Abstract
This study aimed to determine the effects of melatonin administration on testicular vascular perfusion in relation to steroid hormones and semen characteristics in dogs. The study included 12 normospermic German shepherd dogs (weighed 35 ± 0.5 kg and aged 4 ± 0.5 years). Males received a single melatonin administration (melatonin dimethyl sulfoxide + corn oil via subcutaneous route; MEL; n = 6), while the rest of the animals served as controls (dimethyl sulfoxide + corn oil; Control; n = 6). Males were subjected to routine examination on days -15, 0, 15, 30, 45, and 60. All examined dogs were subjected to Doppler screening, semen collection, and blood sampling. The MEL group showed a significant (P < 0.05) elevation in semen volume, concentration, percentage of sperm motility, and total sperm × 106 / ejaculate compared to other control males. Doppler indices as resistance (RI) and pulsatility (PI) indices declined (P < 0.05) from D 30 (1.02 ± 0.01) until day 60 (0.87 ± 0.02) of treatment. In MEL males, the peak systolic point of velocity (PSV; cm/sec) of the testicular artery elevated (P < 0.05) on day 60 (20.15 ± 0.99) compared to its value on day 0 (17.39 ± 1.84). On D 60, the levels of testosterone (T), estradiol 17-ß (E2), and nitric oxide (NO) elevated (P < 0.05). A negative correlation was detected between testicular volume, scrotal circumference (SC), T levels, Doppler indices, and velocities. In conclusion, single melatonin administration could improve testicular vascularization via increasing Doppler velocities and intratesticular colored areas. In addition, it could improve semen picture and steroids (T and E2) and nitric oxide.
Similar content being viewed by others
Introduction
Canines can be bred so long as they are predominantly fertile, and maintaining this species's reproductive ability remains an issue of interest [1]. A male's potential fertility can be predicted by evaluating the quality of the semen before the beginning of its reproductive life [2]. Palpation is regarded as an ineffective approach for measuring the testicular parenchyma [3]. B- mode ultrasonographic examination of the male reproductive organs has gained popularity since it is a simple method for evaluating biometric parameters but lacks information about the organ vasculature [3]. The testicular vasculature system is the primary conduit for nutrients and other hormones to and from the testis [4]. Numerous animal species have employed testicular blood flow measurements to assess the functionality of the testicles [5, 6]. Color Doppler ultrasonographic technology has been demonstrated for the assessment of male fertility in humans via the determination of testicular functionality [7, 8] and has been applied in veterinary medicine to a variety of species, including dogs [9,10,11], rams [12, 13], and stallions [14, 15]. This ultrasound tool may be a good predictor of semen quality in humans [8] and dogs [16]. Testing hemodynamic alterations using pulsed Doppler ultrasound is a crucial step in diagnosing various cases of testicular dysfunction because testicular blood flow is essential for steroidogenic and spermatogenic processes in farm animals [14]. Since basal nitric oxide controls testicular hemodynamics [17], nitric oxide (NO) is regarded as a free radical associated with the erection process [18]. Additionally, testosterone evaluation is essential for identifying subfertility affections, which are problems with fertility [19].
The pineal gland secretes melatonin. Melatonin is a tryptophan derivative that is widely recognized as a potent antioxidant [20, 21]. Melatonin plays a vital role in stimulating antioxidant enzymes in the reproductive system [22, 23], as well as in all body systems, against free radicals [24]. In men, melatonin regulates GnRH and LH secretion, testosterone production, and testicular maturation, thereby preventing environmental toxin-induced testicular damage [25, 26]. Several previous animal studies have demonstrated melatonin's positive role in reproductive performance [22, 27, 28]. To date, the effect of subcutaneous melatonin injection on testicular perfusion is poorly understood in canines. Hence, we hypothesized that examining the effects of melatonin administration could contribute to enhancing semen quality and vascular perfusion. This study determined the impact of melatonin injection on the testicular hemodynamic pattern in relation to steroid hormones and semen quality in dogs.
Materials and methods
The Faculty of Veterinary Medicine at Cairo University accepted all procedures in this study with an approval number Vet CU 24112020262. This work was performed at the Surgery, Anesthesiology, and Radiology Department, Faculty of Veterinary Medicine-Cairo University (30.0154° N, 31.2120° with a temperature 25–33°C, and relative humidity 55%) between September 1st and October 30th, 2020.
Animals and management
Prior to melatonin administration, all males underwent monthly semen collection and evaluation. Twelve dogs (German Shepherd; normospermic; 35±0.5 kg BW, age: 4±0.5 years) were included in this study, as all males had excellent fertility confirmed by semen collection and semen picture assessment. During the study, all animals were housed indoors with daily exercise and fed commercial food composed of cereals such as rice bran, fats, vegetables, and vitamins, with free access to water all day. All males underwent the clinical examination, followed by ultrasonographic scanning of the male genital organs [29, 30].
