Abstract
Objective
Prostate cancer (PC) is a significant disease affecting men’s health worldwide. More than 60% of patients over 65 years old and more than 80% are diagnosed with localized PC. The current choice of treatment modalities for localized PC and whether overtreatment is controversial. Therefore, we wanted to construct a nomogram to predict the risk factors associated with cancer-specific survival (CSS) and overall survival (OS) in elderly patients with localized PC while assessing the survival differences in surgery and radiotherapy for elderly patients with localized PC.
Methods
Data of patients with localized PC over 65 years were obtained from the Surveillance, Epidemiology, and End Results (SEER) database. Univariate and multivariate Cox regression models were used to determine independent risk factors for CSS and OS. Nomograms predicting CSS and OS were built using multivariate Cox regression models. The consistency index (C-index), the area under the subject operating characteristic curve (AUC), and the calibration curve were used to test the accuracy and discrimination of the prediction model. Decision curve analysis (DCA) was used to test the potential clinical value of this model.
Results
A total of 90,434 patients over 65 years and diagnosed with localized PC from 2010 to 2018 were included in the study. All patients were randomly assigned to the training set (n = 63,328) and the validation set (n = 27,106). Univariate and multivariate Cox regression model analysis showed that age, race, marriage, T stage, surgical, radiotherapy, prostate-specific antigen (PSA), and Gleason score (GS) were independent risk factors for predicting CSS in elderly patients with localized PC. Age, race, marriage, surgery, radiotherapy, PSA, and GS were independent risk factors for predicting OS in elderly patients with localized PC. The c-index of the training and validation sets for the predicted CSS is 0.802(95%CI:0.788–0.816) and 0.798(95%CI:0.776–0.820, respectively). The c-index of the training and validation sets for predicting OS is 0.712(95%:0.704–0.720) and 0.724(95%:0.714–0.734). It shows that the nomograms have excellent discriminatory ability. The AUC and the calibration curves also show good accuracy and discriminability.
Conclusion
We have developed new nomograms to predict CSS and OS in elderly patients with localized PC. After internal validation and external temporal validation with reasonable accuracy, reliability and potential clinical value, the model can be used for clinically assisted decision-making.
Similar content being viewed by others
Background
Prostate cancer (PC) is a significant disease that affects men’s health worldwide. It is the second most common form of cancer in men, after non-melanoma skin cancer, such as basal cell carcinoma and squamous cell carcinoma [1]. In 2022, new cases of PC in the United States were expected to reach 268,490, while in 2022, more than 34,500 deaths are expected to occur from PC in the United States, or about 11% of male cancer deaths [2]. PC is a senile disease, and its onset is closely related to age. However, the age of diagnosis has advanced with the popularity of PSA screening, with more than 60% of patients over 65 [3]. More than 80% of these were diagnosed with localized PC [4]. However, older patients were not eligible for enrollment in large randomized trials, and existing guidelines for the management of patients with prostate cancer do not provide specific treatment recommendations for older men [5]. Therefore, it is urgent to provide a clinical treatment basis for elderly patients with localized prostate cancer.
Localized PC refers to a PC with a T stage of T2c and below [6]. According to the current treatment protocol, most patients have a better prognosis. However, PC itself is a highly heterogeneous group of diseases, and patients’ disease progression and prognosis vary greatly. Moreover, the mortality rate of elderly patients is still higher due to comorbidity [7]. Therefore, finding the risk factors for the prognosis and localized PC in old age is essential. Second, current treatment modalities for localized PC include active surveillance, surgical treatment, and radiotherapy [8]. In addition, surgical treatment is considered to be the gold standard for high-risk PC [9]. However, the current choice of treatment modalities for localized PC and whether overtreatment is currently controversial. Therefore, we wanted to construct a predictive model to evaluate further the survival differences in surgical approach and radiotherapy for older patients with localized PC.
