Abstract
Spinal cord injury (SCI) is accompanied by loss of Zn2+, which is an important cause of glutamate excitotoxicity and death of local neurons as well as transplanted stem cells. Dental pulp stem cells (DPSCs) have the potential for neural differentiation and play an immunomodulatory role in the microenvironment, making them an ideal cell source for the repair of central nerve injury, including SCI. The zeolitic imidazolate framework 8 (ZIF-8) is usually used as a drug and gene delivery carrier, which can release Zn2+ sustainedly in acidic environment. However, the roles of ZIF-8 on neural differentiation of DPSCs and the effect of combined treatment on SCI have not been explored. ZIF-8-introduced DPSCs were loaded into gelatin methacryloyl (GelMA) hydrogel and in situ injected into the injured site of SCI rats. Under the effect of ZIF-8, axon number and axon length of DPSCs-differentiated neuro-like cells were significantly increased. In addition, ZIF-8 protected transplanted DPSCs from apoptosis in the damaged microenvironment. ZIF-8 promotes neural differentiation and angiogenesis of DPSCs by activating the Mitogen-activated protein kinase (MAPK) signaling pathway, which is a promising transport nanomaterial for nerve repair.
Similar content being viewed by others
Introduction
Globally, 250,000 to 500,000 people suffer from spinal cord injury (SCI) each year, mainly caused by traumatic events, as well as infections, tumors, and degenerative diseases [1]. Since damaged axons cannot be regenerated naturally in the adult central nervous system (CNS), SCI often leads to permanent sensory or motor dysfunction [1]. Primary injury causes compression or transection of the spinal cord, leading damage to nerve cells and disruption of the vasculature and blood-spinal cord barrier [2]. Subsequently, these mechanical damages induce a more terrible secondary injury cascade around the site. Edema and ischemia lead to further spinal cord swelling and compression, at the same time, inflammation and oxidative stress trigger additional apoptosis and poor post-injury microenvironment [3]. Surgery and various drugs such as glucocorticoids and gangliosides have shown limited effects in SCI clinical trials [4]. Therefore, there is an urgent need to develop novel and effective therapeutic strategies to improve neuronal axon regeneration and regulate the oxidative microenvironment to facilitate functional recovery after SCI.
In recent years, stem cell therapies have shown promising possibilities for the treatment of SCI, including mesenchymal stem cells (MSCs), neural stem cells (NSCs), and Schwann cells (SWs). Dental pulp stem cells (DPSCs), a kind of MSCs, has high proliferation potential and low immunogenicity, which are beneficial for allotransplantation. DPSCs originate from the neural ridge ectoderm and expresses more neural crista-related neural markers and neurotrophic factors, such as glial fibrillary acid protein (GFAP), beta III tubulin (βIII), brain-derived (BDNF) and glial neurotrophic factors (GDNF), than other MSCs [5]. This provides DPSCs with better neuroprotection and neurotrophic function to cope with nervous system injury. Some previous studies have reported that DPSCs as seed cells exhibit excellent therapeutic effects in rat SCI models. For example, an overexpression basic fibroblast growth factor of DPSCs engineered using hypoxic response elements has shown excellent angiogenesis for SCI repair [6]. A combination of N1-(4-boronobenzyl)-N3-(4-boronophenyl)-N1, N1, N3, N3-tetramethylpropane-1,3-diaminium and Laponite hydrogels with excellent reactive oxygen species (ROS) clearance and iron death inhibition, combined with DPSCs to regulate the ratio of excitatory and inhibitory synapses. The results show that the composite biomaterial can effectively reduce muscle spasms and promote the recovery of SCI [7].