Melatonin injection
Dogs were categorized as males who received a single dose of melatonin: melatonin+ DMSO+ corn oil (MEL group; n=6), and dogs that served as the control group (Control group; n=6) received only DMSO + corn oil. Melatonin (from Sigma Chemicals) was dissolved in DMSO with corn oil of 1 ml [31] at a final concentration of 18 mg of melatonin/animal by the subcutaneous route with 2 ml of the final mixture (MEL group; n=6) as previously done in cats [32]. The drug solubility was approximately 30 mg/ml. Due to its short half-life, melatonin was dissolved in the early morning and administered immediately at day zero [33]. The dose was estimated by mixing 108 mg of melatonin powder in 6 ml of DMSO and extended with an equal volume of corn oil (6 ml).
Experimental design
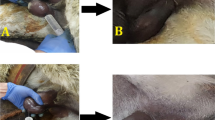
Males were subjected to routine examination (every 15 days: 2 times/month) at days -15, 0, 15, 30, 45, and 60 to determine the effect of a single injection of melatonin on testicular hemodynamics and semen pictures compared to other non-injectable animals serving as controls. Dogs were subjected to blood collection, semen collection, and Doppler examination. The assessment was performed on day −15 before melatonin administration to minimize extragonadal contribution (Fig. 1), and the examination was extended to day 60.
Semen collection and evaluation
This procedure was best carried out in the presence of an estrous bitch. The dog's penis was initially vigorously rubbed through the prepuce at the level of the bulbus glandis until a partial erection appeared. Then, a complete erection was achieved by squeezing the penis between the index inger and thumb, followed by pelvic thrusting. The first two fractions were collected to determine the semen volume (mL), and the obtained semen samples were then sent to the lab for additional examination. All semen samples were collected in falcon tubes (50 ml, one collection every 15 days). In a calibrated tube, direct measurements of the canine semen volume were determined. With the aid of a light microscope and a hemocytometer, the sperm cell concentration was calculated [34]. The sperm cell concentration was used to calculate the total number of sperm in the ejaculate [35]. Immediately after collection, the percentage of sperm motility was subjectively estimated to the nearest 5%, using a phase-contrast microscope with a heated stage (37°C) at 200× magnification [36]. Two observers each examined a sample, and the variation within a sample never exceeded 5%.
Blood sampling and hormonal assaying
Blood samples were drawn from the male dog's jugular vein and centrifuged at 3000 xg for 15 minutes prior to grey and Doppler assessments. Prior to hormonal analysis, plasma and serum samples were kept at 20°C. Serum samples were utilized to assess nitric oxide (NO), which was previously measured in accordance with the instructions of the commercial kit as serum samples were mixed with an equal amount of Griess reagent and incubated for 10 minutes at room temperature. Plasma samples were used to analyze both testosterone (T) and estradiol 17-ß (E2).
Scrotal circumference measurement
As previously performed in bucks, the circumference of the entire scrotum was measured by tape in both control and MEL-treated dogs [36].
Ultrasonographic evaluation
The same operator performed all ultrasound measurements using a lineararray probe. The settings of the Doppler device (EXAGO, France) were optimized as follows: frequency ranged from 7.5 to 10 MHz[37], the pulse repetition frequency (PRF) was 4000 kHz, the Doppler angle of insonation in the spectral mode was 45°±5, the wall filter was 150, and the gate window size was 1 mm [38, 39].
Measurement of the testicular artery Doppler parameters
The three best continuous waves with complete systolic and diastolic endpoints were measured to determine all Doppler velocimetry measurements, including peak systolic velocity (PSV; cm/sec), end-diastolic velocity (EDV; cm/sec), and both Doppler indices expressed by the resistance index (RI) and pulsatility index (PI) that most commonly used [40, 41]. The distal branch of the testicular artery was identified using image-specific waves [42].
Evaluation of pampiniform colored area% and testicular volume
The testicular volume could be calculated using the ellipsoid formula: length (L), width (W), and height (H) x0.5236; meanwhile, the pampiniform colored area/pixels divided by the area of the region/pixels was used to calculate the percentage of colored areas in the pampiniform plexus. All frozen images were stored in flash memory for pixel analysis using the Photoshop tool in version CCX64 [43].
