Abstract
Photothermal therapy (PTT), which converts light energy to heat energy, has become a new research hotspot in cancer treatment. Although researchers have investigated various ways to improve the efficiency of tumor heat ablation to treat cancer, PTT may cause severe damage to normal tissue due to the systemic distribution of photothermal agents (PTAs) in the body and inaccurate laser exposure during treatment. To further improve the survival rate of cancer patients and reduce possible side effects on other parts of the body, it is still necessary to explore PTAs with high selectivity and precise treatment. In this review, we summarized strategies to improve the treatment selectivity of PTT, such as increasing the accumulation of PTAs at tumor sites and endowing PTAs with a self-regulating photothermal conversion function. The views and challenges of selective PTT were discussed, especially the prospects and challenges of their clinical applications.

Similar content being viewed by others
Introduction
Cancer therapy is one of the most significant challenges facing the health care industry today [1]. According to a recent survey, in 2020, the number of new cancer patients globally is approximately 19.29 million, and the number of deaths has reached 9.6 million. Cancer’s high incidence and mortality have led researchers worldwide to work hard to develop more accurate and rapid diagnostic strategies and effective anticancer methods [2, 3]. As an effective treatment, traditional treatments (chemotherapy, radiotherapy, and surgery) are the most commonly employed clinical treatment methods. However, patients may have a high risk of treatment failure or posttreatment side effects during or after traditional treatment [4, 5]. Among the emerging cancer therapies, photothermal therapy (PTT) utilizes the photothermal effect of photothermal agents (PTAs), which converts absorbed light energy to heat to cause thermal burns on the tumor. PTT has high research value because of its simple operation, short treatment time, and rapid recovery [6, 7]. More importantly, PTT is a highly effective and noninvasive therapy that can eliminate various types of cancer. It is well known that the ultimate goal of cancer treatment is to kill cancer cells without damaging normal cells [8,68] proposed a novel synergistic triggering mechanism to realize the self-assembly of gold nanospheres. Au@ZIF-8 does not produce photoacoustic signal and photothermal conversion capability in normal tissue. In contrast, in the presence of overexpressed glutathione and hydrogen ions in the tumor, gold nanospheres were released from Au@ZIF-8 to form aggregates and showed solid signals for imaging and effective PTT. This work provides a new strategy for designing therapeutic agents with sequential response steps to avoid interfering with diagnostic signals from normal tissue and to reduce damage to normal tissue during treatment.
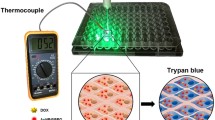
However, the excitation window of existing PTT is mainly located in the visible or NIR region, with insufficient penetration depth and relatively low interaction with tissues, limiting its thermal sensitivity effect. Therefore, Professor Zhang Dong et al. [69] developed an activatable NIR-II plasmonic theranostics system based on silica-encapsulated, self-assembled, gold nanochains (AuNCs@SiO2). In this study, the optical properties were precisely controlled by the structural changes of plasmonic nanoparticles in response to the tumor microenvironment, leading to accurate diagnosis and effective treatment of tumors. In normal tissue, the self-assembled gold nanochain does not change its structure and shows photoacoustic and photothermal “OFF” states in the NIR-II region. When the gold nanochain enters malignant tumor tissue, it will obtain electron conductivity through the fusion of its chain structure, and the electric field intensity is significantly enhanced, so that the surface plasmonic resonance extinction peak has a redshift, presenting an NIR-II region of photoacoustic and photothermal “ON” states. Because of the existence of “hot spots” between the gold nanoparticles and the electronic conductivity effect of the chain structure, the photoacoustic enhancement effect is significant, and the photoacoustic signal at the malignant breast tumor is greatly enhanced to realize the specific diagnosis and PTT of breast cancer. This activated strategy can realize in situ and sensitive tumor detection while effectively killing tumors, which may prominently improve the survival rate of cancer patients and introduce a new way for optical nanoengineering to become intelligent, accurate, and non-invasive in the NIR-II window. Although all these studies reported the PTT of tumors by stimuli-responsive self-assembling AuNPs, an evaluation methodology for damage to normal tissues and skin is still lacking. To validate the possibility of specifically killing tumor cells, we established an in vitro selective photothermal transformation model (Fig. 6a), a “one facula” experiment (Fig. 6b, c), and an in vivo skin-damaging assessment model (Fig. 6d) [61]. This study is the first attempt to construct an evaluation methodology for precise PTT using in vitro and in vivo models.

