Abstract
Background
The temporomandibular joint (TMJ) is a complex joint that facilitates mandibular movements during speech, chewing, and swallowing activities. The Axis I evaluation of the DC/TMD focuses on assessing physical diagnoses related to TMDs. It includes an assessment of pain and functional limitations, such as jaw opening range, joint sounds, and joint tenderness. The Axis II evaluation of the DC/TMD provides information on the patient’s psychological status and quality of life. This Systematic Review with Meta-Analysis aimed to evaluate the accuracy of Temporomandibular Disorders diagnosis considered through the Diagnostic Criteria for Temporomandibular Disorder (DC/TDM) axis II compared to the Axis I evaluations.
Methods
A search was made in PubMed, Web of Science and Lilacs for articles published from the inception until 20 January 2023. We applied the Population, Exposure, Comparator, and Outcomes (PECO) model [1] to assess document eligibility. Only studies that evaluated patients by DC/TMD Axis I and Axis II were considered. Review Manager version 5.2.8 (Cochrane Collaboration) was used for the pooled analysis. We measured the odds ratio (OR) between the two groups (Axis I and Axis II).
Results
Fifty-one articles were selected because of the search. Four papers were excluded before the screening: 2 pieces were not in English, and two were reviewed. The remaining 47 articles were selected for the title and abstract screening to evaluate whether they met the PECO criteria. Among these, four papers were established; the overall effect showed that there was no difference in TMD diagnosis between Axis I and Axis II (RR 1.17; 95% CI: 0.80– 1.71; Z:0.82; P = .41), suggesting that there is no difference between Axis I and Axis II.
Conclusion
In conclusion, DC/TMD is an effective tool for the diagnosis of TMD. It improves the accuracy of TMD diagnosis, allows for the classification of subtypes, and assesses psychosocial factors that may impact the development or maintenance of TMD symptoms.
Similar content being viewed by others
Introduction
The temporomandibular joint (TMJ) is a complex joint that facilitates mandibular movements during speech, chewing, and swallowing activities. Temporomandibular disorders (TMDs) affect the TMJ and its associated muscles and structures, resulting in pain, dysfunction, and other symptoms. Diagnosing TMDs can be challenging due to their varied etiologies and clinical presentations [2, 3].
To address this challenge, the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) was developed in the early 1990s. Since then, the diagnostic criteria have been updated, and the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) were published in 2014. The DC/TMD is a comprehensive, standardized diagnostic tool that includes both an Axis I and an Axis II evaluation [4,5,6,7,8,9,10,11,12,13].
The Axis I evaluation of the DC/TMD focuses on assessing physical diagnoses related to TMDs. It includes an assessment of pain and functional limitations, such as jaw opening range, joint sounds, and joint tenderness. Additionally, it consists of evaluating parafunctional habits, such as clenching and grinding, and occlusal factors, such as dental malocclusion [14,15,16,17,18,19,20,21].
In contrast, the Axis II evaluation of the DC/TMD assesses the psychosocial aspects of TMDs, such as anxiety, depression, and quality of life. The Axis II evaluation includes self-report questionnaires and interviews that evaluate the patient’s emotional status, pain-related disability and the impact of the TMD on their daily activities [22,23,24,25,26,27,28,29,30,31,32,33].
The DC/TMD has been widely accepted and implemented in clinical and research settings to improve the accuracy and consistency of TMD diagnosis. By including both Axis I and Axis II evaluations, the DC/TMD allows for a comprehensive review of the patient’s condition, leading to a more personalized and effective treatment approach.
The DC/TMD has been shown to have high validity and reliability in various populations, including children, adults, and older adults. It has also been used in studies investigating the prevalence and risk factors of TMDs and the effectiveness of various treatment modalities.
One of the key differences between the Axis I and Axis II evaluations is that the Axis I evaluation focuses on physical diagnoses. In contrast, the Axis II evaluation focuses on psychosocial factors. This reflects the multifactorial nature of TMDs, often influenced by physical and psychological factors [34].
The Axis I evaluation of the DC/TMD provides essential information on the nature and severity of the patient’s physical symptoms. This information can help guide the selection of appropriate treatment modalities, such as medication, physical therapy, or splint therapy. The Axis I evaluation can also help identify any underlying physical conditions contributing to the patient’s TMD symptoms, such as arthritis or joint degeneration.