Statistical analysis
Data were assessed using SPSS software (SPSS, 2007). All data are presented as the mean ± standard error of the mean and were first checked for normality by the Shapiro‒Wilk test. The paired t-test was used to compare between two means of the same animal; the right and left sides of the animals. To compare time points within the group and investigate the effects of treatment and time, repeated measures ANOVA was used to examine differences in concentrations, sperm motility %, volume, the total count of sperm per ejaculation, and Doppler parameters. The significant means (P<0.05) were separated using Duncan multiple range tests. In MEL dogs, correlation coefficients were calculated between testicular blood flow waveform measurements and semen analytical parameters.
Results
Testicular volume assessment
The investigation was completed to examine the impact of melatonin administration throughout various time intervals (days 0, 15, 30, 45, and 60). In dogs, there were no variations between the right and left testicles. Testicular length, width, and height were calculated via grey B- mode to determine the testicular volume, as shown in (Fig. 2a & b).
Semen characteristics evaluation
From day 30 (7.03 mL± 0.02) until the end of the examination (D 60, 7.65 mL± 0.02), there was an increase (P <0.05) in semen volume in the MEL group compared to controls. The MEL dogs showed a substantial increase in sperm concentration from D 15 following melatonin injection (266×106± 40.31/mL) when compared to D 60 (310×106± 15.62/mL). In advance, the total sperm number/ejaculation was increased (P <0.05) in the MEL dogs at day 30 after melatonin injection (952×106 spermatozoa/total ejaculated) when compared to day 60 (995×106 spermatozoa/total ejaculated), as depicted in Table 1. At day 30, the sperm motility % (P< 0.05) increased from 85.01 ± 3.71 to 90.21 ± 3.55.
Testicular hemodynamics
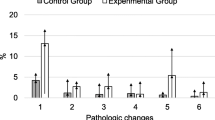
Melatonin reduced the main Doppler pulsatility (PI) and resistance (RI) indices from D 30 (1.02±0.0.01 for PI, and 0.51±0.01 for RI) when compared to D 60 (0.87±0.02 for PI and 0.44±0.01 for RI; Table 2). The percentage of the pampiniform colored region (Fig. 3) was elevated (P<0.05) from D 30 (81.62±2.91) when compared to D 60 (88.97±7.21) in the MEL group compared to the control group at days 30 and 60 (71.88±3.58 and 76.15±3.81).
Scrotal circumference, morphometry, Doppler velocities, and hormonal levels on day 0 and day 60
However, melatonin injection did not significantly alter the testicular volume (P> 0.05). The distal supra-testicular artery PSV (cm/sec) was elevated significantly (P<0.05) at day 60 when compared to day 0 in the MEL males, but its value did not show a marked difference in normal dogs in two-time points (18.09±2.14 on D 0, and 18.32±2.05 on D 60; Table 3). The EDV (cm/sec) was unaffected by melatonin treatment (P > 0.05), but the scrotal circumference (cm) was slightly increased (P> 0.05) by the melatonin treatment at day 60 compared to day 0 since this elevation was non-significant.
The intratesticular colored area was increased in the MEL group at the end of examination (5999±45.21) compared to D0 of melatonin treatment (4985±26.32; Table 3), while in the normal males, the colored area value on D 0 was 4865±12.54 and on D 60 was 4556±11.82. In addition to testosterone, NO levels were elevated in MEL dogs at D 60 (8.98±0.14 for testosterone and 64.25±5.66 for NO). In contrast, estradiol 17-ß levels were elevated at D 60 (55.21±2.31) compared to D 0(32.15±1.54) in MEL dogs (Table 3). A negative correlation was noticed between distal artery Doppler indices and Doppler velocities, scrotal circumference, plasma testosterone levels, NO levels, and testicular volume in all dogs, as shown in Table 4.
Discussion
The pineal gland secretes an effective antioxidant hormone called melatonin, and this hormone acts as a direct scavenger of all free and hydroxyl toxic radicals and acts as an activator of some antioxidative enzymes such as glutathione peroxidase [44]. In addition, melatonin could protect DNA from damage under the effect of stress [45]. Furthermore, the melatonin hormone improved the process of spermatogenesis in animals when injected a few minutes prior to ischemia, and then after one day, melatonin improved the spermatogenesis process[46]. This finding aligns with our present study as we injected a single dose of melatonin and then assessed the morphometric measurements throughout 60 days. The semen characteristics, including (volume, concentration, total sperms×106/ejaculation, and motility %) were increased in the MEL group, which concluded that melatonin injection could improve the semen quality and spermatogenesis process. Similarly, a study by Hemadi et al. [47] reported that one week of melatonin administration in the vitrified neonate testis that is grafted could play a critical role in the enhancement of the spermatogenesis through increasing the epithelium thickness [48].
