Abstract
Background
The SII (systemic immune-inflammation index) has been extensively reported to have a prognostic value in prostate cancer (PCa), despite the unconformable results. The purpose of this meta-analysis is to quantify the effect of pretreatment SII on survival outcomes in patients with PCa.
Methods
The following databases were searched: Web of Science, Cochrane Library, PubMed, Embase, and China National Knowledge Infrastructure (CNKI). For exploration of the SII’s correlations with the overall survival (OS) and the progression-free survival/biochemical recurrence-free survival (PFS/bRFS) in PCa, the pooled hazard ratios (HRs) were assessed within 95% confidence intervals (CIs).
Results
The present meta-analysis covered 10 studies with 8133 patients. Among the PCa population, a high SII was linked significantly to poor OS (HR = 2.63, 95% CI = 1.87–3.70, p < 0.001), and worse PFS/bRFS (HR = 2.49, 95% CI = 1.30–4.77, p = 0.006). However, a high SII was not linked significantly to T stage (OR = 1.69, 95% CI = 0.86–3.33, p = 0.128), the metastasis to lymph node (OR = 1.69, 95% CI = 0.69–4.16, p = 0.251), age (OR = 1.41, 95% CI = 0.88–2.23, p = 0.150), or the Gleason score (OR = 1.32, 95% CI = 0.88–1.96, p = 0.178).
Conclusions
For the PCa sufferers, the SII might be a promising prognostic biomarker, which is applicable to the high-risk subgroup identification, and provide personalized therapeutic strategies.
Similar content being viewed by others
Background
Apart from being the 2nd commonly diagnosed carcinoma, prostate cancer (PCa) also represents the 5th leading cause of carcinoma-associated mortality among males globally [1]. Based on GLOBOCAN 2020 estimates, there were 1,414,259 new PCa cases and 375,304 PCa-associated deaths in 2020 around the world [1]. The global incidence of PCa varies more than 25-fold, with a higher prevalence in Western countries and a lower prevalence in Asian countries [2]. The last few decades have witnessed an elevation in the global PCa incidence [3]. Its prognosis is heterogeneous, according to tumor stage. Most PCa cases have localized disease, and the 5-year rate of survival is nearly 100% in these populations. However, the patients with metastatic castration-resistant PCa (mCRPC) have poor prognosis, whose median time of survival is 24 months and 5-year rate of survival 30% [4, 5]. Prognostic biomarkers are important for improving the survival outcomes of patients with PCa [6]. For example, a recent study (PRIMERA trial) including 44 patients revealed that androgen receptor (AR), prostate-specific antigen (PSA), and prostate-specific membrane antigen (PSMA) expression in circulating tumor cells (CTC)+ had no significant impact on PSA drop and survival in mCRPC patients [7]. The PRIMERA trial validated the predictive importance of CTC detection in mCRPC patients as a result [7]. Hence, identification of novel biomarkers and treatment targets is imperative, in order to enhance the prognosis for patients with PCa.
As indicated by growing evidence, the systemic inflammatory reactions are significant determinants of cancer development and survival outcomes in various cancer types [8]. Many serum inflammatory parameters, including the ratios of neutrophils/lymphocytes [9], platelets/lymphocytes [10], C-reactive proteins/albumin [11], and the SII (systemic immune-inflammation index) [12], have been reported to be effective prognostic markers in different cancer types. The SII was calculated as follows: platelet quantity × neutrophil quantity/lymphocyte quantity. Its role as a prominent prognostic biomarker has been demonstrated in numerous types of carcinomas, such as the hepatocellular [13], pancreatic [14], breast [15], and non-small cell lung [16] carcinomas. Despite the prior explorations on SII’s prognostic significance among the PCa population, unconformable results have been yielded [17,18,19,20,21,22,23,24,25,26]. High SII in PCa has been considered a valid prognostic biomarker for the poor outcome by several researchers [19, 21, 24], whereas others have denied this association [20]. Hence, the objective of the present meta-analysis is to evaluate SII’s prognostic value in PCa based on current evidence.