The Axis II evaluation of the DC/TMD provides information on the patient’s psychological status and quality of life. This information can identify any underlying psychosocial factors contributing to the patient’s TMD symptoms, such as anxiety, depression, or stress. Addressing these psychosocial factors can help improve the patient’s overall well-being and response to treatment [35].
In conclusion, the DC/TMD is a comprehensive and standardized diagnostic tool that includes both an Axis I and an Axis II evaluation. The DC/TMD has been widely accepted and implemented in clinical and research settings and has been shown to have high validity and reliability. The Axis I and Axis II evaluations provide essential information on the physical and psychosocial aspects of TMDs, respectively, allowing for a more personalized and effective treatment approach [36].
This Systematic Review with Meta-Analysis aimed to evaluate the accuracy of Temporomandibular Disorders diagnosis considered through the Diagnostic Criteria for Temporomandibular Disorder (DC/TDM) axis II compared to the Axis I evaluations.
Materials and methods
Eligibility criteria
The PECO is the following:
-
P) Participants consisted of the population.
-
E) The Exposure consisted of Temporomandibular Disorders.
-
C) The Comparison consisted of Temporomandibular Disorders diagnosis evaluated through the Diagnostic Criteria for Temporomandibular Disorder (DC/TDM) axis II compared to the Axis I evaluations.
-
O) The Outcome consisted of the Accuracy of Temporomandibular Disorders diagnosis evaluated through the Diagnostic Criteria for Temporomandibular Disorder (DC/TDM) axis II compared to the Axis I evaluations.
Search strategy
The Search were made in PubMed, Web of Science and Scopus until May 1, 2023. Table 1 reports the complete keywords used for the search.
The systematic review has been registered in PROSPERO with CRD42022327470.
Data extraction
The following data were extracted: (1) First author; (2) Year of publication; (3) Nationality; (4) Number of study participants (5) Age of study participants (case vs. controls); (6) Diagnostic criteria/tools used for the diagnosis of TMD; (7) Correlation between Axis I and II (8) Significance of the study.
Quality assessment
The bias were evaluated using RoB2 by Cochrane. Two reviewers evaluated the possible bias using six domains.
Statistical analysis
The statistical analysis was performed using Review Manager version 5.2.8. We measured the difference between Axis I and Axis II.
Results
Study characteristics
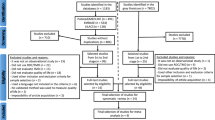
Four studies were included in the systematic review and were considered for the metanalysis, as illustrated in the PRISMA 2020 flowchart in Fig. 1. The included studies have been published between 2022 and 2023. The four included studies were Prospective studies in design or retrospective studies. All of these studies compare the effectiveness of DC/TMD Axis I with DC/TMD Axis II to assess how they can be interchangeable in some cases and how TMDs are caused not only by physiological issues but also by a psycho-social component. The data extracted from each study, as reported in the paragraph “data extraction”.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: https://doi.org/10.1136/bmj.n71
Main findings
The included subjects in this review were 773. The ‘average age of the study participants is 35 years old. All patients were evaluated and underwent DC/TMD Axis I, followed by Axis II.
