Abstract
Background
The effect of cancer diagnosis affects the psychological well-being of the caregivers of cancer patients and results in a risk of psychiatric morbidity. This study aimed to determine the prevalence and associated factors of depression among primary caregivers of adult cancer patients.
Objective
This study aimed to assess the magnitude of depression and associated factors among primary caregivers of adult cancer patients.
Methodology
Hospital-based cross-sectional study was conducted among primary caregivers of adult cancer patients. The convenient sampling method used to recruit caregivers of cancer patients. The data was collected by using the Amharic version patient health questionnaire and analyzed by SPSS version 25. Descriptive statistics were used to describe the prevalence of depression and bivariable and multivariable regression models were used to determine the net effect of each independent variable on depression.
Results
The overall prevalence of depression among adult cancer patient caregivers was 54.1% (95% CI 47.6, 60.6). Household size < 3; (AOR = 4.5, 95% CI: 1.1–13), Monthly income < 600 (AOR = 2.8, 95% CI:2.5–15.9), Caring hours ≥ 9 (AOR = 9, 95% CI:4–21), Burden level ≥ 20 ;(AOR = 10.7, 95% CI:9.3–11.6) were independent factors of depression among primary caregivers of cancer patients.
Conclusion
The results of this study showed a higher prevalence of depressed symptoms among primary caregivers of cancer patients. Long caring hours, small household size, low-income level, and higher burden level were independent factors of caregiver depression, indicating the urgent necessity to investigate and deal with it through interdisciplinary approaches.
Similar content being viewed by others
Introduction
Global Burden of Disease estimates for 2018 show that there were 9.6 million cancer deaths and 18.1 million new cases worldwide, respectively [1]. In the United States, the lifetime risk of develo** invasive cancer is estimated to be 42% for men and 38% for women [2]. Africa and other low- and middle-income nations accounted for over half of all cancer cases and roughly two-thirds of cancer-related fatalities. In this area, cancer patients and their families experience prolonged depression and have little to no hope [3].
According to estimates, Ethiopia has 64,285 new cases of cancer per year, more than 44,000 fatalities, and a 5.8% overall national mortality rate. There is an 11.3% and 9.4% chance, respectively, of receiving a cancer diagnosis and passing away from the illness [4]. Because cancer affects a patient’s social environment, its effects extend beyond the individual suffering from the disease. There is a chance of psychiatric morbidity as a result of the impact cancer has on the mental health of those who care for cancer patients [2].
Cancer diagnosis and treatment are traumatic experiences that place a heavy load on carers and can elicit emotional reactions like depression and anxiety [5]. Although they are valuable members of the oncology team, carers for cancer patients are frequently disregarded. From diagnosis through treatment and ultimately death, care has an impact. The effects of providing care are still mainly unclear in develo** nations. The patient’s spouse, son, daughter, friend, or other close relatives are the most common family members who take on the role of carer and are crucial to the patient’s care and recovery [6, 7].
Cancer causes many disruptions to carers, but the most significant burden is related to their psychological well-being. In the psychological domain of quality of life, the effects manifest as increased depression and difficulty co** with caregiving responsibilities [8,9,10]. Family carers provide long-term care for cancer patients; however, they are not adequately prepared, informed, or supported to carry out these crucial roles [11]. Research showed that carers’ levels of depression are higher and do not gradually subside compared to those of the cancer patients they are caring for, with prevalence rates ranging from 3 to 82% [12,13,14]. The demographic characteristics of the patients and their caregivers, length of hours of stay caring for the cancer patients, clinical variables of the patient, and caregivers’ burden level have been considered to play a role in the development of depression in caregivers of cancer patients [7, 8, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27].
Research indicated that early detection and treatment of depression in carers may lead to better physical and mental health, a higher quality of life, a reduction in suffering, and an enhanced ability to care for cancer patients when provided with psychoeducation, skill development, and therapeutic counselling [13, 28, 29]. Research indicates that in Ethiopia, the prevalence of depression is lower in the general population than in chronic illnesses [30]. Studies on cancer patients’ carers are scarce, though. and the baseline for future research would be this study. Thus, the purpose of this study was to evaluate the prevalence of depression and related variables among primary carers of adult cancer patients who visited the South Ethiopian HUCSH oncology unit in 2019.
