Abstract
Periodontitis is a chronic inflammatory disease caused by the local microbiome and the host immune response, resulting in periodontal structure damage and even tooth loss. Scaling and root planning combined with antibiotics are the conventional means of nonsurgical treatment of periodontitis, but they are insufficient to fully heal periodontitis due to intractable bacterial attachment and drug resistance. Novel and effective therapeutic options in clinical drug therapy remain scarce. Nanotherapeutics achieve stable cell targeting, oral retention and smart release by great flexibility in changing the chemical composition or physical characteristics of nanoparticles. Meanwhile, the protectiveness and high surface area to volume ratio of nanoparticles enable high drug loading, ensuring a remarkable therapeutic efficacy. Currently, the combination of advanced nanoparticles and novel therapeutic strategies is the most active research area in periodontitis treatment. In this review, we first introduce the pathogenesis of periodontitis, and then summarize the state-of-the-art nanotherapeutic strategies based on the triple concerto of antibacterial activity, immunomodulation and periodontium regeneration, particularly focusing on the therapeutic mechanism and ingenious design of nanomedicines. Finally, the challenges and prospects of nano therapy for periodontitis are discussed from the perspective of current treatment problems and future development trends.
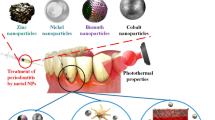
Graphical Abstract

Similar content being viewed by others
Introduction
Periodontitis is a chronic inflammatory disease with clinical manifestations such as bleeding gums, recurrent swelling and pain, and resorption of alveolar bone. If inadequately treated, it can lead to loosening and loss of teeth, chewing function, and even effects on the digestive system [1]. In the world, periodontitis affects 11% of the global population, with prevalence rates ranging from 8 to 46% in develo** countries and 3–18% in developed countries [2]. Periodontitis is more common in the aged due to chronic and cumulative injury. Two thirds of people over 65 years old in the United States have chronic periodontitis [3]. In recent decades, the incidence and prevalence of severe periodontitis in Asian countries, such as India, China and Japan, has been on the rise, and age may be a critical factor for the increasing trend [69, 70]. Chlorin e6 (Ce6) is widely used in PDT therapy because of its strong tissue penetration, great biocompatibility and high yield of singlet oxygen [71, 72]. Sun et al. prepared a core–shell structure nanodrug delivery system (Fe3O4-silane@Ce6/C6) including Fe3O4 nanoparticles, Ce6 and coumarin 6, for PDT antimicrobial therapy [73]. Transmission electron microscopy (TEM) images of Fe3O4 nanoparticles show a diameter of approximately 8 nm and Fe3O4-silane@Ce6/C6 a diameter of about 100 nm. Fe3O4-silane@Ce6/C6 produced O2− under light irradiation and had a killing effect on Streptococcus sanguis, Pg and Fn Under light irradiation, Fe3O4-silane@Ce6/C6 reduced Fn and Pg biofilm colony formation units by approximately 4 log and 5 log, respectively. Notably, Fe3O4-silane@Ce6/C6 can be magnetically induced to concentrate at plaque biofilm sites to further enhance the antibacterial effect. These results indicate that PDT combined with magnetic targeted nanoparticles has potential for antimicrobial therapy for periodontitis.
Although PDT has made important progress in the treatment of periodontal disease, there are some serious problems that still need to be solved before clinical application. The most important limitation of conventional PDT is the weak tissue penetration of ultraviolet or visible light. Therefore, it is highly desirable to design and prepare a PDT system that relies on with the infrared irradiation light, which can perform deep-tissue penetration. Based on this, a strategy was proposed to combine the photosensitizer Ce6 with upconversion nanoparticles (UCNPs) NaYF4:Yb, Er [74]. The combination of Ce6 UCNPs was realized via an amphiphilic silane modification technique (NaYF4@Ce6@silane NPs), which involved the hydrophobic-hydrophobic interaction between the hydrophobic side chain of the silane and hydrophobic groups on the surface of UCNPs [75]. In addition, because the PDT function of the Ce6 molecule should be triggered by excitation by red light, Mn do** is involved in this work, which greatly improves the probability of the red emission transition (NaYF4-Mn@Ce6@silane) (Fig. 4A). The TEM image showed that the size distribution of NaYF4@Ce6@silane NPs was approximately 30 nm, and a thin layer of silane (approximately 2–3 nm) was observed on the surface of the nanoparticles after silane coating. The result showed that 30% Mn was selected to dope into UCNPs to realize the enhancement of red-light emission, and the enhanced upconversion red emission can further improve the PDT effect. The colony forming units of Pg, Fn and P. intermedia after NaYF4-Mn@Ce6@silane NPs with 980 nm irradiation decreased by more than 2 log, and the biofilm matrix was easily disrupted with deeper penetration of infrared light. This highly efficacy against periodontitis-related biofilms should be attributed to the high hydrophilic surface after silane modification, as well as to the upconversion luminescence triggered PDT. This upconversion PDT design can overcome the problems of conventional PDT and provide effective nano strategies for the treatment of periodontitis.
Schematic illustration of periodontitis treatment by photothermal/photodynamic therapy. A The schematic diagram of NaYF4-Mn@Ce6@silane. Reprinted with permission from Ref. [74] Copyright Multidisciplinary Digital Publishing Institute. B Preparation and against periodontitis of TAT-Ce6/TDZ NPs. Reprinted with permission from Ref. [76] Copyright American Chemical Society. C Preparation of sPDMA@ICG NPs and treatment of synergistic PTT and PDT on periodontitis. D TEM images of bacteria after processions of PBS (the control), sPDMA@ICG NPs with and without laser irradiation. E Photos of plaque biofilms after various processions. F Comparison for the mean fluorescence intensities of produced DCF in periodontium. Infrared thermal images of periodontium during laser irradiation after administration of PBS (the control) and sPDMA@ICG NPs. **indicates p < 0.01 compared to the control (+); ##indicates p < 0.01 for comparison between two groups. Reprinted with permission from Ref. [79] Copyright Springer Nature
However, PDT does not always achieve the desired therapeutic outcomes since photosensitizers Ce6 have strong hydrophobic properties and are not taken up efficiently by periodontal pathogenic bacteria. Li et al. designed a nanosystem to improve Ce6 solubility and enhance its bacterial adsorption by promoting its interaction with negatively charged cell walls and penetration through cell membranes [76]. They first hydrophilically-modified Ce6 via conjugation with TAT peptide, a cationic cell-penetrating peptide (TAT-Ce6). Then, TAT-Ce6 was loaded with the antibiotic agent tinidazole to prepare self-assembled nanoparticles (TAT-Ce6/TDZ NPs) to achieve synergistic anti-periodontitis effects by combining PDT and antibiotic therapy (Fig. 4B). TEM image showed that TAT-Ce6/TDZ NPs had a regular spherical shape and exhibited a more compact inner structure. The particle size of TAT-Ce6/TDZ NPs was ~ 146.2 nm, and the zeta potential was approximately + 40.1 mV, which confirmed the surface distribution of the positively charged TAT peptide. The UV absorption of ABDA attenuates when ABDA is decomposed by the ROS produced in the sample solution, and the degree of attenuation is positively correlated with the ROS generation level. The results showed that the attenuation rate of ABDA absorption in the solution of TAT-Ce6/TDZ NPs was much faster than that of free Ce6 during 20 min of laser irradiation, indicating that TAT-Ce6/TDZ NPs had a much higher PDT efficiency. The zeta potentials of Pg were increased from − 11.2 to + 5.86 mV after 1 h of incubation with TAT-Ce6. The above results indicated that TAT-Ce6 significantly promoted the penetration of the bacterial cell membrane through the TAT peptide. TAT-Ce6/TDZ NPs and TAT-Ce6 exhibited much stronger bacterial killing activity, owing to their more efficient absorption by the plaque biofilms via the mediation of TAT peptide. More importantly, TAT-Ce6/TDZ NPs exhibited much stronger bacterial killing activity than TAT-Ce6 NPs with laser irradiation, further confirming their synergistic antibacterial efficacy through combining PDT and antibiotic therapy.