Alrashdan evaluated and compared Axis I with Axis II. By the Axis I DC/TMD procedure, 98 TMD patients had their pain-related disabilities, psychological distress, and stress reactivity evaluated. One third of patients (32%) had high levels of pain-related impairment, and just over half of patients (49%) had high levels of distinctive pain (self-reported TMJ-related pain). Furthermore, most patients (41% and 39%) reported moderate to severe distress and stress reactivity. The Graded Chronic Pain Scale (GCPS) and the pain-related TMD subgroups were significantly correlated [37]. Winocur-Arias compared the effectiveness of DC/TMD in diagnosing local myalgia and myofascial pain using Axis I and Axis II. All consecutive TMD patients who received a DC/TMD diagnosis at our facility between 2015 and 2018 were included in this retrospective analysis. Patients with local myalgia and myofascial pain with referral were compared regarding their Axis I and II results. Statistical significance was defined as a p-value of 0.05. The study involved 255 patients, 114 with local myalgia and 83 with myofascial pain with referral, with a mean age of 37.8 15.34 years. In the latter group, there were significantly greater levels of sadness, non-specific physical symptoms, headaches attributed to TMD (HAattrTMD), and characteristic pain intensity (CPI) [38]. Reiter’s study compared the effectiveness of diagnosing TMD headaches using Axis I and II. This retrospective analysis included 220 patients with painful TMD—60 with and 160 without HAattrTMD—. The patients’ Axis I and II scores were compared using the Diagnostic Criteria for TMD (DC/TMD). Statistical significance was defined as a P value of 0.05. Results: A diagnosis of HAattrTMD was given to 27.3% of the patients. Local myalgia was significantly more prevalent in the non-HAattrTMD group (P 0.001), but myofascial pain with referral was much more commonplace in the HAattrTMD group (P 0.001). The HAattrTMD group had significantly greater levels of depressive symptoms (P = .002), nonspecific physical symptoms (P = .004), graded chronic pain (P = .008), and pain catastrophizing (P = .013), as well as characteristic pain intensity (P = .003). HAattrTMD was positively correlated with non-specific physical symptoms (odds ratio [OR] = 1.098, 95% CI = 1.006 to 1.200, P = .037). A negative correlation existed between local myalgia and HAattrTMD (OR = 0.295, 95% CI = 0.098 to 0.887, P = .030) [39]. Yildiz’s study aims to assess the frequency of DC / TMD diagnoses among people with internal TMJ derangements. Two hundred adults over 18 with internal derangements. Axis I and II of the Diagnostic Criteria for Temporomandibular Disorders (DC / TMD) were used. There were 3.6 times as many female patients as male patients (156 versus 44). The likelihood of internal TMJ derangement in the right or left TMJ did not significantly correlate with gender, age, educational attainment, marital status, or occupation (p > .05).TMJ internal disorder and Axis II scores correlate significantly (p 0.05). Left TMJ internal dysfunction significantly correlates with GAD 7 and PHQ 4 scores (p 0.05) [40]. All results are represented in the Table 2.
Meta-analysis
The included studies had a high heterogeneity (I2 = 84%). Therefore the meta-analysis was conducted by random model effect. We considered as an outcome the difference in the diagnosis of TMD between Axis I and Axis II.
The overall effect, reported in the forest plot (Fig. 2), showed that there was no difference in In the accuracy between Axis I and Axis II for the diagnosis of TMD (RR 1.17; 95% CI: 0.80– 1.71; Z:0.82; P = .41), suggesting that there is no difference between Axis I and Axis II.
Quality assessment and risk of bias
The risk of bias in the included studies was reported in Fig. 3. Regarding the randomization process, all studies had a low risk of bias, and allocation concealment had a high chance. Only three studies excluded a performance; two studies ensured an increased risk of detection bias (self-reported outcomes), and 3 of the included studies present low detection bias (Fig. 3).
Discussion
Temporomandibular disorders (TMD) are a group of conditions affecting the temporomandibular joint (TMJ) and surrounding structures, which can cause pain and dysfunction. The Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) is a comprehensive tool developed to aid in diagnosing TMD. This scientific discussion will describe the use of DC/TMD in temporomandibular diagnosis and discuss the differences between the Axis I and Axis II evaluations [41].
A collaboration of international experts developed DC/TMD, and is currently the most widely used and accepted tool for diagnosing TMD. The diagnostic criteria are organized into two axes: Axis I evaluates the physical examination and clinical history. In contrast, Axis II considers psychosocial factors that may contribute to the development or maintenance of TMD [42,43,44].
The Axis I evaluation includes the patient’s physical examination and clinical history. The physical examination involves assessing the patient’s TMJ, masticatory muscles, and occlusion. Clinical history includes collecting information on the patient’s pain and function, including the duration, intensity, and location of pain and any limitations in jaw movement [45].
The Axis II evaluation assesses psychosocial factors that may influence the development or maintenance of TMD. This includes collecting information on the patient’s anxiety, depression, pain catastrophizing, and quality of life. This evaluation helps identify any psychosocial factors that may require treatment alongside the physical symptoms of TMD.
The use of DC/TMD has several benefits, including standardized diagnostic criteria, improved communication between healthcare professionals, and improved patient management. DC/TMD can aid in accurate diagnosis and treatment planning, improving patient outcomes [46].