Current nomograms developed based on the SEER database have been widely used to predict multiple tumours accurately. Most of the nomograms for PC were concentrated in metastasis patients, especially bone metastasis patients or patients with characteristic GS scores [10,11,12]. However, researchers have yet to develop relevant predictive models for the large group of elderly-limited PCs. Due to comorbidity, its OS cannot respond to cancer-specific deaths from cancer. Therefore, the purpose of this study is to use SEER database data to develop new nomograms to predict independent risk factors related to OS and CSS in elderly localized PC patients and evaluate the survival differences between surgery and radiotherapy to provide auxiliary decision-making for clinicians and patients.
Patients and methods
Data source and data extraction
Information for all patients was extracted from the SEER database, and our target population was patients aged 65 years and older diagnosed with localized PC between 2010 and 2018. The SEER database is a national cancer database containing data from 18 cancer registries, covering approximately 30% of the population. Since the data in the SEER database is publicly available and the patient information is hidden. Ethical approval and patient informed consent was therefore not required. This study followed the research guidelines published in the SEER database.
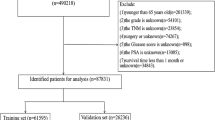
We collected clinicopathological information for all elderly patients with localized PC as well as patient follow-up results, including age, race, year of diagnosis, marital status, histological tumour grade, T stage, surgery, radiotherapy, chemotherapy, PSA, GS, survival status, cause of death, and survival time. According to the official description given in the SEER database, the Grade classification is divided into Grade I: well-differentiated; Grade II: moderately differentiated; Grade III: poorly differentiated; and Grade IV: undifferentiated or anaplastic. The inclusion criteria for this study were: (1) patients aged≥65 years; (2) pathological diagnosis of PC; (3) TNM stage was T1NOMO, T2N0M0. Exclusion criteria: (1) patients younger than 65 years old; (2) tumour grade unknown; (3) T stage above T2 or specific T stage unknown; (4) N1 or N stage unknown; (5) M1 or M stage unknown; (6) unknown surgical method; (7) PSA unknown; (8) GS unknown; (9) survival time less than 1 month or unknown. The flowchart of patient inclusion and exclusion is shown in Fig. 1.
Development and validation of the nomograms
We first randomized the patients into the training set (70%) and the validation set (30%) for nomogram development and internal validation. Furthermore, we performed external temporal validation using data from PC patients from 2016 to 2018. Univariate and multivariate Cox proportional regression models were used to identify independent risk factors that affected patient CSS and OS in the training set. New nomograms were constructed based on multiple Cox regression models and were used to predict the CSS and OS at 3,5 and 8 years, respectively. The accuracy of the nomogram was verified using a calibration curve of 1000 bootstrap samples. The consistency index (c-index) and the area under the subject operating characteristic curve (AUC) were used to test the accuracy and discrimination of the model.
Clinical application
Decision analysis curves (DCA) were used to evaluate the nomogram’s clinical value and compare it with the TNM staging system and the D’Amico risk stratification system. In addition, we also calculated the risk for each patient from the nomogram. All patients were divided into high-risk and low-risk groups based on the cutoff value of the subject’s working characteristic curve (ROC). The Log-rank test and the Kaplan-Meier (K-M) curve examined CSS and OS at 3,5,8 years in high-risk and low-risk patients. In addition, we evaluated the CSS and OS differences in different surgical and radiotherapy methods between patients in the high-risk and low-risk groups.
Statistical analysis
Continuous variables such as age were tested for normal distribution, which can be described by mean and standard deviation, and categorical variables (race, marriage, tumour grade, T stage, surgery, radiotherapy, chemotherapy, PSA, and GS) were described by frequency (%). Chi-square or non-parametric U tests were used for comparison between groups. The Cox regression model analyzed patient prognostic factors, and the log-rank test and K-M curves analyzed patient survival differences. Statistical analysis was performed using R software version 4.1.0 and SPSS26.0.The R package includes “Survival”, “ggDCA”, “DynNom”, and “RMS”.P values less than 0.05 were considered statistically significant.