Contradictory to our findings, another study revealed that melatonin did not affect semen quality and spermatogenesis [49]. However, this can be attributed to the different doses we used in the current study as well as the follow-up analysis every 15 days to demonstrate the effects on semen picture, as melatonin has a critical direct effect on male reproductive performance and share in testosterone synthesis from the Leydig cells in human [50] and animals [46].
In addition, melatonin-treated bulls exhibited an increase in semen picture and motility % by monitoring the hypothalamic-anterior pituitary testicular axis [51]. This enhancement may be due to the melatonin's primary effect on testicular blood flow, accompanied by increased steroid hormones ( estradiol and testosterone) and NO levels.
To our knowledge, the present study is the first to report the effect of subcutaneous injection of melatonin in dogs which a particular preference for the distal branch of supra testicular hemodynamics alterations. The relevant results proved the hypothesis that a single melatonin injection could improve testicular vascular perfusion through enhancement of the semen quality, steroidogenesis, and hormonal profile. This data is significant in improving male dog productivity and reproductive pattern [52].
The improvement of testicular blood flow by the melatonin injection led to a mark in both Doppler indices parameters of the distal supra testicular arteries (PI and RI), which have a strong negative correlation with blood velocities parameters (PSV and EDV), testicular volume and intra-testicular colored areas[53,54,55]. The marked linear decline in both two Doppler indices leads to a substantial decrease in the blood flow resistance pattern and, therefore, an elevation of the testicular blood supply with an increase in sufficient nutrients and oxygen within both testes [56,57,58,59,60].
The administration of melatonin in the form of an implant also leads to the stimulation of GnRH and testosterone levels [61, 62], as the melatonin action on the interstitial cells is related to the presence of melatonin-specific receptors in spermatogonial cells within the testis [63]. Melatonin is known to be involved in the production of estrogen from androgen via aromatase enzyme [64], and our present study reported a significant elevation of estradiol levels linked with a marked declination in both Doppler indices after melatonin administration. This finding can be attributed to the fact that estradiol has a vasodilatation action in testicular artery vascularization [65], in addition to the role of melatonin in the production of estrogen.
According to Zarlingo et al. [66], nitric oxide (NO), which is also evaluated by its blood metabolites (NOMs), plays a significant role in controlling blood flow [67, 68]. Due to the rapid inactivation of NO by reactive oxygen species (ROS), increasing NO levels in melatonin-treated dogs may increase the bioavailability of both NO and NOMs [69]. Melatonin may address this issue by preventing NO and ROS from reacting. Doppler ultrasonography in veterinary Andrology is still uncommon compared to human medicine. This restriction is attributable to two primary factors: the cost of portable devices and the second is the experts' lack of expertise. Finally, the angle of insonation that was impacted by the Doppler shift should be standardized in addition to the animal movement that may alter the Doppler reading measures
Conclusion
This study revealed that one dose of melatonin increases testicular blood flow, triggers a significant rise in testosterone, estradiol, and nitric oxide levels, raises canine semen quality indicators, and decreases both Doppler readings of the distal supra-testicular artery.
Availability of data and materials
All data collected or analyzed during this study are included in this published paper.
References
Nagashima JB, Songsasen N. Canid reproductive biology: norm and unique aspects in strategies and mechanisms. Animals. 2021;11(3):653. https://doi.org/10.3390/ani11030653.
Kustritz MV. The value of canine semen evaluation for practitioners. Theriogenology. 2007;68(3):329–37. https://doi.org/10.1016/j.theriogenology.2007.04.017.
Mihsler-Kirsch L, Wagner H, Failing K, Wehrend A. Downregulation of testicular function in the goat by altrenogest. BMC Vet Res. 2021;17(1):183. https://doi.org/10.1186/s12917-021-02845-6.
Nizanski W, Ochota M, Fontaine C, Pasikowska J. B-Mode and Doppler Ultrasonographic Findings of Prostate Gland and Testes in Dogs Receiving Deslorelin Acetate or Osat0erone Acetate. Animals. 2020;10(6–24):10.
Ortega-Ferrusola C, Gracia-Calvo LA, Ezquerra J, Pena FJ. Use of Colour and Spectral Doppler Ultrasonography in Stallion Andrology. Reprod Domest Anim. 2014;49:88–96. https://doi.org/10.1111/rda.12363.
de Souza MB, Barbosa CC, England G, Mota Filho AC, Sousa C, de Carvalho GG, Silva L. Regional differences of testicular artery blood flow in post pubertal and pre-pubertal dogs. BMC Vet Res. 2015;11:47. https://doi.org/10.1186/s12917-015-0363-3.
Appelbaum L, Gaitini D, Dogra VS. Scrotal ultrasound in adults. Semin Ultrasound CT MR. 2013;34:257–73. https://doi.org/10.1053/j.sult.2013.01.008.