Zinc is essential for the growth and development of human organs and tissues [8]. More than 300 enzymes require zinc to function properly, and zinc is therefore involved in regulating various cellular processes, including cell division and DNA synthesis [9]. Zinc is thought to interact with 10% of the human proteome, and it is essential for processes such as cell division and protein synthesis [10, 11]. More than 99% of intracellular zinc binds to proteins, and although there is growing evidence that interchangeable zinc ions act as second messengers capable of transducing extracellular stimuli into intracellular signaling events, the specific mechanisms remain uncertain [12]. The human body contains about 2–3 g of zinc, which is widely distributed in various tissues and organs of the human body. About 60% of them are in skeletal muscle, 30% are in bone, 5% are in liver and skin, and the rest are distributed in other tissues [13]. Zn2+ disorders are therefore associated with a variety of diseases, including high blood pressure [14], sudden cardiac death [15], cirrhosis of the liver [16], diabetes [17], osteoporosis [18], as well as anti-viral [19] and anti-bacterial deficiencies [20]. Zinc is closely related to neurogenesis. Most zinc chelate is contained in the presynaptic terminal vesicles of dentate granulosa cells forming mosses fiber bundles in the hippocampus, where neurogenesis and neural migration are active in the adult brain [21]. Extensive investigations have shown that zinc deficiency during pregnancy can impair neuronal differentiation and proliferation, leading to neurogenesis and cognitive dysfunction [22,23,24]. Although the exact mechanism is unclear, several studies have shown that zinc supplementation promotes in vitro neural differentiation of stem cells, including adipose-derived MSCs (AD-MSCs) [25] and induced pluripotent stem cells [26]. Zinc is known as an acute phase reactant due to its rapid redistribution from serum to the cell interval, and serum zinc concentrations are dramatically reduced in SCI animal models and clinical cases [27, 28]. Zinc has been associated with neuronal damage associated with traumatic brain injury (TBI), stroke, and epilepsy [29,30,31]. In addition, the loss of serum zinc concentration was negatively correlated with the long-term prognosis of motor function in SCI [30].
As a subfamily of metal-organic frameworks (MOFs), zeolitic imidazolate frameworks (ZIFs) present a zeolite-like crystal topology, which is characterized by large cavities connected by small windows [32]. Zeolitic imidazolate framework–8 (ZIF-8) with a topology of sodalite (SOD) is one of the most promising members of MOFs, given its great biocompatibility, high loading capacity and ROS scavenging activity [33]. Nanoscale ZIF-8 is very suitable for constructing pH-responsive functional scaffolds because of its stability under physiological conditions and decomposes when encountering acidic environments [34]. In addition to the drugs delivered by nano-carries, the Zn2+ released by ZIF-8 plays a vital role in regulating the differentiation of stem cells. ZIF-8 has been shown to promote osteoblast differentiation of bone marrow MSCs (BMSCs) through the classical mitogen-activated protein kinase (MAPK) pathway, providing a molecular basis for its application in bone tissue engineering [35, 36].
In this study, the roles of ZIF-8 in promoting neural differentiation of DPSCs have been revealed for the first time. ZIF-8 promotes neural differentiation and angiogenesis of DPSCs by activating the JNK1/p38 MAPK signaling pathway through the continuous release of Zn2+. In addition, ZIF-8 can help DPSCs resist apoptosis induced by Zn2+ deprivation and improve the survival rate of DPSCs. The therapeutic approach of ZIF-8 carried by DPSCs showed a favorable therapeutic effect in the rat SCI model.
Results
Synthesis and cellular uptake of ZIF-8 nanoparticles
ZIF-8 nanoparticles were successfully synthesized using a previously reported one-pot method. Typical octahedral morphology of ZIF-8 was revealed by SEM and TEM in Fig. 1A and B, respectively. The prepared ZIF-8 nanoparticles have uniform size around 193.1 ± 21.3 nm (Fig. 1C). The powder X-ray diffraction (PXRD) analysis showed that the diffraction peaks of synthesized ZIF-8 were identical to the simulated one, which verified a high-purity phase of ZIF-8 (Fig. 1D). The Fourier-transform infrared (FT-IR) spectra indicated that the synthesized ZIF-8 was highly consistent with the previous crystals in peak position and peak shape, which further confirmed the successful synthesis of ZIF-8 (Fig. 1E) [35]. As expected, these nanoparticles had excellent cytocompatibility as measured by CCK-8 in DPSCs (Fig. 1F). The ZIF-8 nanoparticles were non-toxic to DPSCs up to 100 ug/mL concentration for up to 96 h. Immunofluorescent co-localization analysis showed that the green fluorescent ZIF-8 was largely colocalized with the red fluorescent lysosomes, indicating that ZIF-8 entered cells through endocytosis and accumulated in lysosomes (Fig. 1G). Within 6 h, the cellular uptake efficiency of ZIF-8 in DPSCs could reach up to 98.1% (Fig. 1H). The pH-sensitivity of ZIF-8 was confirmed by Zn2+ release assay. At physiological pH, the release of Zn2+ from ZIF-8 is very slow, however, when pH = 6.5 or pH = 5.5, it is greatly increased and lasts for several hours (Fig. 1I).
