Abstract
Background
Aztreonam-avibactam (ATM-AVI) combination shows promising effectiveness on most carbapenemase-producing Gram-negatives, yet standardized antibiotic susceptibility testing (AST) methods for evaluating the combination in clinical laboratories is lacking. We aimed to evaluate different ATM-AVI AST approaches.
Methods
96 characterized carbapenem-resistant clinical isolates belonging to 9 Enterobacterales (EB; n = 80) and P. aeruginosa (PA; n = 16) species, including 90 carbapenemase producers and 72 strains resistant to both CAZ-AVI and ATM, were tested. Paper disk elution (DE; Bio-Rad) and E-test gradient strips stacking (SS; bioMérieux) were performed for the ATM + CAZ-AVI combination. MIC Test Strip (MTS; Liofilchem) was evaluated for ATM-AVI MIC determination. Results were interpreted applying ATM clinical breakpoints of the EUCAST guidelines and compared to the broth microdilution method (Sensititre, Thermofisher).
Results
According to broth microdilution method, 93% of EB and 69% of PA were tested susceptible to ATM-AVI. The synergistic effect of ATM-AVI was of 95% for EB, but of only 17% for PA. The MTS method yielded higher categorical and essential agreement (CA/EA) rates for both EB (89%/91%) and PA (94%/94%) compared to SS, where the rates were 87%/83% for EB and 81%/81% for PA. MTS and SS yielded 2 and 3 major discrepancies, respectively, while 3 very major discrepancies each were observed for both methods. Concerning the DE method, CA reached 91% for EB and 81% for PA, but high number of very major discrepancies were observed for EB (n = 6; 8%) and for PA (n = 3; 19%).
Conclusions
The ATM-AVI association displayed excellent in vitro activity against highly resistant clinical Enterobacterales strains. MTS method offers accurate ATM-AVI AST results, while the SS method might serve as better alternative then DE method in assessing the efficacy of ATM + CAZ-AVI combination. However, further investigation is needed to confirm the methods' ability to detect ATM-AVI resistance.
Similar content being viewed by others
Introduction and objectives
Multidrug resistance (MDR) in Gram-negative rods represents a major public health issue and epidemiological data indicated a significant increase in the prevalence of carbapenem resistance in Europe and worldwide. Severe infections such as bacteremia caused by carbapenemase-producing organisms (CPO) are of major concern in clinical practice due to the limited therapeutic options available with negative impacting on the outcome of infected patients.
The development of new antimicrobial treatments includes the pairing of modern beta-lactamase inhibitors with traditional beta-lactam agents. Avibactam (AVI), combined with ceftazidime (CAZ) in pharmaceutical available therapy, demonstrates in-vitro and clinical efficacy against several Ambler class A (ESBLs, KPC), C (AmpC) and D (OXA-48) beta-lactamases including carbapenemases, but fails to exhibit efficacy against Enterobacterales that express class B metallo-beta-lactamases (MBL) such as NDM, VIM or IMP, that are capable of hydrolyzing carbapenems, often in conjunction with other β-lactams. On the other hand, aztreonam (ATM), a monobactam beta-lactam, has potent activity against MBLs, but the co-expression in MBL-producing Enterobacterales of other large spectrum aztreonam-hydrolyzing beta-lactamases like ESBLs and/or AmpC cephalosporinases has made the monotherapy use of ATM difficult.
Clinical trials of investigational antibiotic combination aztreonam-avibactam (ATM-AVI) showed promising results from two phase 3 studies [1, 2]. Meanwhile, the combination of ceftazidime-avibactam (CAZ-AVI) and ATM has demonstrated efficacy against MBL-producing Enterobacterales and Pseudomonas aeruginosa and could serve as a therapeutic option awaiting the potential approval and release of ATM-AVI for clinical use [3,4,5,6,7,8]. However, published literature mainly comprises limited clinical experiences through small case series [9].
