Abstract
Background
Seasonal floods pose a commonly-recognised barrier to women’s access to maternal services, resulting in increased morbidity and mortality. Despite their importance, previous GIS models of healthcare access have not adequately accounted for floods. This study developed new methodologies for incorporating flood depths, velocities, and extents produced with a flood model into network- and raster-based health access models. The methodologies were applied to the Barotse Floodplain to assess flood impact on women’s walking access to maternal services and vehicular emergency referrals for a monthly basis between October 2017 and October 2018.
Methods
Information on health facilities were acquired from the Ministry of Health. Population density data on women of reproductive age were obtained from the High Resolution Settlement Layer. Roads were a fusion of OpenStreetMap and data manually delineated from satellite imagery. Monthly information on floodwater depth and velocity were obtained from a flood model for 13-months. Referral driving times between delivery sites and EmOC were calculated with network analysis. Walking times to the nearest maternal services were calculated using a cost-distance algorithm.
Results
The changing distribution of floodwaters impacted the ability of women to reach maternal services. At the peak of the dry season (October 2017), 55%, 19%, and 24% of women had walking access within 2-hrs to their nearest delivery site, EmOC location, and maternity waiting shelter (MWS) respectively. By the flood peak, this dropped to 29%, 14%, and 16%. Complete inaccessibility became stark with 65%, 76%, and 74% unable to access any delivery site, EmOC, and MWS respectively. The percentage of women that could be referred by vehicle to EmOC from a delivery site within an hour also declined from 65% in October 2017 to 23% in March 2018.
Conclusions
Flooding greatly impacted health access, with impacts varying monthly as the floodwave progressed. Additional validation and application to other regions is still needed, however our first results suggest the use of a hydrodynamic model permits a more detailed representation of floodwater impact and there is great potential for generating predictive models which will be necessary to consider climate change impacts on future health access.
Similar content being viewed by others
Background
Geographical barriers to healthcare facilities are linked to poor uptake of maternal health services, and worsened maternal and neonatal outcomes [1,2,3,4,5]. Geographical health access models can be created using GIS (geographical information systems) software [6,7,8,9,10,11,12,13,14,15]. These models can account for the impact of geographical barriers on health access when calculating population travel times and distances to health services. This approach is commonplace in maternal health research as geographic health access models are able to identify underserved populations, provide evidence to support interventions on improving accessibility, and identify the most influential geographical barriers to access [16,17,18,19]. For example, Ruktanonchai et al. [1] used cost-distance analysis as part of their study investigating maternal healthcare utilisation, and found that increased geographical inaccessibility had the strongest association with reducing maternal care usage in five East African countries.
Many geographical barriers are static, permanent features on the landscape such as rivers, mountains, and roads. However, flooding is an important temporary geographic barrier which can impact access [11, 20,21,22]. In low-income countries with distinctive seasonal climates, floods are a regular impactful barrier to accessing health facilities [11, 16, 17, 23,24,25,26]. Many studies have recognised floods as an important geographical barrier [11, 21, 24,25,26] as they can persist for long periods of time, restricting health access and isolating entire communities. They also impact the supply-side of health access by causing medical supply chain shortages and hindering referrals [24, 27]. As a result, in the wet season, morbidity and mortality can be increased compared to the dry season [18, 28,29,30,31,32]. Despite the detrimental impacts of floods on health systems, few studies have considered or modelled the impacts of floods on health access (see [11, 17, 33] for examples). Failure to account for floods leads to models that over-estimate accessibility.
There is a dearth of research on how floods directly impact access through space and time. Blanford et al. [17] presented contrasting maps of dry and wet season access which emphasised significant drops in accessibility due to seasonal impacts, but the maps were otherwise static representations which limited understanding of how access changes between the peak dry and peak wet season as well as the timings of the transitions throughout intermediate flood stages. Makanga et al. [11] pioneered the first spatio-temporal framework for assessing access changes under seasonal conditions using daily records of precipitation and satellite-derived flood extents. Whilst this approach substantially advanced access models, there persists a limited understanding of the relationship between floodwater variables (depth and velocity in addition to extent) and access. Extents can only be treated as impassable barriers in the absence of additional data on depth and velocity that can be utilised to characterise flood hazard. However, not all floodwaters will be equally inaccessible; some floodwaters may be a few centimetres deep and thus navigable at reduced speeds, whilst others may be metres deep. Consequently, including these additional hydrodynamic variables would improve the real-world representativeness of floodwaters in access models. This is advantageous as it better constrains model estimations on the duration of accessibility impact, which populations are isolated, planning medical supplies, and assessing referral capabilities.
This study aims to improve the representation of floodwaters in health access models through a new methodology. For the first time, we couple vector- and raster-GIS-based access models with a hydrodynamic flood model to create novel geospatial frameworks that utilise the hydrodynamic variables of flood depth and velocity. The new framework is applied to the Barotse Floodplain, Zambia, which presents an appropriate case study to investigate two critical scenarios of access to maternal services, for which access models are routinely applied:
-
A)
The ability of women of reproductive age to walk to their nearest healthcare facility (HF) offering maternal services (raster-based model).
-
B)
The ability of delivery sites (facility providing a trained birth attendant) to make pregnancy-related emergency referrals to the nearest emergency obstetric care location (EmOC) by vehicular road transportation (vector-based model).
The following objectives were implemented to assess these scenarios:
Objective 1: To calculate walking travel times for women to their nearest maternal services, and to calculate driving travel times for emergency referrals between delivery sites and EmOC sites.
Objective 2: To calculate the number and percentage of women that have timely walking access within 2-hours to maternal services, and that can be referred within a timely 1-hour from a delivery site to an EmOC site.
Objective 3: To assess the impact of floods on increasing walking and driving travel times, and how that affects the number and percentage of women considered to have timely access to maternal services.
Objective 4: To quantify the number and percentage of women who become inaccessible due to floodwater impact as it varies in each month.
Objective 5: To evaluate the interaction between the ability of women to walk to the nearest delivery site and the referral system.
Methods
Study area
The Barotse Floodplain is a large African floodplain located in the Upper Zambezi valley, Zambia (Fig. 1). Due to the movements of the Inter-Tropical Convergence Zone (ITCZ), the Zambezi has a strongly seasonal discharge which causes the floodplain to experience annual floodwaves. The amount of precipitation that falls in the upstream catchment is significant in determining the magnitude of each floodwave, and the timing of upstream precipitation controls the timing of flooding as there is a delay of approximately two months between peak rainfall and peak inundation ([34]; Additional file 1: Figure S1). Extensive, slow-moving floodwaters typically persist between February and June due to the floodplain being extremely flat and attenuating flow [35]. The peak of the floods occurs in late March or early April where the total inundated area can be as great as 10,750 km2 [36].
The floodplain is inhabited by the semi-nomadic Lozi people, whose population within the study area (Fig. 1) is estimated using the High Resolution Settlement Layer (HRSL) to be ~ 44,600 as of 2021 [37]. With the exception of the Barotse Floodplain Causeway, roads on the floodplain are unpaved and only navigable by four-wheel drive vehicles (4WD) or motorcycles [38]. The Lozi predominantly move on foot, by oxen-cart, and dugout canoes on open waterbodies [39,40,41]. Oxen-cart and dugout canoes are influential local modes of transport but were not incorporated in this study due to a lack of data to characterise their usage and due to a lack of suitable methods for incorporating boats into access models [42,43,44,45].
Access models require data to understand the combination of transport modes, travel speeds, and also other influential variables such as financial cost and waiting times [15, 44, 46,47,48,49]. It is common for access models to represent transport as individualised rather than multimodal in the absence of such data to prevent incurring significant assumptions and uncertainties [46, 50]. The walking model is therefore a conservative measure of access as individuals potentially have access to faster modes of transports, which the walking model doesn’t account for and consequently assumes longer travel times. This is preferable to a model that may include multiple methods of transportation but without substantial data to support its parameterisation, consequently introducing unknown variability that may overestimate accessibility. Oxen-carts have similar travel speeds to walking [51,52,53] so their usage was assumed to be represented adequately in the walking model.
Maternal mortality is a key health concern on the floodplain, with previous studies indicating that Western Province has the highest maternal mortality ratio compared to any other province in Zambia [54, 55]. Efforts are ongoing to increase the number of births at health facilities as a mitigation strategy. Whilst many other socioeconomic and sociodemographic factors also contribute to poor maternal services uptake and consequently poor maternal outcomes [56], geographical access during floods are the primary focus. The annual floods complicate mitigation initiatives as they obstruct women accessing care, hinder emergency referrals, and cause difficulties in ensuring facilities remain operational [38].
