Abstract
Since Molar Incisor Hypomineralization was first described as a pathologic entity, public perception often suggests a considerable rise in prevalence of the respective disease. Since there are still considerable doubts regarding the etiology and—accordingly—prevention of MIH and respective therapeutic approaches are difficult this question is of considerable clinical and public interest. Accordingly, a systematic literature search in accordance with the PRISMA guidelines for systematic reviews on Medline, Cochrane Database, EMBASE, LILACS, Web of Science, Google scholar, Scopus was performed to retrieve original articles reporting the prevalence of MIH as defined by the European Academy of Pediatric Dentistry (EAPD). From initially 2360 retrieved titles, 344 full texts were assessed for possible inclusion and finally 167 articles of mainly moderate to high quality and based on data of 46′613 individuals were included in the meta-analysis. All studies published before 2001 had to be excluded since it was not possible to align the findings with the EAPD classification. Studies varied considerably regarding cohort size (25 to 23′320, mean 1′235)) and age (5.6–19 y, mean 9.8 y). Over all studies, the weighted mean for the prevalence for MIH was 12.8% (95% CI 11.5%-14.1%) and no significant changes with respect to either publication year or birthyear were found. A sub-analysis of eleven studies reporting on the prevalence in different age groups, however, revealed strong evidence for an increasing prevalence between the years 1992 (3%) and 2013 (13%).
Therefore, based on data from cross-sectional studies a possible rise in prevalence of MIH remains unclear. Future prospective large-scale studies under standardized examination conditions with an emphasis on examiner calibration are needed to gain better understanding in the evolution of the prevalence of MIH.
Similar content being viewed by others
Introduction
While hypomineralization in the deciduous and permanent dentition have been found in human teeth 100′000 years of age [1] and have been studied scientifically since over a hundred years [2] a new focus and special clinical interest has been set on this form of developmental tooth disorder in the industrialized and post-industrialized world when caries turned out to be a highly controllable scourge for both deciduous and permanent teeth [3]. In the late 90 s of the twentieth century hypomineralization in otherwise healthy first molars and incisors of the permanent dentition were described and – independently or as a consequence – observed more often [4]. This finding gave rise to concern, and in 2001 the respective manifestation was defined as a new dental disease and was then called the molar-incisor-hypomineralization (MIH). Already in 2003 the European Academy of Pediatric Dentistry stated the pediatric dentists’ awareness to this new dental disease’s symptoms, which was then defined as a hypomineralization of at least one first molar of the permanent dentition, which is often also accompanied by hypomineralization of the central and lateral incisors [5]. Since then, professional alertness towards MIH did not fade. Plenty of studies have been performed on etiology, epidemiology and different methods to treat MIH [6, 7]. While the exact etiology of MIH remains still unclear today’s understanding based on the available evidence is, that MIH has a multifactorial etiology: Genetic reasons with codings on multiple genes seem to constitute only one of umpteen predisposing factors [8]. Furthermore, MIH seems also to be associated with environmental risk factors, of which respiratory issues and infections, malnutrition, certain medication and vitamin D during childhood have been reported to have an effect [9,10,11,12].
Regarding the correct diagnosis for MIH, the special features and the typical localization of MIH lesions have to be carefully distinguished from other kinds of enamel hypomineralization (i.e., Turner teeth especially in case of incisors, initial carious lesions), hypomineralization (i.e., amelogenesis imperfecta) or other chemically induced disturbances during tooth development [13, 14]. The latter are often observed with a symmetrical pattern, while for the others careful clinical differential diagnosis (i.e., affection of all teeth in the case of amelogenesis imperfecta, localization of carious lesions in a dentition with active carious lesions) may lead to the definitive categorization.
For dental professionals, the treatment is often challenging because children affected by MIH are often less compliant due to frequently present tooth hypersensitivity [15, 16]. Furthermore, restorative treatment is technically challenging since it is still matter of discussion how deeply the altered tooth structure should be removed before restoration [17], and respective guidelines are subjected to constant changes [18, 19].
Other than for experts only, MIH has gained a huge repercussion in media [20]. Parents are concerned for their children’s dental wellbeing and studies show that MIH can in fact affect the parents’ quality of life [21].
Within the 20 years since the formulation of a generally accepted and well-established definition of MIH huge effort were taken to assess the prevalence of MIH. In fact, in the meantime, there is data based on a vast number of observational studies from literally nearly all parts of the world [22,23,24]. With symposia specifically held for MIH, media pushing the issue and health care providers advertising specific products for the treatment of MIH (https://www.aapd.org/education/meetings-calendar-aapd/international-symposium-on-molar-hypomineralisation-and-chalkyteeth/https://europe.gc.dental/sites/europe.gc.dental/files/products/downloads/equiaforteht/leaflet/LFL_Treatment_Solutions_for_MIH_de.pdf) there is the perception that MIH has become more and more prevalent since the specific problem had been addressed for the first time in 2001. To the best of the authors’ knowledge there has no systematical approach been made however to scientifically assess whether published data may substantiate the assumed fact of a rising prevalence. Accordingly, the focused question of this review was to assess, whether or not there is – based on the present data of epidemiologic studies – any robust indication for an increasing incidence of MIH. A special focus was set on the meta-analysis of studies reporting on subgroups of different age brackets and the question whether an increased prevalence in younger children was deductible.
Materials and methods
The review was registered on PROSPERO (CRD42021243950) and performed following the guidelines for Preferred Research Items for Systematic Reviews and Meta-Analysis (PRISMA) [25].
Literature search included observational and case–control-studies (control groups were assessed if not adapted to special predisposing factors of the respective cases) which provided prevalence data for MIH according to the definition of the EAPD [5], Weerheijm [4] or if a definition was given that corresponded exactly to the latter.
The electronic search was performed on Medline, Cochrane Database, EMBASE, LILACS, Web of Science, Google scholar, Scopus according to a search strategy adapted to the specific database, combining different search items related to Molar Incisor Hypomineralization and prevalence and study design (see Additional file 1 Table 1).
The inclusion criteria comprised observational (cross-over or case control studies (only control group cohorts of the latter) reporting on the prevalence of MIH in populations which were not preselected (i.e., special exposition to environmental factors) and supposedly representative for the population.
MIH was accepted in terms of the MIH definition by EAPD 2003 [5] or Weerheijm [4] or DDE [26] with modifications which rendered an adaptation to the EAPD definition possible. It was planned to exclude all publications which would not clearly define hypomineralizations of the first molars which were not found to be due to dental fluorosis, enamel hypoplasia, or amelogenesis imperfecta.
No language restrictions were set.
Exclusion criteria encompassed studies assessing specific cohorts of populations which were not rated representative for the whole population, i.e., populations with special medical background and diseases, or cohorts exposed to special environmental factors, or studies addressing one of the sexes only. Likewise, studies which did not report on a clinical method of diagnosis of MIH (i.e., photos, scans, etc.) were excluded.
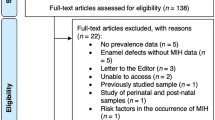
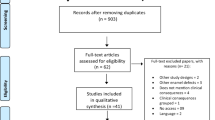
Duplicates from the electronic search were removed. In a first step titles and abstracts were screened for possible inclusion by two independent reviewers. Studies were kept in the screening process if at least one reviewer included it for full text assessment. Subsequently, full texts were assessed for possible inclusion. In order to avoid overestimation of cohorts that were assessed several times, only data of one study were considered. In this regard, the publication with the most comprehensive data was included to the review, or – as a secondary criterium when data was equally comprehensive, the most recent study was considered.
From studies accepted for inclusion and from reviews regarding the topic, reference lists were scrutinized for further studies potentially meeting the inclusion criteria, and potential hits were likewise considered for inclusion.
In a final step data from all full texts which finally fit to the inclusion criteria were extracted and recorded addressing the following items: Author/year, region of clinical examination, clinical assessment period, sampling environment (i.e., dental clinic, school room,…), study type (cross-sectional or case–control), MIH definition, equipment used for the clinical examination (i.e., air drying, headlight, etc.), cohort characteristics/population (age and gender proportions, provenience), cohort size, prevalence of MIH (and which teeth were reported), treatment needs, funding sources and data regarding the quality assessment of the studies (Table 1).
Quality assessment
With the aim to assess the risk of potential bias of the individual studies, a modified GRADE scale for risk assessment was used, involving the parameters representativeness of the cohort, sample size calculation, calibration of the examiners and case definition. If no high risk of bias for any of these parameters were detected, the study was rated as high quality, with one parameter with a high risk of bias the study was rated moderate and with more than one parameter with high risk of bias the study was rated as low quality.