Indocyanine green (ICG), a photosensitizer with PDT properties, has been approved for clinical use by the US Food and Drug Administration [77]. Nagahara et al. first explored PDT of photosensitizer indocyanine green, which has high absorption at a wavelengths of 800–805 nm [78]. They designed ICG-loaded PLGA nanospheres coated with chitosan (ICGNano/c) and explored the PDT of ICGNano/c in Pg. The study showed that ICG-Nano/c with low-level diode laser (0.5 W, 805 nm) irradiation showed a PDT-like effect, which might be useful for potential photodynamic periodontal therapy. Recently, combined treatment with PTT and PDT has further improved the efficiency of periodontitis treatment. However, due to its negative charge and water solubility, ICG has difficulty passing through bacterial cell membranes. To address this problem, Shi and his colleagues incorporated it into positively charged polycationic brush nanoparticles (sPDMA@ICG NPs) (Fig. 4C) [79]. CD-Br was synthesized by esterifying β-cyclodextrin with 2-bromoisobutyryl bromide via an esterification reaction. Next, star-shaped polycationic brush poly (2-(dimethyl amino) ethyl methacrylate) was synthesized by an atom transfer radical polymerization reaction using CD-Br as an initiator. Finally, sPDMA@ICG NPs loaded with ICG were prepared by the nanometer precipitation method. The average particle size of sPDMA@ICG NPs was 206 nm and the zeta potential was approximately + 18.4 mV. On the one hand, the temperature of the sPDMA@ICG NPs solution was increased from 22 to 55 °C after irradiation with an 808 nm laser (2 W/cm2), which reflects an excellent PTT performance. On the other hand, sPDMA@ICG NPs also exert PDT properties. The results suggested that sPDMA@ICG NPs can produce ROS after laser irradiation, as detected by SOSG. Confocal microscopy images show that sPDMA@ICG NPs are effectively accumulate in bacterial cells after the administration of sPDMA@ICG NPs. TEM images showed that sPDMA@ICG NPs were clearly visible on the surface of Pg, and that the bacterial film ruptured and bacterial cells disintegrated after laser irradiation (Fig. 4D). In addition, sPDMA@ICG NPs with laser irradiation reduced the growing area of plaque biofilms derived derive from a rat model of periodontitis (Fig. 4E). After sPDMA@ICG NPs administration and laser irradiation, temperature and ROS levels were increased in rats with periodontitis, indicating that sPDMA@ICG NPs exert synergistic PTT and PDT effects in vivo (Fig. 4F).
Immunomodulatory nanotherapeutic strategies
In periodontitis, the presence of plaque microorganisms and their products can activate the host immune response [80]. Local host immune overreaction then, leads to increased inflammation and disruption of homeostasis, exacerbating periodontium lesions. Most tissue damage within periodontitis is caused by the host immune response rather than directly by the infecting microorganism [81, 82]. Therefore, in terms of therapeutic strategies, suitable immunomodulatory targets can be screened to modulate the host immune system to mitigate the inflammatory response. Recently, many nanosystems have been designed to modulate the function of immune cells and inflammation-associated cytokines to alleviate periodontal inflammation, and these nanosystems have achieved excellent therapeutic results both in vitro and in vivo (Table 2).
Remodeling macrophage polarization
In the immune system, immune cells such as macrophages play an important role as the host's first line of defenses against microorganisms. When induced by different factors, macrophages polarize and develop different phenotypes, such as M1 and M2, both of which are involved in regulating the immune response [83]. M1-type macrophages produce the cytokines IL-6 and TNF-α, which promote the inflammatory response [84, 85]. M2 macrophages can be further classified into alternatively activated macrophages (M2a), type 2 macrophages (M2b), deactivated macrophages (M2c), and M2-like macrophages (M2d) by different stimuli and transcription levels [86, 96]. IL-17 has been shown to boost RANKL expression while inhibiting OPG expression in periodontal ligament cells, which might explain why Th17 cells promote alveolar bone loss [95]. However, Tregs can suppress the host immune response in equilibrium with Th17 cells in the periodontium [97, 98]. To date, no drug/nanosystem has been reported to directly regulate the Th17/Treg cells balance, but exosomes derived from periodontal ligament stem cells have been found to have the potential to regulate Th17/Treg cells.
Zhang et al. found that exosomes derived from mesenchymal stem cells (3D-exos) could regulate Th17/Tregs cell balance [99]. Notably, replacing the traditional 2D culture system with a 3D system could increase exosome production. The average particle size of the 3D-exos was 50–200 nm. A significant Th17 reduction and Treg elevation were observed in the periodontium after treatment with 3D-exos in periodontitis mice. Gene Ontology analysis showed that differentially expressed genes in 3D-exo-treated mice with periodontitis were enriched for T-cell chemotaxis. These results suggested that 3D-exos can further regulate Th17/Tregs cells in a periodontitis mice model. Furthermore, RNA-seq and TargetScan results indicated that miR-1246 is the most differentially expressed miRNA in 3D-exo, which targets Nfat5. Nfat5 is a key factor that mediates Th17 cell polarization in a sequence-dependent manner. Therefore, 3D-exo suppresses Th17 cell differentiation by miR-1246 through downregulation of Nfat5 gene expression.
Zheng et al. investigated the effect of exosomes from periodontal membrane stem cells (PDLSC-exos) on Th17/Treg balance [100]. The expression of the Th17-related transcription factor RAR-related orphan receptor C was upregulated and the Treg-related transcription factor forkhead Box P3 was down-regulated in periodontitis patients. This means that the Th17/Treg ratio is unbalanced in patients with periodontitis. The results showed lower Th17-related CD4+/IL‐17+ expression and increased Treg-related CD4+CD25+FOXP3+ expression after treatment of PDLSC-exos in CD4+ T cells, confirming the regulatory effect of PDLSCs-exos on the Th17/Treg balance. In addition, the mechanistic results showed that PDLSC-exos transfer miR-155-5p into CD4+ T cells, which in turn regulates the expression of histone deacetylase protein in CD4+ T cells, thus affecting the Th17/Treg homeostasis. Therefore, miR-155-5p may be a promising target for the treatment of immune imbalance in periodontitis. In summary, exosomes are a potential nano drug delivery system to regulate the balance of Th17 and Treg cells, and their potential in the treatment of periodontitis needs to be further explored.
Regulating pro-/anti-inflammatory cytokine secretion
Inflammatory cytokines secreted from immune or tissue cells are key regulators of the immune response process, and pro-/anti-inflammatory cytokine imbalance is an important factor in the aggravation of periodontitis [37]. Cytokines, such as IL-1β, IL-6 and TNF-α, activate inflammation-related transcription factors or activate related signaling pathways, thereby accelerating the process of periodontitis. The anti-inflammatory cytokines of IL-10, TGF-β and IL-11, downregulate the expression levels of pro-inflammatory factors, protect the periodontium and inhibit the development of periodontitis [101,102,103]. It is extremely important to modulate pro-/anti-inflammatory cytokine secretion for restore immune balance in periodontitis treatment.
Li et al. prepared baicalin and baicalein-loaded mesoporous silica nanoparticles (Nano-BA and Nano-BE) to regulate inflammatory cytokine secretion [104]. The mesoporous silica nanoparticles were modified by 3-aminopropyl-triethoxy silane. An inflammation cell model was established by primary human gingival epithelial cells pretreated with IL-1β stimulation. Nano-BA and Nano-BE downregulated cytokines involved in the immune inflammatory response. Among them, epithelial cell-derived neutrophil-activating peptide 78, monocyte chemoattractant protein-1, and IL-8 function as chemokines leading to inflammation or tissue damage, while granulocyte colony-stimulating factor and granulocyte–macrophage colony-stimulating factor stimulate the differentiation and proliferation of hematopoietic stem cell immune cells.
In another study, Polydopamine nanoparticles (PDA NPs) were synthesized via self-polymerization with dopamine hydrochloride and a solution containing NH4OH and ethanol [105]. PDA NPs effectively reduce the levels of TNF-α and IL-1β inflammatory mediators. After PDA NPs treatment in mice, the cytokine levels of TNF-α, IFN -γ, and IL-1β in serum recovered to normal values. Moreover, all the levels of alanine aminotransferase, aspartate aminotransferase and alkaline phosphatase (ALP) were also in the reference normal ranges. Notably, PDA NPs efficiently reduced the level of ROS in LPS-induced local high fluorescence signals. The above results suggest that reducing ROS levels may help to regulate inflammatory cytokine levels during periodontitis treatment.
Periodontium regeneration nanotherapeutics strategies
The periodontium consists of the gingiva, periodontal ligament, alveolar bone and cementum, which provide physical and mechanical support for the teeth [106, 107]. Severe periodontitis leads to the loss of periodontal attachment, which is one of the major causes of tooth loss in adults. Therefore, the main goal of periodontitis treatment is to reduce the destruction of the periodontium, finally achieving periodontium regeneration. In recent years, researchers have proposed a series of advanced nanotherapeutic strategies to achieve periodontium regeneration by regulating cell differentiation and disturbing osteoclastogenesis (Table 3).
Promoting periodontal membrane stem cell differentiation
Periodontal membrane stem cells (PDLSCs), a subpopulation of mesenchymal stem cells, have self-renewal and immunomodulatory properties [108]. Moreover, PDLSCs can specifically repair the damaged periodontium [109]. PDLSCs can differentiate into fibroblasts, osteoblast-like cells and dental osteoclast-like cells to generate connective and dental osteoid tissue by nanomedicine (Fig. 6A) [110]. Therefore, regulating the differentiation of PDLSCs is a promising strategy for periodontium repair.
A PDLSCs through self-renewal, differentiating into osteoblasts and fibroblasts and regulating the host immune response to maintain the periodontal homeostasis. Reprinted with permission from Ref. [34] Copyright Oxford University Press. B Schematic illustration of M2-Exos promoting osteogenic differentiation of bone marrow stromal cells and inhibiting osteoclast formation of bone marrow-derived macrophages. Reprinted with permission from Ref. [125] Copyright Springer Nature
AuNPs promote the proliferation of human periodontal membrane stem cells via the classical Wnt/β-linked protein signaling pathway [111]. On this basis, Zhang et al. further investigated the potential of AuNPs to promote osteogenic differentiation of PDLCs [173]. In addition, the smart hydrogel can control release nanomedicines through the stimuli-responses including ROS, pH, light, enzymes, etc. MZ@PNM was integrated with chitosan/sodiumβ-glycerophosphate system for pH-responsive release properties due to the remaining amino groups on chitosan matrix. The hydrogel structure was significantly collapse after incubation at pH 4.0 than at pH 7.4, which could release the nanoparticles in the acidic periodontal environment [137].