Methods and materials
Study area and study period
This cross-sectional study was conducted in Hawassa City University Hospital, which is about 300 km away from the capital city of Ethiopia Addis Ababa to the south. The Hospital is the largest in the Southern Nation of the Ethiopian region. The hospital started all cancer treatment starting from 2017 GC. Currently HUCSH cancer center has two senior clinical oncologists, two MSc in clinical oncology nurses, four trained general practitioners, one palliative care physician 12 trained nurses, three clinical pharmacists, two laboratory technologists, and supportive staff. HUCSH Cancer Centre has 18 functional beds and the Centre is on preparation to start radiation therapy. with three months average outpatient visit is 250 per month. Colorectal, breast, cervical, and sarcomas are the commonly seen cases at the Oncology center. The study was conducted from March to June 2019.
The study population
The source population was all cancer patients’ caregivers who attended the oncology unit. The caregivers aged > 18 years, who can understand Amharic, and Caregivers with sufficient general conditions to interview were included in the study. Professional or paid caregivers, caregivers who stayed with the patient for less than two weeks, caregivers with a previous history of depression, and caregivers of newly diagnosed cancer patients with less than 2 weeks were excluded from the study.
Sample size and sampling procedure
The Sample size was determined by calculating using a single population proportion.
Sample size calculation formula n= (zα/2)2pq/d2.
Using a confidence level of 95% (α = 0.05; zα/2= 1.96 and a maximum permissible error of 5% and since there is no similar study found in Ethiopia p = 50% was used. The result of the calculation was n = 384 and considering 10% for missing data and for non-response rate, the final sample size became 422. The final caregivers who attended cancer patients during the survey period were 238. So, the sample size for the study was all caregivers who attended cancer patients during data collection. No specific sampling procedures were employed since all caregivers attended cancer patients were included in the study. For each patient, we selected one caregiver based on cancer patients’ recommendations and inclusion criteria.
Operational definition
Depression in caregivers- depression in caregivers was measured by using the PHQ-9 depression assessment tool. Those caregivers who scored greater than or equal to 10 were taken as depressed [31, 32].
Primary caregivers- Family members include fathers, mothers, sisters, brothers, daughters, sons, uncles, aunts, grandfathers, partners, sons or daughters-in-law, and other blood relations. They should be the ones who stay with the patient for two weeks or more and are not compensated for their care [28].
Caregiver burden -was assessed with the Zarit Burden Interview (ZBI). ZBI consists of 24 questions scored on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), covering five domains evaluating the caregivers’ reactions to caring at the time of the survey. The higher ZBI scores indicate the greater the burden. No burden at scores of less than 10, mild burden at 11 to 20, and severe burden at ≥ 20 [33].
Data collection procedures and quality assurance
The participants were identified by asking the patient who was their caregivers. Data were collected by using structured questionnaires, a patient health questionnaire (PHQ-9), and a Zarit Burden Interview (ZBI). PHQ-9 was validated to be used for screening and diagnosis of depression in caregivers [31]; it was also validated in Ethiopia (Amharic version) with a reliability test of Cronbach’s alpha 0.89 [33]. ZBI was used to assess caregivers’ burden and translated into Amharic language and back to English to check its consistency by fluent English and Amharic speakers [34]. The clinical variables of patients were collected from patients’ health care profiles by prepared format based on the clinical variables that need to be collected. A pilot study was done 2 weeks before data collection at a private Yanet Higher Specialized clinic chemotherapy center.
In this study, a pilot test was conducted on 30 participant caregivers during the pre-test. Structural validity was validated by face validity and internal consistency (reliability) was checked by Cronbach’s alpha and it was α = 0.89. Quality was assured by conducting a pre-test and giving training for the data collectors and supervisors before the actual data collection. Appropriate modifications were made after viewing the pre-test result and overall supervision was made by the principal investigator. The pilot study indicated that the participants needed to be interviewed privately and the necessity of adding some variables. The interviews took 10–15 min for quantitative.
