Abstract
Acceptability is a key concept used to analyze the introduction of a health innovation in a specific setting. However, there seems to be a lack of clarity in this notion, both conceptually and practically. In low and middle-income countries, programs to support the diffusion of new technological tools are multiplying. They face challenges and difficulties that need to be understood with an in-depth analysis of the acceptability of these innovations. We performed a sco** review to explore the theories, methods and conceptual frameworks that have been used to measure and understand the acceptability of technological health innovations in sub-Saharan Africa. The review confirmed the lack of common definitions, conceptualizations and practical tools addressing the acceptability of health innovations. To synthesize and combine evidence, both theoretically and empirically, we then used the "best fit framework synthesis" method. Based on five conceptual and theoretical frameworks from scientific literature and evidence from 33 empirical studies, we built a conceptual framework in order to understand the acceptability of technological health innovations. This framework comprises 6 determinants (compatibility, social influence, personal emotions, perceived disadvantages, perceived advantages and perceived complexity) and two moderating factors (intervention and context). This knowledge synthesis work has also enabled us to propose a chronology of the different stages of acceptability.
Similar content being viewed by others
Background
Acceptability is a central concept reflecting a crucial process for understanding the effects of interventions in public health. As shown during the Covid-19 pandemic, the various responses to fighting the virus, such as the government measures taken, vaccination, technological tools used, etc., were accepted in varying degrees by the populations [1,2,3,4,5]. It is therefore important to measure and understand the acceptability of health interventions so as to adapt the actions implemented and achieve the health objectives targeted.
More specifically, concerning technological innovations, acceptability is often considered a crucial factor in the process of adoption, abandonment or diffusion of an innovation. Technological innovations historically have shaped the organization and transformation of societies, institutions and practices [6]. In the field of health, they are defined as “the application of organized knowledge and skills in the form of medicines, medical devices, vaccines, procedures and systems developed to solve a health problem and improve quality of life” [7]. To achieve these objectives for improving local and global health and social indicators, health technologies are subject to numerous technical evaluations before their dissemination: safety, ergonomics, effectiveness, checking of the results' validity, etc. However, users are not simply receivers of innovations, they have an active role in the innovation process, they are co-creators through their reaction, appropriation, diverted use, adaptation, etc. [8]. It is therefore also necessary to carry out a social assessment of these innovative health technologies in order to document the multiple factors that can influence their introduction and dissemination [9] and understand the processes that will ultimately lead to their adoption or abandonment. This issue is all the more important in low- and middle-income countries (LMIC) whose contexts often present additional challenges, such as unreliable power, poor internet and mobile signal connectivity, lack of transportation systems, medicine stockouts, lack of financial resources, conflict, health literacy, etc. [10, 11].
We are particularly interested in how to measure and understand the acceptability of an innovation in the context of the AIRE project (Améliorer l’Identification des détresses Respiratoires chez l’Enfant). It aims to introduce pulse oximeters (in the Integrated Management of Childhood Illness guidelines) in primary health centers in four West African countries (Burkina Faso, Guinea, Mali, Niger) to reduce mortality of children under five years old [12]. The pulse oximeter is considered here as a technological innovation in health. Thus, one of the AIRE research objectives is to measure the acceptability of this tool by health professionals and caregivers of children. We wanted to base this research on theories and analytical frameworks, as this is very important for ensuring the quality and rigor of the research [13]. We therefore initiated an informal literature review (with keywords related to theories, models, conceptual frameworks; as well as keywords related to acceptability and innovations), but it did not allow us to find a framework adapted to our study.
Our informal exploration of the literature concerning the concept of acceptability instead highlighted the diversity of terminologies or 'proxies' (acceptability, acceptance, adoption, satisfaction, willingness to use, feasibility, enjoyment, etc.) used to define the same concept, also noted by Bucyibaruta and colleagues [14]. While the criteria for assessing the quality of a concept are clarity (in a given context, the term should have only one meaning) and precision (the possibility of effectively distinguishing the empirical phenomena to which it applies from those to which it does not apply) [15], we found that the concept of acceptability does not meet either of these criteria. This conceptual grey area can create ambiguities regarding what is being measured or analyzed, prevent the development of appropriate data collection methods and tools [16] and make it difficult to make comparisons between studies and accumulate scientific knowledge [17]. Too often, the level of acceptability is measured in a simplistic way (agreement or disagreement with use or participation), without seeking to understand its determinants. However, there is a real distinction to be made between participation and acceptability, as shown in the article by Gooding et al. [18]. In their study, many factors influenced participation or non-participation, and it didn't necessarily match the opinion of the respondents.
Acceptability is a concept that is very complex to understand. It is not a simple binary decision, it is a dynamic process [19], determined by several factors and which varies over space and time [20]. Indeed, the level of acceptability of a health technology can evolve. Nadal et al. [17] also point out that most of the models used to measure acceptability do not take this temporality into account. They propose a "technology acceptance lifecycle" based on the evolution between "pre-use acceptability", "initial use acceptance" and "sustained use acceptance". Other authors, such as Sekhon et al. [21], incorporate a three-stage temporality into their model: prospective, concurrent and retrospective. Greenhalgh et al. [9] also capture this temporal evolution through the "continuous integration and adaptation over time" dimension of their framework.
There is a need to detail and circumscribe this concept to be able to produce a conceptual framework for measuring and understanding the acceptability of health innovations. To do so, it is first necessary to define the objective of this conceptualization, following the idea developed by Perski and Short [19]: “from a public health (as opposed to, for example, a philosophical) perspective, it can be argued that the utility of the concept of intervention acceptability lies in its ability to predict and explain key outcomes of interest”. We can therefore understand acceptability as how an actor reacts to a technological innovation, this reaction mechanism being itself influenced by multiple factors and contributing to determining the use (and/or agreement to use) of this technological innovation in health (without the two concepts of acceptability and use being blended).
The objective of our research is to propose a conceptual framework to help assess and understand the acceptability of technological innovations in health in sub-Saharan Africa.
Methods
Definition of innovation
We adopt the proposition formulated by Rogers [6], stating that “an innovation is an idea, practice, or object that is perceived as new by an individual or other unit of adoption”. However, we have focused on technological innovations (object, software, application, etc.), as we assumed that the acceptability of an idea, process, practice or technology was not necessarily determined by the same factors. Indeed, the literature argues that the acceptability of technological innovation can be influenced by the design [22], the ease of use of the tool [23], the level of technical expertise or any technical problems encountered [24]. We also chose to focus on innovations used in the context of a patient-caregiver interaction, rather than tools or software used only by patients (e.g. self-tests) or only by healthcare professionals (e.g. software designed to improve the organization of work in the health center). We hypothesized that the impact of the tool on the relationship and interactions between patient and provider may influence its acceptability [25]. Regarding the perception of the novelty of an object in relation to the context of its introduction, we adopted an emic point of view [26]. We considered as innovations the technologies that were described as such by the authors of the identified articles.