Characterization of nano ZIF-8. (A) SEM, (B) TEM, (C) Statistics of size, (D) PXRD, (E) FT-IR, (F) toxicological evaluation. Different concentrations (0, 5, 10, 20, 50 and 100 µg/ml) of ZIF-8 were added to DPSC for CCK-8 detection at 24,48 and 96 h (G) Intracellular trafficking of C6-labeled ZIF-8 (20 µg/ml; green fluorescence) in DPSCs. LysoTracker (red) was used to label the lysosome, and Hoechst 33,342 (blue) was used to label the nucleus. (H) Quantification of the relative fluorescence intensity of C6-labeled ZIF-8. ***P < 0.001. (I) ZIF-8 nanoparticles were dispersed in α-MEM with different PH values, and Zn2+ levels were detected at different time points
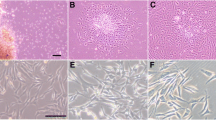
ZIF-8 promotes neural differentiation of DPSCs
DPSCs are ideal seed cells for SCI treatment because they are more easily differentiated in nerve direction and express more neurotrophic factors. Flow cytometry showed that the surface antigens of extracted DPSCs were 87.4% CD73 + cells (Figure S1A), 99.2% CD44 + cells (Figure S1B), and 3.37% CD45 + cells (Figure S1C). DPSCs can be induced to differentiate into osteoblasts (Figure S1D) and lipoblasts (Figure S1E), respectively. Our previous research suggested that an important strategy for repairing nerve damage is to promote the neural differentiation of stem cells [3]. ZIF-8 can release Zn2+ in cells, which was reported to promote neural differentiation of IPSCs and AD-MSCs [25, 26]. To investigate the ability of ZIF-8 nanoparticles to induce neural differentiation, DSPCs were incubated with a concentration gradient of ZIF-8 (0, 2.5, 5, 10, 20, 50 µg/mL) within the B27 medium. The differentiating rate was examined and quantified every two days, as well as the length and the number of branching neurites. At the endpoint of the differentiation culture, the induction group with 20 µg/mL ZIF-8 showed the most desirable neurodifferentiation effect compared to the control group, followed by the group with 50 µg/mL ZIF-8 (Fig. 2A). The neurodifferentiation rate of DPSCs increased with increasing concentration of ZIF-8 in the range of 0 to 20 µg/mL and then decreased at 50 µg/mL (Fig. 2B). The number and length of neurites of DPSCs-derived neuron-like cells increased in a dose-dependent manner in the range of 0 to 20 µg/mL and they were significantly higher than those of the control group when the concentration of ZIF-8 was 20 µg/mL (Fig. 2C, D). Overall, ZIF-8 induced the differentiation of DPSCs into neuron-like cells. Next, we examined the expression of neural marker proteins by western blotting. The expression of βIII-tubulin and NeuN reflects the regeneration of early neuronal cells and mature neurons [37]. GFAP expression indicates glial scar formation [38]. S100b was used to evaluate the proliferation of Schwann cells, which is required for axonal regeneration after injury [39]. Immunofluorescence staining showed that the expression of βIII-tubulin and NeuN in the 20 µg/mL ZIF-8 group was significantly higher compared to the control group, suggesting that ZIF-8 at this concentration significantly promoted the differentiation of DPSCs into neuron-like cells (Fig. 2E). These results were confirmed via western blotting (Fig. 2F). ZIF-8 promoted the expression of neural markers such as βIII-tubulin, Nestin and S100b in DPSCs compared with the control group to varying degrees but did not change the level of GFAP (Fig. 2G). This indicates that ZIF-8 mainly promotes the differentiation of DPSCs into neurons rather than glial cells.
ZIF-8 promotes DPSC neural differentiation. (A) Fluorescent images of calcein-labeled DPSCs cells after different treatments of ZIF-8 (0, 2.5, 5, 10, 20 and 50 µg/ml) within B27 medium for 6 days. Trends of DPSCs neural differentiation (mean ± SD): (B) neural-like cell ratio, (C) the neurite number and (D) neurite length. DPSCs were treated with different concentrations of ZIF-8 (0, 2.5, 5, 10, 20 and 50 µg/ml) in B27 nerve differentiation culture for 7 days (E) Immunofluorescence analysis of expression of βIII-tubulin (green) and NeuN (red). Fluorescence intensity quantification of NeuN and βIII-tubulin is given. (F) Western Blot was used to detect the expression of Nestin, βIII-tubulin, GFAP, S100b and β-actin. (G) Quantitative statistics of gray value were given. ***P < 0.001
ZIF-8 rescues apoptosis of Zn2+ deprivation
SCI is accompanied by a severe reduction of Zn2+ levels in plasma [30]. To determine the bioactive Zn2+ levels at SCI sites, a Zn2+ special fluorescent probe — TSQ was applied. As shown in Fig. 3A, fluorescence quantification showed that the level of Zn2+ in the SCI model group was significantly lower than that in the Sham group, indicating that SCI caused a serious blow to the Zn2+ level in the post-injury microenvironment.
