Abstract
Background
Evidence of possible beneficial effects of dietary diabetes risk reduction score (DDRRS) on reducing the risk of various chronic diseases such as metabolic syndrome (MetS) are limited. This is a prospective, population-based cohort study, which aimed to investigate the relationship of the DDRRS and its components with MetS incident in Iranian adults.
Methods
Individuals without MetS (n=3561) were recruited from participants of the Tehran Lipid and Glucose Study (2009-2011) and followed for a mean of 6.01 years. A validated food frequency questionnaire was used to determine the DDRRS using based on eight components, including higher intakes of cereal fiber, nuts, coffee, and polyunsaturated: saturated fat ratio and lower intakes of red or processed meats, sugar-sweetened beverages, trans fatty acids, and low glycemic index. We used the multivariable logistic regression analysis to determine the odds ratio (ORs) and 95 % confidence interval (CI) of MetS across the tertiles of DDRRS.
Results
The mean (SD) age of individuals was 38.1(12.6) years at baseline. Median (25-75 interquartile range) DDRRS for all participants was 20(18-22). During the study follow-up, 682(19.1 %) new cases of MetS were reported. Based on the age and sex-adjusted model, participants in highest tertile of DDRRS had lower risk of MetS in compared with the lowest one (OR=0.64;95 %CI:0.52-0.79, P for trend=0.001). In the multivariable adjusted model, after adjustment for all possible confounding variables, the risk of MetS is decreased across tertiles of DDRRS (OR=0.60;95 %CI:0.48-0.75, P for trend=0.001). Also, higher scores of some DDRRS components including red and processed meat, sugar sweetened beverages, and coffee were related to decreased incidence of MetS.
Conclusions
The results of this study revealed that greater adherence to DDRRS can be associated with decreased risk of MetS in Iranian adult.
Similar content being viewed by others
Background
Metabolic syndrome (MetS) is a clustering of metabolic risk factors, including central obesity, hypertriglyceridemia, low high-density lipoprotein cholesterol (HDL-C), elevated blood pressure, and hyperglycemia [1], which can increase the risk of type 2 diabetes, cardiovascular disease (CVD), cancer, and all-cause mortality [2, 3]. Insulin resistance and dysregulation of lipid metabolism playing a key role in the pathogenesis of MetS [4, 5]. In addition to genetic predisposition, lifestyle factors (include smoking, physical inactivity, alcohol consumption, and especially inappropriate dietary intakes), and socioeconomic status are the main causative risk factors of MetS [2, 6,7,8].
Quality of the diet plays an important role in the progression of MetS [9] and the role of several nutritional factors in the incidence of MetS has been reported [10,11,12,13,14,15,16,17]. Based on single food group or nutrient-specific data in the etiology of chronic diseases dietary guidelines have some limitations, whereas whole dietary patterns are far more applicable [18, 19]. Hence investigating the association between nutritional factors in the form of a single food pattern score and risk of chronic diseases, such as MetS can provide more accurate and applicable findings.
In 2015, a study by Rhee et al. [20] computed dietary diabetes risk reduction score (DDRRS) as a healthy diet score including SSB, coffee, nuts, red and processed meats, GI, cereal fiber, the ratio of P:S, and trans fats, which indicated that higher adherence to DDRRS could decrease the risk of diabetes incident. However, to the best of our knowledge, the association of DDRRS as a single set of different dietary factors and incident MetS has not yet been assessed. Therefore, in this study, we aimed to investigate the association of DDRRS and its components with the risk of incident MetS after 6.01 years of follow-up among Tehranian adult participants.