Materials and methods
Study guideline and ethics approval
The present meta-analysis was carried out as per the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. The PRISMA checklist was shown in supplemental file 1. This meta-analysis has been registered with INPLASY (Registration No. INPLASY2022110155) and is available from https://inplasy.com/inplasy-2022-11-0155/. Being a literature-based study in nature, ethical approval was unnecessary; moreover, no data containing individual patient information were used.
Data sources and literature search
The following electronic databases were searched thoroughly: Web of Science, Cochrane Library, PubMed, Embase, and China National Knowledge Infrastructure (CNKI). The search duration was from the databases’ inception to November 27, 2022. The search heading terms and keywords included “systemic immune-inflammation index,” “SII,” “prostate cancer,” “PCa,” “prostate carcinoma,” and “prostate neoplasm.” All searches used both subject headings of Medical Subject Headings (MeSH) terms and free test words. The detailed literature strategies for each database are shown in supplemental file 2. No language restrictions were applied. The reference lists were manually searched to find eligibility records.
Selection criteria
The inclusion criteria were identified according to the PICOS (population, intervention, comparator, outcomes, and study) criteria. The inclusion criteria were formulated as shown below:
-
(i)
P (population): Patients whose PCa was confirmed pathologically
-
(ii)
I (intervention): The SII level was examined pretreatment for PCa patients, and studies identified a cutoff value of SII for stratifying patients as low/high SII.
-
(iii)
C (comparator): PCa patients with low SII level
-
(iv)
O (outcomes): Studies reported association between SII and PCa survival outcomes; presented any of such survival outcomes as bRFS (biochemical recurrence-free survival), RFS (recurrence-free survival), DFS (disease-free survival), PFS (progression-free survival), and OS (overall survival); and provided HRs (hazard ratios) and corresponding 95% CIs (confidence intervals) for survival outcomes or provided sufficient data to calculate them.
-
(v)
S (study design): Cohort studies, including prospective and retrospective cohorts published in English or Chinese.
Studies were excluded when any of the following criteria was satisfied: (i) case reports, meeting abstracts, reviews or letters, (ii) studies with overlap** patients, (iii) studies with inadequate data for making HR and 95% CI estimations, and (iv) nonhuman studies.
Data extraction and quality assessment
All of the retrieved studies were assessed by 2 independent investigators (B. Z. and T. X.), who were also responsible for extracting information based on a designated form. Disputes were all resolved through negotiation until a consensus was reached. Information extracted included the name of first author, country, age, year of publication, sample size, research design, study duration, metastatic status of disease, therapeutic management, follow-up, SII cutoff, method for cutoff selection, quantity of patients having low/high SII, models of survival analysis, survival endpoints, study center, and HRs with 95% CIs. The methodological quality of enrolled studies was assessed by two reviewers (B. Z. and T. X.) independently on the NOS (Newcastle–Ottawa scale) [28], which achieves quality evaluation from 3 dimensions: selection, comparability, and outcome of interest. The NOS scores varied between 1 and 9 points, and the quality of studies was considered high when the NOS scores ≥ 6.
Statistical analysis
SII’s prognostic significance for OS and PFS was assessed by estimating the pooled HRs with 95% CIs. For the evaluation of inter-study statistical heterogeneity, the χ2-based Q-test combined with Higgins’ I2 test was employed. Inter-study heterogeneity was considered significant when the p-value of Q-test (Ph) < 0.10 and I2 > 50%; accordingly, we adopted the random-effects model. In other cases, a fixed-effects model was utilized. Further exploration was made via the subgroup analysis. The association of SII with the clinicopathological traits of PCa was examined through computation of ORs (odds ratios) and 95% CIs. Sensitivity analysis was used to examine the stability of the results. Possible publication bias was detected by utilizing the Egger’s test in conjunction with Begg’s funnel plot. All of the statistical analyses were made via the Stata 12.0 (StataCorp, TX, USA), and p-values of < 0.05 were regarded as statistically significant.
