Abstract
Background
The objective of this study was to assess public hospital efficiency, including quality outputs, inefficiency determinants, and changes to efficiency over time, in an Italian region. To achieve this aim, the study used secondary data from the Veneto region for the years 2018 and 2019.
Methods
A nonparametric approach—that is, multistage data envelopment analysis (DEA)—was applied to a sample of 43 hospitals. We identified three categories of input: capital investments (Beds), labor (FTE), operating expenses. We selected five efficiency outputs (outpatient visits, inpatients, outpatient visit revenue, inpatient revenue, bed occupancy rate) and two quality outputs (mortality rate and inappropriate admission rate). Efficiency scores were estimated and decomposed into two components. Slack analysis was then conducted. Further, DEA efficiency scores were regressed on internal and external variables using a Tobit model. Finally, the Malmquist Productivity Index was applied.
Results
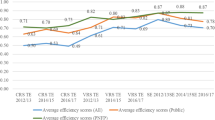
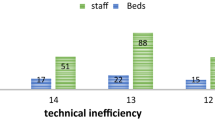
On average, the hospitals in the Veneto region operated at more than 95% efficiency. Technical and scale inefficiencies often occurred jointly, with 77% of inefficient hospitals needing a downsizing strategy to gain efficiency. The inputs identified as needing significant reductions were full-time employee (FTE) administrative staff and technicians. The size of the hospital in relation to the size of the population served and the length of patient stay were important factors for the efficiency score. The major cause of decreased efficiency over time was technical change (0.908) rather than efficiency change (0.974).
Conclusions
The study reveals improvements that should be made from both the policy and managerial perspectives. Hospital size is an important feature of inefficiency. On average, the results show that it is advisable for hospitals to reorganize nonmedical staff to enhance efficiency. Further, increasing technology investment could enable higher efficiency levels.
Similar content being viewed by others
Background
The recent global economic crisis has influenced the budgets of public organizations, including those of public hospitals and national health systems in general. According to the World Health Organization, for high-income and upper-middle-income countries, such as Italy, the main challenge relating to the provision of health services is to continue improving efficiency, quality, and equity [1]. Moreover, within the evolving social and economic environment, budget constraints have prompted a search for new ways of monitoring and controlling organizational finances that focus on the efficient and effective use of public resources [2]. Monitoring the performance of healthcare providers is a relevant issue worldwide, particularly in contexts such as hospitals given their significant effect on population health and the economy. The main problem facing hospitals has been inefficient use of existing resources rather than a lack of resources [3]. Therefore, hospital efficiency plays a strategic role in healthcare organizations. Assessing the determinants of efficiency allows managers to formulate appropriate organizational strategies to meet the challenges associated with continuous change. Focusing on the Italian National Health System, Guerrini et al. [4] note that in recent years, increasing attention has been paid to ensuring financial equilibrium and reducing the average annual growth rate of total health expenditure per capita. Italy has a regionally based National Health System that provides universal coverage free of charge [5]. Regional governments allocate resources to healthcare organizations and have a significant degree of autonomy in organizing the provision of healthcare planning and monitoring, as well as determining the number and vocation of healthcare providers [6], and the size of hospitals in terms of number of beds. One of the most important choices of Italy’s regional governments in relation to hospitals is the number of beds.
Literature review
Over the past 30 years, many research studies on hospital efficiency evaluation have been conducted in different countries. Färe et al. [7] published the first European study, and this was followed by many others [8,9,10,11,12,13]. Such studies have now been conducted in many other countries around the world, including in China, Iran, Brazil, Ukraine, and Angola [14,15,16,17,18].