Le MT, Nguyen DN, Tam Nguyen TT, Nguyen VQH, Pham CK, Le D, Cao NT. Should Scrotal Color Doppler Ultrasound Be Routinely Indicated in Fertility Evaluation of Non-Azoospermic Men?Current Urology 2020;14: 4 https://doi.org/10.1159/000499236
Carrillo JD, Soler M, Lucas X, Agut A. Colour and Pulsed Doppler ultrasonographic study of the canine testis. Reprod Domest Anim. 2011;47:655–9. https://doi.org/10.1111/j.1439-0531.2011.01937.x.
Abdelnaby E A, Abd El khalek K G, Emam IA. The beneficial effects of enriched diet on testicular blood flow and seminal parameters using colour and pulsed Doppler ultrasound in dogs. Bulg. J. Vet. Med 2021 (online first), https://doi.org/10.15547/bjvm.2021-0037.
Abdelnaby EA, Abouelela YS, Yasin NAE. Evaluation of penile blood flow in dogs with TVT before and after chemotherapeutic treatment with special reference to its angioarchitecture. Adv Anim Vet Sci. 2021;9(8):1159–68.
El-Sherbiny H, Shahat A, Hedia M, El-Shalofy A. Effect of sexual maturation on testicular morphometry and echotexture and their association with intratesticular blood flow in ossimi rams. Indian Journal of Small Ruminants. 2022;28(1):85–90.
Fadl AM, Abdelnaby EA, El-Sherbiny HR. Supplemental dietary zinc sulfate and folic acid combination improves testicular volume and haemodynamics, testosterone levels and semen quality in rams under heat stress conditions. Reprod Domest Anim. 2022;57(6):567–76. https://doi.org/10.1111/rda.14096 (Epub 2022 Feb 16 PMID: 35147249).
Pozor MA, McDonnell SM. Color Doppler ultrasound evaluation of the testicular blood flow in stallions. Theriogenology. 2004;61:799–810. https://doi.org/10.1016/s0093-691x(03)00227-9.
Ortiz-Rodriguez JM, Anel-Lopez L, Martín-Muñoz P, Álvarez M, Gaitskell-Phillips G, Anel L, Rodríguez-Medina P, Peña FJ, Ortega FC. Pulse Doppler ultrasound as a tool for the diagnosis of chronic testicular dysfunction in stallions. PLoS ONE. 2017;12(5): e0175878. https://doi.org/10.1371/journal.pone.0175878.PMID:28558006;PMCID:PMC5448730.
Zelli R, Troisi A, Elad Ngonput A, Cardinali L, Polisca A. Evaluation of testicular artery blood flow by Doppler ultrasonography as a predictor of spermatogenesis in the dog. Res Vet Sci. 2013;95(2):632–7. https://doi.org/10.1016/j.rvsc.2013.04.023 (Epub 2013 May 25 PMID: 23714041).
Barlas M, Hatiboğlu C. The effect of nitric oxide in testicular ischaemia-reperfusion injury. Int Urol Nephrol. 2002;34(1):81–6. https://doi.org/10.1023/a:1021311029572.
Gur S, Kadowitz PJ, Sikka SC, Peak TC, Hellstrom WJ. Overview of potential molecular targets for hydrogen sulfide: a new strategy for treating erectile dysfunction. Nitric oxide: biology and chemistry/official. J Nitric Ox Soc. 2015;50:65–78. https://doi.org/10.1016/j.niox.2015.08.005.
Ball BA. Diagnostic Methods for Evaluation of Stallion Subfertility: A review. J Equine Vet. 2008;28(11):650–65. https://doi.org/10.1016/j.jevs.2008.10.003.
Reiter RJ, Tan D, Manchester LC, Qi W. Biochemical reactivity of melatonin with reactive oxygen and nitrogen species: a review of the evidence. Cell Biochem Biophys. 2001;34:237–56. https://doi.org/10.1385/CBB:34:2:237.
Reiter RJ, Mayo JK, Tan D, Sainz RM, Alatorre-Jimenez M, Qin L. Melatonin as an antioxidant: under promises but over delivers. J Pineal Res. 2016;61(3):253–78.
Abdelnaby EA. Higher doses of melatonin affect ovarian and middle uterine arteries vascular blood flow and induce oestrus earlier in acyclic ewes. Reprod Domest Anim. 2020;55(7):763–9. https://doi.org/10.1111/rda.13678.
Abdelnaby EA, Abo El-Maaty AM. Melatonin and CIDR improved the follicular and luteal hemodynamics, uterine and ovarian arteries vascular perfusion, ovarian hormones and nitric oxide in cyclic cows. Reprod Domest Anim. 2021;56(3):498–510. https://doi.org/10.1111/rda.13888.