The latest treatment guidelines issued by European Society of Clinical Microbiology and Infectious Diseases (ESCMID) conditionally recommend the combination of ATM and CAZ-AVI (ATM + CAZ-AVI) for the treatment of patients with severe infections caused by carbapenem-resistant Enterobacterales (CRE) harboring MBLs and/or showing resistance to all available antibiotics, especially when the strain is also cefiderocol-resistant [10]. However, a practical and standardized antibiotic susceptibility testing (AST) method for evaluating the efficacy of the ATM + CAZ-AVI combination in clinical laboratories is currently lacking.
This study aimed to assess the performance of various methods for the AST of the ATM + CAZ-AVI combination and of a commercial ATM-AVI gradient strip diffusion method using a collection from the Belgian National Reference Center for Antibiotic-Resistant Gram-Negative Bacilli (NRC) of CRE and MDR P. aeruginosa, including a majority of carbapenemase producers.
Materials and methods
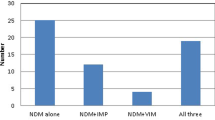
This study panel included 96 previously characterized non-duplicate carbapenem-resistant clinical isolates belonging to 9 Enterobacterales and 1 non-fermentative (P. aeruginosa) species which are summarized in Table 1. Phenotypically and/or genotypically defined resistance mechanisms to beta-lactams are detailed in Supplementary data S1. The study panel included 70 strains that were resistant to both CAZ-AVI and ATM, 8 strains that were sensitive to CAZ-AVI but resistant to ATM, and 18 strains that were resistant to CAZ-AVI but sensitive to ATM as determined by Sensititre broth microdilution (BMD) assays. Furthermore, this panel included 14 strains exhibiting resistance to cefiderocol by BMD. Such selection was intended to challenge the efficacy of the ATM + CAZ-AVI combination against a collection of MDR strains widely resistant to last-line molecules.
All 96 clinical strains were tested using freshly prepared overnight subcultures on 5% sheep blood trypti-soya agar plates. Species identification was carried out using matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) with MALDI Biotyper (Bruker, Germany). The evaluated AST methods (once per method per strain) included disk elution (DE), gradient diffusion strip stacking (SS), and MIC Test Strip aztreonam-avibactam (MTS; Liofilchem). Reference MIC and category results for ATM-AVI were defined by BMD using Sensititre (MIC range 0,03/4–64/4 μg/mL) (Thermo Fisher Scientific, Waltham, MA, USA). To ensure the reproducibility of the methods employed, three selected MBL-producing positive control strains underwent five repetitions of DE, SS, and MTS in conjunction with BMD for ATM-AVI. In case of an invalid result, the strain was retested with the same method.
Combination disk elution (DE) was performed using CAZ-AVI 10/4 µg disk and ATM 30 µg disk (Bio-Rad Hercules, CA, USA) as described previously [11]. Briefly, a 0,5 McFarland suspension was prepared and 12 µL of this suspension were inoculated onto three separate tubes containing 2 mL of Mueller–Hinton broth (Thermo Fisher Scientific, Waltham, MA, USA). Afterwards, one ATM disk was added to the first tube (theoretical concentration of ATM of 15 µg/mL), two CAZ-AVI disks were added to the second tube (concentration of CAZ-AVI of 10/4 µg/mL), one ATM and two CAZ-AVI disks were added to the third tube (concentration of ATM 15 µg/mL and CAZ-AVI 10/4 µg/mL). After 30-min incubation at room temperature, antibiotics disks were removed, then the tubes were vortexed and incubated for 24 h at 37 °C. The presence or absence of bacterial turbid growth were observed following the incubation by two readers. The effectiveness of the ATM + CAZ-AVI combination was determined by the absence of any visible growth in the tube containing both ATM and CAZ-AVI.
Gradient diffusion strip stacking (SS) method was accomplished by combining the use of E-test strips for CAZ-AVI (MIC range 0,016/4–256/4 μg/mL) and for ATM (MIC range 0,016–256 μg/mL) (bioMérieux, Marcy l’Etoile, France). In this approach, the E-test strip of CAZ-AVI was placed on the agar surface for 10 min. Subsequently, the CAZ-AVI E-test strip was removed, and an ATM E-test strip was positioned at the same spot. After an incubation of 18 h, the MIC was read [11].