Hospital efficiency has been evaluated in relation to many factors (see Table 1). Kohl et al. [19] consider capital investment of great importance in efficiency analysis. Chilingerian and Sherman [20] note the importance of labor to the service process in hospitals, identifying this factor as essential in assessing performance. In addition, other organizational choices, such as teaching status and the provision of first aid, are often considered relevant in assessing hospital efficiency in the literature [21]. A frequently investigated aspect of hospital efficiency is patient length of stay. Among previous studies there is consensus that an increase in the number of hospitalization days has a negative effect on hospital performance [22, 23]. Rebba and Rizzi [24] have found that a high number of beds per inhabitant is one of the major causes of hospital inefficiency because it increases overhead costs. In addition, Daidone and D’Amico [25] and Shahhoseini et al. [26] argue that efficiency is positively affected by hospital size. Nevertheless, this relationship remains controversial because research such as that of Nayar et al. [27] has found that small hospitals have higher efficiency and quality scores than do large hospitals. In addition, Chang [28] argues that the number of service types offered is negatively related to efficiency because a greater scope of service means a higher level of management complexity. This is supported by Campedelli et al. [29], who found that hospitals that provide a first-aid service incur higher costs than hospitals that do not provide this service.
Many studies on hospital efficiency assess pure technical efficiency (PTE) and scale efficiency [30, 31]. PTE represents managerial efficiency [32], which refers to management’s ability to save inputs to produce a certain amount of outputs or to produce more outputs with a given level of inputs [33, 34]. Scale efficiency indicates whether an organization operates at the most productive scale size [35].
However, despite the numerous studies on hospital efficiency conducted in many different countries, few studies have attempted to include quality measures [36], particularly those undertaken in the European context. One possible reason for this gap could be that the scientific community has not yet agreed on a common standard for addressing questions of quality in hospitals [19]. However, according to Chatfield [37], efficiency studies without quality considerations are neglecting a critical factor. Some research that does consider quality has been conducted in the United States [38, 39], and it identifies mortality rate as a good valuation of quality.
The purpose of this study was to assess the efficiency of public hospitals while including measures of quality. To fulfill this aim, the study attempted to answer the following research questions: (1) What are the main organizational factors that generate hospital inefficiency? (2) How do internal and external features affect hospital efficiency? (3) How has hospital efficiency changed over time? To answer these questions, the study employed multistage data envelopment analysis (DEA).
Data envelopment analysis
DEA is a nonparametric technique developed by Charnes et al. [40]. It is used to rank and compare the efficiency of various entities, defined as decision-making units (DMUs). DEA is grounded in an optimization algorithm that assigns a score between 0 and 1 to the DMUs given the input consumed and the output produced. DEA models allow assessment of the relative efficiency of DMUs by creating a production frontier using the best practice of the observed data. In addition, DEA can be considered an alternative to parametric frontier methods and financial ratio analysis. Rhodes [41] highlights that financial ratios allow benchmarking among a multitude of operating units, focusing on their financial results. Nayar et al. [27] note that the main flaw in measuring performance using this kind of methodology is the lack of technical indicators that enable evaluation of the efficiency of structures and the quality of services provided. According to Worthington [42] and O’Neill et al. [43], methods of nonparametric analysis such as DEA overcome the weaknesses of financial ratios and parametric analysis because they do not require any assumption related to the functional form of the relationship between outputs and inputs [44]. Further, DEA can not only identify inefficient units but can also assess the degree of inefficiency. DEA uses linear programming to construct a piecewise convex linear-segmented efficiency frontier, making it more flexible than econometric frontier analysis. Moreover, DEA can include multiple inputs and outputs. Despite these identified benefits, DEA presents a drawback: it attributes every deviation from the best practice frontier to inefficiency. However, such deviations might be due to statistical noise (e.g., measurement errors).
Methods
Study design
The study adopted a cross-sectional design to assess the efficiency of public hospitals in the Veneto region for the years 2018 and 2019. It used a longitudinal design to analyze the trend in technical efficiency in general hospitals from 2018 to 2019. More specifically, a Charnes, Cooper, and Rhodes (CCR) input-oriented model, decomposition of the obtained scores, and slack assessment were developed for 2018 and 2019. Subsequently, Tobit regression was applied to understand the internal and external sources of inefficiency. Finally, the Malmquist Productivity Index was used to assess how efficiency has changed over time.
