Abstract
Objective
In China, rural residents experience poorer health conditions and a higher disease burden compared to urban residents but have lower healthcare services utilization. Rather than an insurance focus on enhanced healthcare services utilization, we aim to examine that whether an income shock, in the form of China’s New Rural Pension Scheme (NRPS), will affect outpatient, inpatient and discretionary over-the-counter drug utilization by over 60-year-old rural NRPS residents.
Methods
Providing a monthly pension of around RMB88 (USD12.97), NRPS covered all rural residents over 60 years old. Fuzzy regression discontinuity design (FRDD) was employed to explore the NRPS causal effect on healthcare services utilization, measured by outpatient and inpatient visits and discretionary over-the-counter drug purchases. The nationwide China Health and Retirement Longitudinal Study (CHARLS) 2018 provided the data.
Results
Without significant changes in health status and medication needs, 60-plus-year-old NRPS recipients significantly increased the probability of discretionary OTC drug purchases by 33 percentage points. NRPS had no significant effect on the utilization of outpatient and inpatient utilization. The increase in the probability of discretionary OTC drug purchases from the NRPS income shock was concentrated in healthier and low-income rural residents. Robustness tests confirmed that FRDD was a robust estimation method and our results are robust.
Conclusion
NRPS was an exogenous income shock that significantly increased the probability of discretionary over-the-counter drug purchases among over 60-year-old rural residents, but not the utilization of inpatient or outpatient healthcare services. Income remains an important constraint for rural residents to improve their health. We recommend policymakers consider including commonly used over-the-counter drugs in basic health insurance reimbursements for rural residents; provide health advice for rural residents to make discretionary over-the-counter drug purchases; and to mount an information campaign on over-the-counter drug purchasing in order to increase the health awareness of rural residents.
Similar content being viewed by others
Introduction
Income-related socioeconomic factors have a significant impact on the health of a population [1, 2], with the healthy aging of those in the lower socioeconomic strata emerging as a major global challenge. Rural populations have both lower income and poorer health. In China and the U.S., the health status of rural residents is poorer than urban residents [3, 4]. Many studies have demonstrated that rural residents do not exhibit a strong awareness or behavior to maintain or improve their health, even when they already have chronic conditions [5, 6]. Chinese rural residents have fewer sources of health information than urban residents, and significantly poorer health literacy [7]. Besides weaker health awareness, Chinese rural residents have poorer innate endowments in medical resource accessibility and per capita healthcare resources [8]. An empirical analysis using the China Health and Nutrition Survey (CHNS) found that the ratio of the actual urban–rural healthcare utilization was 1.744 [9], identifying the urban–rural income gap as an important cause of the unequal rural–urban access to healthcare.
Most of the existing literature focuses on the impact of health insurance on healthcare resource utilization. Regarding rural residents in China, the most studied is the New Rural Cooperative Medical System. But there is evidence that the implementation of the New Rural Cooperative Medical System has not successfully reduced the out-of-pocket costs of rural residents [10,11,12]. The literature on health insurance has not reached uniform conclusions, and cannot fully explain changes, in the use of health care resources among rural residents [13, 14]. Rather than an insurance focus on medical utilization, there is emerging research on the impact of pension receipts on healthcare utilization in develo** countries [15], and poverty alleviation strategies on non-free healthcare services in China [16].
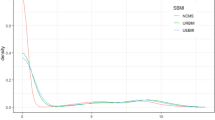
Self-medication behaviors using over-the-counter (OTC) drugs are prevalent in China [RDD Model To test healthcare utilization by NRPS residents, we use a regression discontinuity design (RDD) [35]. This method requires the probability of receiving a pension for rural residents participating in NRPS having a distinct discontinuity at age 60. Figure 1 shows that a significant discontinuity exists at age 60 by conducting a preliminary test for age discontinuity, which allows us to use the regression discontinuity design. Regression discontinuity design (RDD) can be classified as sharp regression discontinuity design (SRDD) and fuzzy regression discontinuity (FRDD). FRDD allows for a small jump in the probability of an individual being assigned to the experimental group at the discontinuity, spanning between zero and one. It means that the individuals on either side of the discontinuity do not coincide with the actual intervention status received, such that individuals on the right side of the discontinuity do not necessarily receive the intervention, and individuals on the left side of the discontinuity may also receive the intervention. The actual age of receiving the pension may not always be exactly 60 years old given the differences in policy and financial status across regions and the seasonality and intensity of policy implementation at the county level [31]. FRDD is thus more germane to the bulk of clinical and policy questions in the sphere of healthcare [36]. Therefore, the discontinuity point formed by the retirement system is a fuzzy discontinuity and FRD is used