Results
Clinical features
A total of 90,434 elderly patients diagnosed with localized PC between 2010 and 2018 were included in this study. It was randomly assigned to the training set (n = 63,328) and the validation set (n = 27,106). The mean age of the training set and validation set was 71.4 ± 5.28 years and 71.4 ± 5.33 years, respectively. Our patients were predominantly white according to race (78.3%) and married according to marital status (67.6%). Tumours included grade I (18.97%), grade II (44.73%), grade III (36.27%), and grade IV (0.03%). All the T stages were mainly T1c (60.8%). Patients receiving non-surgical treatment (73.2%), patients undergoing local tumour resection (5.8%), and patients undergoing radical prostatectomy (21.0%). Only 0.2% of the patients received chemotherapy. 34.0% of the patients received Beam radiation, 6.1% received Radioactive implants or isotopes, and 4.4% received Combination radiotherapy, while 55.5% did not. The detection rates of GS 1–6, GS 7 and GS 8–10 were 36.6, 44.5 and 18.8%, respectively. PSA<10 ng/ml(71.9%), 10 ≤ PSA<20 ng/ml(19.4%), PSA ≥ 20 ng/ml(8.7%)。There was no significant statistical bias in the data of both groups, and the results are shown in Table 1.
COX regression analysis
The univariate Cox regression model was first used to analyze and screen for factors associated with patient survival in the training set. The results showed that age, race, marriage, tumour grade, T stage, surgery, chemotherapy, radiotherapy, PSA, and biopsy GS were all factors associated with patient outcome. Then, a multivariate Cox regression model was used to screen for independent risk factors associated with CSS and OS in older patients with PC localized PC. The results showed that age, race, marriage, T stage, surgery, radiotherapy, PSA, and GS were independent risk factors affecting patients’ CSS. In contrast, age, race, marriage, surgery, radiotherapy, PSA, and GS were independent risk factors affecting patients’ OS. Analysis results are shown in Tables 2 and 3, respectively.
Nomogram development for CSS and OS at 3,5 and 8 years
Based on the multivariable Cox regression model, we constructed new nomograms that could predict CSS and OS in elderly localized PC patients at 3,5 and 8 years (Fig. 2). The nomograms showed that surgery and radiotherapy were the most critical factors affecting CSS and OS in elderly patients with localized PC, followed by GS and PSA. In addition, age, marriage, and ethnicity influenced patient CSS and OS.
Validation of the nomograms
Internal cross-validation was used to test the accuracy and identifiability of the model. The c-index of the training and validation sets for the predicted CSS is 0.802(95%CI:0.788–0.816) and 0.798(95%CI:0.776–0.820, respectively). The predicted OS’s c-index of the training and validation sets is 0.712(95%:0.704–0.720) and 0.724(95%:0.714–0.734, respectively). The results show that the nomograms predicting CSS and OS have good discrimination power. The calibration curve shows that in the training and validation sets of the CSS and OS, the predicted values of this model are highly consistent with the actual observed values (Fig. 3). The results show that both CSS and OS nomograms have good accuracy. In the CSS training set, the AUC was 81.4,81.3, and 79.8, respectively, and in the CSS validation set, 80.4,80.3, and 80.7, respectively. In the OS training set, the AUC was 71.9,71.9, and 72.9, respectively, and in the OS validation set, the AUC was 72.1,73.4, and 74.0, respectively. The results showed that the nomogram has a strong discriminability (Fig. 4).
Calibration curve of the nomograms for predicting 3-,5-,8-year CSS and OS in elderly patients with localized prostate cancer. A Calibration curve of the nomograms for predicting CSS in the training set. B Calibration curve of the nomograms for predicting CSS in the validation set. C Calibration curve of the nomograms for predicting OS in the training set. D Calibration curve of the nomograms for predicting OS in the validation set. The horizontal axis is the predicted value in the nomogram, and the vertical axis is the observed value
AUC for predicting 3-, 5-, and 8-year CSS and OS in elderly patients with localized prostate cancer. A The AUC at 3-, 5-, and 8-year for CSS in the training set. B The AUC for CSS in the validation set. C The AUC at 3-, 5- and 8-year for OS in the training set. D The AUC at 3-, 5- and 8-year for OS in the validation set
Furthermore, we performed external temporal validation, which shows that the external validation set C index for predicting CSS is 0.795(95%CI:0.764–0.826), while the external validation set C index for predicting OS is 0.728(95%CI:0.712–0.744). The calibration curve shows that in the external validation set of CSS and OS, the predicted values and the actual observations are highly consistent (Fig. S1). The AUC of the external validation set showed CSS of 79.2,77.3, and 78.1 at 1, 2, and 3 years, respectively, versus 72.5,69.9 and 69.9 at 1,2 and 3-year OS (Fig. S2).