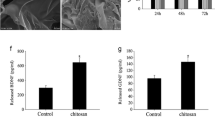
ZIF-8 contributes to resistance to apoptosis induced by Zn-deprivation and promotes angiogenesis of DPSCs. (A) TSQ fluorescence staining was used to detect Zn2+ in normal control (labelled as ‘Con’) or SCI rat spinal cord tissue cells (n = 6, mean ± SD); (B) DPSCs were treated with TPEN (0 and 0.5 µM) combined with ZIF-8 of concentration gradient (0, 2.5, 5, 10, 20 and 50 µg/ml). After 24 h treatment, flow cytometry was used to detect FITC and PE; (C) Statistical diagram of apoptotic cell distribution; (D) DPSCs were treated with TPEN (0 and 0.5 µM) combined with ZIF-8 of concentration gradient (0 and 20 µg/ml). Western Blot was used to detect Bcl2, BAX and GAPDH. Quantitative statistics of gray value were given. (E) DPSCs were treated with TPEN (0 and 0.5 µM) combined with ZIF-8 of concentration gradient (0, 2.5, 5, 10, 20 and 50 µg/ml) or Zncl2 (0, 0.5, 1, 2, 4 and 10 µM). After 24 h treatment, CCK-8 was used to detect cell viabilities. (F) After 72 h treated with ZIF-8 (0, 10, 20 and 50 µg/ml), the medium was co-culture with HUVECs. Then cells stained with the crystal violet stain for Transwell experiments. (G) The number of traversed cells is counted by the ImageJ software. (H) Western Blot of VEGF-a and GAPDH of DPSCs treated with ZIF-8 (0, 2.5, 5, 10, 20 and 50 µg/ml). Quantitative statistics of gray value (I) were given. (J) VEGF-a in the medium was quantified by ELISA. *P < 0.05; **P < 0.01; ***P < 0.001
Zinc plays vital roles in various biochemical pathways and enzymes and participates in antioxidant defense and immune response, making it particularly important in the oxidative stress and inflammatory processes after SCI [40]. To determine the association between Zn2+ deprivation and survival of transplanted stem cells, we constructed an in vitro Zn2+ removal model by using N,N,N0,N0-tetrakis(2-pyridylmethyl)-ethylenediamine (TPEN), a Zn2+ chelator. As shown in Fig. 3B, TPEN significantly induced DPSCs apoptosis. However, the effect of TPEN-induced apoptosis was rescued by ZIF-8 treatment in a dose-dependent manner, and plateaued after 20 µg/mL (Fig. 3C). In addition, TSQ fluorescence showed that 20 µg/mL ZIF-8 could restore the intracellular Zn2+ to normal level (Figure S2A, S2B). Western blot also verified the reversal effect of ZIF-8 on TPEN-induced apoptosis in DPSCs. TPEN significantly inhibited the expression of antiapoptotic protein Bcl-2 and promoted the expression of the apoptotic protein Bax in DPSCs. After treatment of ZIF-8, the BAX and Bcl-2 expression level was restored (Fig. 3D). In addition, different concentrations of ZnCl2 and ZIF-8 were added to DPSCs with or without the treatment of 0.5 µM TPEN to detect the effect of Zn2+ on their viability. As shown in Fig. 3E, both ZnCl2 and ZIF-8 showed a significant effect against TPEN treatment. Importantly, ZIF-8 presented more effective than ZnCl2 due to its controlled release of Zn2+ (Fig. 3E). Taken together, these results suggested that ZIF-8 could contribute to DPSCs resist apoptosis induced by Zn2+-deprivation.
ZIF-8 enhances the angiogenic effect of DPSCs
To determine whether ZIF-8 promotes the pro-angiogenesis of DPSC, human umbilical vein endothelial cells (HUVECs) were used in transwell migration assay (Fig. 3F). The results showed that more cells migrated through the membrane in the ZIF-8 groups, especially at the concentration of 20 µg/mL, indicating a strong angiogenic capacity of ZIF-8 (Fig. 3G). Western blotting showed significant upregulated expression of VEGF-a in DPSCs with increased concentrations of ZIF-8 (Fig. 3H and I). The concentration of VEGF-a in the supernatant of DPSCs treated with ZIF-8 for 3 days was quantified by ELISA, and the results indicated that ZIF-8 dose-dependently elevated the level of VEGF-a in the conditioned medium of DPSCs (Fig. 3J). In addition, cell migration from the transplant site to the injured ischemic area is an important step in stem cell therapy [41]. Transwell migration assay showed that more cells migrated across the membrane in the ZIF-8 group than in the control group. (Supplemental Fig. 2C and 2D). These results suggest that ZIF-8 enhances the expression and secretion of VEGF-a, thereby promoting the angiogenesis activity of DPSCs, as well as the migration ability.