To be considered an innovation in our study, there are three criteria: |
An innovation is (i) a technological innovation (object, software, application, etc.), (ii) used in the context of a patient-caregiver interaction, and (iii) perceived and described as new in the context of its introduction |
Sco** review methodology
We first carried out a sco** review. We followed the steps proposed by Arksey and O'Malley [27]: (a) identifying the research question; (b) identifying relevant studies; (c) studies selection; (d) charting the data; and (e) summarizing and analyzing the results. We also followed the methodological improvements suggested by the VERDAS consortium (pilot round realization) [28]. The main question guiding our research was: "What theories, methods and conceptual frameworks are used to measure and understand the acceptability of technological innovations in health in sub-Saharan Africa?".
We used the search strategies presented in Appendix 1 to search the databases. Depending on each database, we used specific thesauri if available, and searched for our keywords in the abstracts and titles of articles. We ran our search equations in eight different databases during February 2020: PubMed, Scopus, EBSCOhost (Psychology and Behavioral Sciences Collection, Academic Search Premier, eBook Collection (EBSCOhost), EconLit, PsycArticles, PsychInfo, Business Source Complete), Web of Science, Cochrane (the whole Cochrane Library), Cairn, Opengrey, Scielo. All the collected references were registered in Zotero, which removed the duplicates. We then carried out a two-stage selection: first, we selected the articles based on their title and abstract and then based on their full text. The inclusion criteria were: the article (1) is in English, French or Spanish; (2) focuses on one or more sub-Saharan African country; (3) is about a technological innovation in health (as defined above); (4) its objective (secondary or main) is to study the acceptability of this innovation. The PRISMA flow diagram [29] was used to guide the selection process.
We then analyzed the bibliographies of the studies included in order to find any additional references. Articles that met all the criteria were then analyzed further. We used a checklist to extract the data of interest from each article. The extracted data were the characteristics of the article (authors, journal, year of publication, etc.); the characteristics of the innovation and the conditions of its introduction (country of introduction, type of innovation, target population, etc.); the definition, the theories or frameworks used (definition of acceptability, whether a theory or analytical framework was used, etc.); and finally, the evaluation (type of evaluation, data collection tools, main results, etc.).
Best fit framework synthesis methodology
The sco** review could not identify a conceptual framework or theory (for an explanation of the difference between the two, see: [13]) relevant to our study, given the specificities of the context (sub-Saharan Africa), the field (health) and the type of innovation (see our definition). We therefore decided to use the best fit framework synthesis approach [30, 31] to construct a conceptual framework specific to the acceptability of health innovations. This approach assumes that existing frameworks do not necessarily fully match the subject of interest. However, they are the best that exist to date for producing an initial framework and study themes to be adapted, tested and improved with the empirical data of interest. Therefore, the approach proposes building on one or more existing framework to construct an 'a priori framework'. The best fit framework approach recommends combining several relevant models to provide a more complete basis for analysis, rather than arbitrarily choosing a single framework to serve as an a priori framework [31]. We have therefore based our work on the different frameworks identified through our sco** review [6, 23, 32, 33]. To this, we added two other frameworks not mentioned in the articles included in the sco** review but found during our informal exploration of the literature or through discussion within our team about the frameworks currently used in research to measure the acceptability of innovation [21, 34]. First, we built our a priori framework based on all the themes of the five frameworks identified. As recommended [31], we conducted a thematic analysis of the different dimensions of the five frameworks by identifying the commonalities and differences between the conceptual frameworks and theories and grou** them into themes (Appendix 2). We defined each of these themes to ensure a common understanding of the concepts and to facilitate subsequent coding of data. Then, following an abductive approach (back and forth between theoretical conjectures and empirical data), we confronted the different dimensions of the a priori framework with the empirical data from the articles identified through our sco** review.
The best fit framework method recommends carrying out a double literature review: the first identifies the conceptual frameworks or theories that can feed the formulation of the framework a priori, and the second collects the empirical data that will serve to improve the framework initially constituted [31]. In our case, our sco** review allowed us to identify both conceptual frameworks and empirical data, since our research was focused on the concept of acceptability, without being limited to either frameworks and theories or empirical data. We included protocols only to document the use of frameworks or theories to study acceptability, but then excluded them from further analysis since they do not present empirical data. We had also previously conducted an informal review of the literature to try to identify relevant frameworks or theories.
Empirical data on the subject of interest were therefore extracted from the results sections of the articles selected in our sco** review (excluding protocols). These data were then coded against the constructed themes of the a priori framework with Nvivo12. They were used as a basis for develo**, improving, expanding, reducing or completing the themes of the framework initially built [30, 31]. Indeed, during this comparison between the a priori framework and the new data, the “Relationships between the themes of the framework are then either recreated or generated based on the evidence from the primary research studies included in the review” [31].
Results
What the sco** review tells us about acceptability
We obtained 3426 results from our database search. We finally included 38 articles for analysis (Fig. 1) [32, 33, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70]. Five of the articles were research protocols, while the other 33 presented empirical data. The oldest study was published in 1997, but the majority of studies (over 80%) were published after 2014.
Regarding the geographical distribution of the studies (some studies covered several countries), the country with the most studies is Ghana (n = 5), followed by Kenya, South Africa and Tanzania (n = 4). A map** of the studies included is provided in Fig. 2. The setting in which the innovation under study was introduced was rural in 10 articles, urban or peri-urban in 6, both rural and urban in 13, and undocumented in 9.
We have classified the innovations according to their type, the health problem targeted, the target population, etc. (Appendix 3). The three most targeted health problems are maternal and newborn health (n = 10), malaria (n = 7) and diseases affecting children under five (n = 6).
Theories and conceptual frameworks
Of all the articles included (n = 38) that aimed to assess the acceptability of a health innovation, only seven defined acceptability (all in different ways) (Table 1).
Only five papers used a theory or framework to measure and understand acceptability (Table 2). These were used a priori (to guide data collection) in four articles and a posteriori (to guide data analysis) in one. The notion of acceptability was often assimilated or swapped with other concepts such as perception, satisfaction, adoption, use, willingness to use, etc. Many articles present results relative to the acceptability of a health innovation without even defining precisely what they mean by acceptability and therefore what was being studied. The results of our sco** review confirm the lack of clear theoretical or conceptual definitions and foundations for measuring and empirically understanding the acceptability.
Assessment of acceptability
To measure and understand acceptability, 15 studies used qualitative methods, six used quantitative methods, eight used mixed methods, and for nine articles the method was not specified. The authors documented most often the opinion of health workers (n = 29; some studies had several target populations), followed by those of patients for 21 of the studies. Finally, the acceptability of managers (n = 7), stakeholders in general (n = 4), community members who were not necessarily patients at the time of the study (n = 3), other medical staff (pharmacists, laboratory technicians, etc.) (n = 3), and researchers (n = 1) was also considered. In two studies, the innovation was considered acceptable, but it was not clear for whom this acceptability was assessed. In the majority of articles that presented results, acceptability was described as generally positive.