in our study. Using age 60 as the cutoff, a nonparametric approach was used to estimate the FRDD instrumental variables [37]. Medical resource utilization, for individual i can be expressed as: where \({D}_{i}\) represents the pension-receiving status of an individual, \({D}_{i}\)=1 represents the individual receiving the pension and \({D}_{i}\)=0 represents the individual who does not receive the pension. \({Y}_{i}\) is outcome variable and represents the medical resource utilization for individual i; \({Y}_{1i}\) represents the potential outcome of medical resource utilization when the individual receives a pension and Y0i represents the potential outcome of medical resource utilization when the individual does not receive a pension. The causal effect of pensions on individual outcome variables is: Near the cutoff, the simplicial equation expressed as a conditional expectation function of Yi is: Processing variable Di in the first stage: Therefore, the local average treatment effect (LATE) of the regression discontinuity of pensions on medical resource utilization is estimated by the parsimonious formula after finding the left and right limits at the discontinuity for Eq. (1) as: X is denoted as a set of predetermined variables. In terms of the specific operations of the nonparametric approach, this paper draws on Calonico’s method [37] to obtain the numerator and denominator of the estimated Eq. (5). How to choose the appropriate bandwidth is a key issue in performing nonparametric estimation. The (smaller) larger the bandwidth chosen, the (smaller) larger the sample size included, and the representativeness will (decrease) improve, but the reliability will (improve) decline. The optimal bandwidth for the baseline regression was selected by using the minimum mean square error to balance representativeness and credibility [38]. All analyses are performed by Stata16.0. We used cross-sectional data from the newly released 2018 China Health and Retirement Longitudinal Study (CHARLS). CHARLS data after 2018 is not available to the public. A representative sample covering economic, health, medical and retirement aspects of households and individuals, the CHARLS database has over 19,816 observations on over 45-year-old rural residents from 150 county-level and 450 village-level units across China [39]. In our analysis, we include NRPS enrollees who were 45–75 years old and whose household registration was rural, with no missing data on the outcome variables, which yielded 7878 observations. We used three core healthcare services utilization categorical explanatory variables: 1) whether they made discretionary OTC drug purchases assessed by the question "Did you purchase medicine during the past month (not including prescription medications)"; 2) whether they visited an outpatient clinic during the past month; 3) and whether they received inpatient care in the past year. Covariates include socio-demographic variables and health-related variables. Socio-demographic variables include sex, marital status, income and education level. Income is calculated as personal wage income plus net agricultural income minus pensions, where net agricultural income is the value of the current year's crop minus the proportion for own use, minus input costs. Since a significant proportion (30%) of income was negative and therefore cannot be treated logarithmically, the quartile method was adopted. To accurately identify eligibility for retirement, we generate monthly level age data. For example, the monthly age of a rural resident born in January 1968 is 50 plus one-twelfth, which is 50.083. Health-related variables comprised self-rated health (0 for bad and very bad answers and 1 otherwise); the number of chronic diseases; whether they took a prescribed drug; health insurance (1 yes and 0 no); and depression status. Prescribed drug is an integrated variable consisting of multiple questionnaire responses. In the CHARLS 2018 questionnaire, for certain health conditions (such as diabetes and hypertension) the question was "whether you take the following measures to treat a certain disease" which included both Chinese and Western medicine. In addition to chronic diseases, for certain ailments (such as pain), the respondents were also asked whether they had taken any prescribed treatment measures, including both Chinese and Western medicine. Individuals were assigned a value of 1 when they took prescribed drugs and 0 otherwise. Based on the Center for Epidemiologic Studies Depression Scale (CES-D-10) a score of 10 and above in CHARLS was used to define 1 depression, 0 otherwise [40].Database and sample selection
Dependent variables
Covariates
Results
General characteristics of the respondents
Table 1 presents the general characteristics of the respondents, including outcome variables and convertibles. In addition to the general characteristics of the overall population, Table 1 also show the characteristics of the different age groups, using 60 as a cut-off.
Impact of NRPS on the utilization of healthcare services
Table 2 shows the estimation results for outpatient and inpatient medical service utilization and discretionary over-the-counter drug utilization. The first stage results are about the relationship between age and access to pensions. The standardized age at the discontinuity point is 60 years old. From Fig. 1, the probability of receiving an NRPS pension jumped significantly around age 60, which is consistent with the design of the NRPS system. In addition, the first stage results in Table 2 show the effect of age on pension receipt, and the results are all significant, which provides ample evidence that the cutoff at age of 60 years old was appropriate as an "instrumental variable" for whether to receive a pension.