MIC Test Strip aztreonam-avibactam (MIC range 0,016/4–256/4 μg/mL) (MTS™, Liofilchem®) was performed according to manufacturers’ instructions and evaluated for the determination of ATM-AVI MIC.
Recorded raw results were interpreted according to the EUCAST 2023 clinical breakpoints, applying the established ATM criteria to assess the ATM-AVI combination as previously performed in other studies (Table 2) [12,13,14].
The MIC and category results obtained by different methods were compared to the BMD results. Categorical agreement (CA: agreement of category results), essential agreement (EA: MICs within ± 1 dilution of reference MICs, adapted to the range of the tested dilutions by excluding all extreme values of ≤ X and > Y mg/L), very major discrepancy (VMD: false drug-sensitive result), major discrepancy (MD: false drug-resistant result) and minor discrepancy (minD: susceptible by the evaluated routine method versus susceptible at high dose by the reference method or vice-versa) rates were calculated for each method compared to the reference BMD. All methods were evaluated according to the ISO Standard 20776-2 criteria (EA and CA > 90%, VMD < 3%). Regarding the MIC-based methods, activity synergy was defined as a reduction of at least 3 dilutions in the MIC comparing the lowest MIC obtained for either CAZ-AVI or ATM, with MIC of the combination (ATM-AVI). For DE method, synergy was defined as the total growth inhibition when CAZ-AVI and ATM were combined, specifically for strains resistant to CAZ-AVI and ATM separately (CAZ-AVI R, ATM R).
Results
Reproducibility
Five results per strain were obtained for reproducibility testing per method. Reproducibility was perfect for all methods (100%) for E. coli and K. pneumoniae isolates. Regarding P. aeruginosa strain, reproducibility reached 100% except for DE method and SS method which were only 80%. (Supplementary data Table 2).
Method comparison on clinical collection strains
Out of 80 Enterobacterales strains tested with ATM-AVI BMD, 66 (82,5%) were susceptible, 8 (10,0%) were susceptible at increased exposure and 6 (7,5%) were resistant to the combination. ATM-AVI resistant strains were 4 E. coli (one producing NDM-4 with CTX-M-15 and CMY-6, one NDM-7 with CTX-M-15, one NDM-1 with PER-3, CMY-6 and DHA-1, and one NDM-5 with CMY-42) showing MIC range of 8 to 16 mg/L and 2 S. marcescens (one OXA-427 and one non-carbapenemase hyperproducing cephalosporinase) having both a MIC of 16 mg/L. Among the 66 Enterobacterales strains resistant to both CAZ-AVI and ATM separately, 93% (n = 62/66) exhibited restored susceptibility with ATM-AVI.
Out of 16 P. aeruginosa strains tested with ATM-AVI BMD, 11 (68,7%) were considered susceptible (MIC of 8–16 mg/L) and 5 (31,3%) were resistant (MIC of 64 mg/L) to the combination using the EUCAST ATM clinical resistance breakpoint of > 16 mg/L. ATM-AVI resistant strains were 3 non-carbapenemase strains, one VIM-2 producer and one strain co-producing NDM-1 and VIM-5. Among P. aerguinosa strains resistant to CAZ-AVI and to ATM separately, 58% (n = 7/12) had susceptibility restored with ATM-AVI.
The synergistic activity (defined as threefold MIC reduction) with the ATM-AVI combination was observed for 87,5% (n = 70/80) of Enterobacterales (including 95% (n = 63/66) that were resistant to both CAZ-AVI and ATM) and only 12,5% (n = 2/16) of P. aeruginosa strains (representing one-third of the MBL producers).
MIC-based methods
A total of 96 organism-drug results per method were obtained to calculate categorization performance (CA, VMD, MD, minD) for MTS, and SS methods. No invalid results were observed by any of the testing methods. Due to truncations in the concentration range of the evaluated method and/or of the reference method, the numbers of evaluable organism-drug results were lower for the calculation of EA (87 for MTS and SS methods). All agreement and discrepancy rates for MIC based methods are detailed in Table 3.