Results
Study selection process
Figure 1 displays a PRISMA flowchart for screening studies. A total of 118 records were identified upon the initial literature retrieval, and after elimination of duplicate records, 59 studies were retained. Next, 31 of these 59 studies were excluded upon examination of their titles and abstracts, and the remaining 28 studies were subjected further to the full-text examination. Thereafter, 18 studies were eliminated due to absence of data on survival (12 studies), recruitment of overlap** patients (3 studies), no cutoff value (2 studies), and the absence of data on SII (1 study). Finally, the number of studies included in the present meta-analysis totaled 10, involving 8133 patients [17,18,19,20,21,22,23,24,25,26].
Characteristics of the included studies
Table 1 details the basic traits of the enrolled studies [17,18,19,20,21,22,23,24,25,26], which were published from 2016 to 2022. The size of samples varied from 80 to 6039, with a median value of 204.5. Four studies were conducted in China [19, 22, 23, 25], two in Italy [17, 21], and one each in Spain [18], Japan [20], Poland [26], and Austria [24]. Language of publication was English for 9 studies [17,18,19,20,21,22, 24,25,26] whereas was Chinese for 1 study [23]. Six studies included mCRPC patients [17,18,19,20,21,22], and four studies included patients with nonmetastatic PCa [23,24,25,26]. Nine studies were retrospective [17, 19,20,21,22,23,24,25,26] and one was a prospective trial [18]. Eight studies were single-center studies [18,19,20,21,22,23, 25, 26], while two were multicenter studies [17, 24]. The SII cutoff varied between 200 and 900, with a median of 576. Eight studies offered data concerning the SII–OS correlation [17,18,19,20,21,22,23, 26], and two studies presented data on the correlation between the SII and PFS [19, 20], and two studies reported the data on connection between SII and bRFS [24, 25]. Variation scope of NOS scores was 6–9 for the enrolled studies, exhibiting a median of 8, suggesting that the quality of entire enrolled studies was high (Table 1).
Prognostic of SII for OS in PCa
Eight studies with 1803 patients [17,18,19,20,21,22,23, 26] provided HR and 95% CI statistics concerning SII for OS. Since the heterogeneity was significant (I2 = 73.1%, p <0.001), we adopted the random-effects model. As is clear from the pooled results in Fig. 2 and Table 2, high SII was linked significantly to the poor OS (HR = 2.63, 95% CI = 1.87–3.70, p < 0.001). According to the subgroup analysis results, a SII elevation remained a prominent prognostic biomarker for OS, irrespective of research design, and investigated center, region, sample size, cutoff, metastatic state, therapeutic management, or type of survival analysis (Table 2).
Prognostic of SII for PFS/bRFS in PCa
Four studies involving 6578 patients [19, 20, 24, 25] provided data on SII and PFS/bRFS prognosis. According to the pooled HR and 95% CI statistics in Fig. 3 and Table 3, a high SII was a prominent prognostic biomarker for poor PFS/bRFS among the PCa population (HR = 2.49, 95% CI = 1.30–4.77, p = 0.006; I2 = 89.8%, Ph < 0.001). As revealed by the subgroup analysis, region and cutoff were not influencing factors of SII’s prognostic function in PFS/bRFS (Table 3).
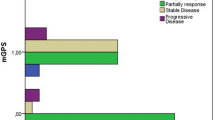
Correlation between SII and clinicopathological factors in PCa
Data concerning SII’s association with the clinicopathological parameters in PCa, including the Gleason score (≥ 8 vs. < 8), lymph node (LN) metastasis (yes vs. no), T stage (≥ 3 vs 1–2), and age (≥ 70 vs. < 70) were reported in 5 studies involving 7056 patients [22,23,24,25,26]. As demonstrated by the results in Fig. 4 and Table 4, a high SII was not linked significantly to T stage (OR = 1.69, 95% CI = 0.86–3.33, p = 0.128), the metastasis to LN (OR = 1.69, 95% CI = 0.69–4.16, p = 0.251), age (OR = 1.41, 95% CI = 0.88–2.23, p = 0.150), or the Gleason score (OR = 1.32, 95% CI = 0.88–1.96, p = 0.178).
