Abstract
Background
Current ankle prostheses for people with unilateral transtibial amputation (TTA) or transfemoral amputation (TFA) are unable to mimic able-bodied performance during daily activities. A new mechanical ankle–foot prosthesis was developed to further optimise the gait of people with a lower-limb amputation. This study aimed to evaluate the Talaris Demonstrator (TD) during daily activities by means of performance-related, physiological and subjective outcome measures.
Materials and methods
Forty-two participants completed a protocol assessing performance and functional mobility with their current prosthesis and the TD. The protocol comprised the L-test, 2 min of stair climbing, 2 min of inclined treadmill walking, 6 min of treadmill walking at 3 different speeds in consecutive blocks of 2 min, and a 3-m Backward Walk test (3mBWT). Heart rate was measured during each task, and oxygen uptake was collected during all tasks except for the L-test and 3mBWT. Time of execution was recorded on the L-test and 3mBWT, and the rate of perceived exertion (score = 6–20), fatigue and comfort (score = 0–100) were assessed after each task. Paired sample t-tests and Wilcoxon Signed-rank tests were performed to compare outcomes between prosthetic devices. Benjamini–Hochberg corrections were applied to control for multiple comparisons with a level of significance set at α = 0.05.
Results
Subjects with a TTA (N = 28) were faster with their current prosthesis compared to the TD on the L-test and 3mBWT (p = 0.005). In participants with a TFA (N = 14), we observed a tendency towards a higher heart rate during the L-test and towards increased comfort during inclined walking, with the TD compared to the participants’ current prosthetic device (0.05 < p < 0.10). Further, no significant results were observed.
Conclusion
The Talaris Demonstrator is a novel state-of-the-art passive ankle–foot prosthesis for both people with a TTA and TFA. Subjective measures indicate the added value of this device, while overall task performance and intensity of effort do not differ between the Talaris Demonstrator and the current prosthesis. Further investigations unravelling both acute and more prolonged adaptations will be conducted to evaluate the TD more thoroughly.
Similar content being viewed by others
Introduction
After lower limb amputation, individuals with a transfemoral amputation (TFA) and transtibial amputation (TTA) require an ankle–foot prosthesis to regain their ability to ambulate [1]. Nowadays, three different types of ankle–foot prostheses are marketed, namely passive, quasi-passive, and active devices [2, 3]. Passive prostheses rely on a fixed spring and offer basic functionality [4]. Passive ankle–foot prostheses are most commonly used as they are inexpensive and implement cushioning during gait [5]. Unfortunately, those passive ankle–foot prostheses are still unable to mimic able-bodied performance during daily activities as they fail to provide sufficient range of motion and net positive joint work [6, 7]. This induces higher metabolic energy consumption during daily activities, asymmetrical limb loading, and altered gait patterns compared to able-bodied individuals [8,9,10]. Quasi-passive prostheses are also mechanical but equipped with microprocessor technology enabling them to adapt to situations such as walking on an inclined surface [4]. They are incapable of generating power but store and release energy to support forward propulsion. Active or powered prostheses can generate an external force through an actuator and therefore have the ability to mimic intact limb functional characteristics [2, 11].
Mimicking the human ankle function is one of the biggest challenges in replicating non-pathological gait due to the loss of function reducing ankle push-off power during walking [7, 12]. Despite the transition from passive to quasi-passive and more recently to active prosthetic devices, which try to alleviate the loss of function by means of an actuator, the challenge remains [13]. An explanation for not attaining able-bodied functioning is the limited range of motion of the conventional prosthetic ankle joint [14, 15]. The absence of an articulated ankle joint entails increased compensatory strategies such as increased muscle activity of the intact limb and trunk, increased intact limb loading, dam**, and increased trunk rotation [16, 17]. Subsequently, these compensations cause balance disturbance and lead towards an increased risk of falling, which in turn lowers the quality of life [18,19,20]. Furthermore, reduced mobility and gait asymmetries contribute to the increased onset of low back pain, arthritis of the healthy knee, bilateral hip osteoarthritis, reduced hip bone density of the amputated limb, and muscle atrophy in people with a unilateral lower-limb amputation compared to able-bodied individuals [21,22,23,24]. Novel prosthetic devices strive towards restoring physical functioning and preventing secondary injuries by mimicking the gait pattern of able-bodied individuals as closely as possible by obtaining gait symmetry and optimizing comfort. Reducing postural imbalances, enhancing prosthetic functioning, and thereby lowering the onset of secondary injures and thus improving quality of life requires research into the development of ankle–foot prostheses with an articulated ankle joint [25,26,27]. Therefore, a new passive ankle–foot prosthesis (i.e., Talaris Demonstrator) was developed.