(Reprinted from Ref. [61] with permission. Copyright 2022, Elsevier Ltd)
a Schematic diagram of the in vitro selective photothermal transformation model; b Schematic diagram of a “one facula” experiment; c Infrared thermal images and the temperature evolution of the tumor and skin tissue of mice treated with Au nanostar and S-AuNPs at 808 nm laser irradiation (3.33 W/cm2) at a different time; d Schematic illustration of specificity killing of the tumor cells under laser irradiation without skin damage
In addition to self-assembling gold nanoparticles, other materials can be used to self-assemble nanomaterials at tumor sites to achieve better photothermal conversion and selective thermal burn of tumors. As a rising star in the family of two-dimensional materials, BP has attracted much attention from researchers. BP has unique optical properties, and relevant reports have proven that BP two-dimensional material can serve as an efficient photothermal preparation, and phosphorus is an essential element in organisms, making its application in the biomedical field an unparalleled advantage [70,71,72]. Recently, Han Zhang et al. [Increase the concentration difference between the tumor site and normal tissue The photothermal conversion ability of most PTAs is in direct proportion to the concentration. Hence, increasing the concentration of photothermal nanomaterials at tumor sites is an effective method for improving the PTT accuracy. Intratumoral injection, targeting systems, biomimetic systems, and programmed targeting systems aim to increase the PTAs concentration in tumors. Although intratumoral injection can effectively cause the concentration difference between normal tissue and tumor tissue to selectively increase the temperature of the tumor site, this method cannot be directly employed for metastatic and deep tissue tumors in vivo. Additionally, many times intratumoral injections may cause to tumor metastasis. Intelligent transportation systems (targeting systems, biomimetic systems, and programmed targeting systems) enhance the uptake of tumor cells. Nevertheless, most PTAs are filtered from the body before entering tumor cells, which makes the amount of enrichment in tumor sites is far from expected. Therefore, although the method increases the concentration difference between the tumor site and normal tissue, which is feasible in theory, actual results will not materialize unless the nano-drug delivery system achieves rapid progress. Assume that PTAs have weak photothermal conversion ability in normal tissue and strong photothermal conversion ability in the tumor site. In this case, the temperature of the tumor site will selectively increase after the same enrichment amount and infrared laser irradiation, with either minimal or no damage to normal cells. Therefore, endowing PTAs with a self-regulating photothermal conversion capability through the responsive activation of PTAs at the tumor site can achieve a better precision killing effect on tumors. Although the self-regulating photothermal conversion ability of PTAs has been realized by stimulus–response systems (such as the self-assembly of gold nanoparticles or dye molecules) in vitro and animal experiments, the complexity of the in vivo environments of the body is still a significant challenge for the precisely controlled. As a non-invasive and spatiotemporally controllable tumor treatment method, PTT is still in the preliminary clinical research stage and has proven excellent anticancer efficacy in the laboratory and clinic [30, 77]. All the above mentioned methods are theoretically selective, and relevant experiments have not verified the safety of normal skin and body organs. For effective clinical translation of selective PTT, the following aspects should be taken into account: (1) provide in vitro and in vivo new evaluation methods to evaluate the ability of selective PTT; (2) improve the sensitivity of self-regulating PTAs to achieve selective PTT; and (3) investigate the long-term prognosis of selective PTT. Although the complete clinical application of PTT has not fully emerged, it offers new hope for the clinical treatment of cancer. Highly selective PTT will render the construction of clinical PTT more refined and intelligent and become a new opportunity to develop clinical cancer therapy. With rational technological innovation and strategic improvements, there is a considerable scope for clinical expansion of the new PTT platform. Simultaneously, we hope that this review will provide valuable information and insights for future research into selective PTT.Endowing PTAs self-regulating photothermal conversion capability
Prospects and challenges of clinical applications
Availability of data and materials
Not applicable.