Locations of maternal services and women of reproductive age
A geolocated dataset of public health facilities on and surrounding the floodplain (n = 75) was acquired from Zambia’s Ministry of Health Master Facility List (MFL) [57]. The MFL provides no information on services provided at facilities, so the 2012 List of Health Facilities in Zambia [57] was used to supplement information on facility type and maternal services (Table 1); this document contained the most up-to-date information available. For facilities constructed since 2012 (n = 25), their services were assumed by assigning the most common services typically offered by health facilities of the same type; the majority were health posts (the lowest level of healthcare catering to distant communities). EmOC can be classified as either basic or comprehensive, depending on the presence of specific signal functions (major interventions for reducing maternal and neonatal mortalities) [58]. The 2012 facility list makes no reference to signal functions, so EmOC is assumed to be at least basic for all facilities and to meet UN standards. Data on women of reproductive age as of August 2021 were obtained from the HRSL dataset [37]. HRSL provides gridded population density data at a spatial resolution of 30 m. The HRSL data were estimated using a binary top-down modelling approach where census data were proportionally attributed to buildings identified through convolutional neural networks operating on satellite imagery with a spatial resolution of 50 cm [37]. For the purpose of this study, these were converted into geolocated points representing the number of women (n = 8,130) living within each 30 m grid cell of the study area.
No complete road network dataset was available for the Barotse Floodplain, so floodplain roads were manually delineated by visual inspection of very high resolution (< 5 m) composite satellite imagery sourced in the dry season from Google Earth and Microsoft Bing Maps. Delineation was conducted between October 2019 and October 2020, with additional checks of network completeness conducted in April, June, and July 2021 before the dataset was used. Roads were classified as either primary, secondary, track, elevated highway, or water crossing. Road type was unpaved, with the exception of the Barotse Floodplain Causeway (an elevated highway running across the floodplain). Beyond the floodplain, OpenStreetMap (OSM) [59] data were sourced in June 2021 and recoded to match the same classification as the floodplain roads (Additional file 1: Table S1). Gaps in OSM coverage were resolved through manual delineation. GPS tracks of recorded journeys across the floodplain were used to validate the accuracy of the delineation procedure. Additional ground-truthing was provided by local health officers who provided guidance on the local environment.
Permanent waterbodies and floodwaters
A shapefile of the positions and average widths of rivers and canals on the floodplain were provided by Willis et al. [60]. These waterbodies are permanent and hence were modelled as static barriers to access. To convert the waterbodies shapefile to raster, the waterbodies were first buffered according to their average width and then rasterised. Non-static, temporary floodwaters were obtained through flood modelling. The LISFLOOD-FP hydrodynamic inundation model [61] was run for the Barotse Floodplain between October 2017 and October 2018 to produce monthly rasters containing information on floodwater depth (m), velocity (m s− 1), and extent (m2). The 2018 hydrological year was selected for modelling as the floodwave was one of the largest experienced in recent years yet remained within the expected interannual flood magnitude, and the temporal aspect of the floodwave was characteristic of a typical year [62].
The flood model set up is described by Willis et al. [60] and was configured to represent the hydrological processes operating on the floodplain, assuming flows are mostly subcritical and low velocity. Terrain data for the flood model were obtained from a high-resolution TanDEM-X1 Digital Elevation Model (DEM) from 2016, which has a vertical accuracy of ~ 2 m on the floodplain and a native spatial resolution of 12 m [63] but was resampled to 100 m for the flood model due to computational costs. The model was calibrated and validated using both gauge data provided by the Water Resources Management Agency (WARMA) and remotely-sensed flood extents derived from Landsat (30 m spatial resolution). Willis et al. [60] demonstrated that the model reproduced the characteristics of the 2018 floodwave, with its best performance occurring at the flood peak (goodness of fit, F2 = 0.62). Lower performance metrics were returned during the intermediate flood stages (F2 = 0.10); however, these values likely reflect issues with using satellite-derived flood extents for validation. Optical sensors such as Landsat are unable to recognise vegetated waters, so areas denoted as “false positive inundation” during validation are likely truly inundated but not detectable by Landsat [64].
Modelling access to care: walking
A semi-automated raster-based model was created that estimated walking travel times for women to their nearest delivery site, EmOC location, and maternity waiting shelter respectively (Fig. 2). Travel times were computed from each populated point (placed at the centroid of the 30 m cells containing a population in the gridded HRSL dataset) rather than aggregating the HRSL population data into a coarser geographic unit. Women were assumed to walk to the nearest healthcare facility offering a maternal service rather than bypass in favour of facilities further away.
Impedance surfaces were first created in an automated workflow within FME Workbench 2020.2 [65, 66]. Impedance (also known as friction) surfaces are a grid of cells representing the ease of movement across a geographical landscape; each cell contains a value which denotes how difficult it is to move through [13, 67]. In this study, impedance surfaces with a 10 m spatial resolution were output at a monthly timestep by mosaicking together data on roads, permanent waterbodies, and the corresponding month’s floodwater rasters representing depth, velocity, and extent. The flood rasters were used to determine whether flood hazard was great enough to render an area inaccessible. In the walking scenario for pregnant woman, areas were modelled as impassable if flood depths exceeded 1 cm. Where data overlapped when creating the impedance surface, the maximum impedance value was represented in the final surface. Slope and land use data were not considered due to the floodplain being extremely flat with a near-homogenous land use. A walking speed of 5 km hr− 1 is typically used to represent an average walking speed in the absence of topographical impediments [2, 12, 68,69,70,71]. In this study walking speeds were parametrised to reflect a decreased mobility of pregnant women: 4 km hr− 1 for on-road travel, 3 km hr− 1 for off-road travel, and 0 km hr− 1 for areas that were flooded as any cells that contained floodwaters exceeding 1 cm depth were considered to be completely impassable. Flooded cells were completely removed from the impedance surfaces so that they could not be routed through.
The monthly impedance surfaces were then transferred to QGis Desktop 3.16.6 with GRASS 7.8.5. The cost-distance algorithm r.cost [72] was used to compute monthly minimum isotropic accumulated cost surfaces of access [12, 67, 73]. These surfaces were computed from the population points to delivery sites, EmOC, and MWS respectively. The r.cost algorithm was selected due to its superior accuracy over other cost-distance algorithms resulting from movement calculations occurring over 16-cells rather than 8-cells [74,75,76,77]. The cost surfaces were discretised into travel time thresholds with 2-hours identified as the critical threshold representing timely access to a maternal service [46, 78,79,80]. A closest facility analysis was then performed by extracting the shortest path travel times for each populated point and identifying health facility service areas.
Modelling access to care: driving
An automated network-based model was created in FME Workbench 2020.2 to calculate emergency referral travel times between delivery sites and emergency obstetric care locations (Fig. 3). The referral chain modelled assumes that women walk to their nearest delivery site, experience obstetric complications during labour, and are then immediately referred to the nearest EmOC location by an emergency 4WD vehicle. Hence, emergency referral times refer explicitly to the time taken to drive between delivery sites and EmOC locations, and there is no consideration of referrals for women who experience obstetric complications at home and may bypass facilities to immediately access EmOC.
Maternal referral systems, including Zambia’s, are typically hierarchical and designed for healthcare practitioners to make referrals [81,82,83] with practices in place that can result in discouraging self-referrals [84]. Hence, referral models commonly are set-up to observe only referral pairs of sending and receiving facilities, with no consideration of women bypassing facilities to self-refer [85, 86].
To calculate travel times, speed limits were first assigned for each road segment in the road network dataset (Table 2 ; [87]) whilst speed limits do not apply to emergency vehicles, the values represent maximum possible speeds along the different road conditions. To account for the impacts of floodwater variables on road accessibility, the road network dataset was intersected at a monthly time interval with the corresponding floodwater depth and velocity rasters (Fig. 3).
The updated road network dataset for each month thus designated speed limits by the monthly flooded status of each road. If no floodwaters intersected a road segment, it was assumed to be dry and unflooded, so a speed limit was assigned based upon Zambia’s speed limit regulations [87]. If floodwaters intersected a road segment, a series of conditional statements were used to determine the impact to accessibility (either a speed limit reduction or complete impassability) (Table 2).