In conclusion, DC/TMD is a comprehensive tool for diagnosing TMD. Axis I and II evaluations provide a thorough assessment of the patient’s physical symptoms and psychosocial factors. Implementing DC/TMD can aid in accurately diagnosing and treating TMD, leading to improved patient outcomes [47].
Furthermore, there is a need for continued research to validate the tool’s effectiveness and improve its utility. More studies are needed to assess the reliability and validity of DC/TMD in different populations, such as children and elderly patients, and to investigate its sensitivity and specificity for diagnosing TMD [48, 49].
In conclusion, the DC/TMD is a comprehensive tool that aids in accurately diagnosing and treating TMD by assessing physical and psychosocial factors. While its use has some limitations, its benefits make it an essential tool in diagnosing and managing TMD. Ongoing research is necessary to refine and validate the device, leading to better patient outcomes in the future.
Several studies have evaluated the effectiveness of DC/TMD in diagnosing TMD [50, 51]. A systematic review of 38 studies found that DC/TMD had a high diagnostic accuracy in identifying patients with TMD, with a sensitivity of 0.85 and a specificity of 0.80 [52]. Another study found that using DC/TMD improved the accuracy of TMD diagnosis and reduced misclassification rates compared to non-standardized diagnostic criteria.
In addition to improving the accuracy of TMD diagnosis, DC/TMD has also led to a better understanding of the different subtypes of TMD. Axis I evaluation assesses physical factors, including joint or muscle pain, jaw dysfunction, and malocclusion. Based on the results of Axis I evaluation, patients can be classified into subtypes, including muscle disorder, joint disorder, or a combination of both. This classification system allows for a more targeted and effective treatment plan for each subtype of TMD [53].
Axis II evaluation assesses psychosocial factors, such as anxiety, depression, and pain catastrophizing. These factors may impact the development, progression, or maintenance of TMD symptoms. By including Axis II evaluation in TMD diagnosis, healthcare professionals can develop a comprehensive treatment plan that addresses physical and psychosocial factors. This approach has improved patient outcomes, such as reduced pain and improved quality of life [54, 55]. Effective management of TMDs requires an integrated approach that considers both Axis 1 and Axis 2 findings. Treatments may include:
Physical Therapies: Such as physical therapy exercises, massage, and the application of heat or cold.
Dental Interventions: Including occlusal appliances (mouthguards) to reduce clenching and grinding, and corrective dental treatments to address bite abnormalities.
Medications: Pain relievers, muscle relaxants, or anti-inflammatory drugs to manage symptoms.
Behavioral Therapies: Cognitive-behavioral therapy (CBT) and stress management techniques to address psychological and behavioral factors.
Education and Self-care: Teaching patients about their condition and strategies to manage symptoms, such as relaxation techniques and posture correction.
In conclusion, the axis 1 and axis 2 classification system for TMDs facilitates a comprehensive diagnostic approach, allowing healthcare providers to address the multifaceted nature of these disorders. By considering both the physical and psychosocial dimensions of TMDs, clinicians can develop more effective, personalized treatment plans, ultimately improving outcomes for patients suffering from these complex conditions.
Limitations of this study
In this meta-analysis, only symptoms such as headache and internal damage of TMJ and not the complexity of TMD symptoms were considered in the studies only. Only Alrashdan’s study evaluated all types of TMD symptoms by comparing Axis I with Axis II. Therefore the results of the meta-analysis show high heterogeneity for this reason. Also, there could be, as shown in the various studies, some symptoms more associated with the psychological aspect and other symptoms less associated with the psychological aspect. In these cases, Axis II would give false negatives. Therefore, more studies taking into account single symptomatology are needed to correlate Axis I with Axis II effectively.
Conclusion
In conclusion, DC/TMD is an effective tool for diagnosing TMD. It improves the accuracy of TMD diagnosis, allows for the classification of subtypes, and assesses psychosocial factors that may impact the development or maintenance of TMD symptoms. By comprehensively setting physical and psychosocial factors, DC/TMD can lead to a more targeted and effective treatment plan, improving patient outcomes.
Data availability
The data will be available on reasonable request from the corresponding author.