Statistical methods
The outcome of interest was the prevalence of MIH reported across studies. The summary estimate for MIH across studies was obtained with a random effects meta-analysis model, based on restricted maximum likelihood estimation. For each meta-analysis, the estimated heterogeneity variance parameter τ2 was reported together with the measure of heterogeneity I2. In graphical representations, the prevalences reported across studies were shown in relation to assessment period and birth period.
In order to show forest plots, subgroups of studies including different birth cohorts were displayed. Further, there were some studies that reported an age-dependent prevalence of MIH, with different follow-up times across studies. The reported prevalences are shown in a visualization, indicating which prevalence resulted from the individual cohort. In this context, a generalized linear regression model was fitted in order to evaluate in an exploratory approach, whether there was evidence for an increasing prevalence over time. For this, the repeated measurements across studies were addressed with a random intercept, but the size of the included studies was not accounted for in a meta-analysis framework. Statistical calculations were performed with the programming language R version 4.1.1 (2021–08-10) in a fully scripted approach using dynamic reporting.
Results
The electronic search revealed 2′369 titles and abstracts. Of these, 344 full-texts were considered for possible inclusion. After removing studies reporting on the same cohort, studies which did not provide suitable data presentation for the prevalence of MIH as defined in the method chapter and studies which assessed cohorts obviously non-representative for the general population, data of 167 distinct studies were finally included into the meta-analysis.
None of the publications before 2001 were found to allow for a proper definition of hypomineralizations of the first molars, or rather a clear delimitation from dental fluorosis, enamel hypoplasia, or amelogenesis imperfecta. Accordingly, all these studies were excluded from the meta-analysis.
The entire study selection process is illustrated in Fig. 1.
Quality assessment
While most of the studies included to the meta-analysis were of medium quality (148), the studies covered the whole range from high (58) over moderate (70) to low (31) quality. The most frequent reason for limited quality was missing sample size calculation (199) followed by missing inter-examiner reliability (134) (Additional file 1 Table 2).
Studies included to the review were published after 2001 but several examinations had taken place considerably before. Data from 46′613 individuals had been considered in the present review. The assessed cohorts in the different studies varied from 25 to 23′320 children with a mean cohort size of 1′235 infants across studies. The assessed population varied in age from 5.6 to 19 years of age and were at a weighted mean age of 9.8 years old. The weighed mean proportion of boys, where reported, was 51% across studies, ranging from 28 to 100% while in 42 of the included studies, no information on children’s sex was reported.
Figure 2a indicates the prevalences of MIH related to the year of publication, while Fig. 2b shows the prevalences related to the birthyears of the study participants, by subtracting the cohort’s mean age from the year of examination. The prevalences were loess-smoothed, and the curve is shown with 95% confidence intervals.
a and b Prevalences of MIH in the included studies. A Reported prevalences of MIH related to year of publication and B) related to birthyear of the respective cohort. Each black dot indicates the prevalence reported in an individual study. The blue line shows the loess-smoothed prevalence of all studies related to publication year or birth year, while the grey area indicates 95% confidence interval
Across all studies, the prevalence of MIH ranged between 0.48% and 46.6% resulting in a summary estimate across studies based on a random-effects meta-analysis model of 12.8% (95% CI 11.5%-14.1%), with τ2 being 0.56, and I2 being equal to 98.5%. To address the question whether a different classification scheme would affect the estimation of the prevalence, the classification type was added as a moderator in a random effects model. The corresponding p-value was 0.17, indicating that there was no evidence for a moderating effect of the classification scheme.
To show the prevalence of MIH in forest plots, subgroups of birth year ranges were defined with the cut-off values for the birth years being A) before 1997, B) between 1997–2003 and C) from 2003 on (Fig. 3a-c). With overall estimates of the mean prevalence and 95% confidence intervals of 13% (9% to 18%), 13% (11% to 14%), and 13% (11% to 15%), respectively, there was no evidence for a difference between the subgroups of birth year categories.
a Prevalences of MIH in studies reporting on populations with a mean birth year before 1997 The column on the left indicates first author and year of publication. The position of the boxes indicate the mean value for the prevalence of MIH while the size of the boxes indicates their weight in the meta-analysis. Whiskers depict the confidence interval (CI). Means and CI are given in the column on the right. The rhombus indicates the mean (position) and the CI (horizontal extention) of the overall summary estimate. RE indicates a random effects model for meta-analysis. The heterogeneity variance τ2 was estimated to be 0.56, I2 was estimated to be 97.7%. b Prevalences of MIH in studies reporting on populations with a mean birthyear from 1997 to 2003. The column on the left indicates first author and year of publication. The position of the boxes indicate the mean value for the prevalence of MIH while the size of the boxes indicates their weight in the meta-analysis. Whiskers depict the confidence interval (CI). Means and CI are given in the column on the right. The rhombus indicates the mean (position) and the CI (horizontal extention) of the overall summary estimate. RE indicates a random effects model for meta-analysis. The heterogeneity variance τ2 was estimated to be 0.25, I2 was estimated to be 96.8%. c Prevalences of MIH in studies reporting on populations with a mean birthyear after 2003. The column on the left indicates first author and year of publication. The position of the boxes indicate the mean value for the prevalence of MIH while the size of the boxes indicates their weight in the meta-analysis. Whiskers depict the confidence interval (CI). Means and CI are given in the column on the right. The rhombus indicates the mean (position) and the CI (horizontal extention) of the overall summary estimate. RE indicates a random effects model for meta-analysis. The heterogeneity variance τ2 was estimated to be 0.79, I2 was estimated to be 98.8%
Prevalence across studies with repeated follow-up assessments.
The analysis on the data of studies which reported repeatedly prevalences in groups at different ages was based on 11 studies (see Table 1a [27,28,29,30, 32,33,34,35,36,37, 143]). The respective data is based on a total of 50`611 (range 404–23320) patients with an aged from 6 to 15y from Western Europe and Asia. In all studies, MIH was diagnosed based on ethe EAPD criteria or according to Weerheijm. Regarding the proportion of males and females there was no relevant deviation. Generally, MIH prevalence ranged from 2.9 to 19.3 in the respective studies. It shows a continuous rise in prevalence for MIH from the earliest examination in 1992 to the most recent available in 2011 (Fig. 4). The corresponding p-value for a linear time trend showed strong evidence for an increasing prevalence. Based on the merged data on the respective studies the prevalence of MIH show a rise from 6 to 14% from the years 2000 to 2010. A sub-analysis of the prevalence over time shows considerable differences for the prevalence of MIH between the regions previously described by Schwendicke et al. [22]. While for most areas there are few studies and they are therefore not eligible for a sound analysis, the areas “North African and Middle East” and “Central Latin America” show a rise in prevalence while the areas “Tropical Latin America” and “High-income Asia Pacific” show a respective decline (see Additional file 1 Fig. 1).
Prevalences of MIH in studies reporting separately on the prevalence of MIH for different ages. Each black dot indicates the prevalence of an individual study. Grey lines connect data from the same study population. The continuous black line shows the loess-smoothed prevalence across all study cohorts, the dashed lines indicate 95% confidence limits [27,28,29,30, 32,33,34,35,36,37, 143]
Discussion
Molar incisor hypomineralization has become an important topic in pediatric dentistry within the last 20 years [19, 182]. Since the perceived prevalence is continuously rising and the impact for affected children and their families are considerable [21] plenty of epidemiologic studies have been performed all over the world [22], but so far, no systematic approach has been investigating whether there is actually any indication for any rise in prevalence from scientific literature.
Merging data on weighted means of prevalence for MIH failed in either of the performed calculations to indicate a rise over time: Neither for the raw data presented in 167 studies nor after adjusting the data to the actual age of the populations in which the studies had been performed revealed an enhanced prevalence. Ideally, however, the question whether there is a raise in the prevalence of MIH would be answered by studies assessing children of the same age group after a considerable time span of several years under standardized and well-calibrated conditions. Therefore, in a separate analysis on data from studies with age-specific prevalences for the assessed children and adolescents was performed. The results draw a different conclusion: Based on this specific data from 11 high quality studies (see Supplemental Table 2), in fact, a considerable rise based on studies from Europe, Africa, Asia, South America and Oceania in the prevalence of MIH becomes evident. Important to highlight, however, that this result is not based on a meta-analysis model due to the complexity of the data structure with multiple reportings across single studies. For this reason, the results will need confirmation in prospective studies.
With an average of 12.8% the mean value from the studies considered for the present meta-analysis are slightly lower than those of two recent reviews with 13.1% and 14.2% [22, 183]. Nevertheless, the results are in the same range, and small differences may be attributed to the later publication date or recent publications which have not been considered in the previous reviews. Given that both, age distribution and proportion of males and females did not differ considerably to the previous reviews, renders the latter options for a potential bias rather unlikely and seems to confirm the relevance of more recent data.