Following Calonico’s method [38], we calculated the optimal bandwidth under the minimum mean square error and estimated the regression results for the fuzzy discontinuity. From Table 2 Panel A, when the dependent variable is inpatient care, the optimal bandwidth is 3.379 years. The treatment effect of discontinuity regression is not significant with the growth of 9.9 percentage point. From Table 2 Panel B, the optimal bandwidth is 2.739 years when the dependent variable is outpatient visits and the treatment effect of discontinuity regression is not significant with the growth of 11 percentage point. In Table 2 Panel C, when the dependent variable is discretionary OTC drug purchases, the optimal bandwidth is 2.299 years and the discontinuity regression treatment effect is significantly positive. These regression results show that NRPS pension had no significant effect on inpatient and outpatient healthcare services utilization, but had a significant effect on discretionary OTC drug purchasing behavior. Figure 2 visualizes a significant upward jump in the probability of discretionary OTC drug purchasing behavior of individuals after receiving an NPRS pension, where the pension income shock increased the probability of discretionary OTC drug purchases by 33 percentage points among rural residents. When rural residents receive the pension, their income increase one fixed amount compared with no-pension status. The results show that pension receipt significantly increases the probability of spontaneous drug purchase by rural residents. The effect of pensions on outpatient and inpatient services was also positive, but not significant.
Subsample analysis
We conducted a subsample analysis based on health status and income. Health status includes respondents' self-rated health status, whether they are depressed and whether they have chronic diseases. Based on their median household wage income plus net agricultural income, respondents were divided into high-income and low-income groups. In the subsample analysis, we found there were no significant changes in outpatient and inpatient service utilization at age 60. But we confirmed a significant increase in the probability of discretionary OTC drug purchases from the NRPS income shock in healthier populations. Table 3 shows that the impact of the pension income shock on over-the-counter drug purchases was more pronounced among those who were free of depression and chronic illness and who self-rated their health status as moderate or healthy. This suggests that healthier individuals were more likely to increase their investment in their health through over-the-counter discretionary OTC drug purchases after receiving NRPS compared to unhealthy individuals.
Table 3 also shows that self-rated moderate or healthy individuals had a significant 27 percentage point increase in the probability of discretionary OTC drug purchases in response to the NPRS pension shock. The income shock effect on the group that answered poor health was not significant. Similar results were found for the subsample on depression and chronic diseases, where the effect of NPRS on the utilization of health services, including over-the-counter drugs, were not significant, but on the receipt of NPRS, the probability of discretionary OTC drug purchasing behavior increased among rural residents who did not suffer from depression (28%) and did not have chronic diseases (25%). We believe that individuals in poor health, experiencing depression, and self-rating their health as unhealthy might have increased prescribed drug purchases as part of curative inpatient and outpatient services. In contrast, discretionary OTC drug purchases were mainly for symptom relief and disease prevention [41]. The receipt of NRPS relaxed the budget constraint on individual consumption behavior that provided funds for discretionary OTC drug purchases, especially among those who were without chronic diseases and knowledgeable about their health.
Finally, we divided the sample into low- and high-income groups using the mean value of income. The results in Table 3 show that receipt of NRPS mainly influenced the over-the-counter drug purchases of the low-income group, with the probability of discretionary OTC drug purchases by the low-income group increasing by about 50 percentage points. This is consistent with our theoretical framework where income reflects the ability to access related resources and is an important factor influencing the utilization of discretionary drug services. The budget constraint is weaker for the high-income group, while the demand for discretionary drugs is suppressed for the low-income group before receipt of the NRPS. The pension income brought by the NPRS relaxed the budget constraint for the low-income group.
Robustness tests
To test the robustness that over-the-counter drug utilization was driven by the pension, we conducted continuity, data hea**, placebo and regressions using different bandwidths and cutoff tests.
-
1. Continuity test
The prerequisite of applying discontinuity regression is that all predetermined variables are free from discontinuity at the cutoff. All covariates were tested by discontinuity regression, and the regression results are shown in Table 4 and Fig. 3. We first tested the continuity of each predetermined variable at the cutoff, and the regression settings are the same as in the previous regressions, except that the dependent variables are replaced with covariates. In Table 4, the estimation results for variables (1)-(9) show that there is no discontinuity at the cutoff for all the antecedent variables.
-
2. Data hea** test
The fulfillment of the continuity assumption requires that there is no data hea** in the sample population at the cutoff [42]. To test for data hea**, a histogram of the data distribution is shown in Fig. 4, and it is clear from Fig. 4 that there is no data hea**.
-
3. Placebo test
The placebo test shows that the health care burden is affected only by the pension income shock, and not by other factors, when the regression results are insignificant at other ages away from 60. The regression results should be insignificant when we make a "pseudo cutoff" at other ages away from 60 years old. In Table 5, the regression results for "pseudo-cutoff" ages 57, 58, 59, 61, 62, and 63 were not significant, which suggests that the increase in the probability of discretionary OTC drug purchase near the age of 60 was due to NRPS.