References
Morgan RL, Whaley P, Thayer KA, Schünemann HJ. Identifying the PECO: a framework for formulating good questions to explore the association of environmental and other exposures with health outcomes. Environ Int. 2018;121(Pt 1):1027–31.
Dimitroulis G. Management of temporomandibular joint disorders: a surgeon’s perspective. Aust Dent J. 2018;63(Suppl 1):79–90.
Kalladka M, Young A, Thomas D, Heir GM, Quek SYP, Khan J. The relation of temporomandibular disorders and dental occlusion: a narrative review. Quintessence Int. 2022;53(5):450–9.
Easterbrook S, Keys J, Talsma J, Pierce-Talsma S. Osteopathic manipulative treatment for Temporomandibular disorders. J Am Osteopath Assoc. 2019;119(6):e29–30.
Choi S, Kang YS, Yeo ISL. Influence of Implant–Abutment Connection Biomechanics on Biological Response: A Literature Review on Interfaces between Implants and Abutments of Titanium and Zirconia. Prosthesis [Internet]. 2023;5(2):527–38. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85163744250amp;doi=10.3390%2fprosthesis5020036amp;partnerID=40amp;md5=aefc7b44f87fbad41c2c5d9ee7c9ca89.
Rapani A, Berton F, Tramontin A, Turco G, Marchesi G, Di Lenarda R et al. Surface Roughness of Enamel and Dentin after Preparation Finishing with Rotary Burs or Piezoelectric Instruments. Prosthesis [Internet]. 2023;5(3):711–20. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85172778398amp;doi=10.3390%2fprosthesis5030050amp;partnerID=40amp;md5=81eb3123240119b35e4932f6d20ab0f4.
Ramadanov N, Marinova-Kichikova P, Hable R, Dimitrov D, Becker R. Comparison of Postoperative Serum Biomarkers after Total Hip Arthroplasty through Minimally Invasive versus Conventional Approaches: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Prosthesis [Internet]. 2023;5(3):694–710. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85172900513amp;doi=10.3390%2fprosthesis5030049amp;partnerID=40amp;md5=f2c6464404446b043c4e90619a4ae403.
Russell J, Bergmann JHM. Real-Time Intent Sensing for Assistive Devices with Implications for Minimising Maintenance. Prosthesis [Internet]. 2023;5(2):453–66. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85163723053amp;doi=10.3390%2fprosthesis5020031amp;partnerID=40amp;md5=345458d3fce72da21fc99f0c29c5ce03.
Carossa M, Scotti N, Alovisi M, Catapano S, Grande F, Corsalini M et al. Management of a Malpractice Dental Implant Case in a Patient with History of Oral Bisphosphonates Intake: A Case Report and Narrative Review of Recent Findings. Prosthesis [Internet]. 2023;5(3):826–39. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85172931273amp;doi=10.3390%2fprosthesis5030058amp;partnerID=40amp;md5=3aa293cf5e3754c2c29466779dac9d88.
Singh K, Rajoria S, Kumar P, Urs AB. Potential role of mast cells and eosinophils in establishing the clinical severity of oral lichen planus. Minerva Dental and Oral Science [Internet]. 2023;72(3):137–43. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85163898694amp;doi=10.23736%2fS2724-6329.23.04726-5amp;partnerID=40amp;md5=962a6b0f2b1d9edfd56acaac921d923a.
Chandan C, Shetty SK, Shetty SK, Shah AK. Quality of life assessment in patients with long-term neurosensory dysfunction after mandibular fractures. Minerva Dental and Oral Science [Internet]. 2023;72(2):118–23. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85152312536amp;doi=10.23736%2fS2724-6329.21.04462-9amp;partnerID=40amp;md5=a3217c3b938e69cac0dbf5ad3a9dad69.
Rosa A, Miranda M, Franco R, Guarino MG, Barlattani A, Bollero P. Experimental protocol of dental procedures in patients with hereditary angioedema: the role of anxiety and the use of nitrogen oxide. Oral Implantol (Rome). 2016;9:49–53. https://doi.org/10.11138/orl/2016.9.2.049.
Franco R, Gianfreda F, Miranda M, Barlattani A, Bollero P. The hemostatic properties of chitosan in oral surgery. Biomedical Biotechnol Res J (BBRJ). 2020;4(3):186.