Statistical analysis
All filled checklists/questionnaires were checked for completeness and consistency, cleaned manually, and entered into Statistical Package for Social Science (SPSS) Windows version 25. Descriptive statistics were used for the socio-demographics, caregivers’ related burden, and clinical variables of the patient and depression. The variables with a p-value less than 0.25 in bivariate logistic regression were interred into multivariate logistic regression. The variable with a p-value less than 0.05 in multivariate logistic regression was declared as a predictive associative factor of depression of primary caregivers among adult cancer patients attending the HUCSH oncology unit.
Results
Socio-demographic characteristics of the cancer patients’ caregivers
A total of 238 study participants were enrolled in the study 231 responded with a response rate of 97%. The mean age of the caregivers was 35 years. About 139 (60%) of the respondents of cancer patients’ caregivers were female whereas, 155 (67.1%) of the caregivers were male. The majority 203 (87.4%) of the participant patients were married. The mean, median, and maximum household sizes of the caregivers were 5, 5, and 16 respectively. 78.4% of caregivers were employed, more than 90% of caregiver’s education level was primary and above, 61.5% of the caregivers live with their patients and only 2.2% of the caregivers did not know the diagnosis of their relatives’ disease type (Table 1).
Caregiver characteristics
Regarding the type of caregivers of cancer patients, the husband and son of the patient were the predominant numbers of caregivers (Fig. 1).
Clinical characteristics of cancer patients
Breast cancer accounts for a large proportion of distribution in treatment centers (34.2%) followed by GI (15.2%) and NHL (13.4%) cancers and others were classified under 14 different less frequent cancer types categorized under other types accounting for 25.1%. About 213(92.2%) of patients were under treatment among these 118(51.1%) chemotherapies (either on daycare or inpatient). The 7(3.03%) of cancer patients were capable only of limited self-care and confined to bed or chair for more than 50% of working hours (with performance status ECOG 3). The majority of the patients were in the advanced stage; presented with stage three 89(38.5%) and stage four 81 (35.1%). Around 25(10.8%) cancer patients have co-morbidity (Table 2), (Fig. 2).
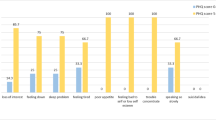
Depression and burden level of caregivers
The mean caregivers’ depression score was 9.5 with a standard deviation of 5.7. A 6(2.6) % of caregivers had severe depression. The mean burden score of the respondent caregivers was 15 and the median score was 13. The mean hours of the caregivers who stay with and give care for the patients were 9.36 (SD 8.41) and the median hour is 6. 51 out of 231 caregivers respond that give care for their relatives 24 h per day. One-third (32.9%) of the caregivers spent their time caring for their relatives more than the mean hours of caring. The majority 96(41.6%) has a burden were 10–20 and the majority 76(32.9%) have a depression range of 10–14 (Table 3), (Fig. 3).
Bivariate and multivariate analysis of factors associated with depression
To identify the independent factors of depression among caregivers of cancer patients attending HUCSH, bivariate and multivariate regression models were used. The bivariate regression model age, household size, monthly income, caring hours, and burden level showed a significant association with caregiver depression (Table 4). After multivariate analysis, four baseline factors were identified: household < 3; (AOR = 4.5, 95% CI: 1.1–13), Monthly income < 600 (AOR = 2.8, 95% CI:2.5–15.9), Caring hours ≥ 9 (AOR = 9, 95% CI:4–21), Burden level ≥ 2020 ;(AOR = 10.7, 95% CI:9.3–11.6) are independent factors of depression among primary caregivers of cancer patients (Table 4).