Chronology of the acceptability study
Theoretical articles on acceptability in the literature distinguish between three main stages in acceptability: before the introduction (or before use) of an innovation, during its introduction (or initial use), and after its introduction (or sustained use) [17, 21]. Based on the included studies, we were able to distinguish, for each of these three phases, two potential sub-phases in the acceptability process (Fig. 3). Depending on the period in which acceptability is studied, the influencing factors will not have the same impact on acceptability. Nevertheless, not all of these times are necessarily experienced for each of the innovations introduced (for example, sometimes the innovation is introduced directly into the care routine, or there is no scaling up).
First, at the “conceptual” time, acceptability is measured after explaining the idea or concept of the innovation, but before its introduction or physical presentation. For example, De Haan and al. [46] measured the acceptability of a tool only after giving the participants an information sheet that explained the device. The second stage, the “tangible” (or concrete) time, is a measure of acceptability after having physically presented the innovation but before it was used and integrated into practices. For example, in a study about a new tool for injecting vaccines, the authors stated: “study staff injected vaccine into oranges to demonstrate CPAD [Compact, prefilled, autodisable device] use, as CPAD is not yet licensed for delivery of pentavalent vaccine in the study countries. […]” [44]. The third stage is the “experimental use”. It is when acceptability is measured while the innovation is being used, but not in the way it should normally be used. For example, Ginsburg et al. [55] explain that “we wanted to ensure the application was not used in the clinical care of the patient and that it did not influence the care of the patient in any way. Therefore, we set the oxygen saturation to read 99 percent at all times”. Then, when the innovation is integrated into the care routines, as it should be used normally, it is the time of "routine use". This is the case of a study conducted in Ghana where the acceptability of malaria rapid diagnostic tests (RDTs) was measured after their introduction into care routines [35]. We have identified a fifth time, the time of "sustained use". There, acceptability is measured when the innovation is integrated into care routines during an intervention, but the support and implementation phases are over. For example, Jensen et al. [38] show differences in responses to acceptability questionnaires that were administered before and at the end of the implementation of the intervention. Finally, the last moment of measurement is the time of “scaling up”, when the innovation is diffused beyond its initial place of introduction. The article by Ansbro et al. [32], for example, shows a relative drop in acceptability after the scaling up of a syphilis point-of-care test: “93.8% of pilot HCWs [health care workers] (15/16) and 62.5% of rollout HCWs (15/24) thought patients were somewhat or very accepting of the RST [rapid syphilis test]”. In the context of a scale-up, we can see both the effect of time (evolution between the different phases of the intervention until scale-up) and of the characteristics of the intervention (who implements the intervention and how) on the acceptability of the technology.
Building a new framework with the best fit framework synthesis
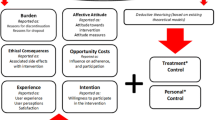
Based on the results of the sco** review, we followed the methodology of the best fit framework synthesis presented earlier [30, 31] in order to build a new framework. We drew on five conceptual frameworks and theories of acceptability [6, 21, 23, 32,33,34] and began by building an "a priori framework" (Fig. 4). It comprises seven dimensions: perceived complexity, social influence, compatibility, perceived advantages, perceived disadvantages, personal emotions and context. The last theme, 'context’, was supported by only one of the frameworks [32]. This shows the lack of attention to and conceptualization of contextual elements [17], although they are often described as fundamental to understanding acceptability [14].
We then compared the a priori framework to the empirical data of the articles included in our sco** review [30, 31], excluding protocols without empirical results (n = 5) so the remainder of the article is based on the analysis of 33 articles. This comparison validated the dimensions of the a priori framework. We found the perceived complexity dimension in 22 out of 33 articles, perceived disadvantages in 23, personal emotions in 21, social influence in 7, perceived advantages in 28 and compatibility in 8. The empirical data also allowed us to redefine the influence of the context dimension and add a dimension related to the intervention.
While in the a priori framework, the context was considered as one of the seven dimensions capable of influencing acceptability directly, the evidence from the empirical studies suggested that context should be understood as a set of elements that can influence each of the other six determinants of acceptability. We also added another specific dimension of influence linked to the intervention itself. Indeed, how the intervention introducing an innovation was designed, implemented, evaluated, and by whom, may influence the acceptability of that technology. For example, an intervention based on randomization between participants may not be accepted (it may result in a refusal to participate), not necessarily because the treatment itself is not accepted but because the form of evaluation is not [19, 77]. Similarly, whether the innovation is introduced by a non-governmental organization or through state support, for example, influences the form of the intervention and may influence the level of acceptability. We found evidence to support these arguments in the studies, as we will see in the next section.
The empirical data also helped us to identify the type of relationship between the different dimensions and acceptability. Indeed, our conceptual framework is built to highlight causal links between influencing variables and the level of acceptability. We constructed the relationships between acceptability and the six dimensions as "a moderated causal relationship" [78]. The strength and outcome of this relationship (positive, neutral or negative influence) will be moderated by the context and the form of the intervention, considered here as "moderators" or "mediating variables" [78]. The specific link between context and interventions has been little studied in the literature. Nevertheless, on the basis of a few articles [79, 80], we concluded that this link is more of a bidirectional causal relationship [78] since the two variables can influence each other. Indeed, the activities of the intervention will take place in a particular context to which they will have to adapt constantly, and the context itself will evolve following the implementation of the program activities [81, 82]. Thus, starting with the five existing frameworks, then modifying the link between context and other elements and adding the impact of the form of the intervention on the acceptability of the technology, we ended up with the new framework presented in Fig. 5. We will now give more details on each of the dimensions of the framework.
Perceived complexity
We defined perceived complexity as the degree to which an innovation and the behavior(s) required to use it are perceived as difficult to understand and to use/perform. In several articles, we found that health workers thought that: "the technology was very easy or easy to use, all mentioning the limited training required to be able to use the device" [49]. The perceived ease of use has a positive impact on the acceptability of the technology. On the contrary, in other studies, some health workers perceived difficulties in using the innovation: "they did not always act on the lights because they were confused. They felt that the yellow light was reported too frequently when patients appeared well” [45]. Here, experience plays an important role in relation to perceived complexity, highlighting the importance of documenting the timing of the acceptability study, as noted earlier: "HCPs [health care providers] struggled to identify how to change their answer selections but were later able to self-correct with practice" [55].
It is also important to compare the perceived understanding with the actual understanding of the technology. For example, the malaria RDT was considered by the patients as "a generic test able to identify any cause of illness, not just malaria, and expectations that a test should result in a diagnosis, even following a negative result" [35]. Another article points out that some patients wanted to receive antimalarials despite a negative RDT result [33]. Here, healthcare professionals may be pressured by patients to obtain a diagnosis or treatment that technology alone cannot provide. Thus, a poor understanding of the technology, even if not necessarily perceived (respondents thought they understood the innovation), can negatively influence the acceptability of the innovation.