The MTS method demonstrated higher CA and EA for both Enterobacterales (88,8% and 90,9%) and P. aeruginosa (93,8% and 93,8%) than SS method (Enterobacterales 87,5% and 83,1%, P. aeruginosa 81,3% and 88,9%)). This method resulted in 3,7% VMD, 1,3% MD, and 6,2% minD for Enterobacterales and 0% VMD and 6,2% MD for P. aeruginosa. E. coli species displayed higher rate of VMD, MD and minD among Enterobacterales with 15,8%, 5,3% and 10,5% respectively. All other subspecies have a higher CA and EA for MTS than for SS method. Overall, the MTS method yielded 2 MD and 3 VMD. All VMD came from E. coli ATM-AVI resistant strains (one NDM-4, CTX-M-15, CMY-6, one NDM-7, CTX-M-15 and one NDM-5 CMY-42 strains) while the 2 MD came from 1 E. coli strain (one NDM-5, TEM-187 and CMY-42 strain) and 1 P. aerguinosa (GES-5).
Regarding the SS method, we observed a CA and an EA of 87,5% and 83,1% respectively for Enterobacterales and 81,3% and 81,3% for P. aeruginosa. 1,2% of VMD, 2,5% of MD and 8,8% of minD were found for Enterobacterales. E. coli showed the highest rate of minD with 15,8%. No VMD or MD were found for other Enterobacterales. Regarding P. aeruginosa, 12,5% of VMD and 6,3% of MD were found. Overall, the SS method yielded 3 MD and 3 VMD. Similarly to the MTS method, 1 VMD came from one NDM-7-producing E. coli strain while the two other VMD came from 2 strains of non-carbapenemase P. aeruginosa. The 3 MD came from a MBL (IMP-1, VEB-1)-producing P. aeruginosa and from 2 NDM-producing E. coli (1 NDM-5 TEM-187 and CMY-42 strain and 1 NDM-5 and CMY-42 strain).
MIC of ATM-AVI using MTS and SS compared with BMD are shown in Table 4. For Enterobacterales, MIC values obtained with the SS method tend to be higher when compared to the BMD (bias + 55%) while the MTS method tends to yield MIC values that are lower in comparison to the BMD (bias − 18,8%). When examining P. aeruginosa, MIC values obtained from both the SS and MTS methods tend to be lower when compared to those obtained through BMD (bias: − 37,5% for both methods).
Disk elution method
Of the 96 results obtained with the DE method, CA reached 91% for Enterobacterales and 81% for P. aeruginosa, but a high number of VMD were observed for EB (n = 6; 8%) and for P. aeruginosa (n = 3; 19%) compared to other methods.
Discussion
Carbapenem-resistant Enterobacterales (CRE), and particularly carbapenemase-producing Enterobacterales (CPE) are increasing worldwide and threaten the global public health. In Belgium, class B carbapenemases are produced currently by 40% of CPE strains with a significant increase in NDM-type CPE (from 11% in 2017 to 28% in 2022), which has become the second most prevalent carbapenemase after OXA-48 according to the National Reference Center for Antibiotic-Resistant Gram-Negative Bacilli [15].
The combined administration of ATM and CAZ-AVI has been used in various infections caused by MBL-producing Enterobacterales, including bloodstream, urinary, pulmonary, and joint infections [3, 16, 17]. ATM + CAZ-AVI proved to be the most effective among combinations against MBL-producing Enterobacterales [18] achieving a clinical resolution rate of 80% in infected patients according to a systematic review [13]. ATM + CAZ-AVI could serve as an interesting alternative strategy, awaiting the availability of ATM-AVI combination, in treating infections by MBL-producing Enterobacterales or strains that are resistant to cefiderocol or other last-line molecules. Data are more controversial regarding the efficacy of the combination against MBL-producing P. aeruginosa [19, 20].