In addition, bio-sponges with porous structures have ideal loading properties, biocompatibility and biodegradability, which gain attention in the field of hemostasis and wound healing. Wang's group prepared bio-sponges based on carboxymethyl chitosan/ poly-gamma-glutamic acid/platelet-rich plasma that adhere and coagulate red blood cells to accelerate blood clotting via releasing epidermal growth factor and vascular endothelial growth factor [174]. In the field of periodontitis treatment, bio-sponge platforms are absorbable and relatively inert during bone regeneration. Mesenchymal stem cell exosome-loaded collagen sponge promoted newly-formed bone and periodontal ligament regeneration by increasing periodontal ligament cell migration and proliferation [175].
Electrets have attracted widespread interest in bone regeneration and drug delivery due to the great performance in endogenous electrical stimulation for enhancing cell proliferation and differentiation [176]. Yu et al. designed an electret-based host-coupled biological nanogenerator through electrical stimulation to increase cytoplasmic calcium ions to activate osteogenic differentiation. The result showed that electret significantly promoted the osteogenic differentiation of bone marrow mesenchymal stem cells in vitro and bone regeneration in vivo [177]. The development of nanocomposite delivery systems utilizing the advantages of charge retention and high surface charge density of electrets nano-materials such as ZnO and SiO2, may be a potential therapeutic strategy for the treatment of periodontitis.
Opportunities of periodontitis comorbidities treatment
Periodontitis is associated with diabetes, rheumatoid arthritis, Alzheimer's disease, hypertension, inflammatory bowel disease, and even autoimmune diseases and cancer (Fig. 11) [178,179,180]. Therefore, nanodelivery systems also have promising applications in the treatment of periodontitis with comorbidities. For instance, there is a bidirectional association between periodontitis and diabetes [181]. Periodontitis may increase the prevalence of diabetes and affect the effective control of blood glucose [182, 183]. On the other hand, metabolic disorders in diabetic patients lead to excessive production of ROS, which has a damaging effect on alveolar bone. The damage to periodontal tissue in diabetic patients with periodontitis was more destructive than that in patients with periodontitis alone. To address this problem, Zhao et al. developed a ROS-responsive drug delivery system loaded with both doxycycline and metformin that worked effectively in periodontitis with diabetes [184]. Wang et al. prepared injectable nano-hydrogels using mesoporous silica nanoparticles incorporating poly(d, l-lactide)-block-poly(ethylene glycol)-block-poly(d, l-lactide) to model the mesenchymal stem cells "recruitment-osteogenic" cascade for periodontal bone regeneration [185]. Nanotherapeutic strategies will provide more opportunities for the treatment of periodontitis complications.
Periodontitis and associated inflammatory comorbidities. Reprinted with permission from Ref. [186] Copyright Springer Nature
Nanotherapeutic potential of natural active ingredients
Antibiotics and non-steroidal anti-inflammatory agents have potential problems in the treatment of periodontitis including drug resistance, dysbacteriosis and gastrointestinal adverse effects. Natural components derived from natural sources are currently attracting interest from researchers. Natural ingredients with proven therapeutic effects on periodontitis include quercetin, resveratrol, baicalin, curcumin, etc. [187].
Quercetin has a potential protective effect against chronic inflammation-related periodontitis by suppressing the Akt/AMPK/mTOR pathway [188]. In another study, quercetin was found to reduce alveolar bone loss by inhibiting inflammation in periodontitis rats [189]. Resveratrol protects against periodontitis-induced tissue damage by augmenting HO-1 via Nrf2-mediated signaling [190]. Curcumin significantly reduced the expression of TNF-α and IL-6 by inhibiting the phosphorylation of p38 MAPK and reducing the inflammatory response in macrophages [191]. Plumbagin down-regulating the mRNA expression of the pro-inflammatory cytokines TNF-α, IL-1β and IL-6 in periodontium, thereby retarding the development of inflammation [192].
Natural ingredients have achieved excellent experimental results in the treatment of periodontitis. However, most of the natural ingredients have poor solubility and safety problems. In addition, little is known about the in vivo pharmacokinetic studies of natural active ingredients, which limits the clinical translation of natural active ingredients in the treatment of periodontitis. The use of advanced nanodrug delivery systems is expected to solve the problems of drug formation of natural ingredients in the future.
Conclusion
The in-depth study of pathogenesis and the development of nanomaterial engineering promote the development of nanotherapeutic strategies for periodontitis. The diverse physicochemical properties and targeting properties of nanodelivery systems create a favourable platform for drug delivery to treat periodontitis. In this article, we review the nanotherapeutic strategies for periodontitis to provide inspiration for future advances in periodontitis treatment and innovations in the design of nanodelivery systems. Overall, nanotherapeutics have shown great potential at preclinical levels, but their clinical performance remains to be evaluated. More work is needed to refine the development of novel nanotherapeutic strategies. We believe that nanotherapeutic strategies will soon provide new opportunities for the treatment of periodontitis, thereby alleviating patient suffering and the medical burden on society.
Availability of data and materials
Not applicable.
Abbreviations
- ABC:
-
Alveolar bone crest
- ALP:
-
Alkaline phosphatase
- Au NBPs:
-
Au nano bipyramids
- AuNPs:
-
Au nanoparticles
- BMDM:
-
Bone marrow derived macrophage
- BMSCs:
-
Bone marrow stem cells
- BV/TV:
-
Bone volume/tissue volume
- C5aR:
-
Component 5a receptor
- Ce6:
-
Chlorin e6
- CEJ:
-
Cement-enamel junction
- CeO2 :
-
Cerium oxide nanoparticles
- CXCL:
-
C-X-C motif chemokine ligand
- COL-1:
-
Collagen type I
- CXCR3:
-
C-X-C motif chemokine receptor 3
- DCs:
-
Dendritic cells
- Fn:
-
Fusobacterium nucleatum
- Gel MA:
-
Gelatin methacrylate
- ICG:
-
Indocyanine green
- IFN‐γ:
-
Interferon‐γ
- IL:
-
Interleukin
- LPS:
-
Lipopolysaccharide
- Micro-CT:
-
Micro computed tomography
- NF-κB:
-
Nuclear transcription factor-κB
- NIR:
-
Near infrared
- OCN:
-
Osteocalcin
- OPG:
-
Osteoprotegerin
- PDLSCs:
-
Periodontal membrane stem cells
- PDT:
-
Photodynamic therapy
- Pg:
-
Porphyromonas gingivalis
- PLGA:
-
Poly (D, L-lactide-co-glycolide)
- PTT:
-
Photothermal therapy
- RANKL:
-
Receptor activator of nuclear factor kappa-Β ligand
- RNA-seq:
-
RNA sequencing
- ROS:
-
Reactive oxygen species
- RUNX2:
-
Runt-related transcription factor 2
- SEM:
-
Scanning electron microscopy
- STAT:
-
Signal transducer and activator of transcription
- Tb.N:
-
Trabecular number
- TEM:
-
Transmission electron microscopy
- TGF-β:
-
Transforming growth factor-β
- Th-:
-
T helper
- TNF-α:
-
Tumor necrosis factor-α
- TRAP:
-
Tartrate resistant acid phosphatase
- Treg:
-
Regulatory T cell
- ZIF-8:
-
Zeolite imidazole skeleton-8
- ZnO:
-
Zinc oxide
References
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–60.
Jiao J, **g W, Si Y, Feng X, Tai B, Hu D, Lin H, Wang B, Wang C, Zheng S, et al. The prevalence and severity of periodontal disease in Mainland China: data from the Fourth National Oral Health Survey (2015–2016). J Clin Periodontol. 2021;48:168–79.
Eke PI, Wei L, Borgnakke WS, Thornton-Evans G, Zhang XY, Lu H, Mcguire LC, Genco RJ. Periodontitis prevalence in adults ≥ 65 years of age, in the USA. Periodontol. 2000;2016(72):76–95.
Luo LS, Luan HH, Wu L, Shi YJ, Wang YB, Huang Q, **e WZ, Zeng XT. Secular trends in severe periodontitis incidence, prevalence and disability-adjusted life years in five Asian countries: a comparative study from 1990 to 2017. J Clin Periodontol. 2021;48:627–37.
Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation. Nat Rev Immunol. 2015;15:30–44.
Zieba M, Chaber P, Duale K, Martinka Maksymiak M, Basczok M, Kowalczuk M, Adamus G. Polymeric carriers for delivery systems in the treatment of chronic periodontal disease. Polymers (Basel). 2020;12:1574.
Hajishengallis G. Interconnection of periodontal disease and comorbidities: Evidence, mechanisms, and implications. Periodontol 2000. 2022;89:9–18.