Rodriguez C, Mayo JC, Sainz RM, Antolín I, Herrera F, Martín V, Reiter RJ. Regulation of antioxidant enzymes: a significant role for melatonin. J Pineal Res. 2004;36:1–9. https://doi.org/10.1046/j.1600-079x.2003.00092.x.
Li C, Zhou X. Melatonin and male reproduction. Clin Chim Acta. 2015;446:175–80. https://doi.org/10.1016/j.cca.2015.04.029.
Yu K, Deng SL, Sun TC, Li YY, Liu YX. Melatonin Regulates the Synthesis of Steroid Hormones on Male Reproduction: A Review. Molecules. 2018;23(2):447. https://doi.org/10.3390/molecules23020447.PMID:29462985;PMCID:PMC6017169.
Fathi M, Salama A, El-Shahat KH, EL-Sherbiny HR, Abdelnaby EA. Effect of melatonin supplementation during IVM of dromedary camel oocytes (Camelus dromedarius) on their maturation, fertilization, and developmental rates in vitro, Theriogenology 2021;172: 187–192
Delgadillo JA, Velez LI, Flores JA. Continuous light after a long-day treatment is equivalent to melatonin implants to stimulate testosterone secretion in Alpine male goats. Animal. 2016;10:649–54. https://doi.org/10.1017/S1751731115002177.
Alonge S, Melandri M, Aiudi GG, Lacalandra GM. Advances in prostatic diagnostics in dogs: the role of Canine Prostatic specific esterase in the early diagnosis of Prostatic Disorders. Top Companion Anim Med 2018;33(4):105–8.
Alonge S, Melandri M, Leoci R, Lacalandra GM, Aiudi GG. Ejaculation effect on blood testosterone and prostatic pulsed-wave Doppler ultrasound in dogs. Reprod Domest Anim. 2018;53(2):70–3. https://doi.org/10.1111/rda.13277.
Pan X, Zhu L, Lu H, Wang D, Lu Q, Yan H. Melatonin attenuates oxidative damage induced by Acrylamide In Vitro and In Vivo. Oxid Med Cell Longev. 2015;2015:703–9.
Gulyuz F, Tasal I, Uslu BA. Effects of melatonin on the onset of ovarian activity in Turkish van cats. J Anim Vet Adv. 2009;8:2033–7.
Avery D, Lenz M, Landis C. Guidelines for prescribing melatonin. Ann Med. 1998;30(1):122–30. https://doi.org/10.3109/07853899808999394.
Mickelsen WD, Memon MA, Anderson PB, Freeman DA. The relationship of semen quality to pregnancy rate and litter size following artificial insemination in the bitch. Theriogenology. 1993;39:553–60. https://doi.org/10.1016/0093-691x(93)90397-n.
Freshman JL. Semen collection and evaluation. Clin Tech Small Anim Pract. 2002;17(3):104–7. https://doi.org/10.1053/svms.2002.34326.
El-Sherbiny HR, Abdelnaby EA, Samir H, Fathi M. Addition of autologous platelet rich plasma to semen extender enhances cryotolerance and fertilizing capacity of buffalo bull spermatozoa. Theriogenology. 2022;194:104–9.
Abdelnaby EA, Emam IA. Testicular vascularization at two locations in relation to hormonal levels, and pixel echotexture in bulls at different ages. Asian Pacific Journal of Reproduction. 2022;11(4):193–200.
Daghash SM, Yasin NAE, Abdelnaby EA, Emam I, Tolba A, Abouelela YS. Histological and hemodynamic characterization of corpus luteum throughout the luteal phase in pregnant and non-pregnant buffalos in relation to nitric oxide levels based on its anatomical determination. Front Vet Sci. 2002;9:896581.
Abouelela YS, Yasin NAE, El Karmoty AF, Khattab MA, El-Shahat KH, Abdelnaby EA. Ovarian, uterine and luteal hemodynamic variations between pregnant and non-pregnant pluriparous Egyptian buffalos with special reference to their anatomical and histological features. Theriogenology. 2021;173:173–82. https://doi.org/10.1016/j.theriogenology.2021.06.022,PMID34392170.
Abdelnaby EA, Emam IA, El-Sherbiny HR, Fadl AM. The effects of aging and gestational month on uteroplacental vascular perfusion and umbilical artery hemodynamics in pregnant jennies. BMC Vet Res. 2022. https://doi.org/10.1186/s12917-022-03499-8.
Maher MA, Farghali HAM, Elsayed AH, Emam A, Abdelnaby EA, Reem RT. A potential use of Doppler sonography for evaluating normal hemodynamic values of the hepatic, pancreatic and splenic vessels in domestic rabbits. Adv Anim Vet Sci. 2020;8(5):506e18.