Methods
Subjects
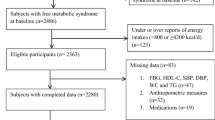
This study was performed in the framework of the Tehran Lipid and Glucose Study (TLGS), a population-based cohort study conducted to assess the risk factors for non-communicable diseases among a representative urban population of Tehran, including 15,005 participants aged ≥3 years [21]. In the fourth survey of the TLGS (2009–2011), of 12,823 participants, 7956 were randomly selected for dietary assessment. For the current study, 4660 adult men and women (aged>18 years) free of MetS at baseline, with complete baseline data, were recruited. We excluded participants who under- or over-reported energy intakes (< 800 kcal/d or > 4200 kcal/d, respectively) (n=255), or were on specific diets for hypertension, diabetes, or dyslipidemia (n=32), those with a history of myocardial infarction, cerebral vascular accident, cancer (n=47), and pregnant and lactating women (n=94); some individuals fell into more than one exclusion category. Finally, 4249 participants were followed until survey VI, for a mean period of 6.01 years from the baseline examination. After excluding the participants who left the study (n=688), final analyses were conducted on data of 3561 adults (Fig. 1).
Dietary assessment
The dietary intake of participants over the previous year was assessed using a valid and reliable 168-item semi-quantitative food frequency at baseline [22]. Trained dietitians asked participants to designate their consumption frequency for each food item during the previous year on a daily, weekly, or monthly basis; portion sizes of consumed foods, reported in household measures, were then converted to grams. Since, the Iranian Food Composition Table (FCT) is incomplete and has limited data on the nutrient content of raw foods and beverages, the United States Department of Agriculture (USDA) FCT [23] was used. For national foods not listed in the USDA FCT, the Iranian FCT [24] was used.
We have determined dietary diabetes risk reduction score based on the Rhee et al. study [20] with focusing on eight components, including higher intakes of cereal fiber, nuts, coffee, and P:S ratio and lower intakes of red or processed meats, sugar-sweetened beverages, trans fatty acids, and GI. For each component, subjects were classified into quartiles according to their intake ranking, and component scores were used for cereal fiber, nuts, coffee, and P:S ratio to determine the individual’s quartiles rankings, e.g. participants in the lowest quartile were assigned 1 point, and those in the highest quartile were assigned 4 points. Scores were reversed for red or processed meats, sweetened beverages, trans fat, and GI. Therefore, individuals in the lowest quartile were given a score of 4 points, and those in the highest quartile were scored 1 point. We then summed up the points for all eight items to compute the DDRRS. The range of total DDRRS was from 8 (minimum adherence) to 32 (maximal adherence).
Physical activity assessment
The physical activity levels of participants were determined using a modifiable activity questionnaire (MAQ), previously modified and validated among Iranians [25]. Participants were asked to report and identify the frequency and time spent on activities of light, moderate, hard, and very hard intensity during the past 12 months, according to a list of common activities of daily life; physical activity levels were reported as metabolic equivalent hours per week (MET-h/wk).
Demographic, anthropometric, and lifestyle measures
Data on demographic, anthropometric, and biochemical variables were assessed at baseline (2006–2008). Trained interviewers used pretested questionnaires to collect information, including demographic data, medical history, medications, and smoking habits. We measured the weight of participants to the nearest 100 g using digital scales with minimal clothing and without shoes. Height was measured to the nearest 0.5 cm using a tape meter, in a standing position without shoes. Body mass index (BMI) was calculated as weight (kg) divided by the square of the height (m2). Blood pressure of each participant was measured twice on the right arm with a minimum interval of 30 s via a standardized mercury sphygmomanometer with an accuracy of 2 mmHg after a 15-minute rest sitting on a chair; the mean of the two measurements was considered to be the blood pressure of the participant.