Kim WJ, Soh Y, Heo SM. Recent advances of therapeutic targets for the treatment of periodontal disease. Biomol Ther (Seoul). 2021;29:263–7.
Sgolastra F, Petrucci A, Ciarrocchi I, Masci C, Spadaro A. Adjunctive systemic antimicrobials in the treatment of chronic periodontitis: a systematic review and network meta-analysis. J Periodontal Res. 2020;56:236–48.
Kherul Anuwar AH, Saub R, Safii SH, Ab-Murat N, Mohd Taib MS, Mamikutty R, Ng CW. Systemic antibiotics as an adjunct to subgingival debridement: a network meta-analysis. Antibiotics (Basel). 2022;11:1716.
Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:17038.
Wang L, Li Y, Ren M, Wang X, Li L, Liu F, Lan Y, Yang S, Song J. pH and lipase-responsive nanocarrier-mediated dual drug delivery system to treat periodontitis in diabetic rats. Bioact Mater. 2022;18:254–66.
Ding Y, Wang Y, Li J, Tang M, Chen H, Wang G, Guo J, Gui S. Microemulsion-thermosensitive gel composites as in situ-forming drug reservoir for periodontitis tissue repair through alveolar bone and collagen regeneration strategy. Pharm Dev Technol. 2023;28:30–9.
Wang Y, Li C, Wan Y, Qi M, Chen Q, Sun Y, Sun X, Fang J, Fu L, Xu L, et al. Quercetin-loaded ceria nanocomposite potentiate dual-directional immunoregulation via macrophage polarization against periodontal inflammation. Small. 2021;17:e2101505.
Tian Y, Li Y, Liu J, Lin Y, Jiao J, Chen B, Wang W, Wu S, Li C. Photothermal therapy with regulated Nrf2/NF-kappaB signaling pathway for treating bacteria-induced periodontitis. Bioact Mater. 2022;9:428–45.
Hajishengallis G, Chavakis T, Lambris JD. Current understanding of periodontal disease pathogenesis and targets for host-modulation therapy. Periodontol 2000. 2020;84:14–34.
Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018;16:745–59.
Abdulkareem AA, Al-Taweel FB, Al-Sharqi AJB, Gul SS, Sha A, Chapple ILC. Current concepts in the pathogenesis of periodontitis: from symbiosis to dysbiosis. J Oral Microbiol. 2023;15:2197779.
Pai SI, Matheus HR, Guastaldi FPS. Effects of periodontitis on cancer outcomes in the era of immunotherapy. Lancet Healthy Longev. 2023;4:e166–75.
Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner AC, Yu WH, Lakshmanan A, Wade WG. The human oral microbiome. J Bacteriol. 2010;192:5002–17.
Benoit DSW, Sims KR Jr, Fraser D. Nanoparticles for oral biofilm treatments. ACS Nano. 2019;13:4869–75.
Su X, Zhang J, Qin X. CD40 up-regulation on dendritic cells correlates with Th17/Treg imbalance in chronic periodontitis in young population. Innate Immun. 2020;26:482–9.
Wei Y, Deng Y, Ma S, Ran M, Jia Y, Meng J, Han F, Gou J, Yin T, He H, et al. Local drug delivery systems as therapeutic strategies against periodontitis: a systematic review. J Control Release. 2021;333:269–82.
Uriarte SM, Edmisson JS, Jimenez-Flores E. Human neutrophils and oral microbiota: a constant tug-of-war between a harmonious and a discordant coexistence. Immunol Rev. 2016;273:282–98.
Zhu Y, Winer D, Goh C, Shrestha A. Injectable thermosensitive hydrogel to modulate tolerogenic dendritic cells under hyperglycemic condition. Biomater Sci. 2023;11:2091–102.
Wilensky A, Segev H, Mizraji G, Shaul Y, Capucha T, Shacham M, Hovav AH. Dendritic cells and their role in periodontal disease. Oral Dis. 2014;20:119–26.
Zou J, Zeng Z, **e W, Zeng Z. Immunotherapy with regulatory T and B cells in periodontitis. Int Immunopharmacol. 2022;109:108797.
Arun KV, Talwar A, Kumar TS. T-helper cells in the etiopathogenesis of periodontal disease: a mini review. J Indian Soc Periodontol. 2011;15:4–10.
Jiang Q, Huang X, Yu W, Huang R, Zhao X, Chen C. mTOR signaling in the regulation of CD4+ T cell subsets in periodontal diseases. Front Immunol. 2022;13: 827461.
Kidd P. Th1/Th2 balance: the hypothesis, its limitations, and implications for health and disease. Altern Med Rev. 2003;8:223–46.
El-Awady AR, Elashiry M, Morandini AC, Meghil MM, Cutler CW. Dendritic cells a critical link to alveolar bone loss and systemic disease risk in periodontitis: immunotherapeutic implications. Periodontol 2000. 2022;89:41–50.
Meghil MM, Ghaly M, Cutler CW. A tale of two fimbriae: how invasion of dendritic cells by Porphyromonas gingivalis disrupts DC maturation and depolarizes the T-cell-mediated immune response. Pathogens. 2022;11:328.
Fu J, Huang Y, Bao T, Liu C, Liu X, Chen X. The role of Th17 cells/IL-17A in AD, PD, ALS and the strategic therapy targeting on IL-17A. J Neuroinflammation. 2022;19:98.
Zhang Z, Deng M, Hao M, Tang J. Periodontal ligament stem cells in the periodontitis niche: inseparable interactions and mechanisms. J Leukoc Biol. 2021;110:565–76.
Cafferata EA, Terraza-Aguirre C, Barrera R, Faundez N, Gonzalez N, Rojas C, Melgar-Rodriguez S, Hernandez M, Carvajal P, Cortez C, et al. Interleukin-35 inhibits alveolar bone resorption by modulating the Th17/Treg imbalance during periodontitis. J Clin Periodontol. 2020;47:676–88.
Cheng R, Wu Z, Li M, Shao M, Hu T. Interleukin-1beta is a potential therapeutic target for periodontitis: a narrative review. Int J Oral Sci. 2020;12:2.
Pan W, Wang Q, Chen Q. The cytokine network involved in the host immune response to periodontitis. Int J Oral Sci. 2019;11:30.
Vaquette C, Pilipchuk SP, Bartold PM, Hutmacher DW, Giannobile WV, Ivanovski S. Tissue engineered constructs for periodontal regeneration: current status and future perspectives. Adv Healthc Mater. 2018;7:e1800457.
Makabenta JMV, Nabawy A, Li CH, Schmidt-Malan S, Patel R, Rotello VM. Nanomaterial-based therapeutics for antibiotic-resistant bacterial infections. Nat Rev Microbiol. 2021;19:23–36.
Mi G, Shi D, Wang M, Webster TJ. Reducing bacterial infections and biofilm formation using nanoparticles and nanostructured antibacterial surfaces. Adv Healthc Mater. 2018;7:e1800103.
Mehta D, Saini V, Aggarwal B, Khan A, Bajaj A. Unlocking the bacterial membrane as a therapeutic target for next-generation antimicrobial amphiphiles. Mol Aspects Med. 2021;81:100999.
Guentsch A, Jentsch H, Pfister W, Hoffmann T, Eick S. Moxifloxacin as an adjunctive antibiotic in the treatment of severe chronic periodontitis. J Periodontol. 2008;79:1894–903.
Mudgil M, Pawar PK. Preparation and in vitro/ex vivo evaluation of moxifloxacin-loaded PLGA nanosuspensions for ophthalmic application. Sci Pharm. 2013;81:591–606.
Pinon-Segundo E, Ganem-Quintanar A, Alonso-Perez V, Quintanar-Guerrero D. Preparation and characterization of triclosan nanoparticles for periodontal treatment. Int J Pharm. 2005;294:217–32.
Yao W, Xu P, Pang Z, Zhao J, Chai Z, Li X, Li H, Jiang M, Cheng H, Zhang B, Cheng N. Local delivery of minocycline-loaded PEG-PLA nanoparticles for the enhanced treatment of periodontitis in dogs. Int J Nanomed. 2014;9:3963–70.
Beg S, Dhiman S, Sharma T, Jain A, Sharma RK, Jain A, Singh B. Stimuli responsive in situ gelling systems loaded with PLGA nanoparticles of moxifloxacin hydrochloride for effective treatment of periodontitis. AAPS PharmSciTech. 2020;21:76.
** Y, Wang Y, Gao J, **ao Y, Du J. Dual corona vesicles with intrinsic antibacterial and enhanced antibiotic delivery capabilities for effective treatment of biofilm-induced periodontitis. ACS Nano. 2019;13:13645–57.
Gold K, Slay B, Knackstedt M, Gaharwar AK. Antimicrobial activity of metal and metal-oxide based nanoparticles. Adv Therap. 2018;1:1700033.
Wang Y, Malkmes MJ, Jiang C, Wang P, Zhu L, Zhang H, Zhang Y, Huang H, Jiang L. Antibacterial mechanism and transcriptome analysis of ultra-small gold nanoclusters as an alternative of harmful antibiotics against Gram-negative bacteria. J Hazard Mater. 2021;416:126236.