Study population
To conduct the efficiency analysis, the Veneto region was selected as the case study site [45]. This was because of the region’s high level of interest in researching new ways to control the efficiency of public hospitals. Guerrini et al. [3] found that this region has specific characteristics (i.e., an increase in the elderly population and growing life expectancy of residents) that have led to a gradual increase in comorbidity and chronic diseases and a corresponding increase in demand for high-quality healthcare services. All the data used in this study were provided by Azienda Zero UOC Controllo di Gestione e Adempimenti LEA (Azienda Zero). A full dataset from 2018 to 2019 containing nonpublicly available technical data cost and revenue items was analyzed. The data included in this study are the operative costs and revenue for public hospitals, number of beds, number of FTEs, mortality rate, inappropriate admission rate, bed occupancy rate, length of stay, provision of first aid, and number of residents. During the period under analysis, the Veneto region had 53 public hospitals. One hospital closed in 2018, three hospitals treated only a particular type of patient and were therefore considered nonhomogeneous and noncomparable, and six hospitals presented missing data. Therefore, the final sample included 43 hospitals and 86 observations.
Selection of study variables
Selecting suitable inputs and outputs is crucial for ensuring meaningful efficiency analysis. To obtain the discriminative power of DEA, Dyson et al. [46] recommend being parsimonious with the number of inputs and outputs. According to these researchers, the number of DMUs should always be larger than two∙(#inputs + #outputs) to ensure sufficient discrimination between units. In this research, six inputs and seven outputs were chosen. Therefore, this rule was not violated.
Following Ozcan [47], we used three categories of inputs: capital investment, labor, and operating expenses. As suggested by Kohl et al. [19], a good proxy for capital investment is the number of beds (Beds). This variable is widely used in the literature [48,49,50,51]. As a proxy for labor, we used the number of hospital FTEs. Chilingerian and Sherman [20] note the relevance of labor to hospital efficiency. In addition, these researchers advise distinguishing between different types of personnel. Thus, we identified four categories of personnel: medical (FTE Med), nursing (FTE Nurse), administrative (FTE Admin), and technical (FTE Tech). As a proxy for operating expenses, we used the operating costs (Cost) of hospitals, which is a commonly used variable in the literature [52,53,54].
For the outputs, we used five variables to evaluate hospital efficiency and two variables to evaluate hospital quality. For efficiency-output variables for hospitals, Ozcan [47] advises including inpatient and outpatient visits. Thus, we used the number of outpatient visits (Outpatients) and the number of case-mix-adjusted inpatients (Adj. Inpatients). A commonly used output is operating revenue [55,56,57]. To measure this output, we used revenues from inpatient visits (Inpatient Revenue) and revenues from outpatient visits (Outpatient Revenue). Another variable commonly used to analyze hospital efficiency [89].
Limitations and further research
This study has some limitations. Beyond the typical limitations of basic DEA models [19], some issues are specific to this study. One is that we incorporated only a limited number of quality measures into the model, excluding measures such as hospital readmission rates because of the unavailability of data. In addition, an examination of demographic factors such as the age of population served could reveal significant information for the hospitals we analyzed. In addition, further research could extend this study by assessing hospital efficiency in other Italian regions.
Conclusions
This study contributes to the healthcare management literature because few previous studies in the European context have analyzed hospital efficiency using quality measures as outputs [36]. To fill this research gap, this research used hospitals in the Veneto region as a case study, identifying the organizational causes that affected efficiency, also considering quality measures, and how these changed over a period of two years. The results reveal that more than half of the hospitals under review were efficient. For the hospitals that were found to be inefficient, many had both input utilization and scale inefficiency. This study also provides empirical evidence for the main causes of inefficiency. Hospital size is one of the most important sources of inefficiency. In addition, administrative and technical staff often cause inefficiency. The contextual factors that most influence efficiency are the average patient length of stay and hospital size with respect to the population served. The role of technology is crucial to maintaining or increasing efficiency levels over time.