Biochemical measures
A blood sample was taken after 12-14 h of overnight fasting in a sitting position according to the standard protocol and centrifuged within 30-45 min of collection. All blood analyses were performed at the TLGS research laboratory on the day of blood collection. The samples were analyzed using the Selectra 2 auto-analyzer (Vital Scientific, Spankeren, The Netherlands). An enzymatic colorimetric method with glucose oxidase was used to determine fasting plasma glucose (FPG). Both inter-and intra-assay coefficient variations were 2.2 % for FPG. Triglyceride (TGs) level was measured using an enzymatic colorimetric analysis with glycerol phosphate oxidase. Total cholesterol (TC) was measured with cholesterol esterase and cholesterol oxidase, using the enzymatic colorimetric method. High-density lipoprotein cholesterol was measured after precipitation of the apolipoprotein B-containing lipoproteins with phosphotungistic acid. Analyses were performed using commercial kits (Pars Azmoon Inc., Tehran, Iran) and a Selectra 2 auto-analyzer (Vital Scientific, Spankeren, Netherlands). Inter-assay and intra-assay coefficients of variations were 1.6 % and 0.6 % for TGs, 2 % and 0.5 % for HDL-C, and 2 % and 0.5 % for TC, respectively. Low-density lipoprotein cholesterol (LDL-C) was calculated from the serum TC, TGs, and HDL-C concentrations and expressed in mg/dl using the Friedewald formula.
Definitions
MetS was defined according to the joint interim statement as the presence of any 3 of 5 following factors [26]: (1) abdominal obesity as WC≥95 cm for both genders, according to the new cutoff points of WC for Iranian Adults [27]; (2) FPG≥ 100 mg/dl or drug treatment; (3) fasting TGs≥ 150 mg/dl or drug treatment; (4) fasting HDL-C<50 mg/dl for women and <40 mg/dl for men or drug treatment; and (5) high BP was defined as SBP≥130 mmHg, DBP≥85 mmHg, or antihypertensive drug treatment.
Statistical analysis
The Statistical Package for Social Sciences (Version 15.0; SPSS, Chicago, IL) was used to perform all analyzes. The normality of the variables was checked using histogram charts and Kolmogorov–Smirnov test. Participants were categorized according to tertiles of DDRRS cut-points; baseline characteristics of the participants are presented as the mean ±SD or median (25-75 interquartile) for continuous variables and percentages for categorical variables. Linear regression and Chi-square were used to test the trends of continuous and categorical variables across tertiles of DDRRS, respectively. Multivariable logistic regression models were used with MetS (and its components) as the dependent variable and DDRRS as an independent variable to estimate the risk of 6.01 years incident outcomes and the odds ratio (ORs) and 95 % confidence intervals (CIs) were reported. The first tertile of DDRRS is considered as the reference category. Potential confounders were sex, age, BMI, physical activity, smoking, and daily energy intake. We also assessed the association each DDRRS components with risk of MetS incident, independently (Fig. 2). For scoring each positive component of DDRRS, subjects were classified into quartiles according to their intake ranking, and component scores were used for cereal fiber, nuts, coffee, and P:S ratio to determine the individual’s quartiles rankings, e.g. participants in the lowest quartile were assigned 1 point, and those in the highest quartile were assigned 4 points. Scores were reversed for negative components including red or processed meats, sweetened beverages, trans fat, and GI. Therefore, individuals in the lowest quartile were given a score of 4 points, and those in the highest quartile were scored 1 point. Next, individuals were categorized based on score of each component DDRRS and finally, the odds of MetS were determined across quartiles of each DDRRS components score. P-values <0.05 were considered to be statistically significant.
Results
The mean age of participants (38.8 % male) was 38.1±12.6 years at baseline. During an average of 6.01 years of follow-up, 682 (19.1 %) new cases of MetS were identified. The median (25-75 interquartile range) of the DDRRS for all participants was 20 (18-22).
Baseline socio-demographic and biochemical characteristics of the study population across tertiles of DDRRS are reported in Table 1. Compared to the lowest tertile, participants in the highest tertile of DDRRS were more likely to be older, low smoked, and had higher levels of TC, LDL-C, HDL-C, FPG, and had lower BMI and physical activity level (P<0.05). No significant differences in WC, TGs, SBP, and DBP were observed in participants according to tertiles of DDRRS.
