follow-up in the per protocol population (exercise group n = 28; control group n = 58). Line in box is median and the marker shows the mean. All values at the post-intervention follow-up and at the six-month follow-up in both exercise group and control group are significantly changed from baseline (p ≤ 0.05). Significant differences between the groups are presented with p-value in the figure
Intervention effect on GAS
In the ITT population, the proportions of individuals with achieved goals were equal in the exercise group compared to the control group at both the post-intervention follow-up (29 of 50, 65.9% versus 26 of 59, 52.0%; p = 0.25) and at the six-month follow-up (26 of 50, 56.5% versus 27 of 59, 54.0%; p = 0.97). In the PP population the proportions of individuals with achieved goals at the post-intervention follow-up favoured the exercise group (20 of 28, 80.0% versus 26 of 58, 52.0%; p = 0.033). After 6 months, the between-group difference had disappeared and the proportions of individuals with achieved goals were similar (16 of 28, 59.3% versus 27 of 58, 54.0%; p = 0.84), (Fig. 4).
Participants with achieved goals for ITT and PP populations post-intervention and 6 months postoperatively. ITT intention-to-treat, PP per protocol. Values are presented as proportions (%). Significant difference between exercise group and control group is presented with p-value in the figure. Post-intervention follow-up (exercise group ITT n = 44, control group ITT n = 50; exercise group PP n = 25, control group PP n = 50). Six-month follow-up (exercise group ITT n = 46, control group ITT n = 50; exercise group PP n = 27, control group PP n = 50
Discussion
This randomised clinical trial evaluates the effects of physical exercise in iNPH. Our primary hypothesis that the exercise group would show greater postoperative improvement in the total iNPH scale score than the control group was not confirmed. Secondary outcome analyses showed: (1) after 6 months, the exercise group had improved more in the balance domain scores in both ITT and PP analyses; (2) at the post-intervention follow-up, the exercise PP population achieved their goals to a greater extent.
Even if we could not show an overall effect, for reasons discussed in the limitation section, the improvement in balance after 6 months is notable. The scientific evidence of the effect of balance training in iNPH is limited. In Parkinson’s disease, different interventions improve balance and reduce the number of falls up to 12 months after the end of the interventions [12]. The HIFE programme has previously been evaluated for balance with the Berg Balance Scale as an outcome measure in a population with dementia in a nursing home. In that study there was no between-group difference compared to a low-intensive control intervention at the post-intervention follow-up but long-term effects were found with between-group differences favouring the exercise group after 6 months, [20] similar to the results from our study. Gait speed was improved in the intervention group, both at the post-intervention follow-up and at the long-term follow-up [20].
We found no significant between-group differences in the gait domain scores either in the ITT or in the PP population. However, in the PP population at the six-month follow-up, the exercise group showed a larger change from baseline than the control group at trend level. Difference between groups: mean 8.1 (95% CI − 1.3; 17.5), p = 0.092).
Both the ITT exercise group and the control group increased their total iNPH scale scores from the post-intervention follow-up to the six-month follow-up. Although not significant this increase may indicate a continuing improvement over time after shunt surgery and that longer follow-up periods can be valuable when evaluating outcome in iNPH patients.
The sub-group populations stratified by sex are small, which makes the gender differences in outcome less robust. However, older females are generally less physically active than males [21]. In our study the females had lower physical function at baseline (lower iNPH scale score) even if the sex differences were not significant. This may have contributed to the more pronounced intervention effect on gait among the females. However, our findings generate important questions, e.g. whether females have a lower level of function before surgery, which has been previously reported [5] or whether females wait longer with symptoms before seeking medical advice, which delays surgery, and finally whether there are any differences in rehabilitation effects.
The higher goal attainment at the post-intervention follow-up in the PP population exercise group indicates that the HIFE intervention in combination with the supervision may have influenced the goal achievements. The lack of difference in goal attainment between the exercise group and the control group at the six-month follow-up also supports this notion. Goal setting could be managed by people with mild to moderate dementia, especially when using a structured approach [22]. Impaired memory and executive difficulties in iNPH improve after shunt surgery but are still not at the same level as in healthy individuals of the same age [23]. The cognitive decline can affect the ability to self-manage the goal activities long-term. INPH patients therefore probably need continuous encouragement and support to maintain reached goals. Patient-centred care with the approach to reach self-management is fundamental in the European physiotherapy guideline for Parkinson’s disease. The guideline emphasises education and repeated support from professionals as well as carer involvement to promote the patients’ behavioural changes [9]. We believe that these recommendations are applicable to iNPH patients.