The conditional statements use depth and velocity thresholds collated from literature on vehicular instability to determine the hazard that floods pose to a 4WD vehicle [88,89,90,91,92]. Floodwater depth and velocity are the two primary hydrodynamic variables that determine flood hazard to a vehicle, so assessment of both is critical. For example, floodwaters with shallow water depths and high velocities are equally as hazardous as deep floodwaters with low velocities. The thresholds provided by the Australian Rainfall and Runoff Project [93] are considered the most suitable and best reference for stability criteria [94] as nearly all experiments show vehicular instability to occur at depths and velocities greater than the criteria (Additional file 1: Table S2). In this study, we followed the guidance of the Australian Rainfall and Runoff Project in setting a maximum flood depth stability criteria of 0.5 m, but imposed a more conservative maximum flood velocity stability criteria of 1.0 m s − 1. The resulting statements assume that: drivers have omniscient knowledge of floodwater properties and the hazard they pose to their vehicle; drivers will drive through floodwaters where theoretically safe to do so; depth and velocity are the only variables important to vehicular stability; all emergency referrals use a 4WD vehicle; all road conditions are equal; and drivers always drive safely and at appropriate speed.
Roads are considered dry and accessible at usual speed limits when flood depth is 0 m and flood velocity is 0 m s− 1. Roads are considered wet when flood depth is greater than 0 m but less than 0.01 m, and speed limits are reduced by a third. Roads are denoted as flooded when flood depth is greater than 0.01 m but less than 0.1 m, and deeply flooded when flood depth is greater than 0.1 m but less than 0.5 m, with speed limits drastically reduced. Roads become impassable when either the absolute maximum flood depth threshold of 0.5 m or maximum flood velocity threshold of 1.0 m s− 1 are exceeded.
For each month, an origin-destination cost matrix was then computed between every delivery site and every EmOC location, using Dijkstra’s algorithm to calculate travel times [95]. A closest facility analysis was performed to identify the shortest travel time to EmOC for each delivery site, and the corresponding path and identity of the closest facility. A one hour travel time threshold was used as an indicator of timely access to life-saving emergency obstetric treatment; this “golden hour” is commonly used as an indicator of timely access to EmOC due to drastically reduced morbidity and mortality outcomes if EmOC is administered within an hour [96,97,98]. Health facilities were considered inaccessible and unable to make or receive referrals if they were disconnected from the road network, whether by floodwater impact or simply due to a lack of existing road connection.
Identifying potential referrals between delivery sites and EmOC is complicated by the multiple impacts of floods on different parts of the referral system. Firstly, women must be able to walk to a delivery site, and the proportion of women with access alters due to floodwave passage. Secondly, the positioning of floodwaters alters which delivery sites are being accessed each month; this in turn changes the number of women served by facilities each month. Finally, floods directly impact the ability of delivery sites to make referrals to EmOC. Consequently, herein we accounted for these complications by explicitly considering only referral coverage and referral times in each month for the delivery sites that the walking model showed were being accessed by women. This criterion weighted the referral results based upon the impact to the floodplain population.
Results
Characterisation of the 2018 floodwave
The results showed that both walking times and referrals were impacted monthly between October 2017 and October 2018 due to the changing depths, velocities, and extent associated with the passage of the annual floodwave (Additional file 1: Table S3). Consequently, characterising the floodwave dynamics was important to the interpretation of the access results.
Floodwaters first appear in the Luena Flats in November 2017, with floodwater depths below 0.3 m and velocities below 0.2 m s− 1 (Fig. 4). By December 2017, floodwaters appear in the Luanginga Valley and Barotse Floodplain. All floodwaters increase in extent and depth from January 2018 until the flood peak in March and April 2018 when inundation extent is greatest and deep floodwaters (> 1 m) span to the escarpment of the Barotse Floodplain; floodwaters in the tributary valleys are extensive but shallower. From June 2018, flood drawdown occurs. By October 2018, floodwaters have mostly receded, but some shallow floodwaters (~ 0.2 m) persist in the Luanginga Valley and Luena Flats. Throughout the floodwave, velocities remain low, infrequently exceeding 0.5 m s− 1.
Modelling access to care: walking
Timely access within 2 h was most optimal in the dry season month of October 2017. Of the 8,130 women of reproductive age living on the floodplain, 55% had timely access to their nearest delivery site, 19% had timely access to their nearest EmOC location, and 24% had timely access to the nearest MWS. Despite this being the peak month for access to maternal services, the average journey is long, and large disparity exists in travel times. The average walking times for women of reproductive age living on the floodplain were 109 min (1.8 h) to the nearest delivery site, 280 min (4.7 h) to the nearest EmOC location, and 251 min (4.2 h) to the nearest MWS. However, women located in the most remote areas of the floodplain must walk a maximum travel time of 420 min (7 h) to the nearest delivery site, and 845 min (14.1 h) to both the nearest EmOC location and MWS.
The spatio-temporal distribution of floodwaters negatively impacted the ability of women to walk to their nearest maternal services through increases in travel times and increases in inaccessibility (Figs. 5, 6 and 7; Additional file 1: Table S4). By the peak of flooding in March 2018, the percentage of women of reproductive age with timely access within 2 h to their nearest delivery site, EmOC location, and MWS dropped to 29%, 14%, and 16% respectively. The majority of women had no access at all in March 2018, with 65% of women unable to access any delivery site, 76% of women unable to access any EmOC location, and 74% of women unable to access any MWS.
A higher walking time to the nearest facility in the dry season indicates an increased likelihood of experiencing inaccessibility at the peak of the floods. For women located more than two hours away from their nearest delivery site in October 2017, 89% became unable to access any delivery site by March 2018. In comparison, inaccessibility rose to a maximum of 33% in March 2018 for women who had access to the nearest delivery site within an hour in October 2017. Similar patterns exist for inaccessibility rates to EmOC and MWS. For women located more than 2 hours away from the nearest EmOC location in October 2017, 87% experience inaccessibility by March 2018, compared to 17% of women who have dry season access within an hour. For women located more than two hours away from the nearest MWS in October 2017, 89% experience inaccessibility by March 2018 compared to 14% of women who have dry season access within an hour.
There is temporal variation in both the onset and duration of flood impacts to the different maternal services. Rising floodwaters impact access to EmOC and MWS in December 2017, a month earlier than they impact access to delivery sites. In November 2017, 3% of the 8,130 women are considered unable to access any delivery site, EmOC or MWS. Inaccessibility to EmOC and MWS rises to 45% and 51% respectively in December 2017, whilst inaccessibility to delivery sites only rises to 5% across the same time period (Fig. 6). Similarly, elevated inaccessibility to EmOC and MWS persists from July 2018 onwards whilst accessibility to delivery sites is continually restored. Reductions in inaccessibility to EmOC and MWS completely stagnate from August 2018 until the final model timestep in October 2018 whilst inaccessibility to delivery sites has returned to its pre-flood values; this relates to the modelled continued presence of shallow floodwaters persisting in the Luanginga Valley, which impacts access to EmOC and MWS.
Percentage of women unable to walk to maternal services in each month the analysis was conducted between October 2017 and 2018. The red line indicates modelled floodwater extent as measured across the floodplain study area. Health facility refers to any facility that can be accessed irrespective of services provided
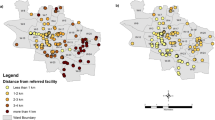
Modelling access to care: driving
In the 2018 hydrological year, 40 healthcare facilities were the nearest delivery site in at least one month for women living on the floodplain. Of these, 7 also provided EmOC services and were assumed not to make road referrals to other EmOC locations. Of the 33 facilities that can only provide delivery services, four lack any direct road connection and were unable to make road referrals year-round.
October 2017 is the optimal month for emergency referrals with 65% of women modelled to have timely referrals within an hour from their nearest delivery site to EmOC. There are 27 health facilities that act as the nearest delivery site to women in October 2017, and all are able to make referrals. Of these, only 4 are unable to make referrals to the nearest EmOC location within an hour. The average referral time is 30 min, whilst the maximum referral time is 89 min.
As the floodwave progresses, the referral system is shown to be impacted (Additional file 1: Table S5). The total number of delivery sites able to make referrals and to make timely referrals within an hour decreased with an increase in mean floodwater depth and extent (Figs. 8 and 9). By March 2018, floods had most detrimentally impacted emergency referrals with the proportion of women modelled to have timely referrals drop** to just 23%. There are 25 health facilities operating as the nearest delivery site to women living on the floodplain, but only 17 are able to make a referral to an EmOC site, and only 14 are able to do so within an hour. The mean referral time is only slightly elevated at 35 min, but the maximum referral time increased to 205 min due to floodwater impact.
Vehicular referral times between delivery sites and EmOC locations compared. October 2017 is the optimal month for referrals, whilst March 2018 is the peak of flood impacts on referrals. Areas coloured orange denote routes outside of the “Golden Hour” whether due to high travel times or complete inaccessibility
Delivery sites with the lowest referral times in the dry season were shown to remain consistently accessible with negligible impacts to their referral times throughout the hydrological year, whilst delivery sites with the highest referral times were most impacted. EmOC sites are situated in urban areas, and thus delivery sites located closer to urban areas experienced fewer inundated roads, and had the benefit of denser connectivity of urban roads to mitigate for any closures through the provision of alternate routes. This pattern reflected a disparity in provision of EmOC services to rural and urban populations.