-
4. Regression using different bandwidths
Our optimal bandwidth for the baseline regression was symmetric about both sides of the cutoff. Different bandwidths on both sides of the cutoff were applied as a robustness check [37]. Table 6 shows that the regression results were still significant with a bandwidth of 2.861 years on the left side of the cutoff and a bandwidth of 2.380 years on the right side. We also customize 4 years as the bandwidth, and the results remain robust.
-
5. Cutoff
For rural residents, there is no other policy that uses age 60 as a decomposition [43], so the effect of the age 60 cutoff can be attributed to the NRPS income shock.
Discussion
Our results show that the NRPS income shock had no significant effect on inpatient and outpatient utilization among rural residents, but significantly increased the probability of discretionary OTC drug purchases. We offer possible explanations. First, outpatient and inpatient services are unpredictable and irregular, and both outpatient and inpatient hospital services are costly one-time expenditures. An RMB88 (USD12.97) monthly pension income shock cannot address large inpatient and outpatient expenses. Second, different from inpatient and outpatient hospital services, the cost of discretionary OTC drug purchases was small. Whether short-term for a specific illness or regular preventative therapies, it is well-suited for payment by predictable and regular income supplements brought by NRPS. Evidence suggests that additional non-labor income shocks can increase and improve health status and discretionary OTC drug purchasing was a potential pathway for regular non-labor income shock spending [44,45,46]. Third, the price elasticity of demand is more elastic for drugs than for outpatient and inpatient services [47, 48]. Our finding suggests that the relaxation of income constraints after receiving a pension can explain a significant increase in the probability of discretionary OTC drug purchasing, but not for inpatient and outpatient visits. Fourth, in terms of social security payments, small income shocks may have a significant impact on drug purchasing in countries with less well-developed social security systems [49,50,51,52]. Literature focused on the effect of NRPS on alleviating the health care spending burden argued that subsidize income is better than subsidize health insurance [53].
Our result is consistent with the former research focus on pensions in rural China, which also found that pensions encouraged rural people to choose self-treatment [16]. They found that pension did encourage people in the lowest 25% income group to use both outpatient and inpatient services [16]. When we focus on the lowest income quartile, we expect similar results. However, the sample size after dividing our sample into four equal parts was not sufficient to perform RDD. There is also a literature that finds that NRPS can alleviate the healthcare burden of rural residents [53]. For other low- and middle-income countries (LMICs), a literature review suggests that cash transfers may increase healthcare expenditure [54].
We also found that the increased probability of discretionary OTC drug purchases was not due to age-related deterioration in health. Table 4 and Fig. 3 show that self-rated health, number of chronic illnesses, and depression did not change significantly around the cutoff.
Our data suggest that rural residents faced adverse health conditions and drug needs before the NRPS 60-year-old age. Pre-NRPS, rural residents’ low-income levels meant the absence of financial resources to obtain healthcare services [55]. The subsample analysis reconfirmed this proposition. There was no significant change in the health status of the rural elderly before and after receiving the pension. The impact of the NPRS was concentrated on people with better health and lower income. These people had preventive medical needs, but their need for discretionary OTC drug purchases was suppressed pre-NRPS due to budget constraints. The exogenous NPRS income shock helped release the suppressed demand for discretionary drugs, especially by those with an awareness of their health needs.
The health effects of over-the-counter drugs are well documented. As more and more drugs become available over-the-counter, discretionary OTC drug purchases, which are usually available in pharmacies, offer people the opportunity to promote their own health [56]. First, self-medication with over-the-counter drugs is increasingly becoming the choice of treatment for common self-limiting conditions. If over-the-counter drugs are widely available and have a low abuse rate [57], they can address common symptoms, such as fever and pain relief, and health recovery [25, 56, 58, 59]. Second, over-the-counter drugs enable patients to cultivate their awareness and behavior of self-managed healthcare [27, 28, 60]. Self-managed over-the-counter drug purchases are conducive to relieving disease symptoms and reducing disease harm effects before more severe disease happens [61].
Our data do not allow us to further identify the type of over-the-counter purchased by respondents. A national audit released by IQVIA (2022) shows that in 2021, over-the-counter drugs accounted for 42% of the overall retail pharmacy market in terms of sales share [62]. Traditional Chinese medicine (TCM) accounted for 52% of the over-the-counter drug healthcare market, with TCM more common for preventive healthcare than for curative care [24].