DEA is a good method for measuring hospital performance, in addition to the budgeting process that has traditionally been used in Italy. DEA is particularly useful for its ability to estimate the volume of inputs and outputs that can be optimized and its capacity to identify the main sources of inefficiency.
The results also underscore that a rethink of hospital size on the part of policymakers would be particularly valuable for increasing the current efficiency levels of many hospitals and maintaining constant and high service quality. Improving performance also depends on improving staff efficiency, particularly administrative and technical staff. This may be achieved by providing capacity building such as training staff members on efficient resource utilization. Finally, the results suggest that hospital managers should pay significant attention to advancements in technology and the skills needed to employ new technology in the best possible way.
Availability of data and materials
The data that support the findings of this study are available from Azienda Zero—Veneto Region, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, data are available from the authors upon reasonable request and with the permission of Azienda Zero—Veneto Region.
Abbreviations
- ALOS:
-
Average length of stay
- BCC:
-
Banker, Charnes, and Cooper
- BOR:
-
Bed occupancy rate
- CCR:
-
Charnes, Cooper, and Rhodes
- CRS:
-
Constant return to scale
- DEA:
-
Data envelopment analysis
- DMU:
-
Decision-making unit
- DRS:
-
Decreasing return to scale
- EFFCH:
-
Efficiency change
- FTE:
-
Full-time employee
- IRS:
-
Increasing return to scale
- OTE:
-
Overall technical efficiency
- PECH:
-
Pure efficiency change
- PTE:
-
Pure technical efficiency
- RTS:
-
Return to scale
- SE:
-
Scale efficiency
- SECH:
-
Scale efficiency change
- TE:
-
Technical efficiency
- TECHCH:
-
Technical change
- TFPCH:
-
Total factor productivity change
- VRS:
-
Variable return to scale.
References
World Health Organization. Primary health care on the road to universal health coverage: 2019 monitoring report. Geneva: WHO; 2019.
Rondeau KV, Wagar TH. Downsizing and organizational restructuring: what is the impact on hospital performance? Int J Public Adm. 2003;26(14):1647–68.
Sahin I, Ozcan YA. Public sector hospital efficiency for provincial markets in Turkey. J Med Syst. 2000;24(6):307–20.
Guerrini A, Romano G, Campedelli B, Leardini C. Public vs. private in hospital efficiency: exploring determinants in a competitive environment. Int. J Public Adm. 2018;41(3):181–9.
Lega F, Sartirana M. Making doctors manage … but how? Recent developments in the Italian NHS. BMC Health Serv Res. 2016;16(2):65–72.
Ferré F, de Belvis AG, Valerio L, Longhi S, Lazzari A, Fattore G. Italy: health system review. Health Syst Transit. 2014;16(4):1–168.
Färe R, Grosskopf S, Lindgren B, Roos P. Productivity developments in Swedish hospitals: a Malmquist output index approach. In: Charnes A, Cooper WW, Lewin AY, Seiford LM, editors. Data envelopment analysis: theory, methodology, and applications. New York: Springer; 1994. p. 253–72.
Kontodimopoulos N, Niakas D. Efficiency measurement of hemodialysis units in Greece with data envelopment analysis. Health Policy. 2005;71(2):195–204.
Dotoli M, Epicoco N, Falagario M, Sciancalepore F. A cross-efficiency fuzzy data envelopment analysis technique for performance evaluation of decision making units under uncertainty. Comput Industrial Eng. 2015;79:103–14.
Flokou A, Aletras V, Niakas D. Decomposition of potential efficiency gains from hospital mergers in Greece. Health Care Manag Sci. 2017;20(4):467–84.