Floods evidently have a detrimental impact on referral coverage and travel times. However, when assessing the relative monthly position of women within the referral system (Fig. 10), it is clear the primary reduction in the proportion of women who could be referred to EmOC in a timely manner occurred due to the complete inability of women to even first reach a delivery site rather than because of an increase in the number of women waiting to be referred by a facility with impacted referral abilities.
Number of delivery sites being accessed by women each month and their referral capability. The red line indicates modelled floodwater extent as measured across the floodplain study area. A “serving delivery site” refers to a facility which is being accessed by women and has a direct road connection to EmOC so referrals are possible; the number and location of these changes each month as floodwaters cause women to access different facilities
Discussion
Novelty
This study demonstrated a novel geospatial methodology for incorporating modelled floodwater variables into network-based and raster-based models in order to account for dynamic flood impacts on walking and driving accessibility to maternal health services. To our knowledge, this represents the first time that a hydrodynamic inundation model has been coupled with a raster-based health access model, and the first usage of quantitative hydrodynamic model outputs in network analysis for a low-income country. This work has expanded upon previous geographic access models (e.g., [11, 17, 99, 102]) through the consideration of flood depth and velocity on access to maternal services, develo** frameworks that are more physically representative of this important seasonal phenomenon but still remain appropriate for application in data-limited, low-income countries. Most notably, our approach using flood models offers predictive capabilities to health access models that expands the scope to quantify future access, such as under climate change.
The importance of hydrological seasonality in affecting access has been recognised but seasonal methodologies were nearly all limited to creating static dry and wet season maps (e.g., [17]). The explicit incorporation of monthly flood depth and velocity demonstrated that representation of physical hydrological processes is important. Dynamic spatio-temporal variations in floods interact with the location of maternal services and populations to create dynamic spatio-temporal variations in access. The varied temporal onset and resolution of flood impact on different maternal services is one crucial example of an important access phenomenon that would have otherwise been obscured by previous static methodologies. Consequently, the results of this study support the conclusions of Makanga et al. [11] in stating that continuous fluctuations in access resulting from seasonality are unable to be represented by two contrasting scenarios of wet season access and dry season access.
Consideration of floodwater depths and velocities permitted a more detailed conceptual representation of how floodwaters impact driving rather than simply assuming all floodwaters are impassable. Thresholds to define driving accessibility and driving speeds through different depths and velocities were parameterised from safety criteria recommendations and a comprehensive review of vehicular instability literature [113]. Optical sensors are sensitive to cloud cover which predominates during the wet season; extensive cloud cover above the Barotse Floodplain prevented floodwaters from being visible in MODIS imagery for the entire of March 2018, and others have reported difficulty in obtaining cloud-free imagery for the region [34, 36]. Optical sensors also experience difficulty detecting vegetated waters, as do radar sensors albeit to a lesser extent [114,115,116]. Most readily-available flood extents rely on algorithms suitable for map** open waters [115, 117] leading to flood omission where inundated vegetation is present [113]. Satellite-derived flood extents were found to underestimate flood inundation due to emergent vegetation in the central axis of the Barotse Floodplain and in the Luena Valley in previous studies [36, 60, 114]. This detection limitation is problematic as we have identified herein that women’s access to maternal health service is especially sensitive to the persistent vegetated waters in the Luena Valley, thereby emphasising their need to be adequately represented in an access model. Whilst ground-truthing can be used to improve the accuracy of satellite-derived flood extents, the surveys are expensive and time-consuming [36]. Hydrodynamic models thus offer an alternative as they do not suffer from the same observational biases, can provide reliable flood information at the temporal and spatial resolution of the modeller’s choosing, and additionally provide water velocity information for hazard-based approaches. Modelling offers potential new advantages for assessing flood risk on health access, such as the simulation of extreme events, climate change analysis, near-time forecasting, and development of early-warning systems.
Findings and significance for the Barotse Floodplain
This is the first model detailing geographic access to maternal health services for the Barotse Floodplain, indicating that floods exert a clear control on women’s ability to access crucial maternal health services. The annual floodwave was shown to impact walking times and inter-facility emergency referrals, but at the peak of the floods, the majority of women (65%) were isolated due to floodwater impact and were unable to access any health facility (HF). Rural populations have been shown to utilise services less than their urban counterparts when there are substantial geographic barriers to accessing care [118,119,120], hence floods are likely to be acting as a significant barrier to healthcare uptake in the Barotse Floodplain, with potential implications of increased maternal and neonatal morbidities and mortalities. In the case of the referral system, our findings show that inabilities to make emergency referrals predominantly arise from floods isolating women and preventing them from reaching a delivery site first (where a referral can take place), rather than impacting referrals between delivery sites and EmOC sites. This suggests that efforts to improve the referral system should first ensure women are able to access facilities, such as through the use of interventions like maternity waiting shelters where at-risk women can stay at an EmOC location ahead of delivery. In order to fully comprehend the local situation, this study’s geographic access data requires interpretation with data on health services utilisation and morbidities and mortalities as well as qualitative data on the lived experiences of women in the region. Such analysis would identify the relative importance of geographic access and flood impacts compared with other variables that affect health access, which would be necessary for any future health intervention planning.
In addition to the maternal services of delivery sites, MWS, and EmOC considered here, the lack of access to any HF for many women during the floodwave also has implications for other mother-baby services, such as uptake of antenatal care. Antenatal care is another effective strategy for reducing maternal mortalities, and a minimum of four visits throughout pregnancy are recommended [121, 122]. Given that flooding occurs between December to August for a total of nine months out of the year, a woman can expect to have her access to maternal services impacted at some point throughout her pregnancy. Strong feedback loops can emerge between the perception of flooding and healthcare-seeking behaviours of women [56, 123], so care needs to be taken to ensure that: (1) women are educated on the necessity of antenatal care and skilled professional deliveries so that they are motivated to seek out these services [121, 124] ; (2) the healthcare quality of facilities is maintained throughout flood months to avoid dissatisfaction and a perception that quality is poor year-round [124]; (3) the impacts of floods on access to maternity services are mitigated, such as through the provision of community health workers who can extend access to those located in the most remote regions [125].
Our spatio-temporal approach identified the communities of women on the Barotse Floodplain who experienced exceptional difficulties or isolation in accessing maternal services during flood months, in addition to the mechanism behind why floods had such a disproportionate impact on their access. It is shown that floods impacted women’s access to EmOC and MWS services in December 2017, a month earlier than floods impacted access to delivery sites. This temporal variation is caused by fewer facilities offering EmOC and MWS, which creates geographic vulnerabilities for specific locations of women in the Luena Flats and on the floodplain near Kalabo. A total of 40 health facilities offer delivery sites, and the placement of delivery sites within the existing health infrastructure is optimal as indicated by the pattern of women’s access to the nearest health facility being identical to the pattern of women’s access to the nearest delivery site (Fig. 6). However, only 22 facilities offer MWS, and only 10 offer EmOC. In the Luena Flats, the lack of a MWS situated on the true-right floodplain escarpment prevents many women from being able to access a MWS for the majority of the year. The Luena Flats floods earlier than the Barotse Floodplain and floodwaters persist for longer, preventing women from crossing the valley to reach a MWS. Near to Kalabo, there are 3,288 women living on the floodplain who are geographically restricted within the confinements of the Zambezi. These women rely on connecting roads through to Kalabo to access any EmOC and MWS, but these roads become inundated in December 2017 due to the earlier flooding of the Luanginga Valley. As shallow floodwaters in the valley persist from August 2018 onwards, these women remain unable to access any EmOC and MWS. The identification of this finding permits further investigation into interventions that could potentially be conducted to resolve this inequity in access.
Confidence in the access model findings were ascertained through comparison with available literature. The flood model well-recreated the typical inundation pattern of the annual floodwave [60, 114] which resulted in the access models reproducing key accessibility patterns that have been previously reported; these included the impassability of roads in the Luanginga Valley from December onwards [126], and the continued presence of floodwaters in August that impede access [127].
Limitations
This study necessarily simplified the complexity of women’s access to maternal services, and the travel times presented are estimates rather than absolute and precise. The model is explicitly a representation of the physical ability to reach health services, so assumes that people decide to seek care immediately and receive appropriate care at arrival to a facility. This ignores complex delays in seeking care resulting from human decision-making, and delays and problems of receiving good care such as a lack of available staff [27, 56, 121, 123, 128,129,130,131,132].