We make recommendations for the health promotion of rural residents to attenuate the national public health burden. Prior to receiving their pensions, rural residents experienced ongoing illnesses, but budget constraints suppressed their consumption of discretionary drugs. Delaying medication treatment accelerates disease progression and reduces patient quality of life [63]. From a public health and national burden of disease perspective, suppression of healthcare needs often leads to disease exacerbation, causes augmented disease risk and constraints disease treatment and prevention, which increases the social burden of long-run healthcare [64, 65]. In addition, in the individual perspective, studies suggested that the elderly who adopt self-medication are less likely to use inpatient services, and their hospitalization costs are significantly lower [21]. The economic value of self-medication among the Chinese elderly population is also significant at the individual level.
While recognizing China’s public health budget constraints, we recommend expanding access to healthcare services to the rural population to promote optimal self-medication drug use. Self-medication behaviors with over-the-counter drugs were prevalent in China, which was related to residents’ socio-demographic characteristics and health literacy [ Step** outside the framework of previous work on the impact of health insurance on medical service utilization, we explore the impact of China’s rural pension scheme on rural residents’ healthcare utilization. We found that the NRPS pension, as an income shock, significantly increased the probability of discretionary OTC drug purchases, but had no significant effect on the utilization of outpatient and inpatient services. Discretionary OTC drug purchase was more pronounced among healthier rural residents and those with lower incomes. Various robustness tests confirmed our results. Income shocks might relax budget constraints and time limits to promote self-medicated over-the-counter drug purchases. We suggest that the Government and doctors should pay more attention to self-medicating behaviors such as the usage of over-the-counter drugs in rural areas. Our research findings hold significant implications for policymakers and researchers, as they can serve as a basis for formulating and implementing targeted interventions to optimize the allocation and utilization of healthcare resources within rural communities.Conclusion
Availability of data and materials
The datasets analysed during the current study are available in the China Health and Retirement Longitudinal Study (CHARLS) repository, [http://charls.pku.edu.cn] [39].
Abbreviations
- NRPS:
-
New Rural Pension Scheme
- FRDD:
-
Fuzzy regression discontinuity design
- CHARLS:
-
China Health and Retirement Longitudinal Study
- CHNS:
-
China Health and Nutrition Survey
- ORPS:
-
Old Rural Pension Scheme
- TCM:
-
Traditional Chinese medicine
References
Marmot M, Wilkinson RG. Social determinants of health. Public Health: Local and Global Perspectives. 2nd ed. Oxford: Oxford University Press; 1999.
Oldroyd, J. ‘Social determinants of health’, Public Health: Local and Global Perspectives: Second edition. 2019;15(1):105–123. Available at: https://doi.org/10.4159/9780674989207-006.
Li Yanli, Tan Lexiang, Yan Ju'e, et al. Analysis of health inequality and its decomposition among rural residents. Statistics and Decision. 2015; (20):116–118. (In Chinese). https://doi.org/10.13546/j.cnki.tjyjc.2015.20.033.
Jensen L, Monnat SM, Green JJ, Hunter LM, Sliwinski MJ. Rural population health and aging: Toward a multilevel and multidimensional research agenda for the 2020s. Am J Public Health. 2020;110(9):1328–31. https://doi.org/10.2105/AJPH.2020.305782.
Yuan F, et al. Analysis of awareness of health knowledge among rural residents in Western China. BMC Public Health. 2015;15(1):1–8. https://doi.org/10.1186/s12889-015-1393-2.
He, Z. et al. Factors influencing health knowledge and behaviors among the elderly in rural China. Int J Environ Res Public Health. 2016; 13(10).975. https://doi.org/10.3390/ijerph13100975.
Chen, X et al., Differences in rural and urban health information access and use. J Rural Health. 2019; 35(3), 405–417. https://doi.org/10.1111/jrh.12335.
Cheng, D. N., Pan, C.J. The impact of rural health service accessibility and quality on health inequality among the elderly-an empirical analysis based on CLHLS (2011–2014) data[J]. Social Sciences in Guangxi. 2020; (6):76–82. (In Chinese) https://doi.org/10.3969/j.issn.1004-6917.2020.06.013.
Ma Chao, Gu Hai, S.Z. Inequality of Opportunity of Urban-Rural Health Care Utilization under Compensation Principle’. China Economic Quarterly. (In Chinese). 2017.https://doi.org/10.13821/j.cnki.ceq.2017.03.02.
Lei X, Lin W. The New Cooperative Medical Scheme in Rural China: does More Coverage Mean More Service and Better Health? Health Econ. 2009;18(S2):S25–46. https://doi.org/10.1002/hec.1501.
Long Q, Zhang T, Xu L, Tang S, Hemminki E. Utilisation of maternal health care in western rural China under a new rural health insurance system (New Co-operative Medical System). Tropical Med Int Health. 2010;15(10):1210–7. https://doi.org/10.1111/j.1365-3156.2010.02602.x.