Clinical application of the nomograms
The DCA results showed that our nomogram had good clinical potential value in both CSS and OS training and validation sets (Fig. 5). In the validation set of 3,5, and 8 years, both CSS and OS nomograms showed the best clinical potential value, followed by D’Amico risk stratification and the final T stage. We used the ROC curve to calculate the risk value and the optimal cutoff value for each patient. Patients were then divided into a high-risk group (total score of 180.23) and a low-risk group (total score < 180.23), a high-risk group with predicted OS (total score of 70.84), and a low-risk group (total score < 70.84). The K-M curve showed that CSS and OS rates were higher in low-risk than high-risk groups in both the training and validation set (Fig. 6). CSS rates at 3,5 and 8 years in the low-risk group were 99.7, 99.3, and 98.3%, respectively, while 3,5, and 8-year CSS rates were 97.6, 95.3, and 90.5% in the high-risk group. The 3-year, 5-year and 8-year survival rates were 97.1, 94.0, and 87.5%, respectively, compared with the 3-year, 5-year and 8-year OS rates of 90.5, 81.5, and 65.3% in the high-risk group. We found that in the low-and high-risk groups, patients had the highest rates of CSS and OS for radical prostatectomy, but most patients did not undergo surgery, with the lowest CSS and OS rates for local tumour resection (Fig. 7). However, the survival difference analysis of radiotherapy mode showed that patients in the high-risk group, patients who did not receive radiotherapy, had the lowest CSS and OS rates.
Kaplan-Meier curves of patients in the low-risk and high-risk groups. The K-M curve showed that the CSS rate of the patients in the high-risk group was significantly lower than that in the low-risk group both in the training set (A) and validation set (B). The K-M curve showed that the OS rate of the patients in the high-risk group was significantly lower than that in the low-risk group both in the training set (C) and validation set (D)
Kaplan-Meier curves of patients with surgery. A The CSS rate of patients in the low-risk group underwent different surgery. B The CSS rate of patients in the high-risk group underwent different surgery. C The OS rate of patients in the low-risk group underwent different surgery. D The OS rate of patients in the high-risk group underwent different surgery
In contrast, patients underwent CSS and OS rates with combined radiotherapy and Radioactive implants or isotopes, but both were higher than local irradiation. In the low-risk group, patients who did not receive radiotherapy had the highest CSS and OS rates. In contrast, local irradiation patients had the lowest CSS and OS rates. There was no significant difference in CSS and OS rates between patients combined with radiotherapy and Radioactive implants or isotopes (Fig. 8).
Kaplan-Meier curves of patients with radiotherapy. A The CSS rate of patients in the low-risk group underwent different radiotherapy. B The CSS rate of patients in the high-risk group underwent different radiotherapy. C: The OS rate of patients in the low-risk group underwent different radiotherapy. D The OS rate of patients in the high-risk group underwent different radiotherapy
Discussion
Localized PCs account for more than 80% of elderly patients [4]. However, due to the heterogeneity of the disease, it is imperative to find factors related to its prognosis, and we have a nomogram for predicting CSS and OS based on the SEER database.
The treatment of localized PC mainly focuses on the choice of active monitoring, surgery, and radiotherapy, and it is controversial whether localized PC is overtreated. A randomized controlled trial conducted by Anna Bill-Axelson et al. showed that radical prostatectomy reduced mortality and risk of metastasis in patients with localized PC [13]. Anna Bill-Axelson et al. also demonstrated a significant reduction in mortality after radical prostatectomy after long-term follow-up. In contrast, most long-term survivors in the observation waiting group did not need palliative care [14]. However, one study found that patients with localized PC undergoing local tumour resection were more likely to relapse than those treated with radical resection [15]. Our nomogram showed that surgery is the most critical factor in predicting CSS and OS in elderly patients with localized PC, consistent with previous studies. At the same time, the KM curve for the surgical method showed that the best survival rate could be obtained for all the patients with radical prostatectomy.