The Talaris Demonstrator (TD) is based on previous research with the Ankle Mimicking Prosthetic (AMP-) Foot, with the fundamental aim of develo** a new prosthetic ankle that restores normal gait and posture of individuals with lower-limb amputation [28,29,30,31]. The TD is a prototype in the development process of an innovative passive ankle prosthesis classified as energy storing and releasing foot. The prosthetic ankle is dorsiflexed during the stance phase while a plantar-flexion torque is applied to the ankle. This plantar-flexion torque is provided by the passive elastic components, supporting the user's forward movement while walking. When leaning forward on the intact limb at the end of the stance phase, the elastic component returns to its initial position and produces a passive supporting push-off. The novelty of the foot compared to most prostheses currently being used by people with an amputation is the articulating ankle joint. This articulating joint allows for plantar and dorsal flexion of the foot and adaptivity to changing environmental conditions enhancing user comfort and safety.
Among daily activities, walking is an essential and undeniable factor influencing quality of life in people with a lower limb amputation [32]. Consequently, the assessment of functional performance is usually conducted through gait tasks in which physiological, biomechanical and subjective information is often collected (e.g., 6 min of walking, stair climbing, and incline walking) to evaluate an individual’s functional capacity, gait ability, balance and postural control [33,34,35,36]. To assess the functionality of this prototype and its impact on an individual with lower limb amputation, the purpose of this study is to evaluate the TD during daily activities by means of performance-related, physiological, and subjective outcome measures.
Results
Participants’ characteristics
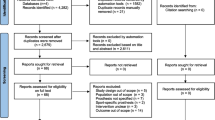
In total, 42 participants completed the study protocol, whereof 28 with a unilateral TTA (female = 5, male = 23) and 14 with a unilateral TFA (female = 3, male = 11). Among individuals with a TTA (right-sided amputation = 8), limb loss was caused by trauma (n = 19), vascular problems (n = 5) and cancer (n = 4). Reasons for limb loss within participants with a TFA (right-sided amputation = 6) were trauma (n = 8), cancer (n = 5) and congenital (n = 1). Furthermore, within individuals with a TTA, 27 had a passive ankle–foot prosthesis and 1 had a quasi-passive one. Within individuals with a TFA, these numbers were 13 and 1, respectively. Participants’ characteristics are displayed in Table 1 and details regarding the individuals' current prosthesis are provided in Table 3 in Appendix. Additionally, the EuroQol-5D questionnaire revealed that the individuals with a TTA indicated having no problems, slight and moderate problems for mobility (n = 22, n = 5 and n = 1, respectively) and pain (n = 13, n = 13 and n = 2, respectively). Furthermore, they reported having slight and moderate problems with anxiety (n = 27 and n = 1, respectively), having no problems, slight and severe problems with daily activities (n = 22, n = 5 and n = 1, respectively) and having no problems with selfcare. Participants with a TFA reported no problems and slight problems with mobility (n = 9 and n = 5, respectively), selfcare (n = 13 and n = 1, respectively), daily activities (n = 10 and n = 4, respectively) and pain (n = 7 and n = 7, respectively), whereas they reported having no problems with anxiety. In terms of perceived health, no significant difference was detected (p = 0.885) between participants with a TTA (86.2 ± 9.4) and TFA (85.9 ± 6.3).
Performance and functional mobility
Table 2 details the means, standard deviations and p-values of the tasks performed with the TD and the current prosthesis. However, within this paragraph the means and standard deviations refer to the pooled means and standard deviations of both prosthetic devices.