Liu, K., Wu, Q. and Liu, J. Examining the association between social health insurance participation and patients’out-of-pocket payments in China: The role of institutional arrangement. Soc Sci Med. 2014; 113.95–103. https://doi.org/10.1016/j.socscimed.2014.05.011.
Ameyaw, E.K., Kofinti, R.E. & Appiah, F. National health insurance subscription and maternal healthcare utilisation across mothers’ wealth status in Ghana. Health Econ Rev. 2017; 7(16). https://doi.org/10.1186/s13561-017-0152-8.
Finkelstein, et al. The Oregon Health Insurance Experiment: Evidence from the first year. Q J Econ. 2012;127(3):1057–106. https://doi.org/10.1093/qje/qjs020.
Lloyd-Sherlock P. Simple transfers, complex outcomes: The impacts of pensions on poor households in Brazil. Dev Chang. 2006;37(5):969–95. https://doi.org/10.1111/j.1467-7660.2006.00509.x.
Chen S, Chen X, Law S, Lucas H, Tang S, Long Q, Wang Z. How and to what extent can pensions facilitate increased use of health services by older people: evidence from social pension expansion in rural China. BMC Health Serv Res. 2020;20:1–12. https://doi.org/10.1186/s12913-020-05831-0.
Zhang, Z., Ge, P., Yan, M., Niu, Y., Liu, D., **ong, P., ... & Wu, Y. Self-Medication Behaviors of Chinese Residents and Consideration Related to Drug Prices and Medical Insurance Reimbursement When Self-Medicating: A Cross-Sectional Study. Int J Environ Res Public Health. 2022; 19(21).13754. https://doi.org/10.3390/ijerph192113754.
Qin S, Zhao J, Zhou M, Cheng Y, Ding Y. Self-medication and its typology in Chinese elderly population: A cross-sectional study. Front Public Health.2022;10:954305. https://doi.org/10.3389/fpubh.2022.954305.
Chang, J., Wang, Q., & Fang, Y. Socioeconomic differences in self-medication among middle-aged and older people: data from the China health and retirement longitudinal study. BMJ open. 2017; 7(12), e017306. https://doi.org/10.1136/bmjopen-2017-017306.
Sun J, Lyu S. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. 2020;274:399–404. https://doi.org/10.1016/j.jad.2020.05.091.
Zheng Z, Feng Z, Zhang D, Sun X, Dong D, Luo Y, Feng D. Does self-medication reduce medical expenditure among the middle-aged and elderly population? A four-wave longitudinal study in China. Front Public Health. 2022;10:1047710. https://doi.org/10.3389/fpubh.2022.1047710.
Ayalew Mohammed Biset. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adherence. 2017;11:401–13. https://doi.org/10.2147/PPA.S131496.
Zhang Y, Salm M, van Soest A. The effect of retirement on healthcare utilization: Evidence from China. J Health Econ. 2018;62:165–77. https://doi.org/10.1016/j.jhealeco.2018.09.009.
Zhou Q, Eggleston K, Liu GG. Healthcare utilization at retirement in China. Health Econ. 2021;30(11):2618–36. https://doi.org/10.1002/hec.4400.
Eticha, T., & Mesfin, K. Self-medication practices in Mekelle, Ethiopia. PloS one. 2014; 9(5), e97464. https://doi.org/10.1371/journal.pone.0097464
Brewer, H. R., Hirst, Y., Sundar, S., Chadeau-Hyam, M., & Flanagan, J. M. Cancer Loyalty Card Study (CLOCS): protocol for an observational case-control study focusing on the patient interval in ovarian cancer diagnosis. BMJ open. 2020;10(9), e037459. https://doi.org/10.1136/bmjopen-2020-037459.
Stoehr GP, Ganguli M, Seaberg EC, Echemen DA, Belle S. Over-the-Counter Medication Use in an Older Rural Community: The Mo VIES Project. J Am Geriatr Soc. 1997;45(2):158–65. https://doi.org/10.1111/j.1532-5415.1997.tb04501.x.
Amoako EP, Richardson-Campbell L, Kennedy-Malone L. Self-medication with over-the-counter drugs among elderly adults. J Gerontol Nurs. 2003;29(8):10–5. https://doi.org/10.3928/0098-9134-20030801-05.
Grossman, M. On the Concept of Health Capital and the Demand for Health. Journal of Political Economy. 1972; 80(2), 223–255. http://www.jstor.org/stable/1830580
Schultz, T. W. Investment in human capital. The American economic review, 1961; 51(1), 1–17. https://www.jstor.org/stable/1818907
Zhang, C., G. John, Zhao Yaohui. Policy Evaluation of China’s New Rural Pension Program. China Economic Quarterly. (In Chinese). 2015; 203–230. https://doi.org/10.13821/j.cnki.ceq.2015.01.012.