Cigdem Karacay B, Sahbaz T. Investigation of the relationship between probable sleep bruxism, awake bruxism and temporomandibular disorders using the Diagnostic Criteria for Temporomandibular disorders (DC/TMD). Dent Med Probl. 2023;60(4):601–8.
González-Sánchez B, García Monterey P, Ramírez-Durán M, del Garrido-Ardila V, Rodríguez-Mansilla EM, Jiménez-Palomares J. Temporomandibular Joint dysfunctions: a systematic review of treatment approaches. J Clin Med. 2023;12(12):4156.
Orzeszek SM, Piotr S, Waliszewska-Prosół M, Jenca A, Osiewicz M, Paradowska -Stolarz A, et al. Relationship between pain severity, satisfaction with life and the quality of sleep in Polish adults with temporomandibular disorders. Dent Med Probl. 2023;60(4):609–17.
Boening K, Wieckiewicz M, Paradowska-Stolarz A, Wiland P, Shiau YY. Temporomandibular disorders and oral parafunctions: mechanism, Diagnostics, and Therapy. Biomed Res Int. 2015;2015:1–2.
Dovigo S, Massariol M, Gandini A, Zuffellato N. Instantaneous dental implant loading technique by fixed dentures: A retrospective cohort study. Dent Med Probl [Internet]. 2023;60(3):375–83. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85171232256amp;doi=10.17219%2fdmp%2f154981amp;partnerID=40amp;md5=22af0fa6ef3f1085cdd8dbb409088c8c.
Sanjuán-Navarro PS, Agudelo-Suárez AA, Mora-Cárdenas AL, Angarita-Navarro MP, Valdés-Payares L, Martínez-Gómez ML et al. Frequency of symptoms and the associated factors of eating disorders in a group of dental students in Medellín, Colombia. Dent Med Probl [Internet]. 2023;60(3):401–11. https://doi.org/10.17219/dmp/149900.
Soundarajan S, Rajasekar A. Antibacterial and anti-inflammatory effects of a novel herb-mediated nanocomposite mouthwash in plaque-induced gingivitis: A randomized controlled trial. Dent Med Probl [Internet]. 2023;60(3):445–51. https://doi.org/10.17219/dmp/150728.
Paradowska-Stolarz AM, Wieckiewicz M, Mikulewicz M, Malysa A, Dus-Ilnicka I, Seweryn P et al. Comparison of the tensile modulus of three 3D-printable materials used in dentistry. Dent Med Probl [Internet]. 2023;60(3):505–11. https://doi.org/10.17219/dmp/166070.
Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am. 2013;57(3):465–79.
Lucchese A, Dolci A, Minervini G, Salerno C, DI Stasio D, Minervini G, Laino L, Silvestre F, Serpico R. Vulvovaginal gingival lichen planus: report of two cases and review of literature. Oral Implantol (Rome). 2016;9:54–60. https://doi.org/10.11138/orl/2016.9.2.054.
Minervini G, Nucci L, Lanza A, Femiano F, Contaldo M, Grassia V. Temporomandibular disc displacement with reduction treated with anterior repositioning splint: a 2-year clinical and magnetic resonance imaging (MRI) follow-up. J Biol Regul Homeost Agents. 2020;34:151–160. DENTAL SUPPLEMENT.
Antonelli A, Bennardo F, Brancaccio Y, Barone S, Femiano F, Nucci L, Minervini G, Fortunato L, Attanasio F, Giudice A. Can bone compaction improve primary implant stability? An in vitro comparative study with osseodensification technique. Appl Sci. 2020;10:8623. https://doi.org/10.3390/app10238623.
Li H, Shen D, Chen Z, Li J. Step-back anterior repositioning splint retraction for temporomandibular joint disc displacement with reduction in adult patients. J Oral Rehabil [Internet]. 2023;50(10):965–71. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85162731331amp;doi=10.1111%2fjoor.13485amp;partnerID=40amp;md5=050674a3564c72016eb7a2e9e60f4f41.