The results of the present systematic review should however be considered with care: Many studies and reviews estimating the prevalence of MIH have been highlighting the limits of the individual reports (due to a considerable bias level as assessed also for the present study): The cohorts themselves might not always exactly depict the population in which the examinations were performed, the definition of MIH might slightly vary while data on the inter-examinators agreement have not always been reported. Furthermore, sample size calculations, a measure which aims for avoiding statistical type II errors, were not performed in all of the studies included into the present review (see Supplemental Table 2, quality assessment) [184]. Then it is important to highlight, that data on prevalence show a vast range from 0.48% and 46.6% within the different studies [185], a strong indicator for the fact that merged data is based on a highly heterogeneous set of data. Generally, merged analysis of data from cohort studies of all different areas of the world bear several immanent risks like different operators and settings, and published changes for the prevalence of MIH in distinct populations or single nations might remain unperceived [54, 138].
On the other hand, the results of this review are based on a comparatively high number of studies: With 167 studies on data of a total of 46′613 patients the results are based on a quite solid base and stands out from most comparative studies in dentistry.
Hypomineralization on first molars of the permanent dentition is not a new finding for sure. Several studies examining prehistoric dentitions show enamel demineralization with the typical features of MIH-affected teeth, namely an increasing mineralization from the enamel-dentine junction towards the tooth surface [186,187,188]. Furthermore, there are plenty of examinations which were performed in the late last century. Though they assess hypomineralizations on a standardized and highly scientific level, a good deal of the respective data could not be used in the present meta-analysis due to the fact that the addressed hypomineralizations had not been specified exactly before 2001 [4], and MIH as an entity has not been defined before 2003 [5]. Accordingly, the greatest part of 59 studies published from 1930 to 2002 had to be excluded, since a valid adaptation of the findings to the definition of MIH was not possible in these studies: Mostly, either the exact location on a permanent molar or a sufficient demarcation towards defects of similar appearance but of different origin like enamel altered by fluorosis, hypoplasia, Turner teeth or discoloration due to tetracyclines [13, 14] was not possible. However, as a lucky matter of fact several examinations which had been performed before 2001 and the definition of MIH were published considerably later, then considering the definition of MIH which had been published recently before. Luckily, the new definition of MIH was quickly spread and adapted on then-published studies, what helped to find comparable data and, therefore, considerable evidence.
The fact that the prevalence of MIH might indeed rise by time is an important puzzle piece in MIH research since quantification of global and regional burden of MIH and the awareness of respective trends and changes in the prevalence is highly relevant for decision makers in the healthcare sector and health care providers [22].
Data on the prevalence of MIH merged in the meta-analyses showed a considerable range. The respective heterogeneity might be to many different reasons: While there might be different sources of bias like different levels of specificity and sensitivity of the operators, partially attributable to the examination settings in which they performed their examinations (see Table 1), the simple fact that all over the world different ethnicities were assessed [22] over a considerable time frame will have contributed to variations in the prevalence data.
With a range from 5.6 to 19 years, there was a considerably large heterogeneity for the age of the examined patients. While some studies assessed patient cohorts at a defined age, others involved children of mixed ages, while other studies assessed the prevalence of MIH in several defined age groups in follow-up appointments (Table 1a). Prevalence of MIH, however, has been reported be age-dependent with a higher proportion in children younger than 10 years of age [183]. In order to standardize examinations and respective results, optimal time points (5y for hypomineralised second primary molars and 8y for MIH) have been suggested [189]. Regarding the inclusion criteria is should be highlighted, that the decision to include data from both, cross-sectional studies and from control cohorts of case–control studies generally bear a higher risk of Berkson’s bias, the latter arising due to testing a subpopulation rather than the general population [190]. This potential risk has been largely double-checked in the present study since the selection bias was assessed in the quality assessment. Thereby however, no substantial inferior quality for the controls cohorts form case–control studies could be determined.
The present review merges data from studies of different quality. The high proportion of low-rated studies might be seen as a limitation. However, low quality was already rated if more than on parameter was considered to have a high risk for a bias, thereby not rendering the study data unreliable, but highlighting the possible source of bias.
Conclusion
Merged data from cross-sectional studies do not indicate a rise in worldwide’s prevalence of MIH. However, studies on age-specifical assessment show a rise from 6 to 14% in the years from 2000 to 2010 for the prevalence of MIH.
Further age-specific re-analysis of existing data on one side and future studies, which assess age-dependent prevalence of MIH on a high-quality level might unearth more knowledge about the dynamic of MIH prevalence than further unspecific reports on just mean prevalences.
Availability of data and materials
Data will be provided on reasonable request to the corresponding author PD Dr. Philipp Sahrmann.
References
Becam G, Chevalier T. Neandertal features of the deciduous and permanent teeth from Portel-Ouest Cave (Ariege, France). Am J Phys Anthropol. 2019;168(1):45–69.
Berten J. Hypoplasie des Schmelzes. Deutsche Monatsschrift für Zahnheilkunde. 1895;13(9):426–600.
Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F, Tagami J, Twetman S, Tsakos G, Ismail A. Dental caries. Nat Rev Dis Primers. 2017;3:17030.
Weerheijm KL, Jalevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35(5):390–1.
Weerheijm KL. Molar incisor hypomineralisation (MIH). Eur J Paediatr Dent. 2003;4(3):114–20.
Lopes LB, Machado V, Mascarenhas P, Mendes JJ, Botelho J. The prevalence of molar-incisor hypomineralization: a systematic review and meta-analysis. Sci Rep. 2021;11(1):22405.
Somani C, Taylor GD, Garot E, Rouas P, Lygidakis NA, Wong FSL. An update of treatment modalities in children and adolescents with teeth affected by molar incisor hypomineralisation (MIH): a systematic review. Eur Arch Paediatr Dent. 2022;23(1):39–64.
Bezamat M, Souza JF, Silva FMF, Correa EG, Fatturi AL, Brancher JA, Carvalho FM, Cavallari T, Bertolazo L, Machado-Souza C, et al. Gene-environment interaction in molar-incisor hypomineralization. PLoS ONE. 2021;16(1): e0241898.
Crombie F, Manton D, Kilpatrick N. Aetiology of molar-incisor hypomineralization: a critical review. Int J Paediatr Dent. 2009;19(2):73–83.
Alaluusua S. Aetiology of Molar-Incisor Hypomineralisation: a systematic review. Eur Arch Paediatr Dent. 2010;11(2):53–8.
Silva MJ, Scurrah KJ, Craig JM, Manton DJ, Kilpatrick N. Etiology of Molar Incisor Hypomineralization - a systematic review. Community Dent Oral Epidemiol. 2016;44(4):342–53.
Kuhnisch J, Thiering E, Kratzsch J, Heinrich-Weltzien R, Hickel R, Heinrich J. group GIs, group LIs: Elevated serum 25(OH)-vitamin D levels are negatively correlated with molar-incisor hypomineralization. J Dent Res. 2015;94(2):381–7.
Mast P, Rodrigueztapia MT, Daeniker L, Krejci I. Understanding MIH: definition, epidemiology, differential diagnosis and new treatment guidelines. Eur J Paediatr Dent. 2013;14(3):204–8.
Denis M, Atlan A, Vennat E, Tirlet G, Attal JP. White defects on enamel: diagnosis and anatomopathology: two essential factors for proper treatment (part 1). Int Orthod. 2013;11(2):139–65.
Linner T, Khazaei Y, Bucher K, Pfisterer J, Hickel R, Kuhnisch J. Hypersensitivity in teeth affected by molar-incisor hypomineralization (MIH). Sci Rep. 2021;11(1):17922.
Raposo F, de Carvalho Rodrigues AC, Lia EN, Leal SC. Prevalence of hypersensitivity in teeth affected by Molar-Incisor Hypomineralization (MIH). Caries Res. 2019;53(4):424–30.
Fragelli CM, Souza JF, Jeremias F, Cordeiro Rde C, Santos-Pinto L. Molar Incisor Hypomineralization (MIH): conservative treatment management to restore affected teeth. Braz Oral Res. 2015;29:S1806.
Lygidakis NA, Garot E, Somani C, Taylor GD, Rouas P, Wong FSL. Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an updated European Academy of Paediatric Dentistry policy document. Eur Arch Paediatr Dent. 2022;23(1):3–21.
Lygidakis NA, Wong F, Jalevik B, Vierrou AM, Alaluusua S, Espelid I. Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an EAPD Policy Document. Eur Arch Paediatr Dent. 2010;11(2):75–81.