ZIF-8 enhances neural differentiation and pro-angiogenic effect of DPSCs through activating MAPK signaling pathway
To further explore the mechanism by which ZIF-8 promotes neural differentiation and angiogenesis of DPSCs, second-generation sequencing was used to detect the changes of transcriptomic profiles. After 4 days of neurodifferentiation, a total of 2153 DEGs were identified, including 870 upregulated genes and 1283 down-regulated genes. The heat map shows the top 40 DEGs (Log2FC > 1.5, P < 0.05). These DEGs subsequently underwent KEGG and GO enrichment analysis (Fig. 4A). As shown in Fig. 4B, ZIF-8 promotes activation of MAPK signaling pathway, mineral absorption, and tyrosine metabolism, which are associated with neural differentiation. Go analysis indicated that ZIF-8 treatment was associated with the biological function of neurogenesis, nervous system process, cell development and immune system process, (Fig. 4C). The down-regulated genes were associated with Cytokine-cytokine receptor interaction, Rap1 signaling pathway, complement and coagulation cascade, etc. signaling pathways, as well as calcium ion binding, serine hydrolase activity and gated channel activity, etc. functional alternation (Fig. 4D F).
ZIF-8 promotes neural differentiation and angiogenesis of DPSCs through MAPK signaling pathways. (A) Heat map showing the top 40 differential gene expression. KEGG analysis of upregulated (B) and downregulated (C) signaling pathways. GO enrichment analysis of upregulated (D) and downregulated (E) signaling pathways. (F) DPSCs were treated with ZIF-8 (0, 2.5, 5, 10, 20 and 50 µg/ml) for 7 days in B27 medium. Western Blot was used to detect the expression of ERK1/2, p-ERK1/2, JNK1, p-JNK1, p38, p-p38 and GAPDH. Quantitative statistics of gray value were given. (G) DPSCs were treated with SP600125 (0 and 40 µM) combined with ZIF-8 (0 and 20 µg/ml). Western Blot was used to detect the expression of p-JNK1, βIII-tubulin, S100b and GAPDH. Quantitative statistics of gray value were given. (H) DPSCs were treated with SB203580 (0 and 20 µM) combined with ZIF-8 (0 and 20 µg/ml). Western Blot was used to detect the expression of p-38, VEGF-a and GAPDH. Quantitative statistics of gray value were given. **P < 0.01; ***P < 0.001
In view of the above analysis, the activation of the MAPK signaling pathway may play an important role in the biological activity of ZIF-8. Interestingly, under neural differentiation conditions, ZIF-8 inhibited the phosphorylation of ERK1 and activated the phosphorylation of two other MAPK key proteins —JNK and p38 (Fig. 4F). The phosphorylation of JNK1 and p38 is liable for the expression of βIII-tubulin and VEGF-a, respectively [42, 43]. This was demonstrated by an increased expression of p-JNK as well as βIII-tubulin and S100b (Fig. 4G) in presence of a specific p-JNK inhibitor, SP600125 when treated with ZIF-8. Similarly, another set of experiments showed an upregulated expression of p-p38 and VEGF-a induced by ZIF-8 could be reversed by SB203080, a p38 MAPK inhibitor (Fig. 4H). These results suggested that ZIF-8 promoted the neural differentiation and angiogenesis [43, 44] of DPSCs through JNK1/p38 MAPK pathways.
ZIF-8 promotes neural differentiation and proangiogenic effects of DPSCs depends on continuous release of Zn2+
To explore whether ZIF-8 promotes neurogenesis of DPSCs by releasing Zn2+, varying amount of TPEN was added to the neural inducing medium containing 20 µg/ml ZIF-8. It was shown that ZIF-8-induced neural morphogenesis of DPSCs was disrupted by TPEN in a dose-dependent manner (Fig. 5A). The proportion of neuronal differentiation, the number and the length of neurites decreased in response to TPEN treatment (Fig. 5B, C, D). ZnCl2 was used to further certify whether Zn2+ can promote neural differentiation of DPSCs. As shown in Fig. 5E, ZnCl2 significantly upregulated the immunofluorescence intensity of βIII-tubulin and NeuN in DPSCs. To further compare the ability of ZIF-8 and ZnCl2 to promote neural differentiation, the same Zn2+ molar concentrations of ZIF-8 and ZnCl2 (1 and 2 µM) were treated with DPSCs. The results indicated that ZIF-8 was more potent than Zncl2 in inducing neural differentiation at the same molar concentration (Figure S3A and S3B). In addition, TPEN significantly downregulated the expression of p-JNK1, p-38, βIII-tubulin and VEGF-a with or without 20 µg/ml ZIF-8 treatment (Fig. 5G, Figure S3C). Regarding angiogenesis, ZIF-8 significantly increased the number of HUVEC migrating across the membrane, which was reduced with the action of TPEN (Fig. 5F). In addition, the ELISA assay showed that the extracellular secretion of VEGF-a stimulated by ZIF-8 can be reversed by TPEN (Figure S3D). Cell viability assay showed that ZnCl2 could rescue TPEN-induced apoptosis, which is inferior to ZIF-8 at the same molar concentration (Fig. 5H). These results suggested that ZIF-8 promotes neural differentiation and proangiogenic effect of DPSCs depends on releasing Zn2+.