El-Shaheed NH, Mostafa AZH, Aboelez MA. Efficacy of stabilisation splint and low-level laser therapy for patients with chronic closed lock from non-reducible displaced temporo-mandibular joint discs: A parallel randomised clinical trial. J Oral Rehabil [Internet]. 2023;50(3):177–93. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85145688549amp;doi=101111%2fjoor.13405amp;partnerID=40amp;md5=a4ff033e549028421d6b50a936413121.
Serrano-Hernanz G, Angulo-Carrere T, Ardizone-García I, Svensson P, Álvarez-Méndez AM. Pressure release technique versus placebo applied to cervical and masticatory muscles in patients with chronic painful myofascial temporomandibular disorder: A randomised clinical trial. J Oral Rehabil [Internet]. 2023;50(9):782–91. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85160649682amp;doi=10.1111%2fjoor.13490amp;partnerID=40amp;md5=5dca942f35eed71cd3003c84ff82d168.
Hua J, Fan X, Nie X, He D. Preliminary evaluation of Kovacs digital occlusal splint in the treatment of temporomandibular disorders: A single-centre, cross-sectional study. J Oral Rehabil [Internet]. 2023;50(8):687–97. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85156210537amp;doi=101111%2fjoor.13466amp;partnerID=40amp;md5=ebdf96a348679547075e5b00f011aa79.
Bracci A, Lobbezoo F, Colonna A, Bender S, Conti PCR, Emodi-Perlman A et al. Research routes on awake bruxism metrics: Implications of the updated bruxism definition and evaluation strategies. J Oral Rehabil [Internet]. 2023; Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85162055444amp;doi=10.1111%2fjoor.13514amp;partnerID=40amp;md5=8929c2aa4afd27bb0be298c180e897df.
Watanabe T, Sieg M, Lunde SJ, Persson M, Taneja P, Baad-Hansen L et al. Nocebo response in dentistry: A systematic review and meta-analysis of adverse events in analgesic trials of third molar removal. J Oral Rehabil [Internet]. 2023;50(4):332–42. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85147213142amp;doi=101111%2fjoor.13414amp;partnerID=40amp;md5=b38192cc874a88fdf950e913b831d1ef.
Karpuz S, Yılmaz R, Yılmaz H. Evaluation of temporomandibular joint dysfunction in traumatic brain injury patients. J Oral Rehabil. 2023;50(6):476–81.
Farook TH, Dudley J. Automation and deep (machine) learning in temporomandibular joint disorder radiomics: A systematic review. J Oral Rehabil [Internet]. 2023;50(6):501–21. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85150507733amp;doi=10.1111%2fjoor.13440amp;partnerID=40amp;md5=7551d0758e36ed693d7557495cb4ea00.
Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician. 2015;91(6):378–86.
Restrepo C, Ortiz AM, Henao AC, Manrique R. Association between psychological factors and temporomandibular disorders in adolescents of rural and urban zones. BMC Oral Health. 2021;21(1):140.
Greene CS, Manfredini D. Transitioning to chronic temporomandibular disorder pain: a combination of patient vulnerabilities and iatrogenesis. J Oral Rehabil. 2021;48(9):1077–88.
Alrashdan MS, Al-Omiri MK. Psychosocial profiles and their correlation with physical diagnosis in temporomandibular disorders, a preliminary report. CRANIO®. 2022;1–9.
Winocur-Arias O, Friedman-Rubin P, Abu Ras K, Lockerman L, Emodi-Perlman A, Greenbaum T, et al. Local myalgia compared to myofascial pain with referral according to the DC/TMD: Axis I and II results. BMC Oral Health. 2022;22(1):27.
Reiter S, Emodi-Perlman A, Kasiel H, Abboud W, Friedman-Rubin P, Arias OW et al. Headache attributed to Temporomandibular disorders: Axis I and II findings according to the Diagnostic Criteria for Temporomandibular disorders. J Oral Facial Pain Headache 35(2):119–28.
Yildiz S, Balel Y, Tumer MK. Evaluation of prevalence of temporomandibular disorders based on DC / TMD Axis I diagnosis in Turkish population and correlation with Axis II. J Stomatol Oral Maxillofac Surg. 2023;124(1S):101303.
Reiter S, Eli I, Mahameed M, Emodi-Perlman A, Friedman-Rubin P, Reiter MA, et al. Pain Catastrophizing and Pain Persistence in Temporomandibular Disorder patients. J Oral Facial Pain Headache. 2018;32(3):309–20.