Gambetta-Tessini K, Marino R, Ghanim A, Calache H, Manton DJ. Knowledge, experience and perceptions regarding Molar-Incisor Hypomineralisation (MIH) amongst Australian and Chilean public oral health care practitioners. BMC Oral Health. 2016;16(1):75.
Leal SC, Oliveira TRM, Ribeiro APD. Do parents and children perceive molar-incisor hypomineralization as an oral health problem? Int J Paediatr Dent. 2017;27(5):372–9.
Schwendicke F, Elhennawy K, Reda S, Bekes K, Manton DJ, Krois J. Global burden of Molar Incisor Hypomineralization. J Dent. 2018;68:10–8.
da Costa RT, Pintor AVB, Magno MB, Maranon-Vasquez GA, Maia LC, Neves AA. Worldwide trends on molar incisor and deciduous molar hypomineralisation research: a bibliometric analysis over a 19-year period. Eur Arch Paediatr Dent. 2022;23(1):133–46.
Bandeira Lopes L, Machado V, Botelho J, Haubek D. Molar-incisor hypomineralization: an umbrella review. Acta Odontol Scand. 2021;79(5):359–69.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160.
FDI. A review of the developmental defects of enamel index (DDE Index). Commission on oral health, research & epidemiology. Report of an FDI working group. Int Dent J. 1992;42(6):411–26.
Abdelaziz M, Krejci I, Banon J. Prevalence of Molar Incisor Hypomineralization in over 30,000 Schoolchildren in Switzerland. J Clin Pediatr Dent. 2022;46(1):1–5.
Amend S, Nossol C, Bausback-Schomakers S, Wleklinski C, Scheibelhut C, Pons-Kuhnemann J, Frankenberger R, Kramer N. Prevalence of molar-incisor-hypomineralisation (MIH) among 6–12-year-old children in Central Hesse (Germany). Clin Oral Investig. 2021;25(4):2093–100.
Hong YL, Wu H, Yuan J, Yao H, Sui W. Prevalence study of molar-incisor hypo mineralisation in primary school children in South China. J Pediatr Care 2017 3(15).
Kukleva MP, Petrova SG, Kondeva VK, Nihtyanova TI. Molar incisor hypomineralisation in 7-to-14-year old children in Plovdiv, Bulgaria–an epidemiologic study. Folia Med (Plovdiv). 2008;50(3):71–5.
Oyedele TA, Folayan MO, Adekoya-Sofowora CA, Oziegbe EO. Co-morbidities associated with molar-incisor hypomineralisation in 8 to 16 year old pupils in Ile-Ife Nigeria. BMC Oral Health. 2015;15:37.
Quispe DMA, de Priego GPM, Manco RAL, Portaro CP. Molar Incisor Hypomineralization: prevalence and severity in schoolchildren of Puno, Peru. J Indian Soc Pedod Prev Dent. 2021;39:246–50.
Rai PM, Jain J, Raju AS, Nair RA, Shashidhar K, Dsouza S. Prevalence of Molar Incisor Hypomineralization among school children aged 9 to 12 years in Virajpet, Karnataka, India. Open Access Maced J Med Sci. 2019;7(6):1042–6.
Thakur H, Kaur A, Singh N, Singh R, Kumar S. Prevalence and clinical characteristics of molar-incisor hypomineralization in 8–16-year-old children in industrial Town of Solan District of Himachal Pradesh. Int J Clin Pediatr Dent. 2020;13(3):230–4.
Verma S, Dhinsa K, Tripathi AM, Saha S, Yadav G, Arora D. Molar Incisor Hypomineralization: prevalence, associated risk factors, its relation with dental caries and various enamel surface defects in 8–16-year-old schoolchildren of Lucknow District. Int J Clin Pediatr Dent. 2022;15(1):1–8.
Yannam SD, Amarlal D, Rekha CV. Prevalence of Molar Incisor Hypomineralization in school children aged 8–12 years in Chennai. J Indian Soc Pedod Prev Dent. 2016;34(2):134–8.
Yi X, Chen W, Liu M, Zhang H, Hou W, Wang Y. Prevalence of MIH in children aged 12 to 15 years in Bei**g China. Clin Oral Investig. 2021;25(1):355–61.
Ahmad SH, Petrou MA, Alhumrani A, Hashim R, Splieth C. Prevalence of molar-incisor hypomineralisation in an emerging community, and a possible correlation with caries, fluorosis and socioeconomic status. Oral Health Prev Dent. 2019;17(4):323–7.
Ahmadi R, Ramazani N, Nourinasab R. Molar Incisor Hypomineralization: a study of prevalence and etiology in a group of Iranian children. Iran J Pediatr. 2012;22(2):245–51.
Al-Hammad NS, Al-Dhubaiban M, Alhowaish L, Bello LL. Prevalence and clinical characteristics of Molar-Incisor-Hypomineralization in school children in Riyadh, Saudi Arabia. Int J Med Sci Clin Invent. 2018;5(3):3570–6.
Allazzam SM, Alaki SM, El Meligy OA. Molar Incisor Hypomineralization, prevalence, and etiology. Int J Dent. 2014;2014:234508.
Americano GC, Jacobsen PE, Soviero VM, Haubek D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int J Paediatr Dent. 2017;27(1):11–21.
Arheiam A, Abbas S, Ballo L, Borowis E, Rashwan S, El Tantawi M. Prevalence, distribution, characteristics and associated factors of molar-incisor hypo-mineralisation among Libyan schoolchildren: a cross-sectional survey. Eur Arch Paediatr Dent. 2021;22(4):595–601.
Arslanagic-Muratbegovic A, Markovic N, Zukanovic A, Tiro A, Dzemidzic V. Molar incisor hypomineralization: prevalence and severity in six to nine-year-old Sarajevo children. Eur J Paediatr Dent. 2020;21(3):243–7.
Bahrololoomi Z, Mostafalu N, Shakib A. Relationship between molar incisor hypomineralization with body mass index and dental caries index in 7–11 year old children in Yazd City. J Shahid Sadoughi Univ Med Sci. 2017;25(1):11–9.
Balmer R, Toumba KJ, Munyombwe T, Duggal MS. A comparison of the presentation of molar incisor hypomineralisation in two communities with different fluoride exposure. Eur Arch Paediatr Dent. 2015;16(3):257–64.
Balmer R, Toumba KJ, Munyombwe T, Godson J, Duggal MS. The prevalence of incisor hypomineralisation and its relationship with the prevalence of molar incisor hypomineralisation. Eur Arch Paediatr Dent. 2015;16(3):265–9.
Balmer R, Toumba J, Godson J, Duggal M. The prevalence of molar incisor hypomineralisation in Northern England and its relationship to socioeconomic status and water fluoridation. Int J Paediatr Dent. 2012;22(4):250–7.
Bhaskar SA, Hegde S. Molar-incisor hypomineralization: prevalence, severity and clinical characteristics in 8- to 13-year-old children of Udaipur, India. J Indian Soc Pedod Prev Dent. 2014;32(4):322–9.
Biondi AM, Cortese SG, Martinez K, Ortolani AM, Sebelli PM, Ienco M, Pavan VH, Mendel N, Bertolino M, Hecht P. Prevalence of molar incisor hypomineralization in the city of Buenos Aires. Acta Odontol Latinoam. 2011;24(1):81–5.
Biondi AM. Lopez Jordi Mdel C, Cortese SG, Alvarez L, Salveraglio I, Ortolani AM: Prevalence of molar-incisor hypomineralization (MIH) in children seeking dental care at the Schools of Dentistry of the University of Buenos Aires (Argentina) and University of la Republica (Uruguay). Acta Odontol Latinoam. 2012;25(2):224–30.
Bonzanini LIL, Arduim ADS, Lenzi TL, Hugo FN, Hilgert JB, Casagrande L. Molar-incisor hypomineralization and dental caries: A hierarchical approach in a populational-based study. Braz Dent J. 2021;32(6):74–82.
Buchgraber B, Kqiku L, Ebeleseder KA. Molar incisor hypomineralization: proportion and severity in primary public school children in Graz Austria. Clin Oral Investig. 2018;22(2):757–62.