Discussion
This study determined the prevalence and associated factors of depression among adult cancer patients’ primary caregivers in the oncology treatment center at Hawassa University Comprehensive Specialized Hospital. The overall prevalence of depression was found to be 54.1% with (95% CI:47.6–60.6). The prevalence of depression was found to be higher than the study finding from U.S.A 6% [6], Uganda 26% [8], Malaysia 29.4% [36], Germany 26% [37], and United Kingdom 3% [38]. The higher prevalence of depression in the current study setting may be due to a comprehensive depression management program alongside cancer management or it could be due to geographical, environmental, lifestyle, and genetic variation. The current study is lower than the findings from South Korea (82.2%) [19] and the UK (58.1%) [39]. These differences may be because of the different sample sizes, service setup, study participants, study period, and sampling technique.
In this study 40–49 age group of caregivers was 78% less likely to develop depression; this finding is similar to the study conducted in Turkey found that younger age groups were more likely to develop depression than older age group [19]. The number of family members of the caregivers was an associated factor of depression among caregivers of cancer patients attending the HUCSH oncology unit. Caregivers with household size < 3 were 4.5 times more likely to be depressed when compared with household size this was congruent with a previous study [40]. This is due to those who have lower household sizes there is limited sharing of burden and a greater chance of longer caring hours which may induce depression in caregivers. So, this may predispose to the development of depression among caregivers.
The monthly income level of caregivers was a significantly associated factor for the development of depression in caregivers. The monthly income of caregivers with better monthly income have a lower chance of getting depression which is similar to previous findings [16, 19]. This may be because they feel mental pain as the reason for the shortage of income due to financial toxicity. After the patient loses his/her wellness, the productivity decreases even some lose their jobs. The caregivers also invest their working hours in the patients and because of this, they may be blamed for not working some are financially punished others are put in a lower position and lower payment. The finding of financial influence on the development of depression among caregivers is similar to an investigation done in Turkey [18].
The daily caring hours were the other associated factor of depression among caregivers of cancer patients. As the caring hour length with patients increases, the development of depression among caregivers increases. Caregivers caring > 9 h per day have a 9 times higher chance of depression. This study’s finding was similar to an investigation done in Athens, Greece, indicating that depression increases with increasing daily caring hours [15]. This may be because of staying longer hours suffering from observing and feeling the hopelessness of the patient, confusion about what to do when the patient suffers from side effects and disease conditions, and sometimes not knowing what to prepare for eating, what is preferable, how to talk to relax him/her.
Burden is a statistically significant associated factor of depression among caregivers of cancer patients. 64.9% of participant caregivers were burdened by their caregiving activities. Caregivers with burden levels 10–20 and < 20 were 5.6 and 10.7 more likely to burden respectively which is Similar to studies conducted in Melbourne Australia, western USA, and Spain [9, 14, 25, 41]. . This may be due to the caregivers not being able to participate in the social function because of caregiving. They couldn’t participate in different weddings, group work, and the like activities. Caregivers were overloaded with their activities. They care for the patient; most of the time generate income, and care for other family members.
This study has certain limitations; First, additional analysis to establish causal inferences was not feasible because of the cross-sectional nature of the study. Second, data was limited to only cancer patients related to the depression of caregivers, making it difficult to extrapolate to other causes of caregivers’ depression. Third the validity of the instruments utilized in this study to measure the outcome variables was not assessed.
Conclusion
This study aimed to assess the prevalence of depression and its associated factors among caregivers of cancer patients. We found that the prevalence of depression among caregivers of cancer patients was high. Long caring hours, small household size, low income level, and higher burden level were independent factors of caregiver depression, indicating the urgent necessity to investigate and deal with it through interdisciplinary approaches. Caregivers of cancer patients need prevention, screening, and management of depression. We recommend that we establish an organization to work on the psychological wellness of caregivers and depression screening for caregivers.
Data availability
All data generated or analysed during this study are included in this article.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- COR:
-
Crude Odds Ratio
- CRA:
-
Caregivers Reaction Assessment
- ECOG:
-
Eastern Cooperative Oncology Group
- PHQ:
-
Patient Health Questionnaire
- ZBI:
-
Zarit Burden Interview
References
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53.