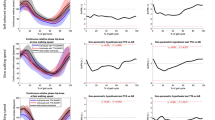
Participants with a TTA performed the L-test and 3-m Backward Walk test (3mBWT) faster with their current prosthesis compared to the TD with mean differences of 1.28 s and 0.56 s, respectively. Heart rate during the L-test and 3mBWT did not differ between prosthetic conditions and amounted to 101 ± 13 bpm during the L-test and 105 ± 15 bpm during the 3mBWT. During stair climbing, slope walking and 6MWT, we observed no differences in walking speed (60 ± 16 steps per minute, 3.2 ± 0.8 m s−1, and 3.4 ± 0.8 m s−1, respectively), heart rate (141 ± 14 bpm, 123 ± 15 bpm and 109 ± 14 bpm, respectively) and oxygen consumption (23.6 ± 6.3 ml · (kg · min)−1, 16.1 ± 4.7 ml · (kg · min)−1 and 11.9 ± 1.2 ml (kg min)−1). On all five tests, we also detected no differences in terms of comfort, fatigue and perceived exertion between the two prostheses.
In participants with a TFA, we found no differences in time required to conduct the L-test (mean time 25.22 ± 6.73 s) and 3mBWT (7.15 ± 3.46 s) between the two prostheses. Heart rate during the L-test and 3mBWT did not differ either, amounting to a mean of 100 ± 13 bpm during the L-test and 98 ± 12 bpm during the 3mBWT. Nonetheless, we observed a tendency towards a higher heart rate during the L-test when walking with the TD. Participants with a TFA did not conduct 2 min of stair climbing because of safety reasons. Furthermore, we detected no differences regarding heart rate (113 ± 15 bpm and 104 ± 14 bpm, respectively), oxygen consumption (14.8 ± 3.6 ml · (kg · min)−1 and 11.6 ± 2.4 ml · (kg · min)−1, respectively) and walking speed (2.9 ± 1.0 m s−1 and 2.8 ± 0.8 m s−1, respectively) during slope walking and 6 min of treadmill walking. During the performance of the four tests, we found no differences in terms of comfort, fatigue and perceived exertion between the two prostheses. However, it must be stressed that we observed a tendency towards significance in terms of comfort during slope walking favouring the TD (mean difference = 14).
System usability
The system usability score is a questionnaire (score = 0–100, mean = 68) that comprises 10 questions aimed at assessing the usability of the TD. Questions 2, 5 and 9 were omitted from the questionnaire because of their irrelevance. We found no difference in scores between participants with a TFA and TTA. The values were 82 ± 16 and 82 ± 17, respectively (p = 0.472).
Discussion
This study aimed at evaluating the TD during daily activities by means of performance-related, physiological, and subjective outcome measures in accordance with the recently published guidelines on prosthetic evaluation [37]. Our results indicated that participants with a TTA were faster with their current prosthesis compared to the TD on the L-test and 3mBWT. Furthermore, our results revealed no significant differences regarding heart rate, oxygen consumption, comfort, perceived exertion, and fatigue in people with a TTA. Yet, we detected a tendency towards a significantly higher level of fatigue during slope walking with the participants’ current device compared to the TD. In addition, despite no differences in comfort being found, it must be noted that comfort was frequently rated higher with the TD compared to the participants’ current device. This could be explained by the more natural feel of the TD's roll-over due to its design. In participants with a TFA, we observed a tendency towards a higher heart rate during the L-test and increased comfort during slope walking and 6 min walking with the TD compared to the participants’ current prosthetic device.