ZIF-8 promotes neural differentiation and angiogenesis of DPSCs depended on Zn2+ release. (A) Fluorescent images of calcein-labeled DPSCs cells treated with TPEN (0, 0.25, 0.5, 1, 1.5 and 2 µM) with ZIF-8 within (20 µg/ml) in B27 medium for 6 days. Trends of DPSCs neural differentiation (mean ± SD): (B) neural-like cell ratio, (C) the neurite number and (D) neurite length. DPSCs were treated with different concentrations of Zncl2 (0, 0.5, 1, 2, 4, 10 and 20 µM) in B27 nerve differentiation culture for 7 days (E) Immunofluorescence analysis of expression of βIII-tubulin (green) and NeuN (red). Fluorescence intensity quantification of NeuN and βIII-tubulin is given. (F) DPSCs were treated with TPEN (0 and 0.5 µM) combined with ZIF-8 of concentration gradient (0 and 20 µg/ml), the medium was co-culture with HUVECs. Then cells stained with the crystal violet stain for Transwell experiments. The number of transferred cells is quantified. (G) DPSCs cells treated with TPEN(0, 0.1, 0.25 and 0.5 µM) with ZIF-8 within (20 µg/ml) in B27 medium for 7 days. Western Blot was used to detect the expression of p-JNK1, p-38, VEGF-a, βIII-tubulin, and GAPDH. Quantitative statistics of gray value (H) were given. (I) DPSCs were treated with TPEN (0 and 0.5 µM) combined with ZIF-8 or Zncl2 of concentration gradient (0, 0.5, 1 and 2 µM). After 24 h treatment, CCK-8 was used to detect cell viabilities. **P < 0.01; ***P < 0.001
ZIF-8-DPSCs promote motor function recovery in rats after SCI
The motor functions of rat hind limbs were assessed on day 7, 14, 21, 28 using Basso-Beattie-Bresnahan (BBB) score, slope test, gait, and footprint analysis. There was no significant difference in BBB scores between the groups in one week after the operation. At subsequent time nodes, the BBB score of the ZIF-8 + DPSCs group was significantly improved, followed by the DPSCs only group (Fig. 6A). In the slope test, rats in the ZIF-8 + DPSCs group could stay at a greater angle than those in the SCI group and other treatment groups (Fig. 6B). At day 28 after the operation, the rats of the SCI model group had no obvious hindlimb activity, and the connection lines of joints were roughly horizontal and straight. In the GelMA group, the hindlimb motor function of the rats was not improved significantly, and only subtle minor joint movements were observed. The rats in the DPSCs group could move their hind limbs. The ZIF-8-DPSCs group showed complete hind limb lift and forward stride, although there was a certain gap with the Sham group (Fig. 6C). Compared with the SCI group and other treatment groups, rats in ZIF-8-DPSCs group had higher height from the ground (Fig. 6D), less foot error (Figure S4A), shorter spasm duration (Figure S4B) and longer forward distance (Figure S4C). The pads of the sham group showed clear footprints equidistantly arranged in two straight lines. However, those of the SCI group and GelMA group showed obvious passive dragging marks. Though the DPSCs group showed initial off-ground movement, the rats in the ZIF-8 + DPSCs group showed the best movement outcome with two orderly linear footprints. Although considerably improved, it is worth noting, that the rats in this group were still dragging tails and had a shorter stride distances (Fig. 6E).