Zhang Y, Chen R, Wang Y, Wang P, Pu J, Xu X, Chen F, Jiang L, Jiang Q, Yan F. Antibiofilm activity of ultra-small gold nanoclusters against Fusobacterium nucleatum in dental plaque biofilms. J Nanobiotechnol. 2022;20:470.
Amna T, Hassan MS, Sheikh FA, Lee HK, Seo KS, Yoon D, Hwang IH. Zinc oxide-doped poly(urethane) spider web nanofibrous scaffold via one-step electrospinning: a novel matrix for tissue engineering. Appl Microbiol Biotechnol. 2013;97:1725–34.
Anitha S, Brabu B, John Thiruvadigal D, Gopalakrishnan C, Natarajan TS. Optical, bactericidal and water repellent properties of electrospun nano-composite membranes of cellulose acetate and ZnO. Carbohydr Polym. 2013;97:856–63.
Kasraei S, Sami L, Hendi S, Alikhani MY, Rezaei-Soufi L, Khamverdi Z. Antibacterial properties of composite resins incorporating silver and zinc oxide nanoparticles on Streptococcus mutans and Lactobacillus. Restor Dent Endod. 2014;39:109–14.
Krol A, Pomastowski P, Rafinska K, Railean-Plugaru V, Buszewski B. Zinc oxide nanoparticles: synthesis, antiseptic activity and toxicity mechanism. Adv Colloid Interface Sci. 2017;249:37–52.
Liu Y, He L, Mustapha A, Li H, Hu ZQ, Lin M. Antibacterial activities of zinc oxide nanoparticles against Escherichia coli O157:H7. J Appl Microbiol. 2009;107:1193–201.
Sirelkhatim A, Mahmud S, Seeni A, Kaus NHM, Ann LC, Bakhori SKM, Hasan H, Mohamad D. Review on zinc oxide nanoparticles: antibacterial activity and toxicity mechanism. Nanomicro Lett. 2015;7:219–42.
Adams LK, Lyon DY, Alvarez PJJ. Comparative eco-toxicity of nanoscale TiO2, SiO2, and ZnO water suspensions. Water Res. 2006;40:3527–32.
Pasquet J, Chevalier Y, Pelletier J, Couval E, Bouvier D, Bolzinger M-A. The contribution of zinc ions to the antimicrobial activity of zinc oxide. Colloids Surf A Physicochem Eng Asp. 2014;457:263–74.
Sanchez-Lopez E, Gomes D, Esteruelas G, Bonilla L, Lopez-Machado AL, Galindo R, Cano A, Espina M, Ettcheto M, Camins A, et al. Metal-based nanoparticles as antimicrobial agents: an overview. Nanomaterials (Basel). 2020;10:292.
Lakshmi Prasanna V, Vijayaraghavan R. Insight into the mechanism of antibacterial activity of ZnO: surface defects mediated reactive oxygen species even in the dark. Langmuir. 2015;31:9155–62.
Madhumitha G, Elango G, Roopan SM. Biotechnological aspects of ZnO nanoparticles: overview on synthesis and its applications. Appl Microbiol Biotechnol. 2016;100:571–81.
Munchow EA, Albuquerque MT, Zero B, Kamocki K, Piva E, Gregory RL, Bottino MC. Development and characterization of novel ZnO-loaded electrospun membranes for periodontal regeneration. Dent Mater. 2015;31:1038–51.
Augustine R, Dominic EA, Reju I, Kaimal B, Kalarikkal N, Thomas S. Electrospun polycaprolactone membranes incorporated with ZnO nanoparticles as skin substitutes with enhanced fibroblast proliferation and wound healing. RSC Adv. 2014;4:24777–85.
Dias AM, da Silva FG, Monteiro APF, Pinzon-Garcia AD, Sinisterra RD, Cortes ME. Polycaprolactone nanofibers loaded oxytetracycline hydrochloride and zinc oxide for treatment of periodontal disease. Mater Sci Eng C Mater Biol Appl. 2019;103:109798.
Mou J, Liu Z, Liu J, Lu J, Zhu W, Pei D. Hydrogel containing minocycline and zinc oxide-loaded serum albumin nanopartical for periodontitis application: preparation, characterization and evaluation. Drug Deliv. 2019;26:179–87.
Chen Y, Gao Y, Chen Y, Liu L, Mo A, Peng Q. Nanomaterials-based photothermal therapy and its potentials in antibacterial treatment. J Control Release. 2020;328:251–62.
Zheng Y, Wei M, Wu H, Li F, Ling D. Antibacterial metal nanoclusters. J Nanobiotechnol. 2022;20:328.
Lin J, He Z, Liu F, Feng J, Huang C, Sun X, Deng H. Hybrid hydrogels for synergistic periodontal antibacterial treatment with sustained drug release and NIR-responsive photothermal effect. Int J Nanomed. 2020;15:5377–87.
Zhong Y, Zheng XT, Zhao S, Su X, Loh XJ. Stimuli-activable metal-bearing nanomaterials and precise on-demand antibacterial strategies. ACS Nano. 2022;16:19840–72.
Jia Q, Song Q, Li P, Huang W. Rejuvenated photodynamic therapy for bacterial infections. Adv Healthc Mater. 2019;8:e1900608.
Zhao J, Zhang Y, Zhang J, Wu H, Li J, Zhao Y, Zhang L, Zou D, Li Z, Wang S. Synthetic and biodegradable molybdenum(IV) diselenide triggers the cascade photo- and immunotherapy of tumor. Adv Healthc Mater. 2022;11:2200524.
Fu X, Yang Z, Deng T, Chen J, Wen Y, Fu X, Zhou L, Zhu Z, Yu C. A natural polysaccharide mediated MOF-based Ce6 delivery system with improved biological properties for photodynamic therapy. J Mater Chem B. 2020;8:1481–8.
Sun X, Wang L, Lynch CD, Sun X, Li X, Qi M, Ma C, Li C, Dong B, Zhou Y, Xu HHK. Nanoparticles having amphiphilic silane containing Chlorin e6 with strong anti-biofilm activity against periodontitis-related pathogens. J Dent. 2019;81:70–84.
Zhang T, Ying D, Qi M, Li X, Fu L, Sun X, Wang L, Zhou Y. Anti-biofilm property of bioactive upconversion nanocomposites containing chlorin e6 against periodontal pathogens. Molecules. 2019;24:2692.
Chen B, Dong B, Wang J, Zhang S, Xu L, Yu W, Song H. Amphiphilic silane modified NaYF4:Yb, Er loaded with Eu(TTA)3(TPPO)2 nanoparticles and their multi-functions: dual mode temperature sensing and cell imaging. Nanoscale. 2013;5:8541–9.
Li Z, Pan W, Shi E, Bai L, Liu H, Li C, Wang Y, Deng J, Wang Y. A multifunctional nanosystem based on bacterial cell-penetrating photosensitizer for fighting periodontitis via combining photodynamic and antibiotic therapies. ACS Biomater Sci Eng. 2021;7:772–86.
Zhang H, Zhang X, Zhu X, Chen J, Chen Q, Zhang H, Hou L, Zhang Z. NIR light-induced tumor phototherapy using photo-stable ICG delivery system based on inorganic hybrid. Nanomedicine. 2018;14:73–84.
Nagahara A, Mitani A, Fukuda M, Yamamoto H, Tahara K, Morita I, Ting CC, Watanabe T, Fujimura T, Osawa K, et al. Antimicrobial photodynamic therapy using a diode laser with a potential new photosensitizer, indocyanine green-loaded nanospheres, may be effective for the clearance of Porphyromonas gingivalis. J Periodontal Res. 2013;48:591–9.
Shi E, Bai L, Mao L, Wang H, Yang X, Wang Y, Zhang M, Li C, Wang Y. Self-assembled nanoparticles containing photosensitizer and polycationic brush for synergistic photothermal and photodynamic therapy against periodontitis. J Nanobiotechnol. 2021;19:413.
Yang B, Pang X, Li Z, Chen Z, Wang Y. Immunomodulation in the treatment of periodontitis: progress and perspectives. Front Immunol. 2021;12:781378.
Balta MG, Papathanasiou E, Blix IJ, Van Dyke TE. Host modulation and treatment of periodontal disease. J Dent Res. 2021;100:798–809.
Xu XW, Liu X, Shi C, Sun HC. Roles of immune cells and mechanisms of immune responses in periodontitis. Chin J Dent Res. 2021;24:219–30.
Sun X, Gao J, Meng X, Lu X, Zhang L, Chen R. Polarized macrophages in periodontitis: characteristics, function, and molecular signaling. Front Immunol. 2021;12:763334.
Funes SC, Rios M, Escobar-Vera J, Kalergis AM. Implications of macrophage polarization in autoimmunity. Immunology. 2018;154:186–95.
Boutilier AJ, Elsawa SF. Macrophage polarization states in the tumor microenvironment. Int J Mol Sci. 2021;22:6995.
Chanmee T, Ontong P, Konno K, Itano N. Tumor-associated macrophages as major players in the tumor microenvironment. Cancers (Basel). 2014;6:1670–90.