Pihut M, Gala A, Kulesa-Mrowiecka M. Temporomandibular disorders and their impact on the development of the overloading changes within temporomandibular joints. Folia Med Cracov. 2022;62(4):45–56.
Minervini G, Marrapodi MM, Cicciù M. Online bruxism‐related information: can people understand what they read? A cross‐sectional study. J Oral Rehabil. 2023;50:1211–16. https://doi.org/10.1111/joor.13519.
Minervini G, Franco R, Marrapodi MM, Fiorillo L, Cervino G, Cicciù M. The association between parent education level, oral health, and oral-related sleep disturbance. An observational crosssectional study. Eur J Paediatr Dent. 2023;24:218–23. https://doi.org/10.23804/ejpd.2023.1910.
Rongo R, Ekberg E, Nilsson IM, Al-Khotani A, Alstergren P, Rodrigues Conti PC, et al. Diagnostic criteria for temporomandibular disorders in children and adolescents: an international Delphi study-part 2-Development of Axis II. J Oral Rehabil. 2022;49(5):541–52.
Alrashdan MS, Al-Omiri MK. Psychosocial profiles and their correlation with physical diagnosis in temporomandibular disorders, a preliminary report. Cranio. 2022;1–9.
Günther T, Schierz O, Hahnel S, Rauch A. Field-testing a psychosocial assessment scoring form for TMD patients - summarizing axis II instruments. BMC Oral Health. 2020;20(1):267.
Mijiritsky E, Winocur E, Emodi-Perlman A, Friedman-Rubin P, Dahar E, Reiter S. Tinnitus in Temporomandibular disorders: Axis I and Axis II findings according to the Diagnostic Criteria for Temporomandibular disorders. J Oral Facial Pain Headache 34(3):265–72.
Hietaharju M, Kivimäki I, Heikkilä H, Näpänkangas R, Teerijoki-Oksa T, Tanner J, et al. Comparison of Axis II psychosocial assessment methods of RDC/TMD and DC/TMD as part of DC/TMD-FIN phase II validation studies in tertiary care Finnish TMD pain patients. J Oral Rehabil. 2021;48(12):1295–306.
Paunonen J, Helminen M, Sipilä K, Peltomäki T. Temporomandibular disorders in class II malocclusion patients after surgical mandibular advancement treatment as compared to non-treated patients. J Oral Rehabil. 2019;46(7):605–10.
Reiter S, Eli I, Friedman-Rubin P, Emodi-Perlman A, Ziv-Baran T, Winocur E. Comparing Axis II scores according to the RDC/TMD and DC/TMD in Israeli patients. J Oral Facial Pain Headache. 2017;31(4):323–30.
Pigozzi LB, Pereira DD, Pattussi MP, Moret-Tatay C, Irigaray TQ, Weber JBB, et al. Quality of life in young and middle age adult temporomandibular disorders patients and asymptomatic subjects: a systematic review and meta-analysis. Health Qual Life Outcomes. 2021;19(1):83.
Schiffman E, Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular disorders for clinical and research applications. J Am Dent Assoc. 2016;147(6):438–45.
Rongo R, Ekberg E, Nilsson IM, Al-Khotani A, Alstergren P, Conti PCR, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for children and adolescents: an international Delphi study-part 1-Development of Axis I. J Oral Rehabil. 2021;48(7):836–45.
Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for Temporomandibular disorders (DC/TMD) for clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28(1):6–27.
Acknowledgements
Not Applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization GM; MMM; methodology, YS; MC; software, VR; and MC; formal analysis, GM and MMM; investigation, MMM; and GM; data curation, YS; and MC; writing—original draft preparation, YS, MC; GM and VR; writing—review and editing, YS; MC; GM; supervision, GM; funding acquisition, YS; administration: YS All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Minervini, G., Marrapodi, M.M., Siurkel, Y. et al. Accuracy of temporomandibular disorders diagnosis evaluated through the diagnostic criteria for temporomandibular disorder (DC/TDM) Axis II compared to the Axis I evaluations: a systematic review and meta-analysis. BMC Oral Health 24, 299 (2024). https://doi.org/10.1186/s12903-024-03983-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-03983-7