ZIF-8-DPSCs promote the recovery of motorial function in SCI rats. (A) The BBB scores of the rats in the Sham, SCI group, GelMA group, DPSCs group and ZIF-8-DPSCs group. (B) The inclined plane test scores of rats in the Sham, SCI group, GelMA group, DPSCs group and ZIF-8-DPSCs group. (C) Video analysis showed the rats walking at a speed of 28 d.a.t. Weight support, leg extensor spasm, walking, and foot placement were analyzed. Foot movements are highlighted by arrows. The initial position of the move is highlighted by the yellow dot. (D) Weight support (quantified as the height of the trunk from the ground). (E) Footprint analysis of Sham, SCI group, GelMA group, DPSCs group and ZIF-8-DPSCs group in 28 d.a.t. **P < 0.01. *** P < 0.001. n.s. means no statistical significance. # P < 0.05 compared with DPSCs group. Data are represented as mean ± SD (n = 6)
Four weeks after the operation, the spinal cord segments around the injury site were dissected for histological analysis. H&E staining showed loose cells in the SCI group and much dense tissue in the ZIF-8-DPSCs group (Fig. 7A). Compared with the control SCI group, the normal tissue area of the ZIF-8-DPSCs group increased significantly (Fig. 7B). Double staining with βIII-tubulin and VEGF-a was used to analyze the regeneration of nerves and blood vessels at the injury site (Fig. 7C). The expression of βIII-tubulin was significantly increased in the ZIF-8-DPSCs group compared with the SCI group, indicating that ZIF-8-DPSCs have strong neural repair effects (Fig. 7D). The expression of VEGF-a was significantly increased in the ZIF-8 + DPSCs group compared with the Sham and SCI groups, indicating the angiogenic potency of ZIF-8 + DPSCs (Fig. 7E). IHC staining verified the activation of JNK and p38 MAPK pathways by ZIF-8 (Figure S5). Quantitative analysis showed that the expression of p-JNK1 and p-p38 in ZIF-8-DPSCs group was significantly improved compared with that in SCI group (Figure S5B, S5C). To verify whether Zn2+ is responsible, Zn2+ levels were assessed using TSQ. The fluorescence image of the SCI group was darker than that of the Sham group, indicating a decrease of the Zn2+ level during SCI (Fig. 7F). Quantitative analysis showed that Zn2+ in the ZIF-8 + DPSCs group was restored, even exceeding the Sham group (Fig. 7G). Interestingly, some concentrated Zn2+ concentration regions of cells could be found in the tissues from ZIF-8 + DPSCs group after 28 days of repairment (white arrows). Nissl staining images showed that the number of Nissl’s body in the injured spinal cord of rats in the ZIF-8-DPSC group was increased (Figure S6A and B). Tunel staining demonstrated that apoptosis in the ZIF-8-DPSCs group was inhibited compared with the SCI group (Figure S6A and C). In summary, ZIF-8-DPSCs significantly improved the recovery of motor function and repairment of neural tissues in rats after SCI.
ZIF-8-DPSCs promote nerve tissue formation in SCI rats. (A) H&E staining transverse section of injured spinal cord tissue 28 days after injury. Above is the spinal cord at low magnification, with scar tissue and cavity visible in the SCI group, and below is the spinal cord at higher magnification. (B) Spinal cord tissue preserved on day 28 after spinal cord injury. Quantitative analysis of HE sections showed that. (C) The expression of VEGF-a and βIII-tubulin in the Sham, SCI group, GelMA group, DPSCs group and ZIF-8-DPSCs group was analyzed by immunofluorescence. Fluorescence intensity quantification of βIII-tubulin (D) and VEGF-a (E) is given. (F) TSQ fluorescence staining was used to detect Zn2+ in the Sham, SCI group, GelMA group, DPSCs group and ZIF-8-DPSCs group. The white arrow points to cells that overexpress Zn2+. (G) Fluorescence intensity of Zn2+ is quantified. *P < 0.05. **P < 0.01. *** P < 0.001. Data are represented as mean ± SD (n = 6)
The cytotoxicity assessment of ZIF-8-DPSCs in vivo
Although the in vivo safety of ZIF-8 nanoparticles or DPSCs has been recognized, the safety of its combination needs to be examined. After 28 days of treatment, the rats were subjected to H&E and TSQ staining of major organs and hematological analysis to determine systemic toxicity of ZIF-8-DPSCs. H&E staining showed that the cell morphology and tissue structure of the major organs included lung, liver, spleen, kidney and heart were not changed by ZIF-8-DPSCs treatment (Figure S7A). Because ZIF-8-DPSCs treatment altered Zn2+ levels in local SCI tissues, Zn2+ levels in other major organs were detected. TSQ results suggested that ZIF-8-DPSCs did not significantly enhance the level of Zn2+ in other tissues. In addition, typical Zn2+ overexpression cells in local SCI tissues were not found in other organs (Figure S7B). Interestingly, treatment with ZIF-8-DPSCs and DPSCs both promoted weight gain in rats (Figure S7C). There was no significant difference in ALT and AST levels between the groups, indicating that ZIF-8-DPSCs did not have significant hepatotoxicity (Figure S7D and S7E). Levels of CREA and UREA were significantly increased in the SCI group. However, treatment with ZIF-8-DPSCs rescued the CREA and UREA levels suggesting the protective effect on the kidneys (Figure S7F and S7G). Similar to histological results, ZIF-8-DPSCs increased serum Zn2+ levels in SCI rats (Figure S7H). These results suggest that ZIF-8-DPSCs have good biocompatibility.