De Pauw et al. found that people with a TTA during treadmill level walking had a self-selected walking speed of 4.1 ± 1.2 km/h, a slow speed of 3.1 ± 0.9 km h−1 and a fast speed of 5.1 ± 1.5 km h−1 [32]. In people with a TFA these values were 2.8 ± 0.9 km h−1, 2.2 ± 0.7 km h−1 and 3.5 ± 1.2 km h−1 respectively [32]. The walking speeds in our study remain within the lower bound of the standard deviations of the values of De Pauw et al. and therefore can be assumed similar. Regarding oxygen consumption, heart rate and rating of perceived exertion, the same conclusion can be drawn [32]. To the best of our knowledge there are currently no studies available on walking speed, heart rate, and oxygen consumption during 2 min slope walking and 2 min of stair climbing. Furthermore, the reference values for performing the L-test amount 29.5 ± 12.8 s in people with a TTA and 41.7 ± 16.8 s in people with a TFA [38]. In our studies people with a TTA and TFA were faster (mean difference: ± 10.5 and 16.7 s, respectively).
The significant difference between the current prosthesis and the TD in time required to complete the L-test and 3mBWT is not deemed clinically relevant as the minimal detectable change for the L-test varies between 2.15 and 3.19 s depending on the cause of amputation and as the minimal detectable change for the 3mBWT ranges between 1.52 and 2.94 s depending on the population [33, 39,40,41]. However, it should be noted that 3mBWT has not yet been validated for people with a limb amputation. The test has been validated originally to identify older adults at risk of falling [42]. It was found that older adults who completed the test in less than 3 s were unlikely to report falling, while those who needed more than 4.50 s were most likely to report falling. Since both older adults and people with a lower limb amputation share a high risk of falling, we opted to implement this test in our protocol [18]. We found that people with a TTA needed on average 4.70 ± 1.44 s to complete the 3mBWT and people with a TFA needed 7.15 ± 3.47 s. Further research validating this test is required to contextualise our results.
Our results generally revealed no discernible differences between the participants' current prosthesis and the TD. This can be attributed to the fact that participants were not provided with a one-month familiarization period to get accustomed to the TD [43]. Only one prototype was built for testing for financial and practical reasons. As such, it was impossible to provide participants with a prosthesis to try out over several weeks. They were allowed approximately 1 h to get acquainted with the prototype, yet this is insufficient to detect true differences in performance [43]. Nevertheless, we observed a tendency towards an instantaneously increment in comfort and decrease in fatigue while walking with the TD compared to the current prosthetic device. This implies that participants might benefit from the TD due to its articulated ankle joint providing flexibility. Furthermore, on average, both participants with a TTA a TFA scored the usability of the TD at 82 out of 100. This score indicates that the device, despite no familiarisation, is rated above average in terms of user convenience and that there is a high probability that participants will recommend the device to other peers [44].
Our study had several limitations. We faced a lot of missing data due to the differences in accommodation among the test facilities. This resulted in 2 participants with TFA being unable to perform the 2-min incline walking, 10 participants with TTA being unable to perform the 2-min stair climbing, and 3 participants with TTA unable to perform 2 min of slope walking. However, the missing data does not outweigh the number of patients we could reach by performing tests in this manner, as finding participants within this population is a challenging task. In addition, we encountered practical issues with the oxygen measuring device, as there was a mismatch between the different user pieces. According to respiratory ventilation (L min−1), the VO2 master is equipped with three different sizes of user pieces. Size R can measure values between 3 and 50 L min−1, size M between 15 and 180 L min−1, and size L between 25 and 250 L min−1. During a strenuous physical task such as climbing stairs, some participants' oxygen consumption was too high for mouthpiece R, and hence no data could be rendered. A combined R and M mouthpiece could solve this bottleneck, as the instrument is easy to handle, portable, reasonably accurate, and features a brief calibration period [45]. Table 4 in Appendix summarises the number of cases analysed per variable.
Secondly, based on the current results of this study, it might have been better to make a sample size calculation to allow for a non-inferiority analysis rather than an analysis aiming at pointing out a difference. This would have enabled us to make a statement about whether the TD is rated equally well as the individuals' current prosthesis. For this study, we estimated the required sample size based on a standard medium effect size of d = 0.5 as studies reporting effect sizes on functional tests evaluating different prostheses are scarce. A total of 28 participants were required to achieve a power of 80% with a level of significance set at 0.05. We did not report any effect size because we found any clinically meaningful differences between the individuals’ current prosthesis and the TD.