Herwartz H, Strumann C. On the effect of prospective payment on local hospital competition in Germany. Health Care Manag Sci. 2012;15(1):48–62.
van Ineveld M, van Oostrum J, Vermeulen R, Steenhoek A, van de Klundert J. Productivity and quality of Dutch hospitals during system reform. Health Care Manag Sci. 2016;19(3):279–90.
Siciliani L. Estimating technical efficiency in the hospital sector with panel data. Appl Health Econ Health Policy. 2006;5(2):99–116.
Liu X, Mills A. The effect of performance-related pay of hospital doctors on hospital behaviour: a case study from Shandong. China Hum Resour Health. 2005;3(11):1–12.
Marnani AB, Sadeghifar J, Pourmohammadi K, Mostafaie D, Abolhalaj M, Bastani P. Performance assessment indicators: how DEA and Pabon lasso describe Iranian hospitals’ performance. HealthMED. 2012;13(3):791–6.
Araújo C, Barros CP, Wanke P. Efficiency determinants and capacity issues in Brazilian for-profit hospitals. Health Care Manag Sci. 2014;17(2):1–13.
Pilyavsky AI, Aaronson WE, Bernet PM, Rosko MD, Valdmanis VG, Golubchikov MV. East–west: does it make a difference to hospital efficiencies in Ukraine? Health Econ. 2006;15(11):1173–86.
Kirigia J, Emrouznejad A, Cassoma B, Asbu EZ, Barry S. A performance assessment method for hospitals: the case of municipal hospitals in Angola. J Med Syst. 2008;32(6):509–19.
Kohl S, Schoenfelder J, Fügener A, Brunner JO. The use of data envelopment analysis (DEA) in healthcare with a focus on hospitals. Health Care Manag Sci. 2019;22(2):245–86.
Chilingerian JH, Sherman HD. Health-care applications: from hospitals to physicians, from productive efficiency to quality frontiers. In: Cooper WW, Seiford LM, Zhu J, editors. Handbook on data envelopment analysis. New York: Springer; 2011. p. 445–93.
Kakeman E, Forushani AR, Dargahi H. Technical efficiency of hospitals in Tehran. Iran Iranian J Public Health. 2016;45(4):494–502.
Staat M. Efficiency of hospitals in Germany: a DEA–bootstrap approach. Appl Econ. 2006;38(19):2255–63.
Dimas G, Goula A, Soulis S. Productive performance and its components in Greek public hospitals. Oper Res. 2012;12(1):15–27.
Rebba V, Rizzi D. Analisi dell’efficienza relativa delle strutture di ricovero con il metodo DEA: il caso degli ospedali del Veneto. Venice: Universita degli Studi di Venezia; 2000.
Daidone S, D’Amico F. Technical efficiency, specialization and ownership form: evidences from a pooling of Italian hospitals. J Productivity Anal. 2009;32(3):203–16.
Shahhoseini R, Tofighi S, Jaafaripooyan E, Safiaryan R. Efficiency measurement in develo** countries: application of data envelopment analysis for Iranian hospitals. Health Serv Manag Res. 2011;24(2):75–80.
Nayar P, Ozcan YA, Yu F, Nguyen AT. Benchmarking urban acute care hospitals: efficiency and quality perspectives. Health Care Manag Rev. 2013;38(2):137–45.
Chang F-K. Structural health monitoring: current status and perspectives. Stanford: CRC Press; 1998.
Campedelli B, Guerrini A, Romano G, Leardini C. La performance della rete ospedaliera pubblica della regione Veneto. L’impatto delle variabili ambientali e operative sull’efficienza, vol. 92. Mecosan: Management ed Economia Sanitaria; 2014. p. 119–31.
Dash U, Vaishnavi SD, Muraleedharan VR. Technical efficiency and scale efficiency of district hospitals: a case study. J Health Manag. 2010;12(3):231–48.