Sensitivity analysis
To test the stability of this meta-analysis, sensitivity analysis was conducted through removing each study in turn to recalculate the combined data. The pooled HR estimates were not significantly changed, indicating that the results were stable (Fig. 5).
Publication bias
Assessment of publication bias was accomplished through the Begg’s and Egger’s tests. However, the publication bias for neither OS (Begg’s test: p = 0.174 and Egger’s test: p = 0.310) (Fig. 6A and B) nor PFS/bRFS (Begg’s test, p = 0.089; Egger’s test, p = 0.139) (Fig. 6C and D) was found significant.
Discussion
In former researches, the potential of SII as a prognostic biomarker has been explored for the PCa population [17,18,19,20,21,22,23,24,25,26], despite the unconformable results. In our current meta-analysis, the exact prognostic role of SII in PCa was clarified by pooling the data from 10 studies involving 8133 patients. According to our findings, a high SII represented an independent prognostic biomarker for PFS/bRFS and OS among the PCa patients. Besides, SII exhibited a reliable prognostic power across varying subgroups. However, elevated SII also not correlated with LN metastasis, T stage, Gleason score, or age in PCa. Based on the evidence obtained from this meta-analysis, we recommend the application of SII as a cost-efficient new biomarker for guiding the management and follow-up for the PCa population.
Increasing evidence has suggested the tight linkage of immunoreactions to the cancer occurrence, development, and metastasis [29, 30]. Tumor-derived proinflammatory cytokines like IL (interleukin)-6, IL-8, VEGF, tumor necrosis factor-α, and interferon-γ can be secreted into the tumor microenvironment, leading to chronic inflammation, thus facilitating tumor progression [31]. The SII is a combination of neutrophil, lymphocyte, and platelet counts; thus, it can be elevated in the event of high quantities of neutrophils, platelets, and/or a low quantity of lymphocytes. Current evidence indicates that a microenvironment is offered by the tumor-infiltrating neutrophils, which facilitates the tumor cell growth; they also promote angiogenesis and cell mobility [32]. By constraining the cytolytic potential of various immunocytes, high neutrophil counts inhibit the immunity system [29]. Platelets can release various matrix metalloproteinases to facilitate the degradation of the extracellular matrix, thereby promoting metastasis of cancer cells [33]. In addition, through the proangiogenic cytokine discharge inside the microvasculature of cancer cells, the platelet aggregation is capable of facilitating the tumor growth [34]. In contrast, for the tumor development suppression, lymphocytes are involved critically in the immunosurveillance for cancer [35]. Lymphocytes, including subsets such as CD8+ and CD3+ T cells, correlated with good prognosis in various cancers [36]. Therefore, a high SII is a promising indicator of a combination of neutrophils, lymphocytes, and platelets.
The exact prognostic significance of PSA (prostate-specific antigen), the most extensively applied PCa biomarker [37], in PCa has been reported in several important latest studies [38,39,40]. A study on 148 patients showed the validity of PSA as a biomarker for forecasting the PCa prognosis when its levels were from 20 to 70 ng/mL [38]. According to another study focusing on PCa sufferers having low levels of PSA, the tumor stage was more advanced when the PSA level at diagnosis was < 3.5 ng/ml compared to that between 3.5 and 10 ng/ml [39]. As suggested by a study enrolling 90 PCa patients whose PSA levels were > 100 ng/mL, the differences in OS or CSS were insignificant among the 3 PSA groups, namely the slightly high (100–200 ng/mL), moderately high (200–1000 ng/mL), and considerably high (> 1000 ng/mL) groups [40]. According to the results of our current meta-analysis, the prognosis of patients was poor when their SII was high. SII is an independent risk factor for PCa and could be a better screening method for PCa before biopsy [41]. Therefore, the SII could be used as a biomarker for improving the diagnostic and prognostic accuracy of PSA. Furthermore, a recent study suggested that the level of CCL2 (serum CC motif (chemokine) ligand 2) is a valid prognostic indicator for poor survival in PCa [42]. Patients with serum CCL2 levels ≥ 320 pg/mL had relatively worse OS, CSS, and CRPC-free survival than those with CCL2 concentrations < 320 pg/mL [42]. The relationship between CCL2 levels and the SII needs to be investigated in future studies.