References
Liu Y, Bhattarai P, Dai Z, Chen X. Photothermal therapy and photoacoustic imaging: via nanotheranostics in fighting cancer. Chem Soc Rev. 2019;48:2053–108.
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941–53.
Farran B, Montenegro RC, Kasa P, Pavitra E, Huh YS, Han YK, et al. Folate-conjugated nanovehicles: strategies for cancer therapy. Mater Sci Eng C. 2020;107:110341. https://doi.org/10.1016/j.msec.2019.110341.
Chen SX, Ma M, Xue F, Shen S, Chen Q, Kuang Y, et al. Construction of microneedle-assisted co-delivery platform and its combining photodynamic/immunotherapy. J Control Release. 2020;324:218–27.
Wang H, Revia R, Wang K, Kant RJ, Mu Q, Gai Z, et al. Paramagnetic properties of metal-free boron-doped graphene quantum dots and their application for safe magnetic resonance imaging. Adv Mater. 2017;29:1605416. https://doi.org/10.1002/adma.201605416.
Moon HK, Lee SH, Choi HC. In vivo near-infrared mediated tumor destruction by photothermal effect of carbon nanotubes. ACS Nano. 2009;3:3707–13.
Liu Y, Crawford BM, Vo-Dinh T. Gold nanoparticles-mediated photothermal therapy and immunotherapy. Immunotherapy. 2018;10:1175–88. https://doi.org/10.2217/imt-2018-0029.
Kim JW, Galanzha EI, Shashkov E V., Moon HM, Zharov VP. Golden carbon nanotubes as multimodal photoacoustic and photothermal high-contrast molecular agents. Nat Nanotechnol. 2009;4:688–94. http://www.nature.com/articles/nnano.2009.231.
Li J, **ao H, Yoon SJ, Liu C, Matsuura D, Tai W, et al. Functional photoacoustic imaging of gastric acid secretion using pH-responsive polyaniline nanoprobes. Small. 2016;12:4690–6.
Liu T, Zhang M, Liu W, Zeng X, Song X, Yang X, et al. Metal ion/tannic acid assembly as a versatile photothermal platform in engineering multimodal nanotheranostics for advanced applications. ACS Nano. 2018;12:3917–27. https://doi.org/10.1021/acsnano.8b01456.
Abbas M, Zou Q, Li S, Yan X. Self-assembled peptide- and protein-based nanomaterials for antitumor photodynamic and photothermal therapy. Adv Mater. 2017;29:1605021. https://doi.org/10.1002/adma.201605021.
Cheng L, Wang C, Feng L, Yang K, Liu Z. Functional nanomaterials for phototherapies of cancer. Chem Rev. 2014;114:10869–939.
Du W, Chong Y, Hu X, Wang Y, Zhu Y, Chen J, et al. Increasing photothermal efficacy by simultaneous intra- and intermolecular fluorescence quenching. Adv Funct Mater. 2020;30:1908073. https://doi.org/10.1002/adfm.201908073.
Cheng Q, Gao F, Yu W, Zou M, Ding X, Li M, et al. Near-infrared triggered cascade of antitumor immune responses based on the integrated core-shell nanoparticle. Adv Funct Mater. 2020;30:2000335. https://doi.org/10.1002/adfm.202000335.
Nam J, La W, Hwang S, Ha YS, Park N, Won N, et al. pH-responsive assembly of gold nanoparticles and “spatiotemporally concerted” drug release for synergistic cancer therapy. ACS Nano. 2013;7:3388–402. https://doi.org/10.1021/nn400223a.
Zhang D, Zheng Y, Lin Z, Lan S, Zhang X, Zheng A, et al. Artificial engineered natural killer cells combined with antiheat endurance as a powerful strategy for enhancing photothermal-immunotherapy efficiency of solid tumors. Small. 2019;15:1902636. https://doi.org/10.1002/smll.201902636.