Our study panel included 96 (100%) carbapenem resistant strains and 14 (15%) cefiderocol-resistant strains. 11 (11,4%) of those strains were resistant to the combination of ATM-AVI including 4 E. coli (all NDM producers), 2 S. marcescens (1 OXA-427 and 1 non carbapenemase) and 5 P. aeruginosa strains (3 non carbapenemase and 2 MBL). Our data of ATM-AVI resistance detected in E. coli isolates are in line with the literature describing similar observations of ATM-AVI resistance mainly in E. coli due to specific mechanisms involved such as PBP3 protein insertions (e.g., YRIN or YRIK) or CMY-42 β-lactamase (produced by two E. coli strains in our study) [21]. These ATM-AVI resistant strains, not often available and tested in other studies, allowed us to challenge evaluated methods. However, the small number of ATM-AVI-resistant strains (n = 6 in Enterobacterales; n = 5 in P. aerguinosa), prevents correctly assessing the ability of the tested methods in detecting such strains. Additionally, the absence of K. pneumoniae or E. cloacae ATM-AVI resistant strains hinders the assessment of the methods' performance in detecting such strains. This limitation was unbiased and reflected current epidemiological situation as depicted by one Belgian study showing no ATM-AVI resistance among Enterobacterales and one French study with few ATM-AVI resistant strains tested [14, 22]. Continuous surveillance should monitor potential significant emergence of ATM-AVI resistant strains.
The primary goal of this study was to evaluate the effects of the ATM-AVI combination and the accuracy of the different testing methods for ATM-AVI. Our results demonstrate that MIC values yielded by MTS method closely aligned with those obtained with BMD (EA > 90%). Other studies have also indicated the reliability of the MTS method [14, 22, 23]. Additionally, MTS method offers a technical convenience compared to the SS and DE methods. However, we highlighted a significant concern regarding the method's capability to detect ATM-AVI resistance, as only 1 out of 4 E. coli strain was accurately categorized as ATM-AVI-resistant. Moreover, we cannot assess the reliability of these methods for the detection of ATM-AVI resistance among K. pneumoniae and other Enterobacterales species given the lack of those strains in this study.
The SS method yielded fewer VMD than the MTS method for Enterobacterales but yielded more MD and minD. The complexity of the SS method, which involves manual operations to remove and replace from the agar plate the pre-incubated CAZ-AVI E-test strip by the ATM strip, may leads to inappropriate diffusion of avibactam in the agar plate or to bacterial contamination. Obviously, the SS method increases workload and costs compared to MTS ATM-AVI. Hence, if available, the MTS test would be the preferred choice for determining ATM-AVI MIC.
The DE method was first described by Khan et al. highlighting its affordability and accessibility in low-resource settings for screening rapidly the synergy between AVI and ATM [11]. In our study for Enterobacterales, DE method was reproducible and reached a good CA (90%), but high VMD (8%) was observed. It could therefore serve as a cheap alternative tool to test for synergy, although should be used with caution due to the risk of missing ATM-AZI resistance. However, this method is not appropriate for P. aeruginosa given the high rate of VMD (19%) and its low reproducibility (80%). We have not been able to provide explanations for the lower reproducibility observed for P. aeruginosa with the DE, as well as for the SS method. Ultimately, DE method has the drawback of not providing a MIC value, which may be important to guide clinical treatment against these difficult-to-treat resistant microorganisms.
Our study also examined whether the two molecules exhibited synergistic effects when combined and if a reduction in MIC values (≥ threefold) was observed compared to individual components. Enterobacterales showed an excellent activity recovery of 95% when exposed to the ATM-AVI combination. Our data are in line with other studies where all MBL-producing Enterobacterales were susceptible to the combination [22, 24, 25] underscoring the importance of considering this combination as empirical therapy for infections caused by these microorganisms. However, it had a limited activity against P. aeruginosa, as our result showed only 17% synergy. This observation supported by other studies is likely due to the coexistence of additional non-carbapenemase resistance mechanisms in P. aeruginosa [11, 22]. Therefore, the combination of ATM-AVI has very limited usefulness for the treatment of multidrug-resistant P. aeruginosa strains.