Notably, this meta-analysis included four studies with the endpoint of PFS [19, 20] and bRFS [24, 25]. Two studies enrolled patients with mCRPC [19, 20], whereas two studies recruited the localized PCa patients [24, 25]. The definition of these endpoints in four studies is not all the same. In Fan’s study [19] with mCRPC patients, PFS referred to an interval from the commencement of the first mCRPC therapy (i.e., docetaxel-prednisone or abiraterone) until the time of radiographic progression. In Kobayashi, H.’s work [20] with mCRPC patients, an interval from the disease diagnosis to progression was regarded as PFS. Besides, disease was considered progressed when the serum level of PSA was elevated by > 2 ng/mL, the rise over nadir was 50%, and/or a new lesion emerged, or the known lesions classified as per the RECIST (ver. 1.1) increased by one or more [43]. In Rajwa’ s study with localized PCa patients, bRFS was defined as the interval from radical prostatectomy to the first PSA rise of two consecutive PSA values > 0.2 ng/ml [24]. Although the definitions are not all the same, our results demonstrated that in PCa, a high SII was a prominent prognostic biomarker for poor PFS/bRFS (Table 3). To probe deeper into SII’s prognostic function among patients with different metastatic status, subgroup analysis was conducted. The results showed that a high SII was not associated with poor PFS/bRFS in localized PCa patients (p = 0.160), as well as not with worse PFS/bRFS in mCRPC patients (p = 0.183) (Table 3). Because of the relatively small size of samples, our results still need be verified through large-scale researches.
SII’s prominent prognostic value has been pinpointed for varying solid tumors by extensive recent meta-analyses [44,45,46,47]. As suggested by a meta-analysis involving 7 studies, an elevated pretreatment SII was linked to inferior carcinoma-specific survival/DFS/PFS and poor OS in pancreatic carcinoma patients [44]. According to another meta-analysis covering 4236 patients, a high pretreatment SII forecasted poor OS in gastric carcinoma [48]. A high SII was also reported to be linked to the poor OS among the renal cell carcinoma sufferers [47]. Through a meta-analysis involving 2,796 patients, Wang et al. reported that elevated pretreatment SII was related to lower OS and earlier time-to-recurrence in hepatocellular carcinoma [49]. As indicated by a latest meta-analysis enrolling 12 studies, high levels of SII were correlated pronouncedly with worse PFS and OS among the colorectal cancer population [50]. Our present results on SII’s prognostic role agree with those in other types of carcinomas.
Regarding several shortcomings of our meta-analysis, first of all, the optimal SII cut-off was not determined. The included studies used different cutoff thresholds, which might have contributed to the heterogeneity among studies. Second, majority of the enrolled studies were retrospective, while there was merely 1 enrolled prospective study. Thus, differences in unadjusted factors could lead to selection bias. Third, our meta-analysis included qualified published studies in English or Chinese only, while failing to enroll relevant articles in other languages, which is also likely to result in inherent heterogeneity.
Conclusively, the present meta-analysis suggests the correlation of an elevated pretreatment SII with the shortened PFS/bRFS and OS among the PCa population. SII monitoring could be a potentially effective approach for improving the survival of patients with PCa.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- SII:
-
Systemic immune-inflammation index
- PCa:
-
Prostate cancer
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- bRFS:
-
Biochemical recurrence-free survival
- OR:
-
Odds ratio
- mCRPC:
-
Metastatic castration-resistant prostate cancer
- CNKI:
-
China National Knowledge Infrastructure
- MeSH:
-
Medical Subject Headings
- RFS:
-
Recurrence-free survival
- DFS:
-
Disease-free survival
- NOS:
-
Newcastle-Ottawa scale
- Ph:
-
p-value of the Q-test
- IL:
-
Interleukin
- PSA:
-
Prostate-specific antigen
- CCL2:
-
Chemokine (CC motif) ligand 2
- ROC:
-
Receiver operating characteristic
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A. Recent global patterns in prostate cancer incidence and mortality rates. Eur Urol. 2020;77(1):38–52.