A final limitation is that the spring of the TD device was not tailored to the participant’s body mass nor size due to time constraints and the design of the prototype itself, possibly affecting performance, fatigue, and comfort.
Conclusion
This study contributes to a possible beneficial effect of the passive TD for participants with a lower limb amputation due to its flexibility as a tendency towards an instantaneously increment in comfort and decrease in fatigue was found during slope walking compared to the current prosthetic device. Future scope, including biomechanical measures, allowing adequate familiarisation periods and unravelling both acute and more prolonged adaptations, needs to be conducted to evaluate the TD more thoroughly.
Methods
Participants with a unilateral transfemoral and transtibial amputation (TFA and TTA, respectively) were recruited through contacting rehabilitation centres and orthopaedic departments of hospitals in Belgium, and through social media between March and August 2021. All participants (aged 25–75 years) completed their rehabilitation and had a Medicare Functional Classification level K2-4. Adults with a bilateral, a trans-articular knee or hip, or additional upper limb amputation, were excluded as well as participants with neurological disorders or with stump pains and wounds. All participants provided their written consent after being written and verbally informed regarding the study protocol. The study was executed in compliance with the Declaration of Helsinki [46] and was approved by the medical Ethics Committee of the University Hospital of the Vrije Universiteit Brussel (B.U.N. 143201526629) and by the Federal Agencies for Medicines and Health Products (FAGG/80M0860).
Participants visited one of the test sites according to their residence: Axiles Bionics (Brussels), Revarte (Antwerp), University Hospital (UGhent) or Matton Orthopaedics (Bruges or Ghent). On arrival, an anamnesis was performed, biometric measurements were collected and the EuroQol-5D questionnaire, measuring quality of life, was completed [47, 48]. The participants completed an experimental protocol assessing performance and functional mobility. It comprised the L-test (ICC > 0.96) [38] followed by 2 min of stair climbing [49], 2 min of inclined treadmill walking at 10% [49], 6 min of treadmill walking in consecutive blocks of 2 min and at last, a 3-m Backward Walk test (3mBWT, ICC > 0.94) [39]. Both the L-test and 3mBWT were performed 3 times. Between different trials of the L-test and 3mBWT, a 30-s pause was provided and between each task a 60-s pause was included. Regarding the consecutive blocks of 2 min during the 6 min treadmill walking, those consisted of walking at self-selected (SS) speed, at 75% of the SS speed and at 125% of the SS speed [3]. The protocol was completed with both the individuals’ current prosthesis and the TD, in a randomized order, to enable comparison. Both devices were fitted to the individuals’ preference of which the TD was fitted by adjusting the length of the pylon and pyramid connector and by customizing the amount of rigidity. After completing the protocol with the TD, the user-friendliness of the device was questioned by means of the system usability scale [50].
Oxygen uptake (VO2, ml·kg−1·min−1) was measured by means of a portable ergospirometer (VM Pro, VO2 Master Health Sensors Inc., Canada) (typical error for absolute VO2 < 0.3L·min−1) [45]. Data was transmitted in real-time to the VO2master’s mobile application (VO2 Master Manager). Heart rate (beats per minute) was measured continuously by means of a chest strap (Cyclus2, RBM elektronik-automation GmbH, Germany) and was also transmitted in real-time to the same application. The VM Pro Analyzer was calibrated according to the manufacturer’s guidelines before each test after which baseline measurements were collected (i.e. heart rate, oxygen uptake, and level of comfort and fatigue by means of visual analogue scales (VAS comfort & VAS fatigue, respectively)) [51]. Heart rate was measured during each task and oxygen uptake was collected on all tasks except for the L-test and 3mBWT since these two tests are too short to obtain reliable data on oxygen uptake [52]. Time was recorded on the L-test and 3mBWT, and the rating of perceived exertion [53], fatigue and comfort were assessed after each task.
Data processing and statistical analysis
The collected data were imported to excel. On all tasks excluding the L-test and 3mBWT, heart rate data and oxygen consumption were averaged over de last 10 s of the measurements. Once data was processed, the excel file was imported in IBM SPSS Statistics, version 27 (IBM Corp., Armonk, N.Y., USA) for statistical analysis. Shapiro–Wilk tests were applied to access normality. If normality was assumed, a paired sample t-test was applied. If normality was not assumed, the non-parametric Wilcoxon Signed-rank test was performed. Benjamini–Hochberg corrections were applied to control for multiple comparisons with a level of significance set at α = 0.05.