Perceived disadvantages
Perceived disadvantages are the amount of effort, risk and cost perceived to be associated with an innovation and its use. These disadvantages can be very diverse, such as increased clinical costs per febrile illness episode [46], painfulness [48], concerns about the safety and hygiene of the device [50], increased administrative constraints [53], increased workload [55], etc. All these disadvantages are distinct from the complications linked to the complexity of using the innovation (perceived complexity). They are the potentially harmful effects caused by the use of the innovation and its integration into routines, and influence the acceptability of the technology negatively. On the contrary, the perception that the use of the innovation will cause very few difficulties and complications for users and beneficiaries can influence acceptability positively.
Personal emotions
We define this dimension as the emotions an individual feels about an innovation and its use. Some articles have reported the "enthusiasm" of health workers using the new tool [33] or the "enjoyment" of patients participating in a consultation using the technology [47]. Regarding the introduction of a new diagnostic test, while 90% of participants reported that "they valued or appreciated the rapid test", among those who refused the technology, "the more common reasons for refusing the skin snip biopsy were that they 'did not like the idea'." [48]. This clearly shows the influence of personal feelings on acceptability. The technology can provide a "sense of relief" [49], can be judged "likeable" [50], or a "satisfying experience" [53]. Patients may be enthusiastic about the use of new technologies in health care: "when you use it on the child, the mother becomes excited. She sees that we are doing something new on the child and for her it means the facility is improving" [54]. On the contrary, some may feel fear, related to the pain that the tool could cause [33], or to the fear that the tool will be used for purposes other than those announced [69]. It may also upset the patients' certainties: "the RDT results challenged the patient's medical knowledge and brought into question their (presumed) control over their family's health" [62]. Depending on how people feel about the technology, this can have a positive or negative impact on acceptability.
Social influence
We defined social influence as the extent to which other people's opinions influence one's degree of acceptability. This dimension took several forms in the empirical data of the articles. From the patients' point of view, the influence exerted by health workers, by their status, was noted: "many respondents conveyed their role as a passive recipient of care, entrusting the clinician with the responsibility to know and prescribe what was 'right' for them. The enactment of this role, coupled with expectations of clinical authority, meant clinical decisions should not be questioned by the patient" [35]. The influence of health authority support was also sometimes highlighted as a positive influence, in contrast to technology manufacturers’ discourse: "Governmental endorsement […] was deemed crucial to acceptability. Congolese practitioners would not perceive evidence provided by other parties, such as manufacturers, as reliable" [46]. Peer influence also plays a role: "Some health workers are not regularly using the CDSS [clinical decision support system] during patient care, which demoralizes other providers who are using the system" [60]. Thus, the opinion of certain key individuals can have both a positive and negative influence on the acceptability of the technology. This influence depends on the opinion of these individuals or institutions on the technology, but also on the importance given to this opinion by the people whose acceptability is being measured.
Perceived advantages
Perceived advantages are the extent to which an innovation is perceived as bringing benefits. This is one of the dimensions most commonly found in the results of the studies included in the sco** review. Some of the perceived advantages include the improved diagnostic capacity and prescription of the right treatment [35], improved patient confidence in health workers [33], reduced consultation time [42], simplification of medical procedures [54], the reduction of unnecessary drug prescriptions [69], etc. All these benefits associated with the introduction of the new technology positively influence its acceptability and encourage its use and integration.
However, sometimes the new technology may seem to offer comparatively fewer benefits than what was previously used, which may have a negative impact on its acceptability. For example, some health workers pointed out that the RDTs for malaria (not able to quantify malaria parasites) were less accurate than the laboratory tests used in the past [33].
Compatibility
Compatibility is the extent to which an innovation is perceived as being consistent with the existing values, past experiences and needs of potential adopters. This dimension is, therefore, necessarily linked directly to the context. In some studies, the influence of the adequacy between the technology introduced and the setting of its introduction has indeed been highlighted: "the device is considered to have limited compatibility with equipment and competences of Congolese practitioners, especially of those active in rural settings" [46]. Here, the lack of compatibility between the technology introduced and the skills and case management possibilities influence the acceptability of the innovation negatively. Other elements may have an effect, such as its compatibility with the existing work organization in the health center. As pointed out in the article by Jensen et al. [38], in their case, the technology integrates well with the existing system: "eIMCI (electronic Integrated Management of Childhood Illness) was easy to accommodate within the daily staff allocation and clinic workflow". Compatibility can also be related to the perception of the tool itself: "Some of these interviewees said that needle length standards are defined for children of high-income countries" [37], or the adequacy with local values and customs, as underlined by this example of a technology using a blood test: " 'I need my husband to allow me to give the child's blood for testing.' […] 'my religion does not permit us to give blood.'" [33]. However, while this compatibility is a dimension that seems to be of important consideration, we found little referring to it in the articles.
Context
We described the ‘context’ dimension as how the contextual environment (organizational, political, economic, social, etc.) influences the degree of acceptability of an innovation. While there was little mention of this dimension in the frameworks used to shape the a priori framework, we found many elements about it in the articles. As explained, we have included the context as a dimension that can impact the influence that each of the factors described above has on acceptability. For example, in a context where the health centers are highly attended, health workers "often noted that once the facility reached around 4 clients per SBA [skilled birth attendants], timely data entry was difficult", thus fueling the perceived disadvantages associated with the system [43]. Similarly, shortages of medicines and medical equipment [60], poor access to electricity in health centers [54], unclear national guidelines [33], or other elements related to the context can also feed the dimension on perceived disadvantages (respectively: impossibility of following the prescription recommendations provided by the innovation; difficulty in charging the device battery; confusion about procedures to follow, etc.).
Another element of the context that can influence acceptability, in particular via the "perceived complexity" dimension, is the level of familiarity with this type of technology or technologies in general. One article notes that the fact that point-of-care tests are regularly performed in health centers was positive because "All health workers agreed that the rapid test was easy to use due to the similarity with the HIV testing" [53]. Similarly, health workers who are familiar with mobile technologies may find a mobile application easier to use than others: "HCPs who did own an android phone demonstrated the ability to move through the application relatively quickly" [55]. On the contrary, unfamiliarity with technologies can have a negative influence, at least at the beginning: "Most HCPs were unfamiliar with touch-screen technology and thus were initially hesitant to use the device" [55].
Regarding perceived advantages, one study explains that in a setting where there is a "shortage of ophthalmic workforce", the new technology could help to overcome this lack of available staff by enabling task shifting and better human resource management [39].
Context can thus influence acceptability through all dimensions. These different examples clearly show the importance of studying the context in which the innovation is introduced and documenting the effects of the context on each of the determinants of acceptability.