Baseline dietary intakes of participants across tertiles of DDRRS score are presented in Table 2. Individuals in the highest tertile of DDRRS had higher intakes of cereal fiber, PUFA: SFA ratio, nuts, and coffee, but lower intakes of red and processed meat, sugar-sweetened beverages, and trans fatty acids. Dietary intakes of total energy, protein, carbohydrates, total dietary fiber, vitamin C, potassium, magnesium, and calcium were significantly increased across DDRRS tertiles (P<0.001), whereas intakes of total fat, sucrose, and GL level were decreased (P< 0.001). There were no significant differences in any other nutritional measures across tertiles of DDRRS.
The OR of MetS according to tertiles of DDRRS is shown in Table 3. In the age and sex-adjusted model, the odds of MetS were lower in the highest tertile of the DDRRS compared to the lowest one (OR=0.64; 95 %CI: 0.52–0.79, P for trend=0.001). Also, in the multivariable-adjusted model, after controlling age, sex, BMI, physical activity, smoking, education level, and daily energy intake, a negative association between the high score of DDRRS and 6-year incidence of MetS remained significant (OR=0.60; 95 %CI:0.48–0.75, P for trend=0.001).
The ORs and 95 % CIs of incident MetS according to quartiles of the DDRRS components scores among participants are presented in Fig. 2. After adjustment of potential confounders including age, sex, smoking status, BMI, physical activity, education level, and total energy intake, OR of MetS for individuals in the highest, compared with the lowest, scores of red and processed meat was 0.59 (95 % CI:0.44-0.75), for sugar sweetened beverages 0.53 (95 % CI:0.40-0.70), and for coffee it was 0.47 (95 % CI:0.37-0.60), P for trend<0.001). In addition, a remarkable reducing linear trend was observed across the scores of red and processed meat, sugar sweetened beverages, and coffee for the risk of incident MetS (P for trend <0.001, Fig. 2).
We also showed the ORs and 95 % CIs of MetS components risk according to tertiles of the DDRRS scores among individuals in Table 4. After adjustment of potential confounders including age, sex, smoking status, BMI, physical activity, education level, and total energy intake, the odds of central obesity (OR=0.71; 95 %CI: 0.55–0.90, P for trend=0.005) and high blood pressure (OR=0.77; 95 %CI: 0.62–0.95, P for trend=0.018) were lower in the highest tertile of the DDRRS compared to the lowest one. Also, after adjustment of potential confounders, OR (95 %CI) of high blood glucose, high TGs, and low-HDL-C for individuals in the highest, compared with the lowest, score of DDRRS was 0.85 (95 % CI:0.67-1.07), 0.84 (95 % CI:0.70-1.02), and 0.94 (95 % CI:0.79-1.11), respectively, (P for trend>0.05).
Discussion
In the current study, we investigated the association of the DDRRS and risk of MetS in the framework of longitudinal population-based study after a 6.01-year follow-up. Findings indicated that greater adherence to the DDRRS is associated with decreased risk of MetS independent of confounding variables including age, sex, smoking status, BMI, physical activity, educational level, and total energy intake. Also, higher scores of some DDRRS components including red and processed meat, sugar sweetened beverages, and coffee were related to decreased risk of MetS incident. Furthermore, our results report a negative association between DDRRS and risk of some MetS components including central obesity and high blood pressure.
To the best of our knowledge, evidence on the association between DDRRS and risk of chronic diseases is limited to the cohort study on the American population, indicating the protective role of DDRRS on the development of diabetes [20]. Our findings regarding the inverse association between DDRRS and incident MetS are consistent with the finding of the Rhee et al. study, which reported that the higher adherence to DDRRS was associated with decreased risk of type 2 diabetes in all racial and ethnic groups by more than 30 % [20]. Also, although there is no study on the association between the DDRRS-style diet and risk of MetS, our study results on the healthy characteristics of the DDRRS are comparable with beneficial effects of healthy dietary indices such as DASH and Mediterranean diet in reducing the risk of MetS. In agreement with the results of our study, Asghari et al. study has revealed that higher adherence to the DASH-style diet rich in nuts, whole grains, fruits, vegetables, and legumes with lower intakes of carbonated beverages and red meat decreased the risk of MetS [28]. Also, higher intakes of healthy food groups including whole grains, monounsaturated fat, plant proteins, seafood, fruits, and vegetables, based on the Mediterranean diet significantly have been associated with the lower risk of MetS [29].