Zhou Y.B., Cao.R. The Effect of China’s New Rural Pension Program on Labor Supply of Middle Aged and Elderly People in Rural Areas of China: Based on PSM-DID, Population and Economics. (In Chinese). 2017; 5(3),95–107. https://doi.org/10.3969/j.issn.1000-4149.
Wang F, Zheng H. Do public pensions improve mental wellbeing? Evidence from the new rural society pension insurance program’. Int J Environ Res Public Health. 2021;18(5):1–15. https://doi.org/10.3390/ijerph18052391.
National Bureau of Statistics of China. China Statistical Yearbook 2019. http://www.stats.gov.cn/tjsj./ndsj/ (Accessed18 December 2022)
Lee DS, Lemieux T. Regression discontinuity designs in economics. Journal of economic literature. 2010;48(2):281–355. https://doi.org/10.1257/jel.48.2.281.
Venkataramani, A. S., Bor, J., & Jena, A. B. Regression discontinuity designs in healthcare research. BMJ. 2016; 352. https://doi.org/10.1136/bmj.i1216.
Calonico S, Cattaneo MD, Farrell MH, Titiunik R. rdrobust: Software for regression-discontinuity designs. Stand Genomic Sci. 2017;17(2):372–404. https://doi.org/10.1177/1536867X1701700208.
Calonico S, Cattaneo MD, Farrell MH. Optimal bandwidth choice for robust bias-corrected inference in regression discontinuity designs. Econometrics Journal. 2021;23(2):192–210. https://doi.org/10.1093/ectj/utz022.
Zhao, Yaohui, Yisong Hu, James P Smith, John Strauss, Gonghuan Yang. 2014. Cohort profile: The China health and retirement longitudinal study (CHARLS), Int J Epidemiol. 2014;43(1): 61–68. https://doi.org/10.1093/ije/dys203.
Lei X, Sun X, Strauss J, Zhang P, Zhao Y. Depressive symptoms and SES among the mid-aged and elderly in China: evidence from the China Health and Retirement Longitudinal Study national baseline. Soc Sci Med. 2014;120:224–32. https://doi.org/10.1016/j.socscimed.2014.09.028.
Klepser ME. Socioeconomic impact of seasonal (epidemic) influenza and the role of over-the-counter medicines. Drugs. 2014;74(13):1467–79. https://doi.org/10.1007/s40265-014-0245-1.
Shigeoka H. The Effect of Patient Cost -Sharing on Utilization, Health, and Risk Protection. American Economic Review. 2014;104(7):2152–84. https://doi.org/10.1257/aer.104.7.2152.
Chen X. Old-age pension and extended families: How is adult children’s internal migration affected? Contemp Econ Policy. 2015;34(4):646–59. https://doi.org/10.1111/coep.12161.
Case. Anne. Does money protect health status? Evidence from South African pensions (NBER Working Paper 8495). Cambridge, MA: National Bureau of Economic Research. 2001; https://doi.org/10.3386/w8495.
Schatz E, Gómez-Olivé X, Ralston M, Menken J, Tollman S. The impact of pensions on health and wellbeing in rural South Africa: Does gender matter? Soc Sci Med. 2012;75(10):1864–73. https://doi.org/10.1016/j.socscimed.2012.07.004.
Kim, S. and Koh, K. The effects of income on health: Evidence from lottery wins in Singapore. Journal of Health Economics.2021; 76.102414. https://doi.org/10.1016/j.jhealeco.2020.102414.
Ellis RP, Martins B, Zhu W. Health care demand elasticities by type of service. J Health Econ. 2017;55:232–43. https://doi.org/10.1016/j.jhealeco.2017.07.007.
Zhou Z, Su Y, Gao J, Xu L, Zhang Y. 2011. New estimates of elasticity of demand for healthcare in rural China. Health policy (Amsterdam, Netherlands), 2011;103(2–3):255–265. https://doi.org/10.1016/j.healthpol.2011.09.005.
Choon, C. N.Social protection in Singapore: Targeted welfare and asset-based social security. Social Protection in East Asia-Current State and Challenges. 2010;90. https://doi.org/10.3390/su11133567.
Haskins, R. Social policy in Singapore: a crucible of individual responsibility. Ethos: J. Soc. Psychol. Anthropol 2011; 9,1–8. https://www.csc.gov.sg/articles/opinion-social-policy-in-singapore-a-crucible-of-individual-responsibility. (Accessed18 December 2022)
Cesarini D, Lindqvist E, Östling R, Wallace B. Wealth, health, and child development: Evidence from administrative data on Swedish lottery players. Q J Econ. 2016;131(2):687–738. https://doi.org/10.1093/qje/qjw001.