Intervention
Elements from the articles also led us to add the ‘intervention’ dimension (how an innovation is introduced) in our framework. Indeed, it is important to document and take into account how the intervention was designed, implemented, evaluated and by whom, as this can influence the acceptability of the innovation introduced. As previously discussed, this influence is also directly related to the context [81, 82].
For example, the type of person designated to use the innovation and the place where it is recommended to be used can influence its acceptability: "Using MAP [microarray patch] during outreach activities at fixed posts was also well anticipated by the majority of participants (average of 87.7%) […]. Using MAP at home during outreach strategies was perceived more cautiously (average of 60.2%)" [44]. Other elements related to the form of intervention, such as the role played by the monitoring team and the emphasis placed on the quality assurance program throughout the study [48], whether the intervention was included in a grant program [46], how the technology training was carried out and by whom [32], the quality of the instructions given both to health workers [54] and patients [54] before using the technology, the level of supervision of the intervention [53], etc., can all influence acceptability.
Therefore, how the intervention was shaped and implemented can influence acceptability both positively and negatively. It is suggested, however, that the high level of involvement of both health workers and the local population in the design and management of the program can enhance its acceptability: "They suggested that training the local population to run the program will overcome any potential obstacles related to acceptability and sustainability. Patients saw the importance of community participation as key to building trust and confidence in the program and put the population at ease" [39].
Discussion
To our knowledge, this study is the first to propose a conceptual framework for studying the acceptability of health innovations in sub-Saharan Africa. To date, the existing literature has emphasized the lack of definition and conceptualization of acceptability [16, 83]. We chose to understand acceptability as a concept made up of multiple dimensions, which help to understand or predict the implementation (if acceptable) or, on the contrary, the de-implementation (if not acceptable) [84] of a health innovation. We believe that our research could help guide researchers, practitioners or anyone who wish to understand the acceptability of an innovation. Our study provides both a timeline of the different times of acceptability, but also a conceptual framework on which different data collection tools, both quantitative and qualitative, can be based in order to document the complex processes of acceptability. Our aim was to provide practical ways of evaluating and understanding acceptability and not merely to think about how to conceptualize this mechanism.
One element that we have not yet addressed, but which seems important to discuss, is the scope of relevance of the framework for the different types of respondents: is there a difference between the factors determining the acceptability of patients and health professionals? In the literature on acceptability, there is often a focus on patients’ acceptability and not on health workers’ acceptability [14], as acceptability is often understood as one of the dimensions of access to care from the patient’s perspective [85, 86]. However, in our study, most technological innovations are used by health workers, so we noticed a reverse trend. It was more often the users of the innovation, i.e. the health workers, who were interviewed. The impact of the different dimensions on acceptability could vary depending on whether the respondent is a health worker using the tool or a patient on or for whom the tool is used. For example, it is more common to measure acceptability in patients through emotional components (in this paper personal emotions), whereas, for health professionals, acceptability is more often understood through more cognitive and technical dimensions (perceived advantages and perceived complexity) [87]. However, the frameworks mobilized and the empirical data from the articles allowed us to hypothesize that, although the strength of their impact on the degree of acceptability may vary, the dimensions of influence that constitute the framework appear to be similar. We believe that the framework can and should therefore be used for all categories of respondent that are directly related to the use of the tool, but it is necessary to confirm this and to study the differences in the influence of the dimensions on acceptability according to the categories of respondent.
Secondly, it might be worthwhile discussing the effect of innovation type on acceptability. In particular, the degree of novelty of the innovation compared to the existing ones, e.g. whether the innovation is radical (fundamental change to the existing) or incremental (minor improvements) [88] can influence its acceptability. For example, an incremental innovation may be perceived as less complex and less risky than a radical innovation (low perceived complexity and perceived disadvantages), but also as offering fewer advantages compared to the previous system (low perceived advantages). Moreover, in the health field, innovations are often linked to scientific advances in clinical or fundamental research. They are, therefore, introduced with the idea that they will necessarily bring added value to the health of populations and their use is therefore often "imposed" on health workers and patients via a top-down approach [89]. All these elements related to the type of innovation studied can influence acceptability and would be useful to study through our framework. Furthermore, in this work, we have focused our research on the empirical data regarding a certain type of innovation (used within the patient-health worker relationship, technological innovations, etc.). It would be advantageous to see if this framework could potentially be extended or adapted to other types of innovation (used by patients or doctors for themselves, social innovations, etc.).
When constructing our framework, since it was initially developed with the aim of collecting empirical data in the context of a West African project, it seemed important to draw on a wide range of theoretical and empirical elements and not only data from high-income countries. It was important to try to avoid ethnocentric bias in implementation studies [90] and a "one-way transfer" of theories, frameworks and experiences from the North to the South [91, 92]. However, none of the frameworks found in the existing literature were initially built specifically on data from LMIC. Consequently, we sought to mobilize empirical research on this topic in sub-Saharan Africa in order to improve existing frameworks. We therefore consider that our framework has benefited from inputs from very different backgrounds and should now be tested to check its suitability in several contexts.
Finally, our study has some limitations. As our sco** review pointed out, acceptability was not necessarily comprehensively and thoroughly understood in most articles. It was sometimes only analyzed as a secondary objective of the research and was often not based on any definition or framework. Thus, the empirical data used to validate and develop the a priori framework may have been limited. For example, other dimensions influencing acceptability, or other links between the different themes, may have been missing from both the conceptual frameworks used for the a priori framework and the empirical data. However, we believe that basing our a priori framework on several different frameworks may have resulted in a robust a priori framework, which may explain its high consistency with the evidence found in the empirical data. In addition, as with all types of systematic reviews, we had to make choices with regard to the databases and keywords used. This may have limited the breadth of empirical data from which we worked on our conceptual framework. It is necessary, therefore, to continue to generate new theoretical perspectives, using the abductive approach that we have initiated here. One of the next steps in this research may also be to consider the construction of indicators and scores out of the different dimensions of this framework. This would allow the development of a ranking and provide a means of measuring acceptability.
Conclusion
Research on the acceptability of health innovations has lacked the guidance and framing needed to conduct rigorous work, allowing for comparisons and the accumulation of knowledge. Our work on the concept of acceptability, through an abductive approach of confronting frameworks and theories with empirical data, has allowed us to propose a consolidated conceptual framework to support the measurement and understanding of the acceptability of health innovations in sub-Saharan Africa.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- AIRE:
-
Améliorer l’Identification des Détresses Respiratoires chez l’Enfant
- CDSS:
-
Clinical Decision Support System
- CFIR:
-
Consolidated Framework for Implementation Research
- CPAD:
-
Compact, Prefilled, Autodisable Device
- eIMCI:
-
Electronic Integrated Management of Childhood Illness
- HCP:
-
Health Care Provider
- HCW:
-
Health Care Worker
- HAS:
-
Health Surveillance Assistant
- LMIC:
-
Low- and Middle Income Countries
- MAP:
-
Microarray Patch
- RDT:
-
Rapid Diagnostic Test
- RST:
-
Rapid Syphilis Test
- SBA:
-
Skilled Birth Attendant
- TAM:
-
Technology Acceptance Model
References
Altmann S, Milsom L, Zillessen H, Blasone R, Gerdon F, Bach R, et al. Acceptability of App-Based Contact Tracing for COVID-19: Cross-Country Survey Study. JMIR Mhealth Uhealth. 2020;8:e19857.