Huang X, Li Y, Fu M, **n H-B. Polarizing macrophages in vitro. In: Rousselet G, editor. Macrophages. Methods in molecular biology. New York: Springer; 2018. p. 119–26.
Wang LX, Zhang SX, Wu HJ, Rong XL, Guo J. M2b macrophage polarization and its roles in diseases. J Leukoc Biol. 2019;106:345–58.
Shi J, Zhang Y, Zhang X, Chen R, Wei J, Hou J, Wang B, Lai H, Huang Y. Remodeling immune microenvironment in periodontitis using resveratrol liposomes as an antibiotic-free therapeutic strategy. J Nanobiotechnol. 2021;19:429.
Shen Z, Kuang S, Zhang Y, Yang M, Qin W, Shi X, Lin Z. Chitosan hydrogel incorporated with dental pulp stem cell-derived exosomes alleviates periodontitis in mice via a macrophage-dependent mechanism. Bioact Mater. 2020;5:1113–26.
Figueiredo RDA, Ortega AC, Gonzalez Maldonado LA, Castro RD, Avila-Campos MJ, Rossa C, Aquino SG. Perillyl alcohol has antibacterial effects and reduces ROS production in macrophages. J Appl Oral Sci. 2020;28:e20190519.
Kim J, Kim HY, Song SY, Go SH, Sohn HS, Baik S, Soh M, Kim K, Kim D, Kim HC, et al. Synergistic oxygen generation and reactive oxygen species scavenging by manganese ferrite/ceria co-decorated nanoparticles for rheumatoid arthritis treatment. ACS Nano. 2019;13:3206–17.
Yang B, Chen Y, Shi J. Reactive oxygen species (ROS)-based nanomedicine. Chem Rev. 2019;119:4881–985.
Deng J, Lu C, Zhao Q, Chen K, Ma S, Li Z. The Th17/Treg cell balance: crosstalk among the immune system, bone and microbes in periodontitis. J Periodontal Res. 2022;57:246–55.
Kini V, Mohanty I, Telang G, Vyas N. Immunopathogenesis and distinct role of Th17 in periodontitis: a review. J Oral Biosci. 2022;64:193–201.
Mousset CM, Hobo W, Woestenenk R, Preijers F, Dolstra H, van der Waart AB. Comprehensive phenoty** of T cells using flow cytometry. Cytometry A. 2019;95:647–54.
Gaffen SL, Moutsopoulos NM. Regulation of host–microbe interactions at oral mucosal barriers by type 17 immunity. Sci Immunol. 2020;5:eaau4594.
Karthikeyan B. Talwar, Arun KV, Kalaivani S: Evaluation of transcription factor that regulates T helper 17 and regulatory T cells function in periodontal health and disease. J Pharm Bioallied Sci. 2015;7:S672-676.
Zhang Y, Chen J, Fu H, Kuang S, He F, Zhang M, Shen Z, Qin W, Lin Z, Huang S. Exosomes derived from 3D-cultured MSCs improve therapeutic effects in periodontitis and experimental colitis and restore the Th17 cell/Treg balance in inflamed periodontium. Int J Oral Sci. 2021;13:43.
Zheng Y, Dong C, Yang J, ** Y, Zheng W, Zhou Q, Liang Y, Bao L, Feng G, Ji J, et al. Exosomal microRNA-155-5p from PDLSCs regulated Th17/Treg balance by targeting sirtuin-1 in chronic periodontitis. J Cell Physiol. 2019;234:20662–74.
Prasad R, Suchetha A, Lakshmi P, Darshan MB, Apoorva SM, Ashit GB. Interleukin-11 - its role in the vicious cycle of inflammation, periodontitis and diabetes: a clinicobiochemical cross-sectional study. J Indian Soc Periodontol. 2015;19:159–63.
Toker H, Gorgun EP, Korkmaz EM, Yuce HB, Poyraz O. The effects of IL-10 gene polymorphism on serum, and gingival crevicular fluid levels of IL-6 and IL-10 in chronic periodontitis. J Appl Oral Sci. 2018;26:e20170232.
Zhang Q, Chen B, Yan F, Guo J, Zhu X, Ma S, Yang W. Interleukin-10 inhibits bone resorption: a potential therapeutic strategy in periodontitis and other bone loss diseases. Biomed Res Int. 2014;2014:284836.
Li X, Luo W, Ng TW, Leung PC, Zhang C, Leung KC, ** L. Nanoparticle-encapsulated baicalein markedly modulates pro-inflammatory response in gingival epithelial cells. Nanoscale. 2017;9:12897–907.
Bao X, Zhao J, Sun J, Hu M, Yang X. Polydopamine nanoparticles as efficient scavengers for reactive oxygen species in periodontal disease. ACS Nano. 2018;12:8882–92.
Liu X, He X, ** D, Wu S, Wang H, Yin M, Aldalbahi A, El-Newehy M, Mo X, Wu J. A biodegradable multifunctional nanofibrous membrane for periodontal tissue regeneration. Acta Biomater. 2020;108:207–22.
Liang Y, Luan X, Liu X. Recent advances in periodontal regeneration: a biomaterial perspective. Bioact Mater. 2020;5:297–308.
Liu J, Wang H, Zhang L, Li X, Ding X, Ding G, Wei F. Periodontal ligament stem cells promote polarization of M2 macrophages. J Leukoc Biol. 2022;111:1185–97.
Lee JS, Lee JB, Cha JK, Choi EY, Park SY, Cho KS, Kim CS. Chemokine in inflamed periodontal tissues activates healthy periodontal-ligament stem cell migration. J Clin Periodontol. 2017;44:530–9.
Zhou M, Liu N, Zhang Q, Tian T, Ma Q, Zhang T, Cai X. Effect of tetrahedral DNA nanostructures on proliferation and osteogenic differentiation of human periodontal ligament stem cells. Cell Prolif. 2019;52:e12566.
Li C, Li Z, Zhang Y, Fathy AH, Zhou M. The role of the Wnt/beta-catenin signaling pathway in the proliferation of gold nanoparticle-treated human periodontal ligament stem cells. Stem Cell Res Ther. 2018;9:214.
Zhang S, Zhou H, Kong N, Wang Z, Fu H, Zhang Y, **ao Y, Yang W, Yan F. l-cysteine-modified chiral gold nanoparticles promote periodontal tissue regeneration. Bioact Mater. 2021;6:3288–99.
Liu J, Dai Q, Weir MD, Schneider A, Zhang C, Hack GD, Oates TW, Zhang K, Li A, Xu HHK. Biocompatible nanocomposite enhanced osteogenic and cementogenic differentiation of periodontal ligament stem cells in vitro for periodontal regeneration. Materials (Basel). 2020;13:4951.
**e L, Chen J, Ren X, Zhang M, Thuaksuban N, Nuntanaranont T, Guan Z. Alteration of circRNA and lncRNA expression profile in exosomes derived from periodontal ligament stem cells undergoing osteogenic differentiation. Arch Oral Biol. 2021;121:104984.
Zhang Z, Shuai Y, Zhou F, Yin J, Hu J, Guo S, Wang Y, Liu W. PDLSCs regulate angiogenesis of periodontal ligaments via VEGF transferred by exosomes in periodontitis. Int J Med Sci. 2020;17:558–67.
Lei F, Li M, Lin T, Zhou H, Wang F, Su X. Treatment of inflammatory bone loss in periodontitis by stem cell-derived exosomes. Acta Biomater. 2022;141:333–43.
Liu W, Konermann A, Guo T, Jager A, Zhang L, ** Y. Canonical Wnt signaling differently modulates osteogenic differentiation of mesenchymal stem cells derived from bone marrow and from periodontal ligament under inflammatory conditions. Biochim Biophys Acta. 2014;1840:1125–34.
Calabrese EJ. Hormesis and bone marrow stem cells: enhancing cell proliferation, differentiation and resilience to inflammatory stress. Chem Biol Interact. 2022;351:109730.
Wang Y, Li J, Zhou J, Qiu Y, Song J. Low-intensity pulsed ultrasound enhances bone marrow-derived stem cells-based periodontal regenerative therapies. Ultrasonics. 2022;121:106678.
Lu L, Liu Y, Zhang X, Lin J. The therapeutic role of bone marrow stem cell local injection in rat experimental periodontitis. J Oral Rehabil. 2020;47(Suppl 1):73–82.
Shen R, Xu W, Xue Y, Chen L, Ye H, Zhong E, Ye Z, Gao J, Yan Y. The use of chitosan/PLA nano-fibers by emulsion eletrospinning for periodontal tissue engineering. Artif Cells Nanomed Biotechnol. 2018;46:419–30.
Ye Z, Xu W, Shen R, Yan Y. Emulsion electrospun PLA/calcium alginate nanofibers for periodontal tissue engineering. J Biomater Appl. 2020;34:763–77.
AlQranei MS, Chellaiah MA. Osteoclastogenesis in periodontal diseases: possible mediators and mechanisms. J Oral Biosci. 2020;62:123–30.
Kitaura H, Marahleh A, Ohori F, Noguchi T, Shen WR, Qi J, Nara Y, Pramusita A, Kinjo R, Mizoguchi I. Osteocyte-related cytokines regulate osteoclast formation and bone resorption. Int J Mol Sci. 2020;21:5169.