Availability of data and materials
The authors declare that all data supporting the findings of this study are available within this article.
Abbreviations
- TTA:
-
Individual with a unilateral transtibial amputation
- TFA:
-
Individual with a unilateral transfemoral amputation
- TD:
-
Talaris Demonstrator
- VAS:
-
Visual analogue scale
- RPE:
-
Rating of perceived exertion
- 3mBWT:
-
3-m Backward Walk test
- SS:
-
Self-selected speed
- VO2 :
-
Oxygen uptake
References
Stevens PM, Rheinstein J, Wurdeman SR. Prosthetic foot selection for individuals with lower-limb amputation: a clinical practice guideline. J Prosthet Orthot. 2018;30(4):175–80.
Versluys R, Beyl P, Van Damme M, Desomer A, Van Ham R, Lefeber D. Prosthetic feet: state-of-the-art review and the importance of mimicking human ankle-foot biomechanics. Disabil Rehabil Assist Technol. 2009;4(2):65–75.
De Pauw K, Serrien B, Baeyens JP, Cherelle P, De Bock S, Ghillebert J, et al. Prosthetic gait of unilateral lower-limb amputees with current and novel prostheses: a pilot study. Clin Biomech. 2020;71:59–67.
Windrich M, Grimmer M, Christ O, Rinderknecht S, Beckerle P. Active lower limb prosthetics: a systematic review of design issues and solutions. Biomed Eng Online. 2016;15(3):140.
Schlafly M, Reed KB. Novel passive ankle-foot prosthesis mimics able-bodied ankle angles and ground reaction forces. Clin Biomech. 2020;72:202–10.
Au SK, Weber J, Herr H. Powered ankle–foot prosthesis improves walking metabolic economy. IEEE Trans Rob. 2009;25(1):51–66.
Winter DA, Sienko SE. Biomechanics of below-knee amputee gait. J Biomech. 1988;21(5):361–7.
Su PF, Gard SA, Lipschutz RD, Kuiken TA. Differences in gait characteristics between persons with bilateral transtibial amputations, due to peripheral vascular disease and trauma, and able-bodied ambulators. Arch Phys Med Rehabil. 2008;89(7):1386–94.
Pickle NT, Grabowski AM, Jeffers JR, Silverman AK. The functional roles of muscles, passive prostheses, and powered prostheses during sloped walking in people with a transtibial amputation. J Biomech Eng. 2017;139(11):1110051–11100511.
Russell Esposito E, Rábago CA, Wilken J. The influence of traumatic transfemoral amputation on metabolic cost across walking speeds. Prosthet Orthot Int. 2017;42(2):214–22.
Cherelle P, Mathijssen G, Wang QN, Vanderborght B, Lefeber D. Advances in propulsive bionic feet and their actuation principles. Adv Mech Eng. 2014;6:984046.
Silverman AK, Fey NP, Portillo A, Walden JG, Bosker G, Neptune RR. Compensatory mechanisms in below-knee amputee gait in response to increasing steady-state walking speeds. Gait Posture. 2008;28(4):602–9.
Lechler K, Frossard B, Whelan L, Langlois D, Müller R, Kristjansson K. Motorized biomechatronic upper and lower limb prostheses-clinically relevant outcomes. Pm r. 2018;10(9 Suppl 2):S207–19.
Heitzmann DWW, Salami F, De Asha AR, Block J, Putz C, Wolf SI, et al. Benefits of an increased prosthetic ankle range of motion for individuals with a trans-tibial amputation walking with a new prosthetic foot. Gait Posture. 2018;64:174–80.
Lamers EP, Zelik KE, editors. Importance of prosthetic ankle range-of-motion for ascending and descending slopes. 40th Annual Meeting of the American Society of Biomechanics, Raleigh, NC, USA; 2016.