Calderara PC, Gerthoux PM, Mocarelli P, Lukinmaa PL, Tramacere PL, Alaluusua S. The prevalence of Molar Incisor Hypomineralisation (MIH) in a group of Italian school children. Eur J Paediatr Dent. 2005;6(2):79–83.
da Costa-Silva CM, Jeremias F, de Souza JF, Cordeiro Rde C, Santos-Pinto L, Zuanon AC. Molar incisor hypomineralization: prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010;20(6):426–34.
da Costa Silva CM, Ortega EMM, Mialhe FL. The Impact of Molar-Incisor Hypomineralisation on dental caries in permanent first molars: a prospective cohort study. Oral Health Prev Dent. 2017;15(6):581–6.
da Silva FMF, Zhou Y, de Fátima Vieira FG, de Carvalho M, de Castro CM, Vieira AR. Defining the prevalence of Molar Incisor Hypomineralization in Brazil. Pesquisa Brasileira em Odontopediatria e Clínica Integrada. 2020;20: e5146.
da Silva Júnior IF, Aguiar NL, Barros WRC, da Silva LS, Arantes DC. doNascimento LS: prevalence and severity of Molar Incisor Hypomineralization in students of Belém, Brazil. Braz Res Pediatric Dentistry Integr Clin. 2015;15(1):377–85.
Dantas-Neta NB, Moura LF, Cruz PF, Moura MS, Paiva SM, Martins CC, Lima MD. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz Oral Res. 2016;30(1): e117.
Davenport M, Welles AD, Angelopoulou MV, Gonzalez C, Okunseri C, Barbeau L, Bansal NK, Vergotine RJ, Hodgson BD. Prevalence of molar-incisor hypomineralization in Milwaukee, Wisconsin, USA: a pilot study. Clin Cosmet Investig Dent. 2019;11:109–17.
Dietrich G, Sperling S, Hetzer G. Molar incisor hypomineralisation in a group of children and adolescents living in Dresden (Germany). Eur J Paediatr Dent. 2003;4(3):133–7.
Ditto D, Ajoor T, Al-Khashram M, Tayab M, Al Sharbati W. Prevalence of molar incisor hypomineralization in seven–nine-year-old Bahraini children: an epidemiological study. J Bahrain Med Soc. 2018;30(1):45–51.
Dourado DG, Lima CCB, Silva RNC, Tajra FS, Moura MS, Lopes TSP, De Deus Moura LFA, de Lima MDM. Molar-incisor hypomineralization in quilombola children and adolescents: a study of prevalence and associated factors. J Public Health Dent. 2021;81(3):178–87.
Duarte MBS, Carvalho VR, Hilgert LA, Ribeiro APD, Leal SC, Takeshita EM. Is there an association between dental caries, fluorosis, and molar-incisor hypomineralization? J Appl Oral Sci. 2021;29: e20200890.
Durmus B, Abbasoglu Z, Peker S, Kargul B. Possible medical aetiological factors and characteristics of Molar Incisor Hypomineralisation in a group of Turkish children. Acta stomatol Croat. 2013;47(4):297–305.
Einollahi M, Hekmatfar S, Molaei M. Association between molar incisor hypomineralization and both prenatal and postnatal factors in 8–10 year old children in ardebil. J Evolution Med Dent Sci. 2020;48(9):3606–10.
Elfrink ME, ten Cate JM, Jaddoe VW, Hofman A, Moll HA, Veerkamp JS. Deciduous molar hypomineralization and Molar Incisor Hypomineralization. J Dent Res. 2012;91(6):551–5.
ElSoud AAA, Mahfouz SM. Prevalence and severity of molar incisor hypomineralization in school children of Suez Canal region: cross-sectional study. Egypt Dent J. 2019;65:909–15.
Emmatty TB, Eby A, Joseph MJ, Bijimole J, Kavita K, Asif I. The prevalence of molar incisor hypomineralization of school children in and around Muvattupuzha, Kerala. J Indian Soc Pedod Prev Dent. 2020;38(1):14–9.
de Farias AL, Rojas-Gualdron DF, Girotto Bussaneli D, Santos-Pinto L, Mejia JD, Restrepo M. Does molar-incisor hypomineralization (MIH) affect only permanent first molars and incisors? New observations on permanent second molars. Int J Paediatr Dent. 2022;32(1):1–10.
Farias L, Laureano ICC, Fernandes LHF, Forte FDS, Vargas-Ferreira F, Alencar CRB, HonOrio HM, Cavalcanti AL. Presence of molar-incisor hypomineralization is associated with dental caries in Brazilian schoolchildren. Braz Oral Res. 2021;35: e13.
Fatturi AL, Menoncin BL, Reyes MT, Meger M, Scariot R, Brancher JA, Kuchler EC, Feltrin-Souza J. The relationship between molar incisor hypomineralization, dental caries, socioeconomic factors, and polymorphisms in the vitamin D receptor gene: a population-based study. Clin Oral Investig. 2020;24(11):3971–80.
Fernandes IC, Forte FDS, Sampaio FC. Molar-incisor hypomineralization (MIH), dental fluorosis, and caries in rural areas with different fluoride levels in the drinking water. Int J Paediatr Dent. 2021;31(4):475–82.
Flexeder C, Kabary Hassan L, Standl M, Schulz H, Kuhnisch J. Is there an association between asthma and dental caries and Molar Incisor Hypomineralisation? Caries Res. 2020;54(1):87–95.
Folayan MO, Chukwumah NM, Popoola BO, Temilola DO, Onyejaka NK, Oyedele TA, Lawal FB. Developmental defects of the enamel and its impact on the oral health quality of life of children resident in Southwest Nigeria. BMC Oral Health. 2018;18(1):160.
Fragelli C, Barbosa TS, Bussaneli DG, Restrepo M, Cordeiro RCL, Santos-Pinto L. Aesthetic perception in children with molar incisor hypomineralization. Eur Arch Paediatr Dent. 2021;22(2):227–34.
Freitas Fernandes LH, Laureano ICC, Farias L, Andrade NM, Soares Forte FD, Barros Alencar CR, Cavalcanti AL. Incisor Molar Hypomineralization and quality of life: a population-based study with Brazilian schoolchildren. Int J Dent. 2021;2021:6655771.
Fteita D, Ali A, Alaluusua S. Molar-incisor hypomineralization (MIH) in a group of school-aged children in Benghazi Libya. Eur Arch Paediatr Dent. 2006;7(2):92–5.
Gambetta-Tessini K, Marino R, Ghanim A, Calache H, Manton DJ. Carious lesion severity and demarcated hypomineralized lesions of tooth enamel in schoolchildren from Melbourne Australia. Aust Dent J. 2018;63:365.
Gambetta-Tessini K, Marino R, Ghanim A, Calache H, Manton DJ. The impact of MIH/HSPM on the carious lesion severity of schoolchildren from Talca Chile. Eur Arch Paediatr Dent. 2019;20(5):417–23.
Garcia-Margarit M, Catala-Pizarro M, Montiel-Company JM, Almerich-Silla JM. Epidemiologic study of molar-incisor hypomineralization in 8-year-old Spanish children. Int J Paediatr Dent. 2014;24(1):14–22.
Georgieva-Dimitrova M. Distribution of molar incisor hypomineralization in children in Northeast Bulgaria. Severity of the dysplasia and sensitivity of the affected teeth. Scripta Scientifica Salutis Publicae. 2019;5:46–51.
Ghanim AM, Manton DJ, Morgan MV, Marino RJ, Bailey DL. Trends of oral health care and dental treatment needs in relation to molar incisor hypomineralisation defects: a study amongst a group of Iraqi schoolchildren. Eur Arch Paediatr Dent. 2012;13(4):171–8.
Ghanim A, Bagheri R, Golkari A, Manton D. Molar-incisor hypomineralisation: a prevalence study amongst primary schoolchildren of Shiraz. Iran Eur Arch Paediatr Dent. 2014;15(2):75–82.
Glodkowska N, Emerich K. The impact of environmental air pollution on the prevalence of molar incisor hypomineralization in schoolchildren: a cross-sectional study. Adv Clin Exp Med. 2020;29(12):1469–77.
Gorbatova MA, Utkina EI, Zinchenko GA, Grjibovski AM, Popova DA, Popov VA, Gorbatova LN. Molar-incisor hypomineralization among 12-years old children in Arkhangelsk region. Stomatologiia (Mosk). 2019;98(2):64–6.
Goswami M, Bhushan U, Pandiyan R, Sharma S. Molar Incisor Hypomineralization-an emerging burden: a short study on prevalence and clinical characteristics in Central Delhi India. Int J Clin Pediatr Dent. 2019;12(3):211–4.
Groselj M, Jan J. Molar incisor hypomineralisation and dental caries among children in Slovenia. Eur J Paediatr Dent. 2013;14(3):241–5.
Gurrusquieta BJ, Nunez VM, Lopez ML. Prevalence of Molar Incisor Hypomineralization in Mexican children. J Clin Pediatr Dent. 2017;41(1):18–21.