Chen X, Wan Z, Yang L, Song S, Fu Z, Tang K, Chen L, Song Y. Exosomes derived from reparative M2-like macrophages prevent bone loss in murine periodontitis models via IL-10 mRNA. J Nanobiotechnol. 2022;20:110.
Bakheet SA, Alrwashied BS, Ansari MA, Nadeem A, Attia SM, Alanazi MM, Aldossari AA, Assiri MA, Mahmood HM, Al-Mazroua HA, Ahmad SF. CXC chemokine receptor 3 antagonist AMG487 shows potent anti-arthritic effects on collagen-induced arthritis by modifying B cell inflammatory profile. Immunol Lett. 2020;225:74–81.
Hiyari S, Green E, Pan C, Lari S, Davar M, Davis R, Camargo PM, Tetradis S, Lusis AJ, Pirih FQ. Genomewide association study identifies Cxcl family members as partial mediators of LPS-induced periodontitis. J Bone Miner Res. 2018;33:1450–63.
Cui ZK, Bastiat G, ** C, Keyvanloo A, Lafleur M. Influence of the nature of the sterol on the behavior of palmitic acid/sterol mixtures and their derived liposomes. Biochim Biophys Acta. 2010;1798:1144–52.
Lari S, Hiyari S, de Araujo Silva DN, de Brito BB, Ishii M, Monajemzadeh S, Cui ZK, Tetradis S, Lee M, Pirih FQ. Local delivery of a CXCR3 antagonist decreases the progression of bone resorption induced by LPS injection in a murine model. Clin Oral Investig. 2022;26:5163–9.
Menicanin D, Hynes K, Han J, Gronthos S, Bartold PM. Cementum and periodontal ligament regeneration. Adv Exp Med Biol. 2015;881:207–36.
Bozbay E, Dominici F, Gokbuget AY, Cintan S, Guida L, Aydin MS, Mariotti A, Pilloni A. Preservation of root cementum: a comparative evaluation of power-driven versus hand instruments. Int J Dent Hyg. 2018;16:202–9.
Wang H, Wang X, Ma L, Huang X, Peng Y, Huang H, Gao X, Chen Y, Cao Z. PGC-1 alpha regulates mitochondrial biogenesis to ameliorate hypoxia-inhibited cementoblast mineralization. Ann N Y Acad Sci. 2022;1516:300–11.
Wang Y, Li Y, Shao P, Wang L, Bao X, Hu M. IL1beta inhibits differentiation of cementoblasts via microRNA-325-3p. J Cell Biochem. 2020;121:2606–17.
Park CH, Oh JH, Jung HM, Choi Y, Rahman SU, Kim S, Kim TI, Shin HI, Lee YS, Yu FH, et al. Effects of the incorporation of epsilon-aminocaproic acid/chitosan particles to fibrin on cementoblast differentiation and cementum regeneration. Acta Biomater. 2017;61:134–43.
Chen E, Wang T, Tu Y, Sun Z, Ding Y, Gu Z, **ao S. ROS-scavenging biomaterials for periodontitis. J Mater Chem B. 2023;11:482–99.
Wang H, Wang D, Huangfu H, Lv H, Qin Q, Ren S, Zhang Y, Wang L, Zhou Y. Branched AuAg nanoparticles coated by metal–phenolic networks for treating bacteria-induced periodontitis via photothermal antibacterial and immunotherapy. Mater Des. 2022;224:111401.
Yan N, Xu J, Liu G, Ma C, Bao L, Cong Y, Wang Z, Zhao Y, Xu W, Chen C. Penetrating macrophage-based nanoformulation for periodontitis treatment. ACS Nano. 2022;16:18253–65.
Chen J, Zhang X, Huang C, Cai H, Hu S, Wan Q, Pei X, Wang J. Osteogenic activity and antibacterial effect of porous titanium modified with metal-organic framework films. J Biomed Mater Res A. 2017;105:834–46.
Zhong L, Chen J, Ma Z, Feng H, Chen S, Cai H, Xue Y, Pei X, Wang J, Wan Q. 3D printing of metal-organic framework incorporated porous scaffolds to promote osteogenic differentiation and bone regeneration. Nanoscale. 2020;12:24437–49.
Sun M, Liu Y, Jiao K, Jia W, Jiang K, Cheng Z, Liu G, Luo Y. A periodontal tissue regeneration strategy via biphasic release of zeolitic imidazolate framework-8 and FK506 using a uniaxial electrospun Janus nanofiber. J Mater Chem B. 2022;10:765–78.
Liu Y, Zhu Z, Pei X, Zhang X, Cheng X, Hu S, Gao X, Wang J, Chen J, Wan Q. ZIF-8-modified multifunctional bone-adhesive hydrogels promoting angiogenesis and osteogenesis for bone regeneration. ACS Appl Mater Interfaces. 2020;12:36978–95.
Xue Y, Zhu Z, Zhang X, Chen J, Yang X, Gao X, Zhang S, Luo F, Wang J, Zhao W, et al. Accelerated bone regeneration by MOF modified multifunctional membranes through enhancement of osteogenic and angiogenic performance. Adv Healthc Mater. 2021;10:e2001369.
Liu Y, Li T, Sun M, Cheng Z, Jia W, Jiao K, Wang S, Jiang K, Yang Y, Dai Z, et al. ZIF-8 modified multifunctional injectable photopolymerizable GelMA hydrogel for the treatment of periodontitis. Acta Biomater. 2022;146:37–48.
Dong Z, Lin Y, Xu S, Chang L, Zhao X, Mei X, Gao X. NIR-triggered tea polyphenol-modified gold nanoparticles-loaded hydrogel treats periodontitis by inhibiting bacteria and inducing bone regeneration. Mater Des. 2023;225:111487.
Burghardt I, Lüthen F, Prinz C, Kreikemeyer B, Zietz C, Neumann H-G, Rychly J. A dual function of copper in designing regenerative implants. Biomaterials. 2015;44:36–44.
Xu Y, Zhao S, Weng Z, Zhang W, Wan X, Cui T, Ye J, Liao L, Wang X. Jelly-inspired injectable guided tissue regeneration strategy with shape auto-matched and dual-light-defined antibacterial/osteogenic pattern switch properties. ACS Appl Mater Interfaces. 2020;12:54497–506.
Liu J, Ouyang Y, Zhang Z, Wen S, Pi Y, Chen D, Su Z, Liang Z, Guo L, Wang Y. The role of Th17 cells: explanation of relationship between periodontitis and COPD? Inflamm Res. 2022;71:1011–24.
Beklen A, Ainola M, Hukkanen M, Gurgan C, Sorsa T, Konttinen YT. MMPs, IL-1, and TNF are regulated by IL-17 in periodontitis. J Dent Res. 2007;86:347–51.
Cavalla F, Hernandez M. Polarization profiles of T lymphocytes and macrophages responses in periodontitis. Adv Exp Med Biol. 2022;1373:195–208.
Papathanasiou E, Conti P, Carinci F, Lauritano D, Theoharides TC. IL-1 superfamily members and periodontal diseases. J Dent Res. 2020;99:1425–34.
Plemmenos G, Evangeliou E, Polizogopoulos N, Chalazias A, Deligianni M, Piperi C. Central regulatory role of cytokines in periodontitis and targeting options. Curr Med Chem. 2021;28:3032–58.
Ni C, Zhou J, Kong N, Bian T, Zhang Y, Huang X, **ao Y, Yang W, Yan F. Gold nanoparticles modulate the crosstalk between macrophages and periodontal ligament cells for periodontitis treatment. Biomaterials. 2019;206:115–32.
Qiu X, Yu Y, Liu H, Li X, Sun W, Wu W, Liu C, Miao L. Remodeling the periodontitis microenvironment for osteogenesis by using a reactive oxygen species-cleavable nanoplatform. Acta Biomater. 2021;135:593–605.
Li S, Wang L, Gu Y, Lin L, Zhang M, ** M, Mao C, Zhou J, Zhang W, Huang X, et al. Biomimetic immunomodulation by crosstalk with nanoparticulate regulatory T cells. Matter. 2021;4:3621–45.
Sun Y, Sun X, Li X, Li W, Li C, Zhou Y, Wang L, Dong B. A versatile nanocomposite based on nanoceria for antibacterial enhancement and protection from aPDT-aggravated inflammation via modulation of macrophage polarization. Biomaterials. 2021;268:120614.
Zhang Y, Wang X, Li H, Ni C, Du Z, Yan F. Human oral microbiota and its modulation for oral health. Biomed Pharmacother. 2018;99:883–93.
Fan R, Zhou Y, Chen X, Zhong X, He F, Peng W, Li L, Wang X, Xu Y. Porphyromonas gingivalis outer membrane vesicles promote apoptosis via msRNA-regulated DNA methylation in periodontitis. Microbiol Spectr. 2023;11:e0328822.
Bustamante M, Oomah BD, Mosi-Roa Y, Rubilar M, Burgos-Diaz C. Probiotics as an adjunct therapy for the treatment of halitosis, dental caries and periodontitis. Probiotics Antimicrob Proteins. 2020;12:325–34.