Sandhu S, Moore CM, Chiong E, Beltran H, Bristow RG, Williams SG. Prostate cancer. Lancet. 2021;398(10305):1075–90.
Elsberger B, Lankston L, McMillan DC, Underwood MA, Edwards J. Presence of tumoural C-reactive protein correlates with progressive prostate cancer. Prostate Cancer Prostatic Dis. 2011;14(2):122–8.
Stafford MYC, Willoughby CE, Walsh CP, McKenna DJ. Prognostic value of miR-21 for prostate cancer: a systematic review and meta-analysis. Biosci Rep. 2022;42(1):BSR20211972.
Bahmad HF, Jalloul M, Azar J, Moubarak MM, Samad TA, Mukherji D, et al. Tumor microenvironment in prostate cancer: toward identification of novel molecular biomarkers for diagnosis, prognosis, and therapy development. Front Genet. 2021;12:652747.
Francolini G, Loi M, Ciccone LP, Detti B, Di Cataldo V, Pinzani P, et al. Prospective assessment of AR splice variant and multi-biomarker expression on circulating tumor cells of mCRPC patients undergoing androgen receptor targeted agents: interim analysis of PRIMERA trial (NCT04188275). Med Oncol (Northwood, London, England). 2022;39(8):119.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Hasegawa S, Eguchi H, Tomokuni A, Tomimaru Y, Asaoka T, Wada H, et al. Pre-treatment neutrophil to lymphocyte ratio as a predictive marker for pathological response to preoperative chemoradiotherapy in pancreatic cancer. Oncol Lett. 2016;11(2):1560–6.
Lu A, Li H, Zheng Y, Tang M, Li J, Wu H, et al. Prognostic significance of neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio, and platelet to lymphocyte ratio in patients with nasopharyngeal carcinoma. Biomed Res Int. 2017;2017:3047802.
Tamai K, Okamura S, Makino S, Yamamura N, Fukuchi N, Ebisui C, et al. C-reactive protein/albumin ratio predicts survival after curative surgery in elderly patients with colorectal cancer. Updates Surg. 2022;74(1):153–62.
Yamashita S, Iwahashi Y, Miyai H, Matsumura N, Hagino K, Kikkawa K, et al. Usefulness of preoperative high systemic immune-inflammation index as a prognostic biomarker in patients who undergo radical cystectomy for bladder cancer: multicenter analysis. Diagnostics. 2021;11(12):2194.
Pang Q, Zhou L, Qu K, Cui RX, ** H, Liu HC. Validation of inflammation-based prognostic models in patients with hepatitis B-associated hepatocellular carcinoma: a retrospective observational study. Eur J Gastroenterol Hepatol. 2018;30(1):60–70.
Zhang K, Hua YQ, Wang D, Chen LY, Wu CJ, Chen Z, et al. Systemic immune-inflammation index predicts prognosis of patients with advanced pancreatic cancer. J Transl Med. 2019;17(1):30.
Chen L, Kong X, Wang Z, Wang X, Fang Y, Wang J. Pre-treatment systemic immune-inflammation index is a useful prognostic indicator in patients with breast cancer undergoing neoadjuvant chemotherapy. J Cell Mol Med. 2020;24(5):2993–3021.
Guo D, Zhang J, **g W, Liu J, Zhu H, Fu L, et al. Prognostic value of systemic immune-inflammation index in patients with advanced non-small-cell lung cancer. Fut Oncol (London, England). 2018;14(25):2643–50.