The HIFE programme is developed and feasible for persons with dementia [16, 24]. Using the programme in nursing home residences, the attendance rate was about 75% [16, 25] and about 70% of all exercise sessions were performed at high intensity [25]. Motivation and co-existing medical conditions seemed not to influence the benefit from high-intensity exercise in persons with dementia [26]. We conducted our research in primary care with the intervention performed by local physiotherapists with the aim of reflecting a clinical routine. This may be one reason for the low adherence to exercise in this study.
Finally, in the research area of iNPH there are relatively few large prospective studies exploring the outcome after shunt surgery [27,28,29]. This study brings not only new information about the role of physical exercise in iNPH but also adds important knowledge about the outcome after a shunt operation. The iNPH scale is constructed to evaluate outcome after surgery as a total score [6] and its potential for use in a larger context is explored here. Our findings are in line with the results of the European iNPH multi-centre study with significant postoperative improvements in the total scale score as well as in all the separate domain scores [5].
Limitations
Our study has several limitations. The most severe limitation is the large dropout rate causing low adherence to the intervention, which entails loss of statistical power. This limitation probably leads to failure to identify differences in favour of intervention, as indicated by the numerical differences seen between the groups for many of the outcome measures. Future studies should be larger and focus on better adherence to exercise intervention. The intervention was performed in clinical practice by physiotherapists with variable experience and conditions that may have caused differences in supervision. There were also logistical problems for the coordinators to initiate the intervention to start in time. Additionally, shunt complications and comorbidity influenced the ability to perform the intervention. Highly supervised physical exercise clinical trials under controlled conditions often generate a higher adherence rate and optimal performance but physical exercise interventions have to be applicable in clinical practice [30]. The dropout risk is important to be aware of when studying iNPH rehabilitation in the future.
The double interventions design may have influenced the results. Both groups increased clearly in all domain scores postoperatively and the surgical effect may have covered the smaller effect from the rehabilitation intervention. Another factor to consider is that the control group may have followed the advice to exercise more than we had expected and that the difference between the groups therefore became smaller and not significant. The magnitude of exercise in the control group was unknown to us.
The primary outcome measure can be questioned. The iNPH scale is developed to evaluate the most affected symptom domains in iNPH after shunt surgery and is not validated to evaluate rehabilitation effects. The HIFE intervention is based on functional exercises of gait and balance and the lack of effects in the neuropsychology and continence domains might have been expected. Aerobic exercise at moderate intensity has been shown to have a positive effect on cognition functions in patients with mild cognitive impairment [31]. However, the HIFE programme has not been shown to have beneficial effects on cognition in individuals with dementia [32]. The individual goals in the present study were set in the enrolment process, months before the surgery. This may have influenced the effect and may have given an advantage to the exercise group overseen by the supervising physiotherapists.
Conclusions
An additional high-intensity exercise intervention did not influence the total iNPH scale scores after shunt surgery for patients with iNPH. The exercise group improved more in the balance domain scores at the long-term follow-up and reached their set goals more frequently. Our results indicate that physical exercise and goal setting can be effective for individuals with iNPH. Future studies are required to understand the effect of different interventions and the feasibility in clinical practice. Research is also required to illustrate whether there are sex differences in the iNPH condition as well as in aspects of rehabilitation.
Availability of data and materials
Anonymised source data are available on reasonable request from the corresponding author.
Abbreviations
- CI:
-
Confidence interval
- GAS:
-
Goal attainment scaling
- HIFE:
-
High-intensity functional exercise
- iNPH:
-
Idiopathic normal pressure hydrocephalus
- ITT:
-
Intention-to-treat
- MMSE:
-
Mini mental state examination
- PP:
-
Per protocol
- RCT:
-
Randomized clinical trial
- SD:
-
Standard Deviation
References
Sørensen PS, Jansen EC, Gjerris F. Motor disturbances in normal-pressure hydrocephalus. Arch Neurol. 1986;43:34.
Blomsterwall E, Bilting M, Stephensen H, Wikkelso C. Gait abnormality is not the only motor disturbance in normal pressure hydrocephalus. Scand J Rehabil Med. 1995;27:205–9.