Abdelkhalek KG, Badawy ABA, Abdelnaby EA. Comparison Between Mediastinum Thickness, Hormonal Levels, Nitric Oxide, and Testicular Hemodynamics in Baladi Bucks at Prepubertal and Postpubertal Stages. Journal of Advanced Veterinary Research. 2022;12(3):241–7.
EL-Sherbiny HR, Shahat A, Hedia M, EL-Shalofy AS. Effect of sexual maturation on testicular morphometry and echotexture and their association with intratesticular blood flow in ossimi rams. Indian J Small Rumin. 2022;28:85–90.
Shaul DB, **e HW, Diaz JF, Mahnovski V, Hardy BE. Surgical treatment of testicular trauma: effects on fertility and testicular histology. J Pediatr Surg. 1997;32:84–7.
Sekmenli T, Gunduz M, Öztürk B, Karabağlı P, Ciftci I, Tekin G. The effects of melatonin and colchicine on ischemia-reperfusion injury in experimental rat testicular torsion model. J Pediatr Surg. 2016;52:582–6.
Parlaktas BS, Atilgan D, Ozyurt H, Gencten Y, Akbas A, Erdemir F, et al. The biochemical effects of ischemia-reperfusion injury in the ipsilateral and contralateral testes of rats and the protective role of melatonin. Asian JAndrol. 2014;16:314–8.
Hemadi M, Zargar M, Sobhani A, Sobhani A. Assessment of morphological and functional changes in neonate vitrified testis grafts after host treatment with melatonin. Folia Morphol (Warsz). 2011;70:95–102.
Ghasemi FM, Faghani M, Khajehjahromi S, Bahadori M, Nasiri E, Hemadi M. Effect of melatonin on proliferative activity and apoptosis in spermatogenic cells in mouse under chemotherapy. J Reprod Contracept. 2010;21:79–94.
Soni KK, Zhang LT, You JH, Lee SW, Kim CY, Cui WS, et al. The effects of MOTILIPERM on cisplatin induced testicular toxicity in Sprague-Dawley rats. Cancer Cell Int. 2015;15:121.
Rocha CS, Rato L, Martins AD, Alves M, Oliveira PF. Melatonin and male reproductive health: relevance of darkness and antioxidant properties. Curr Mol Med. 2015;15:1–13.
Ramadan, T.A., Kumar D, Ghuman S.S., Singh I. Melatonin improved buffalo semen quality during nonbreeding season under tropical condition. Domest Anim Endocrinol. 2019;68:119–25.
Kukk AJ. Associations between Canine Male Reproductive Parameters and Serum Vitamin D and Prolactin Concentrations A Thesis presented to The University of Guelph In partial fulfillment of requirements for the degree of Doctor of Veterinary Science, Canada 2011
El-Sherbiny HR, El-Shalofy AS, Samir H. Exogenous L-carnitine administration ameliorates the adverse effects of heat stress on testicular hemodynamics, echotexture, and total antioxidant capacity in Rams. Front Vet Sci. 2022;9: 860771. https://doi.org/10.3389/fvets.2022.860771.
El-Sherbiny HR, Samir H, El-Shalofy AS, Abdelnaby EA. Exogenous L-arginine administration improves uterine vascular perfusion, uteroplacental thickness, steroid concentrations, and nitric oxide levels in pregnant buffaloes under subtropical conditions. Reprod Domest Anim. 2022;00:1–10. https://doi.org/10.1111/rda.14225.
El-Sherbiny HR, Fathi M, Samir H, Abdelnaby EA. Supplemental dietary curcumin improves testicular hemodynamics, testosterone levels, and semen quality in Baladi bucks in the nonbreeding season. Theriogenology. 2022;188:100–7. https://doi.org/10.1016/j.theriogenology.2022.05.02.
Fadl AM, Abdelnaby EA, El-Sherbiny HR. Supplemental dietary zinc sulfate and folic acid combination improves testicular volume and hemodynamics, testosterone levels and semen quality in rams under heat stress conditions. Reprod Domest Anim. 2022;57:567–76. https://doi.org/10.1111/rda.14096.
Abdelnaby EA, Emam IA, Fadl AM. Assessment of the accuracy of testicular dysfunction detection in male donkey (Equus asinus) with the aid of colour-spectral Doppler in relation to plasma testosterone and serum nitric oxide levels. Reprod Domest Anim. 2021;56:764–74. https://doi.org/10.1111/rda.13916.