The available population and health facility data used in this study also presented additional limitations. The usage of HRSL population density data assumed that the Lozi population remained static throughout the year. However, the Lozi people are semi-nomadic and will move between locations depending on flood stage. As no data were available to characterise these movements, it was not possible to account for these yearly migrations. Therefore, there is some uncertainty regarding the location and number of women in different areas of the floodplain in the wet season. The available published health facility data were a decade old and categorised only three maternal services: delivery site, EmOC, and maternity waiting shelter. This introduced some uncertainty about the number and location of maternal services in the study area. After the study’s completion, it was communicated that all rural and urban health centres offer basic emergency obstetric care (BEmOC), whilst hospitals only offer comprehensive emergency obstetric care (CEmOC). Additional classification of facilities into BEmOC and CEmOC offers additional sophisticated insights into emergency maternal care that should be used in subsequent analyses for the region.
The study also made assumptions that add uncertainty to the modelled travel times. In the network-based model, driving speeds are assigned based on government legislation. However, road condition influences real-world driving speeds, with the modelled driving speeds optimistic for roads in poor condition. Road condition is very variable on and surrounding the Barotse Floodplain; however, this information is difficult to ascertain from satellite imagery alone, hence why distinctions in road condition were not made. Additionally, it is assumed that emergency 4WD vehicles are present and immediately able to make emergency referrals. Whilst a common assumption, in reality, these vehicles are often unavailable in many parts of sub-Saharan Africa due to their upkeep and fuelling expenses, and they are often utilised in other tasks [19, 133]. The model also assumes that all facilities have operational communications equipment with which to communicate referrals with [46, 134]. Consequently, women may experience delays in waiting for appropriate transport to refer them to EmOC locations. Similarly, the raster-based model assumes women can walk to their nearest maternal services; however, some women in labour may be incapable of movement [123] and thus reliant and delayed waiting for alternative modes of transport. For women that can walk, the model attempts to simulate impeded walking by parameterising travel speeds to be lower than average. However, a limitation is that these speeds remain static and there is no accounting for potential decreases in walking speeds due to exhaustion after walking long distances. In general, there is a complexity of variables affecting an individual’s walking speeds [135, 136], including factors such as the weather and time of day, but these were not modelled herein. As a result, in both the vector- and raster-based model, these assumptions and resulting limitations mean that the travel times modelled are best-case-scenario, optimal travel times.
Another limitation of the raster-based model was that it assumed women solely walk to maternal services. In the Barotse Floodplain, this unimodular representation of access doesn’t account for journeys often using oxen-carts or dugout canoes for parts of journeys in combination with walking. Insufficient data were available to adequately characterise and conceptualise this real-world transport behaviour into a model. Oxen-carts have similar travel speeds to walking so the differences in travel times and thus uncertainty is assumed to be minimal. However, dugout canoes operationalise areas that would otherwise be completely inaccessible to walking, thus can facilitate access where land-based transport is unavailable. As a consequence, some populations may be modelled as inaccessible when they may otherwise still be able to access maternal services through the use of a canoe. In the Barotse Floodplain, dugout canoes are commonplace and used on canals, rivers, and on open, unvegetated floodwaters. There is a dearth of research incorporating boats as a mode of transport in access models [42,43,44,45] which prevented their incorporation into the raster-based access model. This study has emphasised the capability of health access models to simulate boats as a focus for ongoing and future research.
Conclusions
Annual floods are common in low-income countries with seasonal climates, but assessing the impact of these floods on women’s access to maternal health services has been hampered by the lack of models able to represent the spatio-temporal impacts of floods on access. The necessity of geographic health access models able to represent this important spatio-temporal barrier is becoming increasingly more important under climate change. This study created novel geospatial models that were able to account for the impacts of floods on women’s walking access to healthcare facilities, and driving times for inter-facility referrals. Floods were shown to evidently have a strong control over women’s access to maternal services, with access asynchronously varying depending on flood stage, the location of women, and the positions of maternal services. Modelling access in this way has positive implications for addressing existing health inequities by providing evidence to facilitate interventions designed to increase all-weather year-round access to maternal health services, and to reduce the disproportionate impacts of floods on the most vulnerable communities of women.
Availability of data and materials
Additional file 1: Table S6 provides a description and source of all data used in this study. The waterbodies shapefile and monthly rasters of floodwater depth and velocity are openly available from the University of Leeds Data Repository: https://doi.org/10.5518/1362. The roads dataset as used in this study (consisting of OpenStreetMap data fused with manually delineated data) are also openly available from the University of Leeds Data Repository: https://doi.org/10.5518/1362. OpenStreetMap is licensed under the Open Data Commons Open Database License (https://www.openstreetmap.org/copyright) and is freely-accessible to use. The HRSL population data for women of reproductive age are freely available from the Human Data Exchange: https://data.humdata.org/organization/facebook?q=high%20resolution%20population%20density&ext_page_size=100. Geolocation information on health facilities in Zambia are freely available from the Ministry of Health Master Facility List: https://mfl.moh.gov.zm/facility/index. Details of the services available in Zambian health facilities as of 2012 are available from the 2012 List of Health Facilities in Zambia report, as cited.
Abbreviations
- GIS:
-
Geographical information systems
- HF:
-
Healthcare facility
- EmOC:
-
Emergency obstetric care
- BEmOC:
-
Basic emergency obstetric care
- CEmOC:
-
Comprehensive emergency obstetric care
- ITCZ:
-
Inter-Tropical Convergence Zone
- HRSL:
-
High Resolution Settlement Layer
- 4WD:
-
Four-wheel drive vehicles
- MFL:
-
Zambia’s Master Facility List
- OSM:
-
OpenStreetMap
- GPS:
-
Global positioning system
- DEM:
-
Digital elevation model
- WARMA:
-
Water Resources Management Agency
- MWS:
-
Maternity waiting shelter
- D:
-
Floodwater depth
- V:
-
Floodwater velocity
References
Ruktanonchai CW, Ruktanonchai NW, Nove A, Lopes S, Pezzulo C, Bosco C, et al. Equality in maternal and newborn health: modelling geographic disparities in utilisation of care in five East African Countries. PLoS ONE. 2016;11(8):e0162006.
Gabrysch S, Cousens S, Cox J, Campbell OMR. The influence of distance and level of care on delivery place in Rural Zambia: a study of linked national data in a geographic information system. PLoS Med. 2011;8(1):e1000394.
Hanson C, Cox J, Mbaruku G, Manzi F, Gabrysch S, Schellenberg D, et al. Maternal mortality and distance to facility-based obstetric care in rural southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. The Lancet Global Health. 2015;3(7):e387–95.
Tegegne TK, Chojenta C, Loxton D, Smith R, Kibret KT. The impact of geographic access on institutional delivery care use in low and middle-income countries: systematic review and meta-analysis. PLoS ONE. 2018;13(8):e0203130.
Kenny A, Basu G, Ballard M, Griffiths T, Kentoffio K, Niyonzima JB, et al. Remoteness and maternal and child health service utilization in rural Liberia: a population–based survey. J Glob Health. 2015;5(2):020401.
Noor AM, Zurovac D, Hay SI, Ochola SA, Snow RW. Defining equity in physical access to clinical services using geographical information systems as part of malaria planning and monitoring in Kenya. Tropical Med Int Health. 2003;8(10):917–26.
Målqvist M, Sohel N, Do TT, Eriksson L, Persson L. Distance decay in delivery care utilisation associated with neonatal mortality. A case referent study in northern Vietnam. BMC Public Health. 2010;10(1):762.
Rekha RS, Wajid S, Radhakrishnan N, Mathew S. Accessibility analysis of health care facility using geospatial techniques. Transp Res Procedia. 2017;27:1163–70.
Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004;3(1):3.
Luo W, Qi Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place. 2009;15(4):1100–7.
Makanga PT, Schuurman N, Sacoor C, Boene HE, Vilanculo F, Vidler M, et al. Seasonal variation in geographical access to maternal health services in regions of southern Mozambique. Int J Health Geogr. 2017;16(1):1.
Ray N, Ebener S. AccessMod 3.0: computing geographic coverage and accessibility to health care services using anisotropic movement of patients. Int J Health Geogr. 2008;7(1):63.
Gething PW, Johnson FA, Frempong-Ainguah F, Nyarko P, Baschieri A, Aboagye P, et al. Geographical access to care at birth in Ghana: a barrier to safe motherhood. BMC Public Health. 2012;12(1):991.
Nesbitt RC, Gabrysch S, Laub A, Soremekun S, Manu A, Kirkwood BR, et al. Methods to measure potential spatial access to delivery care in low- and middle-income countries: a case study in rural Ghana. Int J Health Geogr. 2014;13(1):25.
Ihantamalala FA, Herbreteau V, Révillion C, Randriamihaja M, Commins J, Andréambeloson T, et al. Improving geographical accessibility modeling for operational use by local health actors. Int J Health Geogr. 2020;19(1):27.