Östling R, Cesarini D, Lindqvist E. Association between lottery prize size and self-reported health habits in Swedish lottery players. JAMA Netw Open. 2020;3(3):e1919713–e1919713. https://doi.org/10.1001/jamanetworkopen.2019.19713.
Ma Chao, LI Zhi-le, SUN Zhuanlan3, et al. The Effect of New Rural Pension Scheme on Alleviating the Health Care Spending Burden——Why Subsidize Income Is Better than Subsidize Health Insurance. China Industrial Economics. 2021(4):43–61. (In Chinese). https://doi.org/10.3969/j.issn.1006-480X.2021.04.003.
Pega, F., Pabayo, R., Benny, C., Lee, EY., Lhachimi, SK., & Liu, SY. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on use of health services and health outcomes in low- and middle-income countries. Cochrane Database Syst Rev. 2022 Mar 29;3(3):CD011135. https://doi.org/10.1002/14651858.CD011135.pub3
Ozawa S, Shankar R, Leopold C, Orubu S. Access to medicines through health systems in low-and middle-income countries, Health Policy and Planning.2019; 34,III1–III3. https://doi.org/10.1093/heapol/czz119.
Blenkinsopp, A., & Bradley, C. Patients, society, and the increase in self medication. BMJ (Clinical research ed.).1996; 312(7031):629–632. https://doi.org/10.1136/bmj.312.7031.629.
Cohen JP, Paquette C, Cairns CP. Switching prescription drugs to over the counter. BMJ. 2004;330(7481):39–41. https://doi.org/10.1136/bmj.330.7481.39.
Mukhopadhyay, A., Sarnaik, A. & Deshmukh, D. Interactions of Ibuprofen with Influenza Infection and Hyperammonemia in an Animal Model of Reye's Syndrome.1992. Pediatr Res.31,258–260 https://doi.org/10.1203/00006450-199203000-00012
Hudson GM, Green JM, Bishop PA, Richardson MT. Effects of caffeine and aspirin on light resistance training performance, perceived exertion, and pain perception. The Journal of Strength & Conditioning Research. 2008;22(6):1950–7. https://doi.org/10.1519/JSC.0b013e31818219cb.
Lowe NK, Ryan-Wenger NM. Over-the-counter medications and self-care. Nurse Pract. 1999;24(12):34 (PMID: 10635517).
Brewer, H. R., Hirst, Y., Chadeau-Hyam, M., Johnson, E., Sundar, S., & Flanagan, J. M. Association Between Purchase of Over-the-Counter Medications and Ovarian Cancer Diagnosis in the Cancer Loyalty Card Study (CLOCS): Observational Case-Control Study. JMIR public health surveill. 2023; 9, e41762. https://doi.org/10.2196/41762.
IQVIA Pharma Trend. IQVIA National Audit on Retail Pharmacies in Municipalities at the Prefectural Level https://www.iqvia.com/zh-cn/locations/china/solutions/market-intelligence(Accessed 20 December 2022)
Chan, M. Ten Years in Public Health 2007–2017: Report by Dr Margaret Chan Director-General World Health Organization. 2018. World Health Organization. New York
Mokdad AH, et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–72. https://doi.org/10.1001/jama.2018.0158.
Lichtenberg FR. The impact of pharmaceutical innovation on the burden of disease in Ireland, 2000–2015. J Public Health. 2020;42(4):816–27. https://doi.org/10.1093/pubmed/fdz183.
Ali M, Abbasi BH, Ahmad N, Fazal H, Khan J, Ali SS. Over-the-counter medicines in Pakistan: misuse and overuse. Lancet. 2020;395(10218):116. https://doi.org/10.1016/S0140-6736(19)32999-X.
Cooper, Richard J. Over-the-counter medicine abuse–a review of the literature. J subst use. 2013; 18(2), 82–107. https://doi.org/10.3109/14659891.2011.615002.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
P.Y. contributed to the conceptualization, methodology, formal analysis of the study and drafted the original manuscript. F.L. contributed to the methodology, validation and drafted the original manuscript. S.N., E.M., J.T. and C.C. reviewed and edited the manuscript. C.C. contributed to the validation and management and coordination responsibility for the research. J.W. contributed to Oversight and leadership responsibility for the research activity planning and execution. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. The ethics approval and consent to participate about the datasets analysed during the current study are available in the China Health and Retirement Longitudinal Study (CHARLS) repository, [http://charls.pku.edu.cn] [39].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, P., Li, F., Nicholas, S. et al. Impact of pension income on healthcare utilization of older adults in rural China. Int J Equity Health 22, 166 (2023). https://doi.org/10.1186/s12939-023-01985-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12939-023-01985-5