Czerwosz L, Szczepek E, Blaszczyk J, Sokolowska B, Dmitruk K, Dudzinski K, et al. Analysis of postural sway in patients with normal pressure hydrocephalus: Effects of shunt implantation. Eur J Med Res. 2009;14(SUPPL. 4):53–8. https://doi.org/10.1186/2047-783X-14-S4-53.
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PML. INPH guidelines, part II: diagnosing idio-pathic normal-pressure hydrocephalus. Neurosurgery. 2005. https://doi.org/10.1227/01.NEU.0000168185.29659.C5.
Klinge P, Hellström P, Tans J, Wikkelsø C. One-year outcome in the European multicentre study on iNPH. Acta Neurol Scand. 2012;126:145–53. https://doi.org/10.1111/j.1600-0404.2012.01676.x.
Hellström P, Klinge P, Tans J, Wikkelsø C. A new scale for assessment of severity and outcome in iNPH. Acta Neurol Scand. 2012;126:229–37. https://doi.org/10.1111/j.1600-0404.2012.01677.x.
Toma AK, Papadopoulos MC, Stapleton S, Kitchen ND, Watkins LD. Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir (Wien). 2013. https://doi.org/10.1007/s00701-013-1835-5.
Lundin F, Ulander M, Svanborg E, Wikkelsø C, Leijon G. How active are patients with idiopathic normal pressure hydrocephalus and does activity improve after shunt surgery? A controlled actigraphic study. Clin Neurol Neurosurg. 2013;115:192–6. https://doi.org/10.1016/j.clineuro.2012.05.009.
Physiotherapy guideline—Parkinson’s–ParkinsonNet International. 2020. https://www.parkinsonnet.com/discipline/physiotherapy/. Accessed 21 Dec 2020.
Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, et al. Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD002817.pub4.
Petzinger GM, Fisher BE, McEwen S, Beeler JA, Walsh JP, Jakowec MW. Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. Lancet Neurol. 2013;12:716–26. https://doi.org/10.1016/S1474-4422(13)70123-6.
Mak MK, Wong-Yu IS, Shen X, Chung CL. Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol. 2017;13:689–703. https://doi.org/10.1038/nrneurol.2017.128.
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, et al. Guidelines for management of idiopathic normal pressure hydrocephalus : second edition. Neurol Med Chir (Tokyo). 2012;52:775–8. https://doi.org/10.2176/nmc.52.775.
Isaacs AM, Williams MA, Hamilton MG. Current update on treatment strategies for idiopathic normal pressure hydrocephalus. Curr Treat Options Neurol. 2019. https://doi.org/10.1007/s11940-019-0604-z.
Modesto PC, Pinto FCG. Home physical exercise program: analysis of the impact on the clinical evolution of patients with normal pressure hydrocephalus. Arq Neuropsiquiatr. 2019;77:860–70. https://doi.org/10.1590/0004-282X20190183.
Littbrand H, Rosendahl E, Lindelöf N, Lundin-Olsson L, Gustafson Y, Nyberg L. A high-intensity functional weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: Evaluation of the applicability with focus on cognitive function. Phys Ther. 2006;86:489–98. https://doi.org/10.1093/ptj/86.4.489.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. https://doi.org/10.1016/0022-3956(75)90026-6.
The HIFE Program—English | Fanoe–Umbraco Starter Kit. 2020. https://www.hifeprogram.se/en. Accessed 11 Nov 2020.
Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. 2009;23:362–70. https://doi.org/10.1177/0269215508101742.
Rosendahl E, Lindelöf N, Littbrand H, Yifter-Lindgren E, Lundin-Olsson L, Håglin L, et al. High-intensity functional exercise program and protein-enriched energy supplement for older persons dependent in activities of daily living: a randomised controlled trial. Aust J Physiother. 2006;52:105–13. https://doi.org/10.1016/S0004-9514(06)70045-9.
Li W, Procter-Gray E, Churchill L, Crouter SE, Kane K, Tian J, et al. Gender and age differences in levels, types and locations of physical activity among older adults living in car-dependent neighborhoods. J Frailty Aging. 2017;6:129–35. https://doi.org/10.14283/jfa.2017.15.
Dutzi I, Schwenk M, Kirchner M, Bauer JM, Hauer K. “what would you like to achieve?” Goal-setting in patients with dementia in geriatric rehabilitation. BMC Geriatr. 2019;19:280. https://doi.org/10.1186/s12877-019-1296-7.