Nakaya N, Saito-Nakaya K, Bidstrup PE, Dalton SO, Frederiksen K, Steding-Jessen M, et al. Increased risk of severe depression in male partners of women with breast cancer. Cancer. 2010;116(23):5527–34.
Dent J, Manner CK, Milner D, Mutebi M, Ng A, Olopade OI et al. Africa’s emerging cancer crisis: a call to action. 2017;(June):1–8.
Federal Ministry of Health E. National cancer control plan of Ethiopia, 2016–2020. October 2015. 2015.
Kurtz ME, Kurtz JC, Given CWGB. Depression and physical health among family caregivers of geriatric patients with cancer – a longitudinal view. Med Sci Monit. 2004;10(8):447–57.
Weitzner MA, Haley WECH. The family caregiver of the older cancer patient. Hematol Clin North Am ·. 2000;14(October).
Given B, Wyatt G, Given C, Sherwood P, Gift A, DeVoss D, et al. Burden and depression among caregivers of patients with cancer at the end of life. Oncol Nurs Forum. 2004;31(6):1105–17.
Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Semin Oncol Nurs. 2012;28(4):236–45.
Mollica MA. The role of medical / nursing skills training in caregiver confidence and burden: a CanCORS study. 2017.
Chai YC, Mahadevan R, Ng CG, Chan LF, Md Dai F. Caregiver depression: the contributing role of depression in patients, stigma, social support and religiosity. Int J Soc Psychiatry. 2018;64(6):578–88.
Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119(SUPPL11):2160–9.
Wilson-genderson ÃLAS Jr. SB. Depressive symptoms in lung cancer patients and their family caregivers and the influence of family environment. 2010;1293(January):1285–93.
Rivera HR Jr., ACNP-BC MS. Depression symptoms in cancer caregivers. Clin J Oncol Nurs. 2008;13(2):195–202.
Trevino KM, Prigerson HG, Maciejewski PK. Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psychooncology. 2018;27(1):243–9.
Wadhwa D, Burman D, Swami N, Rodin G, Lo C, Zimmermann C. Quality of life and mental health in caregivers of outpatients with advanced cancer. Psychooncology. 2013;410(December 2011):403–10.
Pitceathly CMP. The psychological impact of cancer on patients’ partners and other key relatives_ a review - ScienceDirect. Eur J Cancer. 2003;39(11):1517–24.
Kim Y, Carver CS, Rocha-Lima C, Shaffer KM. Depressive symptoms among caregivers of colorectal cancer patients during the first year since diagnosis: a longitudinal investigation. Psychooncology. 2013;22(2):362–7.
Öven Ustaalioğlu BB, Acar E. The depression and related factors among cancer patients and their family caregivers in Turkish population. Acta Oncol Turc. 2017;50(2):115–23.
Ayabakan-cot D, Ates E, Kurt B, Nazlican E, Akbaba M. Investigation of depression and quality of life factors in cancer patients’ Caregivers. 2017;22(2):524–9.
Yusuf AJ, Adamu A, Nuhu FT. Caregiver burden among poor caregivers of patients with cancer in an urban African setting. Psychooncology. 2011;20(8):902–5.
Lkhoyaali S, Haj MA, El OF, El, Layachi M, Ismaili N, Mrabti H, et al. The burden among family caregivers of elderly cancer patients: prospective study in a Moroccan population. BMC Res Notes. 2015;8(1):1–4.
Mystakidou K, Tsilika E, Parpa E, Galanos A, Vlahos L. Caregivers of advanced cancer patients: feelings of hopelessness and depression. Cancer Nurs. 2007;30(5):412–8.
Nijboer C, Triemstra M, Tempelaar R, Mulder M, Sanderman R. Van den Bos GAM. Patterns of caregiver experiences among partners of cancer patients. Gerontologist. 2000;40(6):738–46.
Siegel K, Karus DG, Raveis VH, Christ GHMF. Depressive distress among the spouses of terminally ill cancer patients. Cancer practice. Cancer Pract. 1996;4(1):25–30.
Hudson PL, Thomas K, Trauer T, Remedios C, Clarke D. Psychological and social profile of family caregivers on commencement of palliative care. J Pain Symptom Manage. 2011;41(3):522–34.