De Coninck D, d’Haenens L, Matthijs K. Perceived vulnerability to disease and attitudes towards public health measures: COVID-19 in Flanders. Belgium Pers Individ Dif. 2020;166:110220.
Guillon M, Kergall P. Attitudes and opinions on quarantine and support for a contact-tracing application in France during the COVID-19 outbreak. Public Health. 2020;188:21–31.
Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38:6500–7.
Ridde V, Kane B, Gaye I, Ba MF, Diallo A, Bonnet E, et al. Acceptability of government measures against COVID-19 pandemic in Senegal: A mixed methods study. PLOS Global Public Health. 2022;2: e0000041.
Rogers E. Diffusion of innovation. 1995.
World Health Assembly. Sixtieth World Health Assembly—Health Technologies. 2007.
Barnier F, Chekkar R. De l’utilité de l’évaluation de l’acceptabilité des innovations technologiques transformant les contextes professionnels du soin : le cas des technologies de domotique. Innovations. 2021;N° 66:203–34.
Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19:e367.
Leonard E, de Kock I, Bam W. Barriers and facilitators to implementing evidence-based health innovations in low- and middle-income countries: a systematic literature review. Eval Program Plann. 2020;82: 101832.
Ritchie LMP, Khan S, Moore JE, Timmings C, van Lettow M, Vogel JP, et al. Low- and middle-income countries face many common barriers to implementation of maternal health evidence products. J Clin Epidemiol. 2016;76:229–37.
Hedible GB, Louart S, Neboua D, Catala L, Anago G, Sawadogo A-G, et al. Evaluation of the routine implementation of pulse oximeters into integrated management of childhood illness (IMCI) guidelines at primary health care level in West Africa: the AIRE mixed-methods research protocol. BMC Health Serv Res. 2022;22:1579.
Ridde V, Pérez D, Robert E. Using implementation science theories and frameworks in global health. BMJ Glob Health. 2020;5:e002269.
BJ Bucyibaruta, D Peu, L Bamford, A van der Wath. Closing the gaps in defining and conceptualising acceptability of healthcare: a synthesis review and thematic content analysis. preprint. In: Review. 2020.
Daigneault P-M, Jacob S. Les concepts souffrent-ils de négligence bénigne en sciences sociales? Eléments d’analyse conceptuelle et examen exploratoire de la littérature francophone à caractère méthodologique. Soc Sci Inf. 2012;51:188–204.
Nadal C, Sas C, Doherty G. Technology acceptability, acceptance and adoption - definitions and measurement. 2019. p. 6.
Nadal C, Sas C, Doherty G. Technology acceptance in mobile health: sco** review of definitions, models, and measurement. J Med Internet Res. 2020;22:e17256.
Gooding K, Phiri M, Peterson I, Parker M, Desmond N. Six dimensions of research trial acceptability: how much, what, when, in what circumstances, to whom and why? Soc Sci Med. 2018;213:190–8.
Perski O, Short CE. Acceptability of digital health interventions: embracing the complexity. Transl Behav Med. 2021. https://doi.org/10.1093/tbm/ibab048.
Koelle M, Boll S, Olsson T, Williamson J, Profita H, Kane S, et al. (Un)Acceptable!?! Re-thinking the Social Acceptability of Emerging Technologies. In: Extended Abstracts of the 2018 CHI Conference on Human Factors in Computing Systems. New York: Association for Computing Machinery; 2018. p. 1–8.
Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17:88.
Bichard J-A, Coleman R, Coleman R. Does My Stigma Look Big in This? Considering Acceptability and Desirability in the Inclusive Design of Technology Products. In: Stephanidis C, editor. Universal Acess in Human Computer Interaction. Co** with Diversity. Berlin, Heidelberg: Springer Berlin Heidelberg; 2007. p. 622–31.
Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci. 2000;46:186–204.
Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: a systematic review. J Med Internet Res. 2016;18:e121.
Safi S, Thiessen T, Schmailzl KJ. Acceptance and resistance of new digital technologies in medicine: qualitative study. JMIR Res Protoc. 2018;7:e11072.
Pike KL. Etic and Emic Standpoints for the Description of Behavior. In: Hildum DC, editor. Language and Thought: An Enduring Problem in Psychology. London: : Van Nostrand; 1967. p. 32–9.
Arksey H, O’Malley L. Sco** studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Degroote S, Bermudez-Tamayo C, Ridde V. Approach to identifying research gaps on vector-borne and other infectious diseases of poverty in urban settings: sco** review protocol from the VERDAS consortium and reflections on the project’s implementation. Infect Dis Poverty. 2018;7.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Carroll C, Booth A, Cooper K. A worked example of “best fit” framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol. 2011;11:29.
Carroll C, Booth A, Leaviss J, Rick J. “Best fit” framework synthesis: refining the method. BMC Med Res Methodol. 2013;13:37.
Ansbro ÉM, Gill MM, Reynolds J, Shelley KD, Strasser S, Sripipatana T, et al. Introduction of Syphilis Point-of-Care Tests, from Pilot Study to National Programme Implementation in Zambia: A Qualitative Study of Healthcare Workers’ Perspectives on Testing Training and Quality Assurance. PLoS One. 2015;10:e0127728.
Asiimwe C, Kyabayinze DJ, Kyalisiima Z, Nabakooza J, Bajabaite M, Counihan H, et al. Early experiences on the feasibility, acceptability, and use of malaria rapid diagnostic tests at peripheral health centres in Uganda-insights into some barriers and facilitators. Implement Sci. 2012;7:5.
Huijts NMA, Molin EJE, Steg L. Psychological factors influencing sustainable energy technology acceptance: a review-based comprehensive framework. Renew Sust Energ Rev. 2012;16(1):525–31. https://doi.org/10.1016/j.rser.2011.08.018.
Ansah EK, Reynolds J, Akanpigbiam S, Whitty CJM, Chandler CIR. “Even if the test result is negative, they should be able to tell us what is wrong with us”: a qualitative study of patient expectations of rapid diagnostic tests for malaria. Malar J. 2013;12:258.
Blanchet K, Lewis JJ, Pozo-Martin F, Satouro A, Somda S, Ilboudo P, et al. A mixed methods protocol to evaluate the effect and cost-effectiveness of an Integrated electronic Diagnosis Approach (IeDA) for the management of childhood illnesses at primary health facilities in Burkina Faso. Implement Sci. 2016;11:111.