Hellström P, Edsbagge M, Blomsterwall E, Archer T, Tisell M, Tullberg M, et al. Neuropsychological effects of shunt treatment in idiopathic normal pressure hydrosephlaus. Neurosurgery. 2008;63:527–36. https://doi.org/10.1227/01.NEU.0000325258.16934.BB.
Sondell A, Rosendahl E, Gustafson Y, Lindelöf N, Littbrand H. The Applicability of a high-intensity functional exercise program among older people with dementia living in nursing homes. J Geriatr Phys Ther. 2019;42:E16-24.
Telenius EW, Engedal K, Bergland A. Effect of a high-intensity exercise program on physical function and mental health in nursing home residents with dementia: an assessor blinded randomized controlled trial. PLoS ONE. 2015;10: e0126102. https://doi.org/10.1371/journal.pone.0126102.
Sondell A, Littbrand H, Holmberg H, Lindelöf N, Rosendahl E. Is the Effect of a high-intensity functional exercise program on functional balance influenced by applicability and motivation among older people with dementia in nursing homes? J Nutr Heal Aging. 2019;23:1011–20. https://doi.org/10.1007/s12603-019-1269-8.
Marmarou A, Young HF, Aygok GA, Sawauchi S, Tsuji O, Yamamoto T, et al. Diagnosis and management of idiopathic normal-pressure hydrocephalus: a prospective study in 151 patients. J Neurosurg. 2005;102:987–97. https://doi.org/10.3171/jns.2005.102.6.0987.
Wikkelsø C, Hellström P, Klinge PM, Tans JTJ. The European iNPH Multicentre Study on the predictive values of resistance to CSF outflow and the CSF Tap Test in patients with idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2013;84:562–8. https://doi.org/10.1136/jnnp-2012-303314.
Kazui H, Miyajima M, Mori E, Ishikawa M, Hirai O, Kuwana N, et al. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): an open-label randomised trial. Lancet Neurol. 2015;14:585–94. https://doi.org/10.1016/S1474-4422(15)00046-0.
Allen NE, Sherrington C, Suriyarachchi GD, Paul SS, Song J, Canning CG. Exercise and motor training in people with parkinson’s disease: a systematic review of participant characteristics, intervention delivery, retention rates, adherence, and adverse events in clinical trials. Parkinsons Dis. 2012. https://doi.org/10.1155/2012/854328.
Law CK, Lam FM, Chung RC, Pang MY. Physical exercise attenuates cognitive decline and reduces behavioural problems in people with mild cognitive impairment and dementia: a systematic review. J Physiother. 2020;66:9–18. https://doi.org/10.1016/j.jphys.2019.11.014.
Toots A, Littbrand H, Boström G, Hornsten C, Holmberg H, Lillemor LO, et al. Effects of exercise on cognitive function in older people with dementia: a randomized controlled trial. J Alzheimers Dis. 2017;60:323–32.
Acknowledgements
The authors thank the physiotherapists Marielle Kagre in Linkö** and Elisabeth Blomsterwall in Gothenburg who acted as study coordinators. We would also like to express our gratitude to the physiotherapists who supervised the interventions in the local outpatient clinics.
Funding
Open access funding provided by Linkö** University. The study was supported by grants from Region Östergötland, the Rune and Ulla Amlöv foundation, the Edit Jacobson foundation, the foundation Hjalmar Svenssons forskningsfond and the Swedish state under the agreement between the Swedish government and the County Councils, the ALF-agreement (#ALFGBG 720121).
Author information
Authors and Affiliations
Contributions
All authors conceptualised and designed the study. JR, MT and FL interpreted the results. JR reviewed and edited the manuscript for intellectual content. LK, MT, ÅLN, CW, MT and FL revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The medical ethical committee of Linkö** approved the study, approval number: 2015/250–31. Eligible patients received oral and written information and gave written informed consent of acceptance.
Consent for publication
Not applicable.
Competing interests
CW and MT have received honoraria from Codman Integra for lecturing. The other authors have nothing to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Home exercises.
Additional file 2:
INPH scale decription.
Additional file 3:
Changes from baseline in primary and secondary iNPH scale scores for the ITT population.
Additional file 4:
Changes from baseline in primary and secondary iNPH scale scores for the PP population.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rydja, J., Kollén, L., Hellström, P. et al. Physical exercise and goal attainment after shunt surgery in idiopathic normal pressure hydrocephalus: a randomised clinical trial. Fluids Barriers CNS 18, 51 (2021). https://doi.org/10.1186/s12987-021-00287-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12987-021-00287-8