Qiu X, Xu L, Zhang Y, Yuan A, Wang K, Zhao X, et al. Photothermal ablation of in situ renal tumor by PEG-IR780-C13 micelles and near-infrared irradiation. Mol Pharm. 2016;13:829–38. https://doi.org/10.1021/acs.molpharmaceut.5b00734.
Wang S, Song W, Xu Y, Cai S, Yin Y, Zhang Q, et al. Red-blood-cell-membrane-enveloped magnetic nanoclusters as a biomimetic theranostic nanoplatform for bimodal imaging-guided cancer photothermal therapy. J Mater Chem B. 2020;8:803–12.
Chao Y, Chen G, Liang C, Xu J, Dong Z, Han X, et al. Iron nanoparticles for low-power local magnetic hyperthermia in combination with immune checkpoint blockade for systemic antitumor therapy. Nano Lett. 2019;19:4287–96.
Qiu L, Chen T, Öçsoy I, Yasun E, Wu C, Zhu G, et al. A cell-targeted, size-photocontrollable, nuclear-uptake nanodrug delivery system for drug-resistant cancer therapy. Nano Lett. 2015;15:457–63.
Huang P, Gao Y, Lin J, Hu H, Liao H-S, Yan X, et al. Tumor-specific formation of enzyme-instructed supramolecular self-assemblies as cancer theranostics. ACS Nano. 2015;9:9517–27. https://doi.org/10.1021/acsnano.5b03874.
Fan R, Chen C, Hou H, Chuan D, Mu M, Liu Z, et al. Tumor acidity and near-infrared light responsive dual drug delivery polydopamine-based nanoparticles for chemo-photothermal therapy. Adv Funct Mater. 2021;31:2009733. https://doi.org/10.1002/adfm.202009733.
Guo C, Yu H, Feng B, Gao W, Yan M, Zhang Z, et al. Highly efficient ablation of metastatic breast cancer using ammonium-tungsten-bronze nanocube as a novel 1064nm-laser-driven photothermal agent. Biomaterials. 2015;52:407–16.
Zheng R, Wang S, Tian Y, Jiang X, Fu D, Shen S, et al. Polydopamine-coated magnetic composite particles with an enhanced photothermal effect. ACS Appl Mater Interfaces. 2015;7:15876–84. https://doi.org/10.1021/acsami.5b03201.
Núñez C, Capelo JL, Igrejas G, Alfonso A, Botana LM, Lodeiro C. An overview of the effective combination therapies for the treatment of breast cancer. Biomaterials. 2016;97:34–50.
Smith BR, Ghosn EEB, Rallapalli H, Prescher JA, Larson T, Herzenberg LA, et al. Selective uptake of single-walled carbon nanotubes by circulating monocytes for enhanced tumour delivery. Nat Nanotechnol. 2014;9:481–7.
Yallapu MM, Jaggi M, Chauhan SC. Curcumin nanoformulations: a future nanomedicine for cancer. Drug Discov Today. 2012;17:71–80.
Li Z, Huang H, Tang S, Li Y, Yu XF, Wang H, et al. Small gold nanorods laden macrophages for enhanced tumor coverage in photothermal therapy. Biomaterials. 2016;74:144–54.
Bao X, Yuan Y, Chen J, Zhang B, Li D, Zhou D, et al. In vivo theranostics with near-infrared-emitting carbon dots—highly efficient photothermal therapy based on passive targeting after intravenous administration. Light Sci Appl. 2018;7:91.
Ai X, Mu J, **ng B. Recent advances of light-mediated theranostics. Theranostics. 2016;6:2439–57.
Ju E, Dong K, Liu Z, Pu F, Ren J, Qu X. Tumor microenvironment activated photothermal strategy for precisely controlled ablation of solid tumors upon NIR irradiation. Adv Funct Mater. 2015;25:1574–80.
Majera D, Skrott Z, Bouchal J, Bartkova J, Simkova D, Gachechiladze M, et al. Targeting genotoxic and proteotoxic stress-response pathways in human prostate cancer by clinically available PARP inhibitors, vorinostat and disulfiram. Prostate. 2019;79:352–62.