Guillermet E, Dicko HM, Mai LTP, N’Diaye M, Hane F, Ba SO, et al. Acceptability and feasibility of delivering pentavalent vaccines in a compact, prefilled, autodisable device in Vietnam and Senegal. PLoS One. 2015;10:e0132292.
Jensen C, McKerrow NH, Wills G. Acceptability and uptake of an electronic decision-making tool to support the implementation of IMCI in primary healthcare facilities in KwaZulu-Natal, South Africa. Paediatr Int Child Health. 2020;40(4):215–26. https://doi.org/10.1080/20469047.2019.1697573.
Lodhia V, Karanja S, Lees S, Bastawrous A. Acceptability, usability, and views on deployment of peek, a mobile phone mhealth intervention for eye care in kenya: qualitative study. JMIR Mhealth Uhealth. 2016;4:e30.
Lawn J, Wyatt J, Woods D, Bezuidenhout H. Are you blue yet? Develo** low cost, alternative powered pulse oximetry for ill babies and children. The 4th Institution of Engineering and Technology Seminar on Appropriate Healthcare Technologies for Develo** Countries. London; 2006. p. 83–8.
Bezuidenhout H, Woods D, Wyatt J, Lawn J. Does fetal heart rate count? Develo** a low cost, alternative powered Doppler fetal heart monitor for use in low resource high mortality settings. 4th IET Seminar on Appropriate Healthcare Technologies for Develo** Countries; 2006. p. 155–9.
Migowa AN, Macharia WM, Samia P, Tole J, Keter AK. Effect of a voice recognition system on pediatric outpatient medication errors at a tertiary healthcare facility in Kenya. Ther Adv Drug Saf. 2018;9:499–508.
Sanghvi H, Mohan D, Litwin L, Bazant E, Gomez P, MacDowell T, et al. Effectiveness of an electronic partogram: a mixed-method, quasi-experimental study among skilled birth attendants in Kenya. Glob Health Sci Pract. 2019;7:521–39.
Guillermet E, Alfa DA, Phuong Mai LT, Subedi M, Demolis R, Giersing B, et al. End-user acceptability study of the nanopatch™; a microarray patch (MAP) for child immunization in low and middle-income countries. Vaccine. 2019;37:4435–43.
Vousden N, Lawley E, Nathan HL, Seed PT, Brown A, Muchengwa T, et al. Evaluation of a novel vital sign device to reduce maternal mortality and morbidity in low-resource settings: a mixed method feasibility study for the CRADLE-3 trial. BMC Pregnancy Childbirth. 2018;18:115.
de Haan F, Onyamboko MA, Fanello CI, Woodrow CJ, Lubell Y, Boon WPC, et al. Exploring health practitioners’ acceptability of a prospective semi-quantitative pfHRP2 device to define severe malaria in the Democratic Republic of Congo. Malar J. 2015;14:503.
Forssman L, Ashorn P, Ashorn U, Maleta K, Matchado A, Kortekangas E, et al. Eye-tracking-based assessment of cognitive function in low-resource settings. Arch Dis Child. 2017;102:301–2.
Dieye Y, Storey HL, Barrett KL, Gerth-Guyette E, Di Giorgio L, Golden A, et al. Feasibility of utilizing the SD BIOLINE Onchocerciasis IgG4 rapid test in onchocerciasis surveillance in Senegal. PLoS Negl Trop Dis. 2017;11(10):e0005884. https://doi.org/10.1371/journal.pntd.0005884.
Dunning L, Kroon M, Hsiao N-Y, Myer L. Field evaluation of HIV point-of-care testing for early infant diagnosis in Cape Town South Africa. PLoS One. 2017;12:e0189226.
Mugyenyi GR, Atukunda EC, Ngonzi J, Boatin A, Wylie BJ, Haberer JE. Functionality and acceptability of a wireless fetal heart rate monitoring device in term pregnant women in rural Southwestern Uganda. BMC Pregnancy Childbirth. 2017;17:178.
Liu J, Modrek S, Anyanti J, Nwokolo E, De La Cruz A, Schatzkin E, et al. How do risk preferences relate to malaria care-seeking behavior and the acceptability of a new health technology in Nigeria? BMC Health Serv Res. 2014;14:374.
De Schacht C, Lucas C, Sitoe N, Machekano R, Chongo P, Temmerman M, et al. Implementation of point-of-care diagnostics leads to variable uptake of Syphilis, Anemia and CD4+ T-cell count testing in rural maternal and Child Health Clinics. PLoS One. 2015;10: e0135744.
Bocoum FY, Tarnagda G, Bationo F, et al. Introducing onsite antenatal syphilis screening in Burkina Faso: implementation and evaluation of a feasibility intervention tailored to a local context. BMC Health Serv Res. 2017;17:378. https://doi.org/10.1186/s12913-017-2325-x.
Ginsburg AS, Tawiah Agyemang C, Ambler G, Delarosa J, Brunette W, Levari S, et al. mPneumonia, an innovation for diagnosing and treating childhood pneumonia in low-resource settings: a feasibility, usability and acceptability study in Ghana. PLoS ONE. 2016;11:e0165201.
Ginsburg AS, Delarosa J, Brunette W, Levari S, Sundt M, Larson C, et al. mPneumonia: development of an innovative mhealth application for diagnosing and treating childhood pneumonia and other childhood illnesses in low-resource settings. PLoS One. 2015;10:e0139625.
Lenahan JL, Volpicelli G, Lamorte A, Jehan F, Bassat Q, Ginsburg AS. Multicentre pilot study evaluation of lung ultrasound for the management of paediatric pneumonia in low-resource settings: a study protocol. BMJ Open Respir Res. 2018;5:e000340.
Ide N, Hardy V, Chirambo G, Heavin C, O’Connor Y, O’Donoghue J, et al. People welcomed this innovation with two hands: a qualitative report of an mHealth intervention for community case management in Malawi. Ann Glob Health. 2019;85(1):61. https://doi.org/10.5334/aogh.919.
Baker K, Akasiima M, Wharton-Smith A, Habte T, Matata L, Nanyumba D, et al. Performance, acceptability, and usability of respiratory rate timers and pulse oximeters when used by frontline health workers to detect symptoms of pneumonia in sub-saharan Africa and Southeast Asia: protocol for a two-phase, multisite. Mixed-Methods Trial JMIR Res Protoc. 2018;7:e10191.
Nwegbu MM, Isa HA, Nwankwo BB, Okeke CC, Edet-Offong UJ, Akinola NO, et al. Preliminary Evaluation of a Point-of-Care Testing Device (SickleSCAN™) in screening for sickle cell disease. Hemoglobin. 2017;41:77–82.
Sukums F, Mensah N, Mpembeni R, Massawe S, Duysburgh E, Williams A, et al. Promising adoption of an electronic clinical decision support system for antenatal and intrapartum care in rural primary healthcare facilities in sub-Saharan Africa: The QUALMAT experience. Int J Med Inform. 2015;84:647–57.