The beneficial effect of DDRRS on decreasing the risk of MetS could be partly attributed to the inclusion of nuts, coffee, unsaturated fatty acids, and cereal fibers as positive, and red and processed meat, SSB, trans fatty acid, and high GL as negative components [10,11,12,13,14,15,16,17]. Previous reports have shown that higher intakes of each positive component of DDRRS including nuts, coffee, unsaturated fatty acids, and cereal fibers can play an important role in ameliorating the burden of MetS. Strong evidence indicates that high content of fiber in DDRRS along with low dietary GI may decrease the risk of incident MetS by improving metabolic components including glycemic control, insulin resistance, dyslipidemia, obesity, and blood pressure [15]. The mechanisms of dietary fiber on MetS components are suggested to be related to the reduction in nutrients absorption rate, appetite suppression, regulation of energy homeostasis, altering the gut microbiota, modulating inflammatory cytokines and endothelial dysfunction, regulating hormonal, and improving glucose homeostasis [15, 30, 31]. Also, the greater adherence to a high GI and GL diet is associated with the higher risk of develo** MetS and central obesity, indicating an adverse effect of high-GL dietary pattern on the MetS [16]. Furthermore, it has been reported that high intakes of nuts and coffee is related to a more than 10 % reduction in the risk of MetS [14, 32]. The antioxidant components contained in nuts and coffee, including vitamin E, niacin, potassium and magnesium, fiber, MUFA, PUFA, polyphenols, phytosterols, and other dietary antioxidants suggested its protective role in MetS via the effect on inflammation and oxidative status, endothelial function, insulin resistance, and insulin secretion [14, 17, 32].
Lower consumption of negative components of DDRRS, including red and processed meat, SSB, the trans fatty acid is vital for the prevention of MetS [10,11,12]. A meta-analysis revealed that greater intakes of total, red, and processed meat are associated with increased risk of MetS by 14 %, 33 %, and 35 %, respectively [11]. Red and processed meats contain a high amount of total fat, saturated fat, and heme-iron. Higher SFA intake might increase MetS risk by increasing the development of obesity, hyperinsulinemia, and hyperglycemia. High levels of inflammatory mediators including C-reactive protein, increased nitrosamines production, and promotion of oxidative stress in individuals with high red and processed meat consumption might be the main reasons for the increased risk of MetS [11]. Also, high intake of TFA can cause MetS through the adverse effect on circulating lipid levels, triggering systemic inflammation, inducing endothelial dysfunction, increase of visceral adiposity, body weight, and insulin resistance [10]. Sugar-sweetened beverages have high added sugar content, low satiety potential, and incomplete compensatory reduction in energy intake, which leads to positive energy balance, so the high consumption of SSBs can increase the risk of MetS, because of their contribution to weight gain [12]. Overall, according to the components of DDRRS, this dietary score is rich in antioxidant vitamins and minerals, and phenolic compounds, and has a high unsaturated fatty acid content that mediates its effects on metabolic abnormality through possible mechanisms including anti-inflammatory, anti-oxidant, and anti-atherogenic properties, decreasing visceral adiposity and improving hyperglycemia and hyperinsulinemia.
In general, individuals with higher adherence to DDRRS score tend to have higher intakes of plant protein and plant fatty acids and lower intakes of dietary TFA and animal fats. Also, a diet with a higher score of DDRRS is a low GI dietary pattern rich in fiber and phytochemicals and poor in simple sugar. Therefore, a dietary pattern with DDRRS characteristics may be associated with a reduced risk of cardiometabolic risk factors such as insulin resistance, glucose intolerance, dyslipidemia, weight gain, and elevated blood pressure.