The strength of our study is that we used a collection of well-characterized and highly resistant clinical strains including the presence of a few, but yet significant number of ATM-AVI resistant strains, challenging the evaluated testing methods. This study has several limitations given its single-center design with a limited number of isolates (n = 96). Then, the absence of well-defined ATCC reference strains hinders the evaluation of result reproducibility. Finally, we believe the methods should be tested with more strains that exhibit ATM-AVI resistance to better evaluate the performance of resistance detection with the evolving epidemiology.
Conclusion
The ATM-AVI association displayed excellent in vitro synergistic activity against extensively multidrug-resistant clinical Enterobacterales isolates in Belgium. Our data suggest that MTS method offers accurate ATM-AVI AST results on Enterobacterales strains, while the SS method might serve as better alternative then DE method in assessing the efficacy of ATM-AVI combination. Further investigation should ascertain methods’ ability to detect ATM-AVI resistance in Enterobacterales.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Efficacy, Safety, and Tolerability of ATM-AVI in the Treatment of Serious Infection Due to MBL-producing Gram-negative Bacteria. ClinicalTrials.gov ID NCT03580044.
A Study to Determine the Efficacy, Safety and Tolerability of Aztreonam-Avibactam (ATM-AVI) ± Metronidazole (MTZ) Versus Meropenem (MER) ± Colistin (COL) for the Treatment of Serious Infections Due to Gram Negative Bacteria. (REVISIT). ClinicalTrials.gov ID NCT03329092.
Falcone M, et al. Efficacy of ceftazidime-avibactam plus Aztreonam in patients with bloodstream infections caused by metallo-beta-lactamase-producing Enterobacterales. Clin Infect Dis. 2021;72(11):1871–8.
Marshall S, et al. Can ceftazidime-avibactam and aztreonam overcome beta-lactam resistance conferred by metallo-beta-lactamases in Enterobacteriaceae? Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.02243-16.
Bhatnagar A, et al. Aztreonam-avibactam susceptibility testing program for metallo-beta-lactamase-producing Enterobacterales in the antibiotic resistance laboratory network, march 2019 to December 2020. Antimicrob Agents Chemother. 2021;65(8):e0048621.
Lu G, et al. In vitro and in vivo antimicrobial activities of ceftazidime/avibactam alone or in combination with Aztreonam against carbapenem-resistant Enterobacterales. Infect Drug Resist. 2022;15:7107–16.
Sreenivasan P, et al. In-vitro susceptibility testing methods for the combination of ceftazidime-avibactam with aztreonam in metallobeta-lactamase producing organisms: role of combination drugs in antibiotic resistance era. J Antibiot. 2022;75(8):454–62.
Biagi M, et al. Searching for the optimal treatment for metallo- and serine-beta-lactamase producing Enterobacteriaceae: aztreonam in combination with ceftazidime-avibactam or meropenem-vaborbactam. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.01426-19.
Aslan AT, et al. In vitro, in vivo and clinical studies comparing the efficacy of ceftazidime-avibactam monotherapy with ceftazidime-avibactam-containing combination regimens against carbapenem-resistant Enterobacterales and multidrug-resistant Pseudomonas aeruginosa isolates or infections: a sco** review. Front Med. 2023. https://doi.org/10.3389/fmed.2023.1249030.
Paul M, et al. European society of clinical microbiology and infectious diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin Microbiol Infect. 2022;28(4):521–47.
Khan A, et al. Evaluation of susceptibility testing methods for aztreonam and ceftazidime-avibactam combination therapy on extensively drug-resistant gram-negative organisms. Antimicrob Agents Chemother. 2021;65(11):e0084621.
The European Committee on Antimicrobial Susceptibility Testing, Breakpoint tables for interpretation of MICs and zone diameters. Version 13.1. 2023. http://www.eucast.org.
Mauri C, et al. The revival of aztreonam in combination with avibactam against metallo-beta-lactamase-producing gram-negatives: a systematic review of in vitro studies and clinical cases. Antibiotics. 2021. https://doi.org/10.3390/antibiotics10081012.