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):1–10.
Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Soc Psychiatry Psychiatr Epidemiol. 2005;40(6):439–45.
Safaeian Z, Sadat Hejazi S, Delavar E, Hoseini Azizi T, HaresAbadi M. The relationship between caregiver burden, and depression, anxiety and stress in family caregivers of cancer patients referred to Imam Reza Hospital in Bojnurd City. Iran J Psychiatr Nurs. 2017;5(3):7–14.
Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients. Cancer J. 2010;60(5):317–39.
Seid S, Demilew D, Yimer S, Mihretu A. Prevalence and associated factors of mental distress among caregivers of patients with epilepsy in Ethiopia: a cross-sectional study design. Psychiatry J. 2018;2018:1–8.
Derajew H, Tolessa D, Feyissa GT, Addisu F, Soboka M. Prevalence of depression and its associated factors among primary caregivers of patients with severe mental illness in southwest, Ethiopia. 2017;1–8.
Martin A, Rief W, Klaiberg A, Braehler E. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28(1):71–7.
Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–61.
Ojifinni OO, Uchendu OC. Validation and reliability of the 12-item Zarit burden interview among informal caregivers of elderly persons in Nigeria. Arch Basic Appl Med. 2018;6(1):45–9.
Memirie STKM, Asefa Mathewos Tefera Biniyam, Getamesay A, Woldetinsae Mihiret TB. Ababi Girma JATRRVS. Estimates of Cancer incidence in Ethiopia in 2015 using Population-based Registry Data. J Glob Oncol 2018;41–11. 2019.
Katende G, Nakimera L, Katende G. Prevalence and correlates of anxiety and depression among family carers of cancer patients in a cancer care and treatment facility in Uganda: a cross-sectional study. Afr Heal Sci. 2017;17(3):868–76.
Park B, Kim SY, Shin JY, Sanson-Fisher RW, Shin DW, Cho J, et al. Prevalence and predictors of anxiety and depression among family caregivers of cancer patients: a nationwide survey of patient-family caregiver dyads in Korea. Support Care Cancer. 2013;21(10):2799–807.
Ambigga DK, Sherina M. Suthahar a. depression and anxiety among family caregivers of cancer patients in an oncology clinic. Malaysian J Psychiatry. 2005;13(6):35–42.
Turner D, Adams E, Boulton M, Harrison S, Khan N, Rose P, et al. Partners and close family members of long-term cancer survivors: health status, psychosocial well-being and unmet supportive care needs in UK hospitals. Psychooncology. 2013;22(1):12–9.
United Nations, Department of Economic and Social, Affairs PD. Household size and composition around the world 2017. United Nation. 2017;2:4.
Nezu AM, Nezu CM, Felgoise SHZM. Psychosocial oncology. Heal Psychol. 2003;9:267–92.
Acknowledgements
The authors thank the Hospital authority, the Department of Nursing, data collectors, and the record office for their generous support during the entire period of this study. We would like also to acknowledge Addis Ababa University for a preprint that has previously been published.
Funding
The authors were not funded for this work.
Author information
Authors and Affiliations
Contributions
GD and BB Conceptualized the study: All were involved in the data curation, methodology, project administration, and analysis. GD and BT were involved in the visualization; GD and BB took part in the Writing of the original draft GD and BB reviewed & edited and all were involved in the manuscript preparation.
Corresponding author
Ethics declarations
Ethics statement
The official clearance later (Ref No. NUR.133/19) was obtained from the research and ethics committee (REC) of the School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University. After explaining the purpose and possible benefit of the study, oral and written informed consent was obtained from the caregiver before starting the procedure. Permission to access the patients’ records was granted from hospital officials Patient information was anonymous and kept confidential.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Demissie, G., Balta, B. Prevalence of depression and associated factors among primary caregivers of adult cancer patients, Sidama region Southern Ethiopia: cross-sectional study. BMC Nurs 23, 384 (2024). https://doi.org/10.1186/s12912-024-02061-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02061-1