The current study has several important strengths. To the best of our knowledge, this is the first study with a prospective design to investigate the association of DDRRS with the risk of MetS, in a relatively large sample with a long-term follow-up. The use of valid and reliable food-frequency and physical activity questionnaires were important strengths of this study. This study however has its limitations. First, although similar to epidemiological studies, in the current study valid questionnaires were used for dietary and physical activity assessment, some measurement errors are inevitable. Also, although major confounding variables were adjusted in our models, there may still be residual or unmeasured confounders the effects of which cannot be ruled out.
Conclusions
The results of the current study showed that greater adherence to DDRRS are associated with decreased risk of MetS. This is an important finding since it can help to define a dietary pattern that is easily adhered to by the public to prevent the growing poor health outcomes such as metabolic abnormalities.
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
confidence interval
- CVD:
-
cardiovascular disease
- DBP:
-
diastolic blood pressure
- DDRRS:
-
dietary diabetes risk reduction score
- FCT:
-
Food Composition Table
- FFQ:
-
food frequency questionnaire
- FPG:
-
Fasting plasma glucose
- GI:
-
glycemic index
- HDL-C:
-
high-density lipoprotein cholesterol
- MAQ:
-
modifiable activity questionnaire
- MET-h/wk:
-
metabolic equivalent hours per week
- MetS:
-
metabolic syndrome
- OR:
-
odds ratio
- TFA:
-
trans fatty acids
- P:
-
S:polyunsaturated to saturated fats
- PUFA:
-
poly unsaturated fatty acids
- SFA:
-
saturated fatty acids
- SSB:
-
sugar sweetened beverages
- TC:
-
Total cholesterol
- TGs:
-
Triglyceride
- TLGS:
-
Tehran Lipid and Glucose Study
- SBP:
-
systolic blood pressure
- SPSS:
-
Statistical Package for Social Sciences program
References
Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Current Hypertension Reports. 2018;20(2):12.
Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, et al. The metabolic syndrome. Endocrine reviews. 2008;29(7):777–822.
O’Neill S, O’Driscoll L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2015;16(1):1–12.
Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37(12):1595-607.
DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes care. 1991;14(3):173–94.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Jama. 2002;287(3):356–9.
Mirmiran P, Asghari G, Farhadnejad H, Eslamian G, Hosseini-Esfahani F, Azizi F. Low carbohydrate diet is associated with reduced risk of metabolic syndrome in Tehranian adults. International journal of food sciences and nutrition. 2017;68(3):358–65.
Mirmiran P, Asghari G, Farhadnejad H, Alamdari S, Dizavi A, Azizi F. The Relationship Between Occupation Transition Status and Metabolic Syndrome in Adult Women: Tehran Lipid and Glucose Study. Metabolic syndrome and related disorders. 2016;14(5):265–71.
McCullough ML, Feskanich D, Stampfer MJ, Giovannucci EL, Rimm EB, Hu FB, et al. Diet quality and major chronic disease risk in men and women: moving toward improved dietary guidance. The American Journal of Clinical Nutrition. 2002;76(6):1261–71.
Micha R, Mozaffarian D. Trans fatty acids: effects on metabolic syndrome, heart disease and diabetes. Nature reviews Endocrinology. 2009;5(6):335–44.
Kim Y, Je Y. Meat Consumption and Risk of Metabolic Syndrome: Results from the Korean Population and a Meta-Analysis of Observational Studies. Nutrients. 2018;10(4):390.
Malik VS, Popkin BM, Bray GA, Després J-P, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes care. 2010;33(11):2477–83.
Zhang Y, Zhang DZ. Relationship Between Nut Consumption and Metabolic Syndrome: A Meta-Analysis of Observational Studies. 2019;38(6):499–505.
Shang F, Li X, Jiang X. Coffee consumption and risk of the metabolic syndrome: A meta-analysis. Diabetes & metabolism. 2016;42(2):80–7.
Chen J-P, Chen G-C, Wang X-P, Qin L, Bai Y. Dietary Fiber and Metabolic Syndrome: A Meta-Analysis and Review of Related Mechanisms. Nutrients. 2017;10(1):24.