Ngana FR, Karyawati AAINE. Scenario modelling as planning evidence to improve access to emergency obstetric care in eastern Indonesia. PLoS ONE. 2021;16(6):e0251869.
Blanford JI, Kumar S, Luo W, MacEachren AM. It’s a long, long walk: accessibility to hospitals, maternity and integrated health centers in Niger. Int J Health Geogr. 2012;11(1):24.
Makanga PT, Schuurman N, von Dadelszen P, Firoz T. A sco** review of geographic information systems in maternal health. Int J Gynecol Obstet. 2016;134(1):13–7.
Alemu SM, Tura AK, do Amaral GSG, Moughalian C, Weitkamp G, Stekelenburg J, et al. How applicable is geospatial analysis in maternal and neonatal health in Sub-Saharan Africa? A systematic review. J Glob Health. 2022;12:04066.
Stone B, Sambo J, Sawadogo-Lewis T, Roberton T. When it rains, it pours: detecting seasonal patterns in utilization of maternal healthcare in Mozambique using routine data. BMC Health Serv Res. 2020;20(1):950.
Espinet Alegre X, Stanton-Geddes Z, Aliyev S. Analyzing flooding impacts on rural access to hospitals and other critical services in rural Cambodia using geo-spatial information and network analysis. Rochester, NY: Social Science Research Network; 2020 [cited 2021]. Report No.: ID 3614143. https://papers.ssrn.com/abstract=3614143.
Schatz JJ. Floods hamper health-care delivery in southern Africa. Lancet. 2008;371(9615):799–800.
Schoeps A, Gabrysch S, Niamba L, Sié A, Becher H. The effect of distance to health-care facilities on childhood mortality in Rural Burkina Faso. Am J Epidemiol. 2011;173(5):492–8.
Phalkey R, Dash S, Mukhopadhyay A, Runge-Ranzinger S, Marx M. Prepared to react? Assessing the functional capacity of the primary health care system in rural Orissa, India to respond to the devastating flood of September 2008. Global Health Action. 2012;5(1):10964.
Munthali AC, Swartz L, Mannan H, MacLachlan M, Chilimampunga C, Makupe C. "This one will delay us”: barriers to accessing health care services among persons with disabilities in Malawi. Disabil Rehabil. 2019;41(6):683–90.
Oppong JR. Accommodating the rainy season in Third World location-allocation applications. Socio-Economic Plann Sci. 1996;30(2):121–37.
Penfold S, Shamba D, Hanson C, Jaribu J, Manzi F, Marchant T, et al. Staff experiences of providing maternity services in rural southern Tanzania – a focus on equipment, drug and supply issues. BMC Health Serv Res. 2013;13(1):61.
Abdullah ASM, Dalal K, Halim A, Rahman AF, Biswas A. Effects of climate change and maternal morality: perspective from case studies in the rural area of Bangladesh. Int J Environ Res Public Health. 2019;16(23):4594.
Wilunda C, Scanagatta C, Putoto G, Takahashi R, Montalbetti F, Segafredo G, et al. Barriers to Institutional Childbirth in Rumbek North County, South Sudan: a qualitative study. PLoS ONE. 2016;11(12):e0168083.
Firoz T, Vidler M, Makanga PT, Boene H, Chiaú R, Sevene E, et al. Community perspectives on the determinants of maternal health in rural southern Mozambique: a qualitative study. Reprod Health. 2016;13(2):112.
Jammeh A, Sundby J, Vangen S. Barriers to emergency obstetric care services in perinatal deaths in rural Gambia: a qualitative in-depth interview study. ISRN Obstet Gynecol. 2011;2011:1–10.
Myers BA, Fisher RP, Nelson N, Belton S. Defining remoteness from health care: integrated research on accessing emergency maternal care in Indonesia. AIMS Public Health. 2015;2(3):257–73.
Hierink F, Rodrigues N, Muñiz M, Panciera R, Ray N. Modelling geographical accessibility to support disaster response and rehabilitation of a healthcare system: an impact analysis of Cyclones Idai and Kenneth in Mozambique. BMJ Open. 2020;10(11):e039138.
Cai X, Haile AT, Magidi J, Mapedza E, Nhamo L. Living with floods – Household perception and satellite observations in the Barotse Floodplain. Zambia Phys Chem Earth Parts A/B/C. 2017;100:278–86.
Beilfuss R. A Risky Climate for Southern African Hydro: assessing hydrological risks and consequences for Zambezi River Basin Dams. Berkeley: International Rivers; 2012.
Zimba H, Kawawa B, Chabala A, Phiri W, Selsam P, Meinhardt M, et al. Assessment of trends in inundation extent in the Barotse Floodplain, upper Zambezi River Basin: a remote sensing-based approach. J Hydrology: Reg Stud. 2018;15:149–70.
Facebook Connectivity Lab and Center for International Earth Science Information - CIESIN - Columbia University. High Resolution Settlement Layer (HRSL). Source imagery for HRSL © 2016 DigitalGlobe. 2016. https://www.ciesin.columbia.edu/data/hrsl/. Accessed 30 Aug 2021.
BRLi. and NIRAS. Detailed assessment, conceptual design and Environmental and Social Impact Assessment (ESIA) study for the improved use of priority traditional canals in the Barotse sub-basin of the Zambezi. Zambia: BRLi and NIRAS. 2014.
Chikozho C, Mapedza E. In search of socio-ecological resilience and adaptive capacity: articulating the governance imperatives for improved canal management on the Barotse Floodplain, Zambia. Int J Commons. 2017;11(1):119–43.
Flint L. Contradictions and Challenges in representing the past: the Kuomboka Festival of Western Zambia. J South Afr Stud. 2006;32(4):701–17.
Rajaratnam S, Cole SM, Fox KM, Dierksmeier B, Puskur R, Zulu F et al. Social and gender analysis report: Barotse Floodplain, Western Province, Zambia. Program Report: AAS-2015-18. Penang, Malaysia: CGIAR Research Program on Aquatic Agricultural Systems; 2015.
Makkonen T, Salonen M, Kajander S. Island accessibility challenges: rural transport in the Finnish archipelago. Eur J Transp Infrastructure Res. 2013. https://doi.org/10.18757/ejtir.2013.13.4.3005.
Webster K, Arroyo-Mora JP, Coomes OT, Takasaki Y, Abizaid C. A cost path and network analysis methodology to calculate distances along a complex river network in the Peruvian Amazon. Appl Geogr. 2016;73:13–25.
Tenkanen H, Salonen M, Lattu M, Toivonen T. Seasonal fluctuation of riverine navigation and accessibility in western Amazonia: an analysis combining a cost-efficient GPS-based observation system and interviews. Appl Geogr. 2015;63:273–82.
Salonen M, Toivonen T, Cohalan JM, Coomes OT. Critical distances: comparing measures of spatial accessibility in the riverine landscapes of Peruvian Amazonia. Appl Geogr. 2012;32(2):501–13.
Ebener S, Stenberg K, Brun M, Monet JP, Ray N, Sobel HL, et al. Proposing standardised geographical indicators of physical access to emergency obstetric and newborn care in low-income and middle-income countries. BMJ Global Health. 2019;4(Suppl 5):e000778.
Kyei-Nimakoh M, Carolan-Olah M, McCann TV. Access barriers to obstetric care at health facilities in Sub-Saharan Africa—a systematic review. Syst Rev. 2017;6(1):110.
Mao L, Nekorchuk D. Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place. 2013;24:115–22.
Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Soc Sci Med. 2006;63(3):691–705.
Stentzel U, Bahr J, Fredrich D, Piegsa J, Hoffmann W, van den Berg N. Is there an association between spatial accessibility of outpatient care and utilization? Analysis of gynecological and general care. BMC Health Serv Res. 2018;18(1):322.
Deshpande SD. Punctureless rubber-tyred ox-cart for central India. Bioresour Technol. 1994;47(1):37–44.
Deshpande SD, Ojha TP. Development and evaluation of an improved ox-cart for Central India. J Terrramech. 1985;22(3):135–46.
Sieber N. Transporting the yield: appropriate transport for agricultural production and marketing in Sub-Saharan Africa. Transp Reviews. 1999;19(3):205–20.
Ministry of Community Development (MCD) and Ministry of Health (MoH). Roadmap for accelerating reduction of maternal, newborn and child mortality, 2013–2016. Zambia: Lusaka; 2013.
Singini D. A Synopsis of maternal deaths in Zambia based on Maternal Death Review data. [Masters Thesis], Zambia: University of Zambia. 2015.
Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;20:1091.