Bauckneht M, Rebuzzi SE, Signori A, Frantellizzi V, Murianni V, Lodi Rizzini E, et al. The prognostic power of inflammatory indices and clinical factors in metastatic castration-resistant prostate cancer patients treated with radium-223 (BIO-Ra study). Eur J Nucl Med Mol Imaging. 2022;49(3):1063–74.
Donate-Moreno MJ, Lorenzo-Sánchez MV, Díaz de Mera-Sánchez Migallón I, Herraiz-Raya L, Esper-Rueda JA, Legido-Gómez O, et al. Inflammatory markers as prognostic factors in metastatic castration-resistant prostate cancer. Actas Urol Esp (Engl Ed). 2020;44(10):692–700.
Fan L, Wang R, Chi C, Cai W, Zhang Y, Qian H, et al. Systemic immune-inflammation index predicts the combined clinical outcome after sequential therapy with abiraterone and docetaxel for metastatic castration-resistant prostate cancer patients. Prostate. 2018;78(4):250–6.
Kobayashi H, Shiota M, Sato N, Kobayashi S, Matsumoto T, Monji K, et al. Differential prognostic impact of complete blood count-related parameters by prior use of novel androgen receptor pathway inhibitors in docetaxel-treated castration-resistant prostate cancer patients. Anticancer Drugs. 2022;33(1):e541–7.
Lolli C, Caffo O, Scarpi E, Aieta M, Conteduca V, Maines F, et al. Systemic immune-inflammation index predicts the clinical outcome in patients with mCRPC treated with abiraterone. Front Pharmacol. 2016;7:376.
Man YN, Chen YF. Systemic immune-inflammation index, serum albumin, and fibrinogen impact prognosis in castration-resistant prostate cancer patients treated with first-line docetaxel. Int Urol Nephrol. 2019;51(12):2189–99.
Pan Z, Cheng W, Cai H, Zhang H. Correlation between preoperative systemic immune inflammation index and prognosis of high-risk/very high-risk prostate cancer patients after radical operation. Chin Mod Doctor. 2020;58(13):49–52+56.
Rajwa P, Schuettfort VM, D'Andrea D, Quhal F, Mori K, Katayama S, et al. Impact of systemic immune-inflammation index on oncologic outcomes in patients treated with radical prostatectomy for clinically nonmetastatic prostate cancer. Urol Oncol. 2021;39(11):785.e719–27.
Wang S, Yang X, Yu Z, Du P, Sheng X, Cao Y, et al. The values of systemic immune-inflammation index and neutrophil-lymphocyte ratio in predicting biochemical recurrence in patients with localized prostate cancer after radical prostatectomy. Front Oncol. 2022;12:907625.
Zapała P, Garbas K, Lewandowski Z, Zapała Ł, Ślusarczyk A, Ślusarczyk C, et al. The clinical utility of systemic immune-inflammation index supporting Charlson Comorbidity Index and CAPRA-S score in determining survival after radical prostatectomy-a single centre study. Cancers (Basel). 2022;14(17):4135.
Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P: The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2009. Available from: http://www.ohrica/programs/clinical_epidemiology/oxfordasp.
Demaria O, Cornen S, Daeron M, Morel Y, Medzhitov R, Vivier E. Harnessing innate immunity in cancer therapy. Nature. 2019;574(7776):45–56.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Landskron G, De la Fuente M, Thuwajit P, Thuwajit C, Hermoso MA. Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res. 2014;2014:149185.
Neal JT, Li X, Zhu J, Giangarra V, Grzeskowiak CL, Ju J, et al. Organoid modeling of the tumor immune microenvironment. Cell. 2018;175(7):1972–1988.e1916.
Rolli M, Fransvea E, Pilch J, Saven A, Felding-Habermann B. Activated integrin alphavbeta3 cooperates with metalloproteinase MMP-9 in regulating migration of metastatic breast cancer cells. Proc Natl Acad Sci U S A. 2003;100(16):9482–7.
Sierko E, Wojtukiewicz MZ. Platelets and angiogenesis in malignancy. Semin Thromb Hemost. 2004;30(1):95–108.
Bambace NM, Holmes CE. The platelet contribution to cancer progression. J Thromb Haemost. 2011;9(2):237–49.