Juanola-Falgarona M, Salas-Salvadó J, Buil-Cosiales P, Corella D, Estruch R, Ros E, et al. Dietary Glycemic Index and Glycemic Load Are Positively Associated with Risk of Develo** Metabolic Syndrome in Middle-Aged and Elderly Adults. Journal of the American Geriatrics Society. 2015;63(10):1991–2000.
Guo X-F, Li X, Shi M, Li D. n-3 Polyunsaturated Fatty Acids and Metabolic Syndrome Risk: A Meta-Analysis. Nutrients. 2017;9(7):703.
Williams CM, Lovegrove JA, Griffin BA. Dietary patterns and cardiovascular disease. The Proceedings of the Nutrition Society. 2013;72(4):407-11.
Cespedes EM, Hu FB. Dietary patterns: from nutritional epidemiologic analysis to national guidelines. The American Journal of Clinical Nutrition. 2015;101(5):899–900.
Rhee JJ, Mattei J, Hughes MD, Hu FB, Willett WC. Dietary diabetes risk reduction score, race and ethnicity, and risk of type 2 diabetes in women. Diabetes care. 2015;38(4):596–603.
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10:5.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public health nutrition. 2010;13(5):654–62.
The Nutrient Data Laboratory. Food Composition Table (FCT), Food and Nutrition Information Center, United State Department of Agriculture (USDA). 2021. fdc.nal.usda.gov.
Azar M, Sarkisian E. Food composition table of Iran. Tehran: National Nutrition and Food Research Institute, Shaheed Beheshti University. 1980;65.
Momenan AA, Delshad M, Sarbazi N, Rezaei Ghaleh N, Ghanbarian A, Azizi F. Reliability and validity of the Modifiable Activity Questionnaire (MAQ) in an Iranian urban adult population. Archives of Iranian medicine. 2012;15(5):279–82.
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the Metabolic Syndrome. Circulation. 2009;120(16):1640–5.
Azizi F, Hadaegh F, Khalili D, Esteghamati A, Hosseinpanah F, Delavari A, et al. Appropriate definition of metabolic syndrome among Iranian adults: report of the Iranian National Committee of Obesity. Archives of Iranian medicine. 2010;13(5):426–8.
Asghari G, Yuzbashian E, Mirmiran P, Hooshmand F, Najafi R, Azizi F. Dietary approaches to stop hypertension (DASH) dietary pattern is associated with reduced incidence of metabolic syndrome in children and adolescents. The Journal of pediatrics. 2016;174:178–84. e1.
Godos J, Zappalà G, Bernardini S, Giambini I, Bes-Rastrollo M, Martinez-Gonzalez M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: a meta-analysis of observational studies. International journal of food sciences and nutrition. 2017;68(2):138–48.
Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ. Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. The New England journal of medicine. 2000;342(19):1392–8.
He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation. 2010;121(20):2162–8.
Salas-Salvado J, Guasch-Ferre M, Bullo M, Sabate J. Nuts in the prevention and treatment of metabolic syndrome. The American journal of clinical nutrition. 2014;100(suppl_1):399S-407S.
Acknowledgements
We express our appreciation to the participants in the Tehran Lipid and Glucose Study for their enthusiastic support and the staff of the Research Institute for Endocrine Sciences, Tehran Lipid and Glucose Study Unit for their valuable help.
Funding
This work was funded by the Shahid Beheshti University of Medical Sciences, Tehran, Iran. The funding body has no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
H.F, G.A, and K.P contributed to the conception, design, and statistical analysis. H.F and F.T contributed to data collection and manuscript drafting. P.M and F.A supervised the study. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from all participants. All procedures performed in studies involving human participants adhered the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was also approved by the ethics research committee of the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Consent for publication
Not applicable.
Competing interests
The authors declared there is no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mirmiran, P., Farhadnejad, H., Teymoori, F. et al. The association of dietary diabetes risk reduction score and its components with risk of metabolic syndrome incident in Tehranian adults. BMC Endocr Disord 21, 206 (2021). https://doi.org/10.1186/s12902-021-00872-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-021-00872-w