Ministry of Health (MoH). The 2012 List of Health Facilities in Zambia. Preliminary report (version no. 15). Ministry of Health: Lusaka, Zambia; 2012.
Tembo T, Chongwe G, Vwalika B, Sitali L. Signal functions for emergency obstetric care as an intervention for reducing maternal mortality: a survey of public and private health facilities in Lusaka District, Zambia. BMC Pregnancy Childbirth. 2017;17(1):288.
OpenStreetMap contributors (OSM). OpenStreetMap. 2021. https://www.openstreetmap.org/.
Willis TDM, Smith MW, Cross DE, Hardy AJ, Ettrich GE, Malawo H, et al. Hydrodynamic modeling of inundation patterns of a large African floodplain indicates sensitivity to waterway restoration. Water Resour Res. 2022;58(11):e2021WR030107.
Bates PD, De Roo APJ. A simple raster-based model for flood inundation simulation. J Hydrol. 2000;236(1):54–77.
River Flows | Zambezi River Authority. https://www.zambezira.org/hydrology/river-flows. Accessed 06 Jun 2023.
Wessel B, Huber M, Wohlfart C, Marschalk U, Kosmann D, Roth A. Accuracy assessment of the global TanDEM-X Digital Elevation Model with GPS data. ISPRS J Photogrammetry Remote Sens. 2018;139:171–82.
Hardy A, Oakes G, Ettritch G. Tropical Wetland (TropWet) map** tool: the automatic detection of open and vegetated waterbodies in Google Earth Engine for tropical wetlands. Remote Sens. 2020;12(7):1182.
Safe Software. FME 2020.2 – try out features of the newest version. Globema: November 3 2020. https://www.globema.com/fme-2020-2/. Accessed 06 Jun 2023.
Safe Software. FME Desktop: Universal data integration tool. Globema. https://fme.globema.com/fme-desktop/. Accessed 06 Jun 2023.
Delamater PL, Messina JP, Shortridge AM, Grady SC. Measuring geographic access to health care: raster and network-based methods. Int J Health Geogr. 2012;11(1):15.
Campbell OMR, Aquino EML, Vwalika B, Gabrysch S. Signal functions for measuring the ability of health facilities to provide abortion services: an illustrative analysis using a health facility census in Zambia. BMC Pregnancy Childbirth. 2016;16(1):105.
Gabrysch S, Simushi V, Campbell OMR. Availability and distribution of, and geographic access to emergency obstetric care in Zambia. Int J Gynecol Obstet. 2011;114(2):174–9.
Huerta Munoz U, Källestål C. Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int J Health Geogr. 2012;11(1):40.
Ouma P, Macharia PM, Okiro E, Alegana V. Methods of measuring spatial accessibility to health care in Uganda. In: Makanga PT, editor. Practicing health geography: the African context. Cham: Springer International Publishing; 2021. p. 77–90.
r.cost -. GRASS GIS manual. https://grass.osgeo.org/grass82/manuals/r.cost.html. Accessed 25 May 2023
Heywood DI, Cornelius SC, Carver SJ. Data analysis. In: An Introduction to Geographical Information Systems. 4th ed. London: Pearson Prentice Hall; 2011. p. 174–225.
Tomlin D. Propagating radial waves of travel cost in a grid. Int J Geogr Inf Sci. 2010;24(9):1391–413.
Medrano FA. Effects of raster terrain representation on GIS shortest path analysis. PLoS ONE. 2021;16(4):e0250106.
Huber DL, Church RL. Transmission corridor location modeling. J Transp Eng. 1985;111(2):114–30.
Goodchild MF. An evaluation of lattice solutions to the problem of corridor location. Environ Plan A. 1977;9(7):727–38.
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet. 2015;386(9993):569–624.
Rudolfson N, Gruendl M, Nkurunziza T, Kateera F, Sonderman K, Nihiwacu E et al. Validating the Global Surgery Geographical Accessibility Indicator: Differences in Modeled Versus Patient-Reported Travel Times. World Journal of Surgery. 2020. https://doi.org/10.1007/s00268-020-05480-8.
World Health Organisation (WHO). Monitoring emergency obstetric care: a handbook. 2009. https://apps.who.int/iris/bitstream/handle/10665/44121/9789241547734_eng.pdf. Accessed 06 Jun 2023.
Ameyaw EK, Njue C, Tran NT, Dawson A. Quality and women’s satisfaction with maternal referral practices in Sub-Saharan African low and lower-middle income countries: a systematic review. BMC Pregnancy Childbirth. 2020;20(1):682.
Benson AE, Benson MJ, Luke AH. Assessment of maternal referral systems used for a rural Zambian hospital: the development of setting specific protocols for the identification of complications. Afr Health Sci. 2019;19(1):1536–43.
Ministry of Health (MoH). Zambia National Maternal and Neonatal Services Referral Guidelines. 2018. https://www.moh.gov.zm/?wpfb_dl=6. Accessed 06 Jun 2023.
Vwalika B, Stoner MCD, Mwanahamuntu M, Liu KC, Kaunda E, Tshuma GG, et al. Maternal and newborn outcomes at a tertiary care hospital in Lusaka, Zambia, 2008–2012. Int J Gynecol Obstet. 2017;136(2):180–7.
Schmitz MM, Serbanescu F, Arnott GE, Dynes M, Chaote P, Msuya AA, et al. Referral transit time between sending and first-line receiving health facilities: a geographical analysis in Tanzania. BMJ Global Health. 2019;4(Suppl 5):e001568.
Bailey PE, Keyes EB, Parker C, Abdullah M, Kebede H, Freedman L. Using a GIS to model interventions to strengthen the emergency referral system for maternal and newborn health in Ethiopia. Int J Gynecol Obstet. 2011;115(3):300–9.
Statutory Instrument No 007. of 2020 The Road Traffic Act (Speed Limits Regulation).pdf. eNotices. 2020. https://www.enotices.co.zm/download/statutory-instrument-no-07-of-2020-the-road-traffic-act-speed-limits-regulation-pdf/. Accessed 06 Jun 2023.
Mens M. Frameworks for flood event management. FLOODsite report T19-07-03. HR Wallingford: UK. 2008. https://repository.tudelft.nl/islandora/object/uuid%3A0aba18f1-9ac2-41 cc-abea-b1c0befb559d. Accessed 06 Jun 2023.
Teo FY, Liew Y, Falconer R, Lin B. Estimation of flood hazard risk relating to vehicles. Chengdu, China.: Proceedings of 2013 IAHR World Congress; 2013.
Teo FY, **a J, Falconer RA, Lin B. Experimental studies on the interaction between vehicles and floodplain flows. Int J River Basin Manage. 2012;10(2):149–60.
**a J, Falconer RA, **ao X, Wang Y. Criterion of vehicle stability in floodwaters based on theoretical and experimental studies. Nat Hazards. 2014;12:1619.
Martínez-Gomariz E, Gómez M, Russo B. Experimental study of the stability of pedestrians exposed to urban pluvial flooding. Nat Hazards. 2016;82(2):1259–78.
Shand TD, Cox RJ, Blacka MJ, Smith GP. Appropriate Safety Criteria for Vehicles (Report Number: P10/S1/006) australian rainfall and runoff. Water Res Lab. 2010.
Martínez-Gomariz E, Gómez M, Russo B, Djordjević S. Stability criteria for flooded vehicles: a state-of-the-art review. J Flood Risk Manag. 2018;11(S2):817–26.
Dijkstra EW. (Edsger). A note on two problems in connexion with graphs: (Numerische Mathematik, 1(1959), p 269–271). Stichting Mathematisch Centrum. 1959. https://ir.cwi.nl/pub/9256.
Wigley AS, Tejedor-Garavito N, Alegana V, Carioli A, Ruktanonchai CW, Pezzulo C, et al. Measuring the availability and geographical accessibility of maternal health services across Sub-Saharan Africa. BMC Med. 2020;18(1):237.
Anto-Ocrah M, Cushman J, Sanders M, De Ver Dye T. A woman’s worth: an access framework for integrating emergency medicine with maternal health to reduce the burden of maternal mortality in Sub-Saharan Africa. BMC Emerg Med. 2020;20(1):3.
Lerner EB, Moscati RM. The Golden Hour: scientific fact or medical “Urban Legend”? Acad Emerg Med. 2001;8(7):758–60.
Pyatkova K, Chen AS, Butler D, Vo**ović Z, Djordjević S. Assessing the knock-on effects of flooding on road transportation. J Environ Manage. 2019;244:48–60.
Kramer M, Terheiden K, Wieprecht S. Safety criteria for the trafficability of inundated roads in urban floodings. Int J Disaster Risk Reduct. 2016;17:77–84.