Esquenazi A. Gait analysis in lower-limb amputation and prosthetic rehabilitation. Phys Med Rehabil Clin N Am. 2014;25(1):153–67.
Wentink EC, Prinsen EC, Rietman JS, Veltink PH. Comparison of muscle activity patterns of transfemoral amputees and control subjects during walking. J Neuroeng Rehabil. 2013;10:87.
Steinberg N, Gottlieb A, Siev-Ner I, Plotnik M. Fall incidence and associated risk factors among people with a lower limb amputation during various stages of recovery—a systematic review. Disabil Rehabil. 2019;41(15):1778–87.
Barnett CT, Vanicek N, Polman RC. Temporal adaptations in generic and population-specific quality of life and falls efficacy in men with recent lower-limb amputations. J Rehabil Res Dev. 2013;50(3):437–48.
Rodrigues FB, Andrade AO, Vieira MF. Effects of inclined surfaces on gait variability and stability in unilateral lower limb amputees. Med Biol Eng Comput. 2019;57(11):2337–46.
Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29.
Highsmith MJ, Goff LM, Lewandowski AL, Farrokhi S, Hendershot BD, Hill OT, et al. Low back pain in persons with lower extremity amputation: a systematic review of the literature. Spine J. 2019;19(3):552–63.
Probsting E, Blumentritt S, Kannenberg A. Changes in the locomotor system as a consequence of amputation of a lower limb. Z Orthop Unfall. 2017;155(1):77–91.
Rábago CA, Wilken JM. The prevalence of gait deviations in individuals with transtibial amputation. Milit Med. 2016;181(suppl_4):30–7.
Laferrier JZ, Gailey R. Advances in lower-limb prosthetic technology. Phys Med Rehabil Clin N Am. 2010;21(1):87–110.
Soares AS, Yamaguti EY, Mochizuki L, Amadio AC, Serrão JC. Biomechanical parameters of gait among transtibial amputees: a review. Sao Paulo Med J. 2009;127(5):302–9.
Vrieling AH, van Keeken HG, Schoppen T, Otten E, Halbertsma JP, Hof AL, et al. Gait initiation in lower limb amputees. Gait Posture. 2008;27(3):423–30.
Cherelle P, Grosu V, Cestari Soto M, Vanderborght B, Lefeber D. The AMP-Foot 3, new generation propulsive prosthetic feet with explosive motion characteristics: design and validation. Biomed Eng Online. 2016;15:21–36.
Cherelle P, Grosu V, Matthys A, Vanderborght B, Lefeber D. Design and validation of the ankle mimicking prosthetic (AMP-) Foot 2.0. IEEE Trans Neural Syst Rehabil Eng. 2014;22(1):138–48.
Cherelle P, Junius K, Grosu V, Cuypers H, Vanderborght B, Lefeber D. The AMP-Foot 2.1: actuator design, control and experiments with an amputee. Robotica. 2014;32(8):1347–61.
Convens B, Dong D, Furnémont R, Verstraten T, Cherelle P, Lefeber D, et al. Modeling, design and test-bench validation of a semi-active propulsive ankle prosthesis with a clutched series elastic actuator. IEEE Robot Autom Lett. 2019;4(2):1823–30.
De Pauw K, Cherelle P, Roelands B, Lefeber D, Meeusen R. The efficacy of the ankle mimicking prosthetic foot prototype 4.0 during walking: physiological determinants. Prosthet Orthot Int. 2018;42(5):504.
Hunter SW, Frengopoulos C, Holmes J, Viana R, Payne MW. Determining reliability of a dual-task functional mobility protocol for individuals with lower extremity amputation. Arch Phys Med Rehabil. 2018;99(4):707–12.
Cieslak G, Omana H, Madou E, Frengopoulos C, Viana R, Payne MW, et al. Association between changes in subjective and objective measures of mobility in people with lower limb amputations after inpatient rehabilitation. Am J Phys Med Rehabil. 2020;99(11):1067–71.
Lin SJ, Bose NH. Six-minute walk test in persons with transtibial amputation. Arch Phys Med Rehabil. 2008;89(12):2354–9.