Cardot ME. et al. Evaluation of the MTS aztreonam-avibactam strip (Liofilchem) on New Delhi metallo-beta-lactamase-producing Enterobacterales. Eur J Clin Microbiol Infect Dis. 2024. https://doi.org/10.1007/s10096-024-04766-2
Huang T-D, Montesinos I, Evrard S, Berhin C, Bouchahrouf W, Hoebeke M, Wallemme I, Denis O. Microbiological surveillance of carbapenemase-producing Enterobacterales (CPE) in Belgium. Basel: ECCMID; 2023.
Merad Y, et al. Case report: continuous infusions of ceftazidime-avibactam and aztreonam in combination through elastomeric infusors for 12 weeks for the treatment of bone and joint infections due to metallo-beta-lactamase producing Enterobacterales. Front Med. 2023;10:1224922.
Larcher R, et al. Last resort beta-lactam antibiotics for treatment of New-Delhi metallo-beta-lactamase producing Enterobacterales and other difficult-to-treat resistance in gram-negative bacteria: a real-life study. Front Cell Infect Microbiol. 2022;12:1048633.
Emeraud C, et al. Aztreonam plus clavulanate, tazobactam, or avibactam for treatment of infections caused by metallo-beta-lactamase-producing gram-negative bacteria. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.00010-19.
Lee M, Abbey T, Biagi M, Wenzler E. Activity of aztreonam in combination with ceftazidime-avibactam against serine- and metallo-beta-lactamase-producing Pseudomonas aeruginosa. Diagn Microbiol Infect Dis. 2021;99(1):115227.
Karlowsky JA, et al. In Vitro activity of aztreonam-avibactam against Enterobacteriaceae and pseudomonas aeruginosa isolated by clinical laboratories in 40 countries from 2012 to 2015. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/AAC.00472-17.
Sadek M, Juhas M, Poirel L, Nordmann P. Genetic features leading to reduced susceptibility to aztreonam-avibactam among metallo-beta-lactamase-producing escherichia coli isolates. Antimicrob Agents Chemother. 2020. https://doi.org/10.1128/AAC.01659-20.
Verschelden G, et al. Aztreonam-avibactam synergy, a validation and comparison of diagnostic tools. Front Microbiol. 2023;14:1322180.
Deschamps M, Dauwalder O, Dortet L. Comparison of ETEST(R) superposition method and the MTS Aztreonam-avibactam strip with the reference method for aztreonam/avibactam susceptibility testing. J Antimicrob Chemother. 2023. https://doi.org/10.1093/jac/dkad407.
Zou C, et al. In vitro activity of ceftazidime-avibactam and aztreonam-avibactam against carbapenem-resistant Enterobacteriaceae isolates collected from three secondary hospitals in southwest china between 2018 and 2019. Infect Drug Resist. 2020;13:3563–8.
Zhang B, et al. In vitro activity of aztreonam-avibactam against metallo-beta-lactamase-producing Enterobacteriaceae-A multicenter study in China. Int J Infect Dis. 2020;97:11–8.
Acknowledgements
The Belgian national reference center is supported in part by the Belgian Ministry of Social Affairs through a fund within the national health insurance system (INAMI-RIZIV). We thank all Belgian laboratories who referred clinical isolates to the national reference center.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by Florian Belik, Catherine Berhin, Warda Bouchahrouf, Stephanie Evrard, Martin Hoebeke, Merve Okur, Corentin Deckers and Te-Din Huang. The manuscript was written by Corentin Deckers and Florian Belik and reviewed by Olivier Denis, Pierre Bogaerts, Isabel Montesinos and Te-Din Huang. All authors commented on previous versions of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Deckers, C., Bélik, F., Denis, O. et al. Comparison of testing methods assessing the in vitro efficacy of the combination of aztreonam with avibactam on multidrug-resistant Gram-negative bacilli. Ann Clin Microbiol Antimicrob 23, 47 (2024). https://doi.org/10.1186/s12941-024-00708-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-024-00708-0