Duysburgh E, Temmerman M, Yé M, Williams A, Massawe S, Williams J, et al. Quality of antenatal and childbirth care in rural health facilities in Burkina Faso, Ghana and Tanzania: an intervention study. Trop Med Int Health. 2016;21:70–83.
Sequeira AR. The introduction of rapid diagnostic test for malaria in Mozambique: local appropriation and complementary therapeutics. Australas Rev Afr Stud. 2015;36:114–28.
Crehan C, Kesler E, Nambiar B, Dube Q, Lufesi N, Giaccone M, et al. The NeoTree application: develo** an integrated mHealth solution to improve quality of newborn care and survival in a district hospital in Malawi. BMJ Glob Health. 2019;4:e000860.
Meloni ST, Agbaji O, Chang CA, Agaba P, Imade G, Oguche S, et al. The role of point-of-care viral load monitoring in achieving the target of 90% suppression in HIV-infected patients in Nigeria: study protocol for a randomized controlled trial. BMC Infect Dis. 2019;19:368.
Mharakurwa S, Manyame B, Shiff CJ. Trial of the ParaSight-F test for malaria diagnosis in the primary health care system. Zimbabwe Trop Med Int Health. 1997;2:544–50.
Benski AC, Stancanelli G, Scaringella S, Herinainasolo JL, **oro J, Vassilakos P, et al. Usability and feasibility of a mobile health system to provide comprehensive antenatal care in low-income countries: PANDA mHealth pilot study in Madagascar. J Telemed Telecare. 2017;23:536–43.
Litwin LE, Maly C, Khamis AR, Hiner C, Zoungrana J, Mohamed K, et al. Use of an electronic Partograph: feasibility and acceptability study in Zanzibar Tanzania. BMC Pregnancy Childbirth. 2018;18:147.
Tadesse Y, Gelagay AA, Tilahun B, Endehabtu BF, Mekonnen ZA, Gashu KD. Willingness to use mobile based e-partograph and associated factors among care providers in North Gondar Zone, Northwest Ethiopia. Online J Public Health Inform. 2019;11: e10.
Williams HA, Causer L, Metta E, Malila A, O’Reilly T, Abdulla S, et al. Dispensary level pilot implementation of rapid diagnostic tests: an evaluation of RDT acceptance and usage by providers and patients – Tanzania, 2005. Malar J. 2008;7:239.
Drain P, Ngure K, Mugo N, Spinelli M, Chatterjee P, Bacchetti P, et al. Testing a real-time tenofovir urine adherence assay for monitoring and providing feedback to preexposure prophylaxis in Kenya (PUMA): protocol for a pilot randomized controlled trial. JMIR Res Protoc. 2020;9(4):e15029. https://doi.org/10.2196/15029.
Ayala GX, Elder JP. Qualitative methods to ensure acceptability of behavioral and social interventions to the target population. J Public Health Dent. 2011;71:S69-79.
Strasser S, Bitarakwate E, Gill M, Hoffman HJ, Musana O, Phiri A, et al. Introduction of rapid syphilis testing within prevention of mother-to-child transmission of HIV programs in Uganda and Zambia: a field acceptability and feasibility study. J Acquir Immune Defic Syndr. 2012;61:e40-46.
Holden RJ, Karsh B-T. The technology acceptance model: its past and its future in health care. J Biomed Inform. 2010;43:159–72.
Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44:1175–84.
Jeng J. Usability assessment of academic digital libraries: effectiveness. Eff Satisf Learn. 2005;55:96–121.
Jeng J. What is usability in the context of the digital library and how can it be measured. Inf Technol Libr. 2005;24:47–56.
Mills N, Donovan JL, Smith M, Jacoby A, Neal DE, Hamdy FC. Perceptions of equipoise are crucial to trial participation: a qualitative study of men in the ProtecT study. Control Clin Trials. 2003;24:272–82.
Jaccard J, Jacoby J. Theory Construction and Model-Building Skills: A Practical Guide for Social Scientists. 2010.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. Health Technol Assess. 2021;25:1–132.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for develo** and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374: n2061.
Bisset S, Daniel M, Potvin L. Exploring the Intervention— context interface: a case from a school-based nutrition intervention. Am J Eval. 2009;30:554–71.
Minary L, Alla F, Cambon L, Kivits J, Potvin L. Addressing complexity in population health intervention research: the context/intervention interface. J Epidemiol Community Health. 2018;72:319–23.
Dyer TA, Owens J, Robinson PG. The acceptability of healthcare: from satisfaction to trust. Community Dent Health. 2016;33(4):242–51. https://doi.org/10.1922/CDH_3902Dyer10.
Prusaczyk B, Swindle T, Curran G. Defining and conceptualizing outcomes for de-implementation: key distinctions from implementation outcomes. Implement Sci Commun. 2020;1:43.
Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18.
Mcintyre D, Thiede M, Birch S. Access as a policy-relevant concept in low- and middle-income countries. Health Econ Policy Law. 2009;4:179–93.
Toquero CS. Le patient face à la technologie : étude des déterminants de l’acceptabilité des technologies en santé. 2018.
Dewar RD, Dutton JE. The adoption of radical and incremental innovations: an empirical analysis. Manage Sci. 1986;32:1422–33.
Arbelaez-Garces G, Rakotondranaivo A, Bonjour E. Conception innovante en santé: revue de la littérature et cadre conceptuel pour évaluer l’acceptabilité. Conférence Gestion et Ingénierie des Systèmes Hospitaliers GISEH’14. Liège; 2014.
Saetren H. Facts and myths about research on public policy implementation: out-of-fashion, allegedly dead, but still very much alive and relevant. Policy Stud J. 2005;33:559–82.
Connell R. Using southern theory: decolonizing social thought in theory, research and application. Plan Theory. 2014;13:210–23.
Meekosha H. Decolonising disability: thinking and acting globally. Disabil Soc. 2011;26:667–82.
Acknowledgements
We would like to thank Émilie Brunet, in charge of the IRD's document collection, for her valuable help in develo** our research strategy. We would also like to thank Laurence Goury, from the IRD's Scientific and Technical Information Service, who gave us access to several documentary resources needed for our sco** review. Many thanks to Flore-Apolline Roy for making the map shown in Fig. 2. Finally, we would like to express our thanks to all the members of the AIRE study group.
Funding
This study was funded with support from Unitaid.
Author information
Authors and Affiliations
Contributions
SL, GBH, and VR conceptualized the study and worked on the methodology. SL undertook the literature review process and wrote the original version of the article. SL, GBH, and VR reviewed and edited the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix 1.
Search strategies for all databases. Appendix 2. Construction of the a priori framework. Appendix 3. Type of innovation.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Louart, S., Hedible, G.B. & Ridde, V. Assessing the acceptability of technological health innovations in sub-Saharan Africa: a sco** review and a best fit framework synthesis. BMC Health Serv Res 23, 930 (2023). https://doi.org/10.1186/s12913-023-09897-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09897-4