Zhao G, Liu N, Wang S, Guo J, Song X, Qi Y, et al. Prognostic significance of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in patients with metastatic gastric cancer. Medicine (Baltimore). 2020;99(10):e19405.
Duffy MJ. Biomarkers for prostate cancer: prostate-specific antigen and beyond. Clin Chem Lab Med. 2020;58(3):326–39.
Iwamoto H, Izumi K, Kadono Y, Mizokami A. Prognosis of patients with prostate cancer and middle range prostate - specific antigen levels of 20 - 100 ng / mL. Int Braz J Urol. 2019;45(1):61–7.
Izumi K, Ikeda H, Maolake A, Machioka K, Nohara T, Narimoto K, et al. The relationship between prostate-specific antigen and TNM classification or Gleason score in prostate cancer patients with low prostate-specific antigen levels. Prostate. 2015;75(10):1034–42.
Izumi K, Lin WJ, Miyamoto H, Huang CK, Maolake A, Kitagawa Y, et al. Outcomes and predictive factors of prostate cancer patients with extremely high prostate-specific antigen level. J Cancer Res Clin Oncol. 2014;140(8):1413–9.
Wang S, Ji YP, Chen YY, Du P, Cao YD, Yang X, et al. The values of systemic immune-inflammation index and neutrophil-lymphocyte ratio in the localized prostate cancer and benign prostate hyperplasia: a retrospective clinical study. Front Oncol. 2022;11:812319.
Izumi K, Mizokami A, Lin HP, Ho HM, Iwamoto H, Maolake A, et al. Serum chemokine (CC motif) ligand 2 level as a diagnostic, predictive, and prognostic biomarker for prostate cancer. Oncotarget. 2016;7(7):8389–98.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol. 2008;26(7):1148–59.
Li M, Li Z, Wang Z, Yue C, Hu W, Lu H. Prognostic value of systemic immune-inflammation index in patients with pancreatic cancer: a meta-analysis. Clin Exp Med. 2022;22(4):637–46.
Wu Y, Tu C, Shao C. The value of preoperative systemic immune-inflammation index in predicting vascular invasion of hepatocellular carcinoma: a meta-analysis. Brazilian journal of medical and biological research =. Rev Bras Pesqui Med Biol. 2021;54(4):e10273.
Wang Q, Zhu SR, Huang XP, Liu XQ, Liu JB, Tian G. Prognostic value of systemic immune-inflammation index in patients with urinary system cancers: a meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25(3):1302–10.
** M, Yuan S, Yuan Y, Yi L. Prognostic and clinicopathological significance of the systemic immune-inflammation index in patients with renal cell carcinoma: a meta-analysis. Front Oncol. 2021;11:735803.
Qiu Y, Zhang Z, Chen Y. Prognostic value of pretreatment systemic immune-inflammation index in gastric cancer: a meta-analysis. Front Oncol. 2021;11:537140.
Wang B, Huang Y, Lin T. Prognostic impact of elevated pre-treatment systemic immune-inflammation index (SII) in hepatocellular carcinoma: a meta-analysis. Medicine (Baltimore). 2020;99(1):e18571.
Dong M, Shi Y, Yang J, Zhou Q, Lian Y, Wang D, et al. Prognostic and clinicopathological significance of systemic immune-inflammation index in colorectal cancer: a meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920937425.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
BZ and TX conceived the study and drafted the manuscript. BZ and TX conducted the literature search. BX and TX extracted the data. BZ and TX took part in the statistical analysis and interpreted the outcomes. BZ made the figures and tables. All authors revised and checked the final manuscript. All authors contributed to the article and approved the submitted version. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The PRISMA checklist.
Additional file 2.
The detailed search strategies for each database.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, B., Xu, T. Prognostic significance of pretreatment systemic immune-inflammation index in patients with prostate cancer: a meta-analysis. World J Surg Onc 21, 2 (2023). https://doi.org/10.1186/s12957-022-02878-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-022-02878-7