Valencia PM, Hanewich-Hollatz MH, Gao W, Karim F, Langer R, Karnik R, et al. Effects of ligands with different water solubilities on self-assembly and properties of targeted nanoparticles. Biomaterials. 2011;32:6226–33.
Fu S, Luo X, Wu X, Zhang T, Gu L, Wang Y, et al. Activation of the melanocortin-1 receptor by NDP-MSH attenuates oxidative stress and neuronal apoptosis through PI3K/Akt/Nrf2 pathway after intracerebral hemorrhage in mice. In: Tang H, editor. Oxid Med Cell Longev. 2020;2020:1–13. https://www.hindawi.com/journals/omcl/2020/8864100/.
Lu W, **ong C, Zhang G, Huang Q, Zhang R, Zhang JZ, et al. Targeted photothermal ablation of murine melanomas with melanocyte-stimulating hormone analog—conjugated hollow gold nanospheres. Clin Cancer Res. 2009;15:876–86.
Zhang B, Wang H, Shen S, She X, Shi W, Chen J, et al. Fibrin-targeting peptide CREKA-conjugated multi-walled carbon nanotubes for self-amplified photothermal therapy of tumor. Biomaterials. 2016;79:46–55.
Yu J, Yin W, Zheng X, Tian G, Zhang X, Bao T, et al. Smart MoS2/Fe3O4 nanotheranostic for magnetically targeted photothermal therapy guided by magnetic resonance/photoacoustic imaging. Theranostics. 2015;5:931–45.
Zhou Z, Sun Y, Shen J, Wei J, Yu C, Kong B, et al. Iron/iron oxide core/shell nanoparticles for magnetic targeting MRI and near-infrared photothermal therapy. Biomaterials. 2014;35:7470–8.
Huynh E, Leung BYC, Helfield BL, Shakiba M, Gandier JA, ** CS, et al. In situ conversion of porphyrin microbubbles to nanoparticles for multimodality imaging. Nat Nanotechnol. 2015;10:325–32.
Yong T, Wang D, Li X, Yan Y, Hu J, Gan L, et al. Extracellular vesicles for tumor targeting delivery based on five features principle. J Control Release. 2020;322:555–65.
Wang S, Teng Z, Huang P, Liu D, Liu Y, Tian Y, et al. Reversibly extracellular pH controlled cellular uptake and photothermal therapy by PEGylated mixed-charge gold nanostars. Small. 2015;11:1801–10. https://doi.org/10.1002/smll.201403248.
Liu Y, Yang M, Zhang J, Zhi X, Li C, Zhang C, et al. Human induced pluripotent stem cells for tumor targeted delivery of gold nanorods and enhanced photothermal therapy. ACS Nano. 2016;10:2375–85.
Huang X, Peng X, Wang Y, Wang Y, Shin DM, El-Sayed MA, et al. A reexamination of active and passive tumor targeting by using rod-shaped gold nanocrystals and covalently conjugated peptide ligands. ACS Nano. 2010;4:5887–96.
Choi MR, Stanton-Maxey KJ, Stanley JK, Levin CS, Bardhan R, Akin D, et al. A cellular trojan horse for delivery of therapeutic nanoparticles into tumors. Nano Lett. 2007;7:3759–65.
Tchou J, Zhao Y, Levine BL, Zhang PJ, Davis MM, Melenhorst JJ, et al. Safety and efficacy of intratumoral injections of chimeric antigen receptor (CAR) T cells in metastatic breast cancer. Cancer Immunol Res. 2017;5:1152–61. https://doi.org/10.1158/2326-6066.CIR-17-0189.
Du NV, Min HK, Kim DH, Kim CS, Han J, Park JO, et al. Macrophage-mediated delivery of multifunctional nanotherapeutics for synergistic chemo-photothermal therapy of solid tumors. ACS Appl Mater Interfaces. 2020;12:10130–41.
Wang C, Ye Y, Sun W, Yu J, Wang J, Lawrence DS, et al. Red blood cells for glucose-responsive insulin delivery. Adv Mater. 2017;29:1606617. https://doi.org/10.1002/adma.201606617.