Discussion
ZIF-8 is often used in the field of biomedicine as a drug or gene carrier. Interestingly, ZIF-8 has been less studied as a nanoparticle to present biological functions. In this paper, we propose for the first time that ZIF-8 can promote neural differentiation of DPSCs by activating the MAPK signaling pathway through the release of Zn ions. ZIF-8 promoted the expression of VEGF-a and the angiogenic ability of DPSCs. In addition, ZIF-8 can resist the apoptosis of DPSCs caused by Zn2+ deprivation. In vivo experiments, ZIF-8 combined with DPSCs and GelMA hydrogel promoted the recovery of motor function in SCI rats. Tissue slides showed that ZIF-8-DPSCs promoted neural recovery, antiapoptotic and angiogenic function of SCI rats.
SCI is closely related to serum zinc ion concentration. An important correlation is that acute SCI is accompanied by a sharp decrease in serum Zn2+ concentration. Heller et al. reported a 30% decrease in serum Zn2+ concentration in SCI patients at the acute injury stage [28]. This finding was further confirmed in the SCI mouse model [45, 46]. More importantly, acute serum zinc concentrations decreased proportionally with the severity of SCI [28]. Our study found that in the pathological injury of chronic convalescent rats with SCI, intracellular Zn ions were significantly deprived. Mechanistically, monocytes are activated rapidly in response to the intense inflammatory response to injury[30]. Through the TLR4/NF-κΒ/ZIP8 signal pathway, mononuclear cells absorb the serum Zn2+ concentration, and transfer it into the damaged tissues[47,48,49]. Secondary injury of SCI is often a more important cause of neuron loss. Glutamate excitatory toxicity is a common mechanism of neuronal tissue death at this stage [50]. Reduced extracellular Zn2+ concentration induced by trauma can lead to dysregulation of the NF-κB signaling pathway, which leads to glutamate excitotoxicity of astrocytes and promotes apoptosis of oligodendrocytes[51]. In zinc deficiency conditions, oligodendrocyte exposure to glutamate causes toxicity, but not at sufficiently high zinc concentrations, highlighting the importance of zinc in preventing glutamate excitotoxicity. High levels of zinc inhibit Ca2+ current through AMPA (α-amino-3-hydroxy-5-methyl-4-isooxazopropionic acid) receptors, suggesting that Zn2+ inhibits charge current through ionic glutamate receptors[52]. This result is consistent with our findings. In order to mimic the environment of Zn2+ loss in SCI, we constructed an in vitro model of Zn2+ deprivation. With the addition of TPEN, Zn2+ in DPSCs was significantly inhibited. Cell apoptosis was obviously induced and cell activity decreased. This indicated that Zn2+ deprivation significantly inhibited the survival of transplanted stem cells. With the increase of ZIF-8 concentration, the pro- portion of apoptosis decreased and the cell activity increased. Zn2 + supplementation also reversed the TPEN-induced inhibition of cell viability and apoptosis. In addition, ZIF-8 combined with DPSCs can better repair SCI damage in vivo, promote the occurrence of local neurons and blood vessels, and inhibit the apoptosis of damaged local cells.
Currently, a consensus of cell therapy is that the use of scaffolds to concentrate stem cells at the injured site and form a 3D repair environment is conducive to the differentiation and survival of stem cells. Porous gelatin methacryloyl (GelMA) hydrogels with properly connected micropores have a good cellular response and can promote neural stem cell migration, which is suitable for the repair of SCI alone [53] or in combination with seed cells[54, 55]. In this study, the motor function repair potential of ZIF-8 combined with DPSCs after SCI was assessed by transplanting ZIF-8 and DPSCs (labelled ZIF-8-DPSCs) loaded with GelMA hydrogel at the SCI site. We tried to use GelMA hydrogel as scaffold material and DPSCs as seed cells to repair SCI, and the results were similar to those of other studies. The basic logic is that we have successfully used this combination to repair large sciatic nerve defects in rats[Full size image