Gutierrez TV, Ortega CCB, Perez NP, Perez AG. Impact of Molar Incisor Hypomineralization on oral health-related quality of life in Mexican schoolchildren. J Clin Pediatr Dent. 2019;43(5):324–30.
Hamdan MA, Abu-Ghefreh EA, Al-Abdallah M, Rajab LD. the prevalence and severity of Molar Incisor Hypomineralization (MIH) among 8 year-old children in Amman Jordan. Egypt Dental J. 2020;66:1989–97.
Hanan SA, Filho AOA, Medina PO, Cordeiro RCL, Santos-Pinto L, Zuanon ACC: Molar-Incisor Hypomineralization in schoolchildren of Manaus, Brazil. Braz Res Pediatr Dentistry Integr Clinic. 2015;15(1):309-17.
Hartsock LA, Burnheimer J, Modesto A, Vieira AR. A snapshot of the prevalence of Molar Incisor Hypomineralization and fluorosis in Pittsburgh, Pennsylvania, USA. Pediatr Dent. 2020;42(1):36–40.
Hernandez M, Boj JR, Espasa E, Peretz B. First permanent molars and permanent incisors teeth by tooth prevalence of Molar-Incisor-Hypomineralisation in a group of Spanish schoolchildren. Acta Stomatol Croat. 2018;52(1):4–11.
Hertel S, Seume M, Hannig C, Viergutz G. Molar-Incisor-Hypomineralization (MIH) in 7-to 9-year old Dresden pupils. Oralprophylaxe und Kinderzahnheilkunde. 2017;39(2):65–71.
Hoyte T, Kowlessar A, Ali A, Bearn D. Cross-sectional survey to ascertain the prevalence of Molar Incisor Hypo- mineralization in the Trinidad and Tobago population. Am J Biomed Sci Res. 2020;7(3):204.
Hussain G, Al-Halabi M, Kowash M, Hassan A. The prevalence and severity of Molar Incisor Hypomineralization and Molar Hypomineralization in Dubai. UAE J Dent Child (Chic). 2018;85(3):102–7.
Hussein AS, Faisal M, Haron M, Ghanim AM, Abu-Hassan MI. Distribution of Molar Incisor Hypomineralization in Malaysian children attending university dental clinic. J Clin Pediatr Dent. 2015;39(3):219–23.
Hysi D, Kuscu OO, Droboniku E, Toti C, Xhemnica L, Caglar E. Prevalence and aetiology of Molar-Incisor Hypomineralisation among children aged 8–10 years in Tirana. Albania Eur J Paediatr Dent. 2016;17(1):75–9.
Irigoyen-Camacho ME, Villanueva-Gutierrez T, Castano-Seiquer A, Molina-Frechero N, Zepeda-Zepeda M, Sanchez-Perez L. Evaluating the changes in molar incisor hypomineralization prevalence: a comparison of two cross-sectional studies in two elementary schools in Mexico City between 2008 and 2017. Clin Exp Dent Res. 2020;6(1):82–9.
Jalevik B, Klingberg G, Barregard L, Noren JG. The prevalence of demarcated opacities in permanent first molars in a group of Swedish children. Acta Odontol Scand. 2001;59(5):255–60.
Jalevik B, Szigyarto-Matei A, Robertson A. The prevalence of developmental defects of enamel, a prospective cohort study of adolescents in Western Sweden: a Barn I TAnadvarden (BITA, children in dental care) study. Eur Arch Paediatr Dent. 2018;19(3):187–95.
Jankovic S, Ivanovic M, Davidovic B, Lecic J. Distribution and characteristics of molar-incisor hypomineralization. Vojnosanit Pregl. 2014;71(8):730–4.
Jasulaityte L, Veerkamp JS, Weerheijm KL. Molar incisor hypomineralization: review and prevalence data from the study of primary school children in Kaunas/Lithuania. Eur Arch Paediatr Dent. 2007;8(2):87–94.
Jasulaityte L, Weerheijm KL, Veerkamp JS. Prevalence of molar-incisor-hypomineralisation among children participating in the Dutch National Epidemiological Survey (2003). Eur Arch Paediatr Dent. 2008;9(4):218–23.
Jeremias F, de Souza JF, Silva CM, Cordeiro Rde C, Zuanon AC, Santos-Pinto L. Dental caries experience and Molar-Incisor Hypomineralization. Acta Odontol Scand. 2013;71(3–4):870–6.
Jurlina D, Uzarevic Z, Ivanisevic Z, Matijevic N, Matijevic M. Prevalence of Molar-Incisor Hypomineralization and caries in eight-year-old children in Croatia. Int J Environ Res Public Health. 2020;17(17):6358.
Kevrekidou A, Kosma I, Arapostathis K, Kotsanos N. Molar Incisor Hypomineralization of eight- and 14-year-old children: prevalence, severity, and defect characteristics. Pediatr Dent. 2015;37(5):455–61.
Kilinc G, Cetin M, Kose B, Ellidokuz H. Prevalence, aetiology, and treatment of molar incisor hypomineralization in children living in Izmir City (Turkey). Int J Paediatr Dent. 2019;29(6):775–82.
Kim T, Jeong I, Lee D, Kim J, Yang Y. Prevalence and etiology of Molar Incisor Hypomineralization in children aged 8–9 years. J Kor Acad Pediatr Dent. 2016;43(3):410.
Kirthiga M, Poornima P, Praveen R, Gayathri P, Manju M, Priya M. Prevalence and severity of molar incisor hypomineralization in children aged 11–16 years of a city in Karnataka, Davangere. J Indian Soc Pedod Prev Dent. 2015;33(3):213–7.
Koruyucu M, Ozel S, Tuna EB. Prevalence and etiology of molar-incisor hypomineralization (MIH) in the city of Istanbul. J Dent Sci. 2018;13(4):318–28.
Krishnan R, Ramesh M, Chalakkal P. Prevalence and characteristics of MIH in school children residing in an endemic fluorosis area of India: an epidemiological study. Eur Arch Paediatr Dent. 2015;16(6):455–60.
Kuhnisch J, Heitmuller D, Thiering E, Brockow I, Hoffmann U, Neumann C, Heinrich-Weltzien R, Bauer CP, von Berg A, Koletzko S, et al. Proportion and extent of manifestation of Molar-Incisor-Hypomineralizations according to different phenotypes. J Public Health Dent. 2014;74(1):42–9.
Kuhnisch J, Kabary L, Malyk Y, Rothmaier K, Metz I, Hickel R, Heinrich J, Manton D, Standl M. Relationship between caries experience and demarcated hypomineralised lesions (including MIH) in the permanent dentition of 15-year-olds. Clin Oral Investig. 2018;22(5):2013–9.
Kusku OO, Caglar E, Sandalli N. The prevalence and aetiology of molar-incisor hypomineralisation in a group of children in Istanbul. Eur J Paediatr Dent. 2008;9(3):139–44.
Kuscu OO, Caglar E, Aslan S, Durmusoglu E, Karademir A, Sandalli N. The prevalence of molar incisor hypomineralization (MIH) in a group of children in a highly polluted urban region and a windfarm-green energy island. Int J Paediatr Dent. 2009;19(3):176–85.
Li L, Li J. Investigation of molar-incisor hypomineralization among children from 6 to 11 years in Lucheng district, Wenzhou city. Shanghai Kou Qiang Yi Xue. 2012;21(5):576–9.
Llena C, Calabuig E, Sanz JL, Melo M. Risk factors associated with carious lesions in permanent first molars in children: a seven-year retrospective cohort study. Int J Environ Res Public Health. 2020;17(4):1421.
Lopez Jordi Mdel C, Cortese SG, Alvarez L, Salveraglio I, Ortolani AM, Biondi AM. Comparison of the prevalence of molar incisor hypomineralization among children with different health care coverage in the cities of Buenos Aires (Argentina) and Montevideo (Uruguay). Salud Colect. 2014;10(2):243–51.
Lygidakis NA, Dimou G, Briseniou E. Molar-incisor-hypomineralisation (MIH). Retrospective clinical study in Greek children I Prevalence and defect characteristics. Eur Arch Paediatr Dent. 2008;9(4):200–6.
Bulani BM, Shetiya SH, Deepti A. Prevalence of molar incisor hypomineralization amongst 8 to 11 years old government school children in Pune, Maharashtra - 1 cross-sectional study. Pravara Med Rev. 2020;12(3):91–9.
Mahoney EK, Morrison DG. The prevalence of Molar-Incisor Hypomineralisation (MIH) in Wainuiomata children. N Z Dent J. 2009;105(4):121–7.
Mahoney EK, Morrison DG. Further examination of the prevalence of MIH in the Wellington region. N Z Dent J. 2011;107(3):79–84.