Hafner BJ, Askew RL. Physical performance and self-report outcomes associated with use of passive, adaptive, and active prosthetic knees in persons with unilateral, transfemoral amputation: Randomized crossover trial. J Rehabil Res Dev. 2015;52(6):677–700.
Ghillebert J, Bock SD, Flynn L, Geeroms J, Tassignon B, Roelands B, et al. Guidelines and recommendations to investigate the efficacy of a lower-limb prosthetic device: a systematic review. IEEE Trans Med Robot Bionics. 2019;1(4):279–96.
Deathe AB, Miller WC. The L test of functional mobility: measurement properties of a modified version of the timed “up & go” test designed for people with lower-limb amputations. Phys Ther. 2005;85(7):626–35.
Özden F, Özkeskin M, Bakırhan S, Şahin S. The test-retest reliability and concurrent validity of the 3-m backward walk test and 50-ft walk test in community-dwelling older adults. Ir J Med Sci. 2021.
Unver B, Sevik K, Yarar HA, Unver F, Karatosun V. Reliability of 3-m backward walk test in patients with primary total knee arthroplasty. J Knee Surg. 2020;33(6):589–92.
Abit Kocaman A, Aydoğan Arslan S, Uğurlu K, Katırcı Kırmacı Z, Keskin ED. Validity and reliability of the 3-meter backward walk test in individuals with stroke. J Stroke Cerebrovasc Dis. 2021;30(1): 105462.
Carter V, Jain T, James J, Cornwall M, Aldrich A, de Heer HD. The 3-m backwards walk and retrospective falls: diagnostic accuracy of a novel clinical measure. J Geriatr Phys Ther. 2019;42(4):249–55.
Wanamaker AB, Andridge RR, Chaudhari AM. When to biomechanically examine a lower-limb amputee: a systematic review of accommodation times. Prosthet Orthot Int. 2017;41(5):431–45.
Lewis J, Sauro J. Item benchmarks for the system usability scale. J Usability Stud. 2018;13:158–67.
Montoye AHK, Vondrasek JD, Hancock JB 2nd. Validity and reliability of the VO2 Master Pro for oxygen consumption and ventilation assessment. Int J Exerc Sci. 2020;13(4):1382–401.
World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14–8.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Versteegh MM, Vermeulen KM, Evers SM, de Wit GA, Prenger R, Stolk EA. Dutch tariff for the five-level version of EQ-5D. Value in Health. 2016;19(4):343–52.
Reid L, Thomson P, Besemann M, Dudek N. Going places: does the two-minute walk test predict the six-minute walk test in lower extremity amputees? J Rehabil Med. 2015;47(3):256–61.
Brooke J. SUS: A quick and dirty usability scale. Usability Eval Ind. 1995;189.
Lee KA, Hicks G, Nino-Murcia G. Validity and reliability of a scale to assess fatigue. Psychiatry Res. 1991;36(3):291–8.
Xu F, Rhodes EC. Oxygen uptake kinetics during exercise. Sports Med. 1999;27(5):313–27.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81.
Funding
This study is funded by the Innoviris project Talaris and is part of the SRP17 Exercise and the Brain in Health & Disease: The Added Value of Human-Centered Robotics.
Author information
Authors and Affiliations
Contributions
EL drafted the work. EL, MAD, RM and KDP contributed substantially to the conceptualisation of the work. EL, MAD and KDP contributed substantially to the design of the work. EL and TA contributed substantially to the acquisition of the work. EL, MAD and TA contributed substantially to the data analysis and data interpretation of the work. All authors revised the work critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided their written consent after being written and verbally informed regarding the study protocol. The study was approved by the medical Ethics Committee of the University Hospital of the Vrije Universiteit Brussel (B.U.N. 143201526629) and by the Federal Agencies for Medicines and Health Products.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lathouwers, E., Ampe, T., Díaz, M.A. et al. Evaluation of an articulated passive ankle–foot prosthesis. BioMed Eng OnLine 21, 28 (2022). https://doi.org/10.1186/s12938-022-00997-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12938-022-00997-6