Jiang Q, Liu Y, Guo R, Yao X, Sung S, Pang Z, et al. Erythrocyte-cancer hybrid membrane-camouflaged melanin nanoparticles for enhancing photothermal therapy efficacy in tumors. Biomaterials. 2019;192:292–308.
Hu Z, Li X, Yuan M, Wang X, Zhang Y, Wang W, et al. Study on the effectiveness of ligand reversible shielding strategy in targeted delivery and tumor therapy. Acta Biomater. 2019;83:349–58. https://doi.org/10.1016/j.actbio.2018.11.021.
Cole LE, Ross RD, Tilley JM, Vargo-Gogola T, Roeder RK. Gold nanoparticles as contrast agents in X-ray imaging and computed tomography. Nanomedicine. 2015;10:321–41.
Wang S, Huang P, Chen XY. Hierarchical targeting strategy for enhanced tumor tissue accumulation/retention and cellular internalization. Adv Mater. 2016;28:7340–64.
Yang Y. Cancer immunotherapy: harnessing the immune system to battle cancer. J Clin Invest. 2015;125:3335–7.
Gu Z, Zhu S, Yan L, Zhao F, Zhao Y. Graphene-based smart platforms for combined cancer therapy. Adv Mater. 2019;31:1800662. https://doi.org/10.1002/adma.201800662.
Cao J, Gao X, Cheng M, Niu X, Li X, Zhang Y, et al. Reversible shielding between dual ligands for enhanced tumor accumulation of ZnPc-loaded micelles. Nano Lett. 2019;19:1665–74. https://doi.org/10.1021/acs.nanolett.8b04645.
Liang X, Li Y, Li X, **g L, Deng Z, Yue X, et al. PEGylated Polypyrrole Nanoparticles Conjugating Gadolinium Chelates for Dual-Modal MRI/Photoacoustic Imaging Guided Photothermal Therapy of Cancer. Adv Funct Mater. 2015;25:1451–62. https://doi.org/10.1002/adfm.201402338.
Cheng M, Zhang Y, Zhang X, Wang W, Yuan Z. One-pot synthesis of acid-induced: in situ aggregating theranostic gold nanoparticles with enhanced retention in tumor cells. Biomater Sci. 2019;7:2009–22.
Yu CYY, Xu H, Ji S, Kwok RTK, Lam JWY, Li X, et al. Mitochondrion-anchoring photosensitizer with aggregation-induced emission characteristics synergistically boosts the radiosensitivity of cancer cells to ionizing radiation. Adv Mater. 2017;29:1–9.
Yang Y, Aw J, **ng B. Nanostructures for NIR light-controlled therapies. Nanoscale. 2017;9:3698–718.
Wang X, Lin W, Zhang W, Li C, Sun T, Chen G, et al. Amphiphilic redox-sensitive NIR BODIPY nanoparticles for dual-mode imaging and photothermal therapy. J Colloid Interface Sci. 2019;536:208–14. https://doi.org/10.1016/j.jcis.2018.10.051.
Battistelli G, Cantelli A, Guidetti G, Manzi J, Montalti M. Ultra-bright and stimuli-responsive fluorescent nanoparticles for bioimaging. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2016;8:139–50.
Zhao L, Jiang M, Xu Z, Sun F, Wu X, Zhang M, et al. Selective thermotherapy of tumor by self-regulating photothermal conversion system. J Colloid Interface Sci. 2022;605:752–65. https://doi.org/10.1016/j.jcis.2021.07.134.
Nam J, Won N, ** H, Chung H, Kim S. pH-induced aggregation of gold nanoparticles for photothermal cancer therapy. J Am Chem Soc. 2009;131:13639–45.
Cheng M, Zhang Y, Zhang X, Wang W, Yuan Z. One-pot synthesis of acid-induced in situ aggregating theranostic gold nanoparticles with enhanced retention in tumor cells. Biomater Sci. 2019;7:2009–22.
Yang S, Yao D, Wang Y, Yang W, Zhang B, Wang D. Enzyme-triggered self-assembly of gold nanoparticles for enhanced retention effects and photothermal therapy of prostate cancer. Chem Commun. 2018;54:9841–4.