Martinez Gomez TP, Guinot Jimeno F, Bellet Dalmau LJ, Giner Tarrida L. Prevalence of molar-incisor hypomineralisation observed using transillumination in a group of children from Barcelona (Spain). Int J Paediatr Dent. 2012;22(2):100–9.
Martinovic B, Ivanovic M, Cvetkovic A, Todic J, Milojkovic Z, Pavlovic J, Tabakovic SZ, Stosovic-Kalezic I. Prevalence, characteristics and severity of hypomineralization of the first permanent molars and incisors in children from the northern part of Kosovo and Metohija. Srp Arh Celok Lek. 2017;145(7–8):364–9.
Mejia JD, Restrepo M, Gonzalez S, Alvarez LG, Santos-Pinto L, Escobar A. Molar Incisor Hypomineralization in Colombia: prevalence, severity and associated risk factors. J Clin Pediatr Dent. 2019;43(3):185–9.
Menoncin BLV, Portella PD, Ramos BLM, Assuncao L, de Souza JF, Menezes J. Dental anxiety in schoolchildren with molar incisor hypomineralization-a population-based cross-sectional study. Int J Paediatr Dent. 2019;29(5):615–23.
Mishra A, Pandey RK. Molar Incisor Hypomineralization: an epidemiological study with prevalence and etiological factors in Indian pediatric population. Int J Clin Pediatr Dent. 2016;9(2):167–71.
Mittal NP, Goyal A, Gauba K, Kapur A. Molar incisor hypomineralisation: prevalence and clinical presentation in school children of the northern region of India. Eur Arch Paediatr Dent. 2014;15(1):11–8.
Mittal R, Chandak S, Chandwani M, Singh P, Pimpale J. Assessment of association between Molar Incisor Hypomineralization and hypomineralized second primary molar. J Int Soc Prev Community Dent. 2016;6(1):34–9.
Mulic A, Cehajic E, Tveit AB, Stenhagen KR. How serious is Molar Incisor Hypomineralisation (MIH) among 8- and 9-year-old children in Bosnia-Herzegovina? A clinical study. Eur J Paediatr Dent. 2017;18(2):153–7.
Jans M, Diaz MJ, VErgara GC, Zaroro SC. Frequency and severity of the molar incisor hypomineralization in patients treated at the dental clinic of the Universidad de la Frontera. Int J Odontostomat. 2011;5(2):133–8.
Muratbegovic A, Zukanovic A, Markovic N. Molar-Incisor-Hypomineralisation impact on developmental defects of enamel prevalence in a low fluoridated area. Eur Arch Paediatr Dent. 2008;9(4):228–31.
Murietta-Pruneda JF, Torrs-Vargas J, Sánchez-Meza JC. Frequency and severity of Molar Incisor HypoMineralization (him) in a group of Mexican children. Rev Nac Odontol. 2014;12(23):7–14.
Negre-Barber A, Montiel-Company JM, Catala-Pizarro M, Almerich-Silla JM. Degree of severity of molar incisor hypomineralization and its relation to dental caries. Sci Rep. 2018;8(1):1248.
Ng JJ, Eu OC, Nair R, Hong CH. Prevalence of molar incisor hypomineralization (MIH) in Singaporean children. Int J Paediatr Dent. 2015;25(2):73–8.
Nisii F, Mazur M, De Nuccio C, Martucci C, Spuntarelli M, Labozzetta S, Fratini A, Sozzi S, Maruotti A, Vozza I, et al. Prevalence of Molar Incisor Hypomineralization among school children in Rome, Italy. Sci Rep. 2022;12(1):7343.
Nsour H, Masarwa N, Al-Rabati H, Alzoubi T, Aladwan ASA. Prevalence, etiology, severity and treatment of Molar Incisor Hypomineralization for 7 to 9 years old children attending royal medical services clinics in Amman – Jordan. J Royal Med Serv. 2018;25(1):70–7.
Ofi WA, Salih BA. Prevalence and severity of molar-incisor hypomineralisation with relation to its etiological factors among school children 7–9 years of Al-Najaf governorate. J Bagh Coll Dentistry. 2015;27(3):169.
Ordonez-Romero I, Jijon-Granja Y, Ubila-Mazzini W, Porro-Porro L, Alvarez-Giler G. Distribution of Molar Incisor Hypomineralization in Ecuadorian children. Dent Hypotheses. 2019;10:65–9.
Orellana-Herrera C, Bascuñan-Yañez K, Gambetta-Tassini K, Pérez-Valdés V. Underdiagnosis of enamel defects in family health centres of Talca city Chile. J Oral Res. 2020;9(9):195–201.
Oyedele TA, Folayan MO, Adekoya-Sofowora CA, Oziegbe EO, Esan TA. Prevalence, pattern and severity of molar incisor hypomineralisation in 8- to 10-year-old school children in Ile-Ife Nigeria. Eur Arch Paediatr Dent. 2015;16(3):277–82.
Petrou MA, Giraki M, Bissar AR, Basner R, Wempe C, Altarabulsi MB, Schafer M, Schiffner U, Beikler T, Schulte AG, et al. Prevalence of Molar-Incisor-Hypomineralisation among school children in four German cities. Int J Paediatr Dent. 2014;24(6):434–40.
Pitiphat W, Luangchaichaweng S, Pungchanchaikul P, Angwaravong O, Chansamak N. Factors associated with molar incisor hypomineralization in Thai children. Eur J Oral Sci. 2014;122(4):265–70.
Pitiphat W, Savisit R, Chansamak N, Subarnbhesaj A. Molar incisor hypomineralization and dental caries in six- to seven-year-old Thai children. Pediatr Dent. 2014;36(7):478–82.
Portella PD, Menoncin BLV, de Souza JF, de Menezes J, Fraiz FC, Assuncao L. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: a hierarchical approach. Int J Paediatr Dent. 2019;29(4):496–506.
Poureslami H, Shojaiepour R, Abbaspour S, Aminizadeh M, Khedmi M, Abbaspour S. Prevalence of the molar incisor hypomineralization in seven to twelve-year-old students of Kerman, Iran, in 2015–2016. J Oral Health Oral Epidemiol. 2018;7(1):21–6.
Preusser SE, Ferring V, Wleklinski C, Wetzel WE. Prevalence and severity of molar incisor hypomineralization in a region of Germany – a brief communication. J Public Health Dent. 2007;67(3):148–50.
Ray P, Mohanty UK, Sethi D, Mahakur M, Sharma G. Prevalence and treatment need of Molar Incisor Hypomineralisation in 8–12 year old school going children of Cuttack, Odisha. J Clin Diagn Res. 2020;14(3):5–9.
Reis PPG, Jorge RC, Americano GCA, Thiago Pontes NS, Peres A, Silva Oliveira AGE, Soviero VM. Prevalence and severity of Molar Incisor Hypomineralization in Brazilian children. Pediatr Dent. 2021;43(4):270–5.
Rizk H, Al-Mutairi M, Habibullah MA. The prevalence of Molar-Incisor Hypomineralization in primary schoolchildren aged 7–9 years in Qassim Region of Saudi Arabia. J Interdiscip Dentistry. 2018;8:44–8.
Rodriguez-Rodriguez M, Carrasco-Colmenares W, Ghanim A, Natera A, Acosta-Camargo MG. Prevalence and distribution of Molar Incisor Hypomineralization in children receiving dental care in Caracas Metropolitan Area Venezuela. Acta Odontol Latinoam. 2021;34(2):104–1112.
Saber F, Waly N, Moheb D. Prevalence of molar incisor hypomineralisation in a group of Egyptian children using the short form: a cross-sectional study. Eur Arch Paediatr Dent. 2018;19(5):337–45.
Saitoh M, Nakamura Y, Hanasaki M, Saitoh I, Murai Y, Kurashige Y, Fukumoto S, Asaka Y, Yamada M, Sekine M, et al. Prevalence of molar incisor hypomineralization and regional differences throughout Japan. Environ Health Prev Med. 2018;23(1):55.
Sakly E, Amor W, Zokkar N, Charavet C, Amor F: Prevalence of Molar Incisor Hypomineralisation Among School Children aged 7–12 years in Tunis, Tunisia. Pesquisa Brasileira em Odontopediatria e Clínica Integrada 2020 20.
Salem K, Aziz D, Asadi M. Prevalence and predictors of Molar Incisor Hypomineralization (MIH) among rural children in Northern Iran. Iran J Public Health. 2016;45(11):1528–30.
Salih BA, Khalaf MS. Prevalence of molar-incisor-hypomineralization among children attending pedodontic clinic of college of dentistry at Baghdad University. J baghdad Coll Dentistry. 2012;24(4):21–5.