Ram Jat T, San SM. Technical efficiency of public district hospitals in Madhya Pradesh, India: a data envelopment analysis. Glob Health Action. 2013;6(1):21742.
Yusefzadeh H, Ghaderi H, Bagherzade R, Barouni M. The efficiency and budgeting of public hospitals: case study of Iran. Iranian Red Crescent Med J. 2013;15(5):393–9.
Kumar S, Gulati R. An examination of technical, pure technical, and scale efficiencies in Indian public sector banks using data envelopment analysis. Eurasian J Bus Econ. 2008;1(2):33–69.
Taib CA, Ashraf MS, Razimi MSA. Technical, pure technical and scale efficiency: a non-parametric approach of Pakistan’s insurance and takaful industry. Acad Account Financ Stud J. 2018;22(1):1–11.
Farrell MJ. The measurement of productive efficiency. J Royal Stat Soc. 1957;120(3):253–90.
Nayar P, Ozcan Y. Data envelopment analysis comparison of hospital efficiency and quality. J Med Syst. 2008;32(3):193–9.
Chatfield JS. Data envelopment analysis comparison of hospital efficiency, quality and control. Int J Manag Account Res. 2014;4(1):93–109.
Valdmanis VG, Rosko MD, Mutter RL. Hospital quality, efficiency, and input slack differentials. Health Serv Res. 2008;43(5p2):1830–48.
Clement JP, Valdmanis VG, Bazzoli GJ, Zhao M, Chukmaitov A. Is more better? An analysis of hospital outcomes and efficiency with a DEA model of output congestion. Health Care Manag Sci. 2008;11(1):67–77.
Charnes A, Cooper WW, Rhodes E. Measuring the efficiency of decision making units. Eur J Oper Res. 1978;2(6):429–44.
Rhodes EL. Using data envelopment analysis (DEA) to evaluate environmental quality and justice: a different way of looking at the same old numbers. Int J Public Adm. 2002;25(2–3):253–79.
Worthington AC. Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Med Care Res Rev. 2004;61(2):135–70.
O’Neill L, Rauner M, Heidenberger K, Kraus M. A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socio Econ Plan Sci. 2008;42(3):158–89.
Zhang X, Tone K, Lu Y. Impact of the local public hospital reform on the efficiency of medium-sized hospitals in Japan: an improved slacks-based measure data envelopment analysis approach. Health Serv Res. 2018;53(2):896–918.
Yin RK. Validity and generalization in future case study evaluations. Evaluation. 2013;19(3):321–32.
Dyson RG, Allen R, Camanho AS, Podinovski VV, Sarrico CS, Shale EA. Pitfalls and protocols in DEA. Eur J Oper Res. 2001;132(2):245–59.
Ozcan YA. Health care benchmarking and performance evaluation: an assessment using data envelopment analysis (DEA). Berlin: Springer; 2014.
Alatawi AD, Niessen LW, Khan JA. Efficiency evaluation of public hospitals in Saudi Arabia: an application of data envelopment analysis. BMJ Open. 2020;10(1):e031924.
Ghahremanloo M, Hasani A, Amiri M, Hashemi-Tabatabaei M, Keshavarz-Ghorabaee M, Ustinovičius L. A novel DEA model for hospital performance evaluation based on the measurement of efficiency, effectiveness, and productivity. Eng Manag Prod Serv. 2019;12(1):7–19.
Sultan WI, Crispim J. Evaluating the productive efficiency of Jordanian public hospitals. Int J Bus Manag. 2016;12(1):68–83.
Nabilou B, Yusefzadeh H, Rezapour A, Ebadi Fard Azar F, Salem Safi P, Sarabi Asiabar A, et al. The productivity and its barriers in public hospitals: case study of ran. Med J Islamic Repub. Iran. 2016;30:316.