Ruan S, Hu C, Tang X, Cun X, **ao W, Shi K, et al. Increased gold nanoparticle retention in brain tumors by in situ enzyme-induced aggregation. ACS Nano. 2016;10:10086–98.
Liu X, Chen Y, Li H, Huang N, ** Q, Ren K, et al. Enhanced retention and cellular uptake of nanoparticles in tumors by controlling their aggregation behavior. ACS Nano. 2013;7:6244–57.
Cheng X, Sun R, Yin L, Chai Z, Shi H, Gao M. Light-triggered assembly of gold nanoparticles for photothermal therapy and photoacoustic imaging of tumors in vivo. Adv Mater. 2017;29:1604894. https://doi.org/10.1002/adma.201604894.
An L, Cao M, Zhang X, Lin J, Tian Q, Yang S. pH and glutathione synergistically triggered release and self-assembly of Au nanospheres for tumor theranostics. ACS Appl Mater Interfaces. 2020;12:8050–61. https://doi.org/10.1021/acsami.0c00302.
Zhou C, Zhang L, Sun T, Zhang Y, Liu Y, Gong M, et al. Activatable NIR-II plasmonic nanotheranostics for efficient photoacoustic imaging and photothermal cancer therapy. Adv Mater. 2021;33:2006532. https://doi.org/10.1002/adma.202006532.
Sugita N, Obara K, Yoshizawa M, Abe M, Tanaka A, Homma N. Techniques for estimating blood pressure variation using video images. In: 2015 37th Annu Int Conf IEEE Eng Med Biol Soc. IEEE; 2015. p. 4218–21. http://ieeexplore.ieee.org/document/7319325/.
Xu Y, ** P, Wang D, Zhang W. Analysis for the influence of ABR sensitivity on PTT-based cuff-less blood pressure estimation before and after exercise. J Healthc Eng. 2018;2018:1–10. https://www.hindawi.com/journals/jhe/2018/5396030/.
Yali Zheng, Yan BP, Yuanting Zhang, Yu CM, Poon CCY. Wearable cuff-less PTT-based system for overnight blood pressure monitoring. 2013 35th Annu Int Conf IEEE Eng Med Biol Soc. IEEE; 2013. p. 6103–6. http://ieeexplore.ieee.org/document/6610945/
Wang Y, **e J, Kang J, Choi W, Jangili P, Zhang B, et al. Smart acid-activatable self-assembly of black phosphorous as photosensitizer to overcome poor tumor retention in photothermal therapy. Adv Funct Mater. 2020;30:2003338. https://doi.org/10.1002/adfm.202003338.
Peng J, **ao Y, Li W, Yang Q, Tan L, Jia Y, et al. Photosensitizer micelles together with IDO inhibitor enhance cancer photothermal therapy and immunotherapy. Adv Sci. 2018;5:1700891. https://doi.org/10.1002/advs.201700891.
Huang C, Chen X, Xue Z, Wang T. Effect of structure: a new insight into nanoparticle assemblies from inanimate to animate. Sci Adv. 2020;6:eaba1321. https://doi.org/10.1126/sciadv.aba1321.
Liu S, Pan X, Liu H. Two-dimensional nanomaterials for photothermal therapy. Angew Chem Int Ed. 2020;59:5890–900.
Li X, Lovell JF, Yoon J, Chen X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat Rev Clin Oncol. 2020;17:657–74. https://doi.org/10.1038/s41571-020-0410-2.
Acknowledgements
Thanks to Zitong Ma from Qilu University of Technology (Shandong Academy of Sciences) for this review’s vocabulary and grammar guidance. Thanks also to Mogen Zhang from Weifang Medical University for the draw of Scheme 1 in this review.
Funding
The authors are indebted to the financial support from the National Natural Science Foundation of China (No. 81774125, 81973671), the Natural Science Foundation of Shandong Province (No. ZR2019BB071) and the major innovation and technology engineering project of Shandong Province (No. 2019JZZY011106).
Author information
Authors and Affiliations
Contributions
JM and WZ designed research; LZ, XZ, XW, and XG researched and wrote the paper. All authors read and approved the final manuscript.