Zidar A, Kristl J, Kocbek P, Zupancic S. Treatment challenges and delivery systems in immunomodulation and probiotic therapies for periodontitis. Expert Opin Drug Deliv. 2021;18:1229–44.
Wang J, Liu Y, Wang W, Ma J, Zhang M, Lu X, Liu J, Kou Y. The rationale and potential for using Lactobacillus in the management of periodontitis. J Microbiol. 2022;60:355–63.
Jung JI, Kim YG, Kang CH, Imm JY. Effects of Lactobacillus curvatus MG5246 on inflammatory markers in Porphyromonas gingivalis lipopolysaccharide-sensitized human gingival fibroblasts and periodontitis rat model. Food Sci Biotechnol. 2022;31:111–20.
Esteban-Fernández A, Ferrer MD, Zorraquín-Peña I, López-López A. Mira MVM-AA: in vitro beneficial effects of Streptococcus dentisani as potencial oral probiotic for periodontal diseases. J Periodontol. 2019;90:1346–55.
Mittal M, Siddiqui MR, Tran K, Reddy SP, Malik AB. Reactive oxygen species in inflammation and tissue injury. Antioxid Redox Signal. 2014;20:1126–67.
Tan DQ, Suda T. Reactive oxygen species and mitochondrial homeostasis as regulators of stem cell fate and function. Antioxid Redox Signal. 2018;29:149–68.
Del Castillo LF, Schlegel Gomez R, Pelka M, Hornstein OP, Johannessen AC, von den Driesch P. Immunohistochemical localization of very late activation integrins in healthy and diseased human gingiva. J Periodontal Res. 1996;31:36–42.
Haapasalmi K, Mäkelä M, Oksala O, Heino J, Yamada KM, Uitto VJ, Larjava H. Expression of epithelial adhesion proteins and integrins in chronic inflammation. Am J Pathol. 1995;147:193.
Hersel U, Dahmen C, Kessler H. RGD modified polymers: biomaterials for stimulated cell adhesion and beyond. Biomaterials. 2003;24:4385–415.
Ruoslahti E. RGD and other recognition sequences for integrins. Annu Rev Cell Dev Biol. 1996;12:697–715.
Yao W, Xu P, Zhao J, Ling L, Li X, Zhang B, Cheng N, Pang Z. RGD functionalized polymeric nanoparticles targeting periodontitis epithelial cells for the enhanced treatment of periodontitis in dogs. J Colloid Interface Sci. 2015;458:14–21.
He XT, Li X, Zhang M, Tian BM, Sun LJ, Bi CS, Deng DK, Zhou H, Qu HL, Wu C, Chen FM. Role of molybdenum in material immunomodulation and periodontal wound healing: targeting immunometabolism and mitochondrial function for macrophage modulation. Biomaterials. 2022;283:121439.
Wang G, Peng C, Tang M, Wang Y, Li J, Chen H, Chang X, Shu Z, He N, Guo J, Gui S. Simultaneously boosting inflammation resolution and osteogenic differentiation in periodontitis using folic acid-modified liposome-thermosensitive hydrogel composites. Mater Des. 2023;234:112314.
Wang Y, Li J, Tang M, Peng C, Wang G, Wang J, Wang X, Chang X, Guo J, Gui S. Smart stimuli-responsive hydrogels for drug delivery in periodontitis treatment. Biomed Pharmacother. 2023;162:114688.
Li N, **e L, Wu Y, Wu Y, Liu Y, Gao Y, Yang J, Zhang X, Jiang L. Dexamethasone-loaded zeolitic imidazolate frameworks nanocomposite hydrogel with antibacterial and anti-inflammatory effects for periodontitis treatment. Mater Today Bio. 2022;16:100360.
Tang J, Yi W, Yan J, Chen Z, Fan H, Zaldivar-Silva D, Agüero L, Wang S. Highly absorbent bio-sponge based on carboxymethyl chitosan/poly-γ-glutamic acid/platelet-rich plasma for hemostasis and wound healing. Int J Biol Macromol. 2023;247:125754.
Chew JRJ, Chuah SJ, Teo KYW, Zhang S, Lai RC, Fu JH, Lim LP, Lim SK, Toh WS. Mesenchymal stem cell exosomes enhance periodontal ligament cell functions and promote periodontal regeneration. Acta Biomater. 2019;89:252–64.
Zhang X, Zhao J, **e P, Wang S. Biomedical applications of electrets: recent advance and future perspectives. J Funct Biomater. 2023;14:320.
Yu B, Qiao Z, Cui J, Lian M, Han Y, Zhang X, Wang W, Yu X, Yu H, Wang X, Lin K. A host-coupling bio-nanogenerator for electrically stimulated osteogenesis. Biomater. 2021;276:120997.
Gonzalez-Febles J, Sanz M. Periodontitis and rheumatoid arthritis: what have we learned about their connection and their treatment? Periodontol 2000. 2021;87:181–203.
Ray RR. Periodontitis: an oral disease with severe consequences. Appl Biochem Biotechnol. 2023;195:17–32.
Newman KL, Kamada N. Pathogenic associations between oral and gastrointestinal diseases. Trends Mol Med. 2022;28:1030–9.
Li B, **n Z, Gao S, Li Y, Guo S, Fu Y, Xu R, Wang D, Cheng J, Liu L, et al. SIRT6-regulated macrophage efferocytosis epigenetically controls inflammation resolution of diabetic periodontitis. Theranostics. 2023;13:231–49.
Guru SR, Aghanashini S. Impact of scaling and root planing on salivary and serum plasminogen activator inhibitor-1 expression in patients with periodontitis with and without type 2 diabetes mellitus. J Periodontol. 2023;94:20–30.
Wu CZ, Yuan YH, Liu HH, Li SS, Zhang BW, Chen W, An ZJ, Chen SY, Wu YZ, Han B, et al. Epidemiologic relationship between periodontitis and type 2 diabetes mellitus. BMC Oral Health. 2020;20:204.
Zhao X, Yang Y, Yu J, Ding R, Pei D, Zhang Y, He G, Cheng Y, Li A. Injectable hydrogels with high drug loading through B-N coordination and ROS-triggered drug release for efficient treatment of chronic periodontitis in diabetic rats. Biomaterials. 2022;282:121387.
Wang H, Chang X, Ma Q, Sun B, Li H, Zhou J, Hu Y, Yang X, Li J, Chen X, Song J. Bioinspired drug-delivery system emulating the natural bone healing cascade for diabetic periodontal bone regeneration. Bioact Mater. 2023;21:324–39.
Hajishengallis G, Chavakis T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021;21:426–40.
Inchingolo AD, Inchingolo AM, Malcangi G, Avantario P, Azzollini D, Buongiorno S, Viapiano F, Campanelli M, Ciocia AM, De Leonardis N, et al. Effects of resveratrol, curcumin and quercetin supplementation on bone metabolism—a systematic review. Nutrients. 2022;14:3519.
Cao JH, Xue R, He B. Quercetin protects oral mucosal keratinocytes against lipopolysaccharide-induced inflammatory toxicity by suppressing the AKT/AMPK/mTOR pathway. Immunopharmacol Immunotoxicol. 2021;43:519–26.
Taskan MM, Gevrek F. Quercetin decreased alveolar bone loss and apoptosis in experimentally induced periodontitis model in wistar rats. Antiinflamm Antiallergy Agents Med Chem. 2020;19:436–48.
Bhattarai G, Poudel SB, Kook SH, Lee JC. Resveratrol prevents alveolar bone loss in an experimental rat model of periodontitis. Acta Biomater. 2016;29:398–408.
Li Y, Jiao J, Qi Y, Yu W, Yang S, Zhang J, Zhao J. Curcumin: a review of experimental studies and mechanisms related to periodontitis treatment. J Periodontal Res. 2021;56:837–47.
Zheng XY, Mao CY, Qiao H, Zhang X, Yu L, Wang TY, Lu EY. Plumbagin suppresses chronic periodontitis in rats via down-regulation of TNF-alpha, IL-1beta and IL-6 expression. Acta Pharmacol Sin. 2017;38:1150–60.
Acknowledgements
This research was financially supported by the National Natural Science Foundation of China (No. 81873019), the Anhui Province University Leading Talents Team (No. 6), the Key Project of Natural Science Research in Universities of Anhui Province (KJ2021A0538, 2023AH050785), the High- level Talent Support Program of Anhui University of Chinese Medicine (No. 2022rczd003), and the Postgraduate Education Foundation of College of Pharmacy of Anhui University of Chinese Medicine (No. 21pyjj05).
Author information
Authors and Affiliations
Contributions
JL wrote the original article; JL, YW and MT draw the pictures; JL, YF, CZ and ML acquired the date; ML, SG and JG contributed with critical revisions and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Wang, Y., Tang, M. et al. New insights into nanotherapeutics for periodontitis: a triple concerto of antimicrobial activity, immunomodulation and periodontium regeneration. J Nanobiotechnol 22, 19 (2024). https://doi.org/10.1186/s12951-023-02261-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12951-023-02261-y