Hatefi SM, Haeri A. Evaluating hospital performance using an integrated balanced scorecard and fuzzy data envelopment analysis. J Health Manag Inform. 2019;6(2):66–76.
Lyroudi K, Glaveli N, Koulakiotis A, Angelidis D. The productive performance of public hospital clinics in Greece: a case study. Health Serv Manag Res. 2006;19(2):67–72.
Allin S, Veillard J, Wang L, Grignon M. How can health system efficiency be improved in Canada? Healthc Policy. 2015;11(1):33–45.
Nistor CS, Ștefănescu CA, Crișan AR. Performance through efficiency in the public healthcare system—a DEA approach in an emergent country. Studia Universitatis Babes-Bolyai Oeconomica. 2017;62(1):31–49.
Gai R, Zhou C, Xu L, Zhu M, Wang X, Li X. Health resource allocation and productive efficiency of Chinese county hospitals: data from 1993 to 2005. Biosci Trends. 2010;4(5):218–24.
Park JS, Fowler KL, Giebel SA. Measuring hospital operating efficiencies for strategic decisions. Int J Bus Soc Sci. 2011;2(13):56–60.
Dexter F, O’Neill L, **n L, Ledolter J. Sensitivity of super-efficient data envelopment analysis results to individual decision-making units: an example of surgical workload by specialty. Health Care Manag Sci. 2008;11(4):307–18.
Köse T, Uçkun N, Girginer N. An efficiency analysis of the clinical departments of a public hospital in Eskisehir by using DEA. Glob J Adv Pure Appl Sci. 2014;4:252–8.
Bilsel M, Davutyan N. Hospital efficiency with risk adjusted mortality as undesirable output: the Turkish case. Ann Oper Res. 2011;221(1):73–88.
Ferrier GD, Trivitt JS. Incorporating quality into the measurement of hospital efficiency: a double DEA approach. J Prod Anal. 2013;40(3):337–55.
Koopmans TC. Analysis of production as an efficient combination of activities. Activity analysis of production and allocation. New York: Wiley; 1951. p. 33–7.
Pastor JT, Aparicio J. Translation invariance in data envelopment analysis. In: Zhu J, editor. Data envelopment analysis. Boston: Springer; 2015. p. 245–68.
Färe R, Grosskopf S. Modeling undesirable factors in efficiency evaluation: comment. Eur J Oper Res. 2004;157(1):242–5.
Guo H, Zhao Y, Niu T, Tsui KL. Hong Kong Hospital Authority resource efficiency evaluation: via a novel DEA-Malmquist model and Tobit regression model. PLoS One. 2017;12(9):e0184211.
Golany B, Roll Y. An application procedure for DEA. Omega. 1989;17(3):237–50.
Knox Lovell CA, Pastor JT, Turner JA. Measuring macroeconomic performance in the OECD: a comparison of European and non-European countries. Eur J Oper Res. 1995;3(87):507–18.
Sharp JA, Meng W, Liu WA. Modified slacks-based measure model for data envelopment analysis with “natural” negative outputs and inputs. J Oper Res Soc. 2007;58(12):1672–7.
See KF, Yen SH. Does happiness matter to health system efficiency? A performance analysis. Health Econ Rev. 2018;8(1):1–10.
Kirigia JM, Asbu EZ. Technical and scale efficiency of public community hospitals in Eritrea: an exploratory study. Health Econ Rev. 2013;3(1):1–16.
Mujasi PN, Asbu EZ, Puig-Junoy J. How efficient are referral hospitals in Uganda? A data envelopment analysis and Tobit regression approach. BMC Health Serv Res. 2016;16(1):230.
Ayiko R, Mujasi PN, Abaliwano J, Turyareeba D, Enyaku R, Anguyo R. Levels, trends and determinants of technical efficiency of general hospitals in Uganda: data envelopment analysis and Tobit regression analysis. BMC Health Serv Res. 2020;20(1):1–12.