Santos PS, Martins-Junior PA, Paiva SM, Klein D, Torres FM, Giacomin A, Goncalves BM, Konrath AC, Bolan M, Cardoso M. Prevalence of self-reported dental pain and associated factors among eight- to ten-year-old Brazilian schoolchildren. PLos One. 2019;14(4):e0214990.
Schmalfuss A, Stenhagen KR, Tveit AB, Crossner CG, Espelid I. Canines are affected in 16-year-olds with molar-incisor hypomineralisation (MIH): an epidemiological study based on the Tromso study: “Fit Futures.” Eur Arch Paediatr Dent. 2016;17(2):107–13.
Shin J, An U, Kim S, Jeong T. The prevalence of molar incisor hypomineralization and status of first molars in primary school children. J Kor Acad Pediatr Dent. 2010;37(2):179–84.
Shin J, Lee G, Kim J, Kim S. Prevalence and clinical features of Molar-Incisor Hypomineralization in adolescents in Yangsan. J Kor Acad Pediatr Dent. 2017;44(2):210–8.
Shojaeepour S, Jalali F, Shokrizadeh M, Riahi-Madvar R, Torabi-Parizi M, Shojaiepour R. Assessing the prevalence of molar-incisor hypomineralization and its effects on oral health-related quality of life in children aged 8–12 years in the city of Kerman Iran. J Oral Health Oral Epidemiol. 2020;9(3):143–8.
Shrestra R, Upadhaya S, Bajracharya M. Prevalence of Molar Incisor Hypomineralisation among school children in Kavre. Kathmandu Univ Med J. 2014;45(1):38–42.
Sidaly R, Schmalfuss A, Skaare AB, Sehic A, Stiris T, Espelid I. Five-minute Apgar score </= 5 and Molar Incisor Hypomineralisation (MIH) - a case control study. BMC Oral Health. 2016;17(1):25.
Singh R, Srivastan B, Pupta N. Prevalence and pattern of Molar Incisor Hypomineralization in Delhi Region. J Anatomical Soc India. 2021;69(3):150–4.
Sonmez H, Yildirim G, Bezgin T. Putative factors associated with molar incisor hypomineralisation: an epidemiological study. Eur Arch Paediatr Dent. 2013;14(6):375–80.
Sosa-Soto J, Padron-Covarrubias AI, Marquez-Preciado R, Ruiz-Rodriguez S, Pozos-Guillen A, Pedroza-Uribe IM, Bayardo-Gonzalez RA, Garrocho-Rangel A. Molar Incisor Hypomineralization (MIH): prevalence and degree of severity in a Mexican pediatric population living in an endemic fluorosis area. J Public Health Dent. 2022;82(1):3–10.
Subramaniam P, Gupta T, Sharma A. Prevalence of Molar Incisor Hypomineralization in 7-9-year-old children of Bengaluru City India. Contemp Clin Dent. 2016;7(1):11–5.
Tadikonda AN, Acharya S, Pentapati KC. Prevalence of Molar Incisor Hypomineralization and its relation with dental caries in school children of Udupi district South India. World J Dentistry. 2015;6(3):143–6.
Tagelsir Ahmed A, Soto-Rojas AE, Dean JA, Eckert GJ, Martinez-Mier EA. Prevalence of molar-incisor hypomineralization and other enamel defects and associated sociodemographic determinants in Indiana. J Am Dent Assoc. 2020;151(7):491–501.
Ravichandra KS, Muppa R, Srikanth K, Kantipudi MJ, Ram KC. Molar Incisor Hypomineralization prevalence in the schoolchildren of Gannavaram Mandal, Krishna District, Andhra Pradesh, India: a cross-sectional study. Int J Clin Pediatr Dent. 2021;14(6):737–40.
Temilola OD, Folayan MO, Oyedele T. The prevalence and pattern of deciduous molar hypomineralization and molar-incisor hypomineralization in children from a suburban population in Nigeria. BMC Oral Health. 2015;15:73.
Temilola DO, Folayan MO. Distinguishing predisposing factors for enamel hypoplasia and molar-incisor hypomineralization in children in Ile-Ife Nigeria. Braz J Oral Sci. 2015;14(4):318–22.
Tourino LF, Correa-Faria P, Ferreira RC, Bendo CB, Zarzar PM, Vale MP. Association between Molar Incisor Hypomineralization in schoolchildren and both prenatal and postnatal factors: a population-based study. PLos One. 2016;11(6): e0156332.
Villanueva Gutierrez T, Barrera Ortega CC, Garcia Perez A, Gonzalez-Aragon Pineda AE. Relationship between Molar Incisor Hypomineralization (MIH) severity and cavitated carious lesions in schoolchildren. Acta Odontol Latinoam. 2019;32(3):133–40.
Villanueva-Gutierrez T, Irigoyen-Camacho ME, Castano-Seiquier A, Zepeda-Zepeda MA, Sanchez-Perez L, Frechero NM. Prevalence and severity of Molar-Incisor Hypomineralization, maternal education, and dental caries: a cross-sectional study of Mexican schoolchildren with low socioeconomic status. J Int Soc Prev Community Dent. 2019;9(5):513–21.
Wuollet E, Laisi S, Salmela E, Ess A, Alaluusua S. Molar-incisor hypomineralization and the association with childhood illnesses and antibiotics in a group of Finnish children. Acta Odontol Scand. 2016;74(5):416–22.
Wuollet E, Laisi S, Alaluusua S, Waltimo-Siren J. The Association between Molar-Incisor Hypomineralization and dental caries with socioeconomic status as an explanatory variable in a group of Finnish Children. Int J Environ Res Public Health. 2018;15(7):1324.
Zekirulla M, Khormi EA, Bakri HM, Tarrosh MY, Shubayr MA, Almubarak H. Prevalence of Molar Incisor Hypomineralisation (MIH) in 7–10 year old school children in southern Saudi Arabia: a cross-sectional study. Ann Trop Med Public Health. 2018;2:192–207.
Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH. Molar incisor hypomineralisation: prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent. 2011;12(1):31–6.
Paglia L. Molar Incisor Hypomineralization: paediatricians should be involved as well! Eur J Paediatr Dent. 2018;19(3):173.
Zhao D, Dong B, Yu D, Ren Q, Sun Y. The prevalence of Molar Incisor Hypomineralization: evidence from 70 studies. Int J Paediatr Dent. 2018;28(2):170–9.
Guo Y, Pandis N. Sample-size calculation for repeated-measures and longitudinal studies. Am J Orthod Dentofacial Orthop. 2015;147(1):146–9.
Kuhnisch J, Standl M, Hickel R, Heinrich J. Molar incisor hypomineralisation (MIH)-discussion of prevalence and etiology with special reference to the results from the Munich birth cohorts GINIplus and LISA. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2021;64(8):924–30.
Garot E, Couture-Veschambre C, Manton D, Beauval C, Rouas P. Analytical evidence of enamel hypomineralisation on permanent and primary molars amongst past populations. Sci Rep. 2017;7(1):1712.
Crombie FA, Manton DJ, Palamara JE, Zalizniak I, Cochrane NJ, Reynolds EC. Characterisation of developmentally hypomineralised human enamel. J Dent. 2013;41(7):611–8.
Fearne J, Anderson P, Davis GR. 3D X-ray microscopic study of the extent of variations in enamel density in first permanent molars with idiopathic enamel hypomineralisation. Br Dent J. 2004;196(10):634–8 discussion 625.
Elfrink ME, Ghanim A, Manton DJ, Weerheijm KL. Standardised studies on Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPM): a need. Eur Arch Paediatr Dent. 2015;16(3):247–55.
Peritz E. Berkson’s bias revisited. J Chronic Dis. 1984;37(12):909–16.
Acknowledgements
Not applicable.
Funding
Open access funding provided by University of Basel The study was funded by the Clinic of Preventive and Concervative Dentistry, Center of Dental Medicine, University of Zurich.
Author information
Authors and Affiliations
Contributions
P.S. and U.H. conceptualized the review. B.S. and P.S. performed the literature search and data extraction. B.S. performed the quality assessment. U.H. performed the statistics and prepared Figs. 2 3 and 4. P.S. wrote the manuscript text and prepared Fig. 1. K.W.N., F.W. and T.A. carefully revised and corrected the text. All authors reviewed the manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Search masks. Table 2. Quality assessment. Fig. 1. Prevalences of MIH in different areas of the world.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sluka, B., Held, U., Wegehaupt, F. et al. Is there a rise of prevalence for Molar Incisor Hypomineralization? A meta-analysis of published data. BMC Oral Health 24, 127 (2024). https://doi.org/10.1186/s12903-023-03637-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03637-0