Yin J, Yu D, Lin N, Wilby RL. Evaluating the cascading impacts of sea level rise and coastal flooding on emergency response spatial accessibility in Lower Manhattan, New York City. J Hydrol. 2017;555:648–58.
Coles D, Yu D, Wilby RL, Green D, Herring Z. Beyond ‘flood hotspots’: modelling emergency service accessibility during flooding in York, UK. J Hydrol. 2017;546:419–36.
Green D, Yu D, Pattison I, Wilby R, Bosher L, Patel R, et al. City-scale accessibility of emergency responders operating during flood events. Nat Hazards Earth Syst Sci. 2017;17(1):1–16.
Yin J, Yu D, Yin Z, Liu M, He Q. Evaluating the impact and risk of pluvial flash flood on intra-urban road network: a case study in the city center of Shanghai, China. J Hydrol. 2016;537:138–45.
Yu D, Yin J, Wilby RL, Lane SN, Aerts JCJH, Lin N, et al. Disruption of emergency response to vulnerable populations during floods. Nat Sustain. 2020;3(9):728–36.
Karvonen RA, Hepojoki A, Huhta HK, Louhio A. The use of physical models in dam-break analysis. Helsinki, Finland: RESCDAM Final Report Helsinki University of Technology; 2000.
Témez Pelaez JR. Control del desarrollo urbano en las zonas inundables. In: Dolz J, Gómez M, editors. `Inundaciones y redes de drenaje Urbano’. Madrid, España: CICCP Monografías; 1992.
Abt SR, Wittier RJ, Taylor A, Love DJ. Human stability in a high flood hazard zone. JAWRA J Am Water Resour Assoc. 1989;25(4):881–90.
Quirogaa VM, Kurea S, Udoa K, Manoa A. Application of 2D numerical simulation for the analysis of the February 2014 bolivian Amazonia flood: application of the new HEC-RAS version 5. Ribagua. 2016;3(1):25–33.
**a J, Falconer RA, Wang Y, **ao X. New criterion for the stability of a human body in floodwaters. J Hydraul Res. 2014;52(1):93–104.
Jonkman SN, Penning-Rowsell E. Human instability in flood flows. JAWRA J Am Water Resour Assoc. 2008;44(5):1208–18.
Bernhofen MV, Whyman C, Trigg MA, Sleigh PA, Smith AM, Sampson CC, et al. A first collective validation of global fluvial flood models for major floods in Nigeria and Mozambique. Environ Res Lett. 2018;13(10):104007.
Nigro J, Slayback D, Policelli F, Brakenridge GR, NASA/. DFO MODIS Near Real-Time (NRT) Global Flood Map** Product Evaluation of Flood and Permanent Water Detection. 2022. https://www.earthdata.nasa.gov/learn/find-data/near-real-time/modis-nrt-global-flood-product. Accessed 06 Jun 2023.
Hardy A, Ettritch G, Cross DE, Bunting P, Liywalii F, Sakala J, et al. Automatic detection of open and vegetated water bodies using Sentinel 1 to map African malaria vector mosquito breeding habitats. Remote Sens. 2019;11(5):593.
Foroughnia F, Alfieri SM, Menenti M, Lindenbergh R. Evaluation of SAR and optical data for flood delineation using supervised and unsupervised classification. Remote Sens. 2022;14(15):3718.
Bangira T, Iannini L, Menenti M, van Niekerk A, Vekerdy Z. Flood extent map** in the caprivi floodplain using sentinel-1 time series. IEEE J Sel Top Appl Earth Observations Remote Sens. 2021;14:5667–83.
Martinis S, Twele A. A hierarchical spatio-temporal Markov model for improved flood map** using multi-temporal X-Band SAR data. Remote Sens. 2010;2(9):2240–58.
Kyei NNA, Campbell OMR, Gabrysch S. The influence of distance and level of service provision on antenatal care use in rural Zambia. PLoS ONE. 2012;7(10):e46475.
Tatem AJ, Campbell J, Guerra-Arias M, de Bernis L, Moran A, Matthews Z. Map** for maternal and newborn health: the distributions of women of childbearing age, pregnancies and births. Int J Health Geogr. 2014;13(1):2.
Wong KLM, Benova L, Campbell OMR. A look back on how far to walk: systematic review and meta-analysis of physical access to skilled care for childbirth in Sub-Saharan Africa. PLoS ONE. 2017;12(9):e0184432.
Simkhada B, van Teijlingen ER, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in develo** countries: systematic review of the literature. J Adv Nurs. 2008;61(3):244–60.
World Health Organization (WHO). Antenatal care coverage - at least four visits (%) Indicator Metadata Registry Details. 2022. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/80. Accessed 06 Jun 2023.
Gabrysch S, Campbell OM. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9(1):34.
Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med. 2007;65(8):1666–82.
Phiri SC, Prust ML, Chibawe CP, Misapa R, van den Broek JW, Wilmink N. An exploration of facilitators and challenges in the scale-up of a national, public sector community health worker cadre in Zambia: a qualitative study. Hum Resour Health. 2017;15(1):40.
Zambezi Valley Development Initiative (ZVDI). Lyambai Vulnerability and Adaptation Project Stage 2: community based adaptation to climate change (CBA), first field expedition, 20–31 October 2010: report (second draft). Zambia: ZVDI; 2010.
Río TD. Farming systems characterization in three communities from the Barotse floodplains, Zambia: Relating landscape with production and diversity. [Master's thesis]. Wageningen: Wageningen University. 2014;114.
Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–40.
Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18.
Nassoro MM, Chetto P, Chiwanga E, Lilungulu A, Bintabara D, Wambura J. Maternal mortality in Dodoma Regional Referral Hospital, Tanzania. Int J Reproductive Med. 2020;2020:e9082179.
Mupwanyiwa A, Chundu M, Mavesere I, Dengedza M. Exploring factors that influence the uptake of maternal Health Care Services by women in Zimbabwe. Open J Social Sci. 2020;8(10):46–70.
van den Boogaard J, Arntzen B, Chilwana J, Liyungu M, Mantingh A, Stekelenburg J. Skilled or traditional birth attendant? Choices of Communities in Lukulu District, Rural Zambia. whp. 2008;10(1):34–43.
Chen YN, Schmitz MM, Serbanescu F, Dynes MM, Maro G, Kramer MR. Geographic Access modeling of emergency obstetric and neonatal care in Kigoma Region, Tanzania: transportation schemes and programmatic implications. Global Health Sci Pract. 2017;5(3):430–45.
Speranza CI. Flood disaster risk management and humanitarian interventions in the Zambezi River Basin: implications for adaptation to climate change. Climate Dev. 2010;2(2):176–90.
Witt P. The Development of a Predictive Hiking Travel Time Model Accounting for Terrain Variations. In T Jekel, A Car, J Strobl, & G Griesebner, editors, GI_Forum 2012: Geovisualization, Society and Learning. 2012;11.
Bosina E, Weidmann U. Estimating pedestrian speed using aggregated literature data. Physica A. 2017;468:1–29.
Acknowledgements
Ewan McLaughlin is thanked for providing expert support on FME throughout the duration of this project. Chris Stringer is thanked for his technical assistance with creating figures. The Safe Software Team are greatly thanked for their provision of a free FME Desktop license. We also greatly thank the two anonymous reviewers who provided helpful comments.
Funding
This work was supported by the Leeds-York-Hull Natural Environmental Research Council (NERC) Doctoral Training Partnership (Panorama) under Grant NE/S007458/1.
Author information
Authors and Affiliations
Contributions
EM, MS, and TW were involved with conceptualisation and design of the project. TW provided the flood model data. EM digitised the roads data, constructed the GIS, and produced the data. MS and TW supervised the project and assisted with the interpretation of the results. EM wrote the manuscript with contributions and revisions from MS, TW, CT, MN, DS, and CJ. All authors read and approved of the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Reclassification of OpenStreetMap data. Table S2. Vehicular instability thresholds as recommended by the Australian Rainfall and Runoff Project [131]. Figure S1. Boxplot showing the variability in the monthly sum of precipitation as recorded between 1993-2010 for the Upper Zambezi catchment. Table S3. Monthly average depths, velocities, and waterbody and flood extent across the study area. Table S4. The number and percentage of women (total n = 8,130) who are inaccessible and who have timely walking access to maternal services each month. Table S5. The number and percentage of women (total n = 8,130) who are unable to be referred by road to EmOC and those who have timely vehicular referral access to EmOC each month. Table S6. Description and source of all data used in this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mroz, E.J., Willis, T., Thomas, C. et al. Impacts of seasonal flooding on geographical access to maternal healthcare in the Barotse Floodplain, Zambia. Int J Health Geogr 22, 17 (2023). https://doi.org/10.1186/s12942-023-00338-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12942-023-00338-3