Abdelnaby EA. Testicular haemodynamics, plasma testosterone and oestradiol concentrations, and serum nitric oxide levels in the Egyptian buffalo bull after a single administration of human chorionic gonadotropin. Reprod Domest Anim. 2022;57(7):754–60.
Abdelnaby EA, Abouelela YS, Yasin NAE. Evaluation of Penile Blood Flow in Dogs With TVT Before and After Chemotherapeutic Treatment With Special Reference to its Angioarchitecture. Advances in Animal and Veterinary Sciences. 2021;9(8):1–10.
El-Sherbiny HR, Abdelnaby EA, El-Shahat KH, Salem NY, Ramadan ES, Yehia SG, Fathi M. Coenzyme Q10 Supplementation enhances testicular volume and hemodynamics, reproductive hormones, sperm quality, and seminal antioxidant capacity in goat bucks under summer hot humid conditions. Vet Res Commun. 2022. https://doi.org/10.1007/s11259-022-09991-8.
Lincoln GA, Clarke LJ. Refractoriness to a static melatonin signal develops in the pituitary gland for the control of prolactin secretion in the ram. Biol Reprod. 1997;57(2):460–46.
Rosa HJD, Juniper DT, Bryant MJ. Effects of recent sexual experience and melatonin treatment of rams on plasma testosterone concentration, sexual behaviour and ability to induce ovulation in seasonally anoestrous ewes. J Reprod Fertil. 2000;120(1):169–76.
Deng SL, Wang ZP, ** C, Kang XL, Batool A, Zhang Y, Li XY, Liu YX. Melatonin promotes sheep Leydig cell testosterone secretion in a co-culture with Sertoli cells. Theriogenology. 2018;106:170–7.
Alvarez-García V, González A, Martínez-Campa C, Alonso-González C, Cos S. Melatonin modulates aromatase activity and expression in endothelial cells. Oncol Rep. 2013;29:2058–64.
Zelli R, Troisi A, Ngonput EA, Cardinali L, Polisca A. Evaluation of testicular artery blood flow by Doppler ultrasonography as a predictor of spermatogenesis in the dog. Res Vet Sci. 2013;95:632–7.
Zarlingo TJ, Eis AL, Brockman DE, Kossenjans W, Myatt L. Comparative localization of endothelial and inducible nitric oxide synthase isoforms in haemochorial and epitheliochorial placentae. Placenta. 1997;18(7):511–20. https://doi.org/10.1016/0143-4004(77)90004-2 (PMID: 9290145).
Abdelnaby E, Yasin N, Abouelela YS, Rashad E, Daghash S, ElSherbiny H. Ovarian, uterine, and luteal vascular perfusions during follicular and luteal phases in the adult cyclic female rabbits with special orientation to their histological detection of hormone receptor. BMC Vet Res. 2022. https://doi.org/10.1186/s12917-022-03390-6.
El-Seadawy IE, Kotp MS, El-Maaty AMA, Fadl AM, El-Sherbiny HR, Abdelnaby EA. The impact of varying doses of moringa leaf methanolic extract supplementation in the cryopreservation media on sperm quality, oxidants, and antioxidant capacity of frozen-thawed ram sperm. Trop Anim Health Prod. 2022;54:344. https://doi.org/10.1007/s11250-022-03344-y.
Kissner R, Nauser T, Bugnon P, Lye PG, Koppenol WH. Formation and properties of peroxynitrite as studied by laser flash photolysis, high-pressure stopped-flow technique, pulse radiolysis. Chem Res Toxicol. 1997;10(11):1285–92. https://doi.org/10.1021/tx970160x.
Acknowledgements
The author’s sincere acknowledgment to technicians in Veterinary Teaching Hospital, Cairo University, for their help during this study.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Methodology, Doppler investigation, statistical analysis, and manuscript writing were all conducted on Elshymaa A. Abdelnaby. Semen collection, animal availability, proposal writing and revision, and document availability were all handled by Ali Salama and Mohamed Fathi. Ibrahim A. Emam was specialized in statistical analysis and methodology. All authors drafted the manuscript, reviewed it, and approved the last version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Faculty of Veterinary Medicine at Cairo University's Ethical Committee for Animal Use accepted all procedures with approval number Vet CU 24112020262.
All methods were carried out in accordance with relevant guidelines and regulations. All methods are reported in accordance with ARRIVE guidelines. Not applicable.
Consent for publication
Not applicable.
Competing of interests
There are no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Salama, A., Abdelnaby, E.A., Emam, I.A. et al. Single melatonin injection enhances the testicular artery hemodynamic, reproductive hormones, and semen parameters in German shepherd dogs. BMC Vet Res 18, 403 (2022). https://doi.org/10.1186/s12917-022-03487-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12917-022-03487-y