Banker RD, Charnes A, Cooper WW. Some models for estimating technical and scale inefficiencies in data envelopment analysis. Manag Sci. 1984;30(9):1078–92.
Banker RD, Chang H, Cooper WW. Simulation studies of efficiency, returns to scale and misspecification with nonlinear functions in DEA. Ann Oper Res. 1996;66(4):231–53.
Yildirim C, Kacak H, Yildirim S, Kavuncubasi S. Comprehensive efficiency assessment of Turkish teaching hospitals: technical, pure technical and scale efficiencies with data envelopment analysis. J Appl Bus Econ. 2019;21(3):124–40.
Bogetoft P, Otto L. Benchmarking with DEA, SFA, and R, vol. 157. New York: Springer; 2011.
Wang X, Luo H, Qin X, Feng J, Gao H, Feng Q. Evaluation of performance and impacts of maternal and child health hospital services using data envelopment analysis in Guangxi Zhuang autonomous region, China: a comparison study among poverty and non-poverty county level hospitals. Int J Equity Health. 2016;15(1):1–6.
Sultan WI, Crispim J. Measuring the efficiency of Palestinian public hospitals during 2010–2015: an application of a two-stage DEA method. BMC Health Serv Res. 2018;18(1):1–17.
Simar L, Wilson PW. Estimation and inference in two-stage, semi-parametric models of production processes. J Econom. 2007;136(1):31–64.
Banker RD, Natarajan R. Evaluating contextual variables affecting productivity using data envelopment analysis. Oper Res. 2008;56(1):48–58.
Mujasi PN, Kirigia JM. Productivity and efficiency changes in referral hospitals in Uganda: an application of Malmquist Total productivity index. Health Syst Policy Res. 2016;3(1):1–12.
Coelli TJ, Rao DSP, O’Donnell CJ, Battese GE. An introduction to productivity and efficiency analysis. New York: Springer Science; 1998.
Cooper WW, Seiford LM, Zhu J. Handbook on data envelopment analysis. Boston: Kluwer Academic Publishers; 2004.
Ozcan YA. Health care benchmarking and performance evaluation. New York: Springer; 2008.
Tlotlego N, Nonvignon J, Sambo LG, Asbu EZ, Kirigia JM. Assessment of productivity of hospitals in Botswana: a DEA application. Int Arch Med. 2010;3(1):1–14.
Sarabi Asiaba A, Sharifi T, Rezapour A, Khatami Firouzabadi SMA, Haghighat-Fard P, Saeed M-P. Technical efficiency and its affecting factors in Tehran’s public hospitals: DEA approach and Tobit regression. Med J Islamic Repub. Iran. 2020;34(1):1228–36.
Ali M, Debela M, Bamud T. Technical efficiency of selected hospitals in eastern Ethiopia. Health Econ Rev. 2017;7(1):1–13.
Li NN, Wang CH, Ni H, Wang H. Efficiency and productivity of county-level public hospitals based on the data envelopment analysis model and Malmquist index in Anhui, China. Chin Med J. 2017;130(23):2836.
Killick T. Policy economics: a textbook of applied economics on develo** countries. London: Heinemann; 1982.
Acknowledgements
The authors are grateful to Azienda Zero UOC Controllo di Gestione e Adempimenti LEA for granting us the use of the secondary data.
Funding
The authors did not receive any funding for this study.
Author information
Authors and Affiliations
Contributions
LPO and CL conceptualized the study and contributed to the data collection, review of literature, data analysis, interpretation of results and writing of the manuscript. SV and BC contributed to data analysis and review of the manuscript. All authors read and approved the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Piubello Orsini, L., Leardini, C., Vernizzi, S. et al. Inefficiency of public hospitals: a multistage data envelopment analysis in an Italian region. BMC Health Serv Res 21, 1281 (2021). https://doi.org/10.1186/s12913-021-07276-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-07276-5