In contrast, the patients with local tumour resection had the lowest CSS and OS rates at 3,5 and 8 years, considering that the reason may be that fewer patients with local tumour resection could lead to the resulting bias. Secondly, most patients with localized PC only need active monitoring to obtain a better prognosis, so most patients do not receive surgical treatment. Their survival rate is not lower than that of patients undergoing local tumour resection. Based on this, radical prostatectomy is recommended for elderly patients with localized PC if conditions permit. Secondly, active surveillance is a better option for patients who cannot tolerate surgery.
RT provides treatment for localized PC without major surgery and is the preferred treatment for many men [16]. Nina Samson et al. showed that reduced doses of EBRT appeared to be a viable alternative to ADT in older patients with localized PC [17]. Hiromichi Ishiyama et al. confirmed that combination radiotherapy is a safe and effective treatment for patients with localized PC [18]. While our nomogram also found that radiotherapy was another critical factor in predicting CSS and OS in elderly patients with localized PC, radiotherapy was associated with a better prognosis, consistent with previous studies. However, the KM curve for radiotherapy methods showed that patients in the high-risk group had the highest CSS and OS at 3,5 and 8 years, while patients in the low-risk group had the highest survival rate without receiving radiotherapy. The reason may be that low-risk localized PC patients can obtain a better prognosis through active monitoring.
In contrast, elderly patients cannot tolerate the side effects of radiotherapy due to comorbidities, so receiving radiotherapy leads to a worse prognosis. We do not recommend the routine use of radiotherapy for low-risk elderly patients with localized PC. However, radiotherapy is recommended for elderly patients with a high risk.
Chemotherapy is not the preferred treatment for PC, and previous studies also showed no significant prognostic benefit in PC [19]. The conventional TNM stage is strongly related to PC survival. Frederik B Thomsen et al. also showed a higher T stage, a worse prognosis for PC patients, and a higher risk of metastasis [20]. However, our multivariate COX regression analysis showed that neither T stage nor chemotherapy was an independent risk factor for predicting OS. While chemotherapy is a risk factor but not an independent risk factor for CSS in elderly localized PC patients, the reason may be high non-cancer-specific mortality in elderly patients due to comorbidities. Hence, T-stage and chemotherapy are not independent risk factors affecting OS. Secondly, many elderly patients cannot tolerate the toxic side effects of chemotherapy, which makes the prognosis of patients receiving chemotherapy worse, making chemotherapy have no benefit for CSS. The small number of people who finally received chemotherapy has biased the results. However, the nomogram of CSS showed that the prognostic difference in the T stage was not very significant, considering that the T stage of localized PC patients was limited to the T1 and T2 stages, so the overall prognosis was good.
GS score and PSA level are crucial for the prognosis of PC patients, and our study selected GS grading criteria and PSA grading criteria using the criteria in D’Amico risk stratification [21]. Our nomogram showed that GS and PSA were also independent risk factors for predicting CSS and OS in patients with localized PC and that higher GS and PSA were associated with worse outcomes, consistent with clinical experience [22]. The data showed that 20-year PC patients with 2–6,7 and 8–10 cancer-specific mortality were 10, 4%0 and 70%, respectively [23]; previous nomograms also showed that PSA is a critical factor in PC outcomes [24], consistent with our conclusion.
Age is closely related to the incidence of PC, and our nomogram shows that age is an independent risk factor for CSS and OS in elderly localized PC patients. Most previous prediction models for PC also revealed that age is a risk factor for PC patients, and older patients are associated with a poor prognosis [27]. Secondly, marital status and ethnicity were independent factors affecting CSS and OS in elderly patients with localized PC. Our nomogram shows marriage as a protective factor, consistent with previous studies [28]. Cancer patients receive more financial support and psychological comfort through marriage, and married patients seek treatment more actively out of responsibility to their families [29, 30]. Race is also an independent risk factor for CSS and OS in patients with localized PC. Our nomogram showed that blacks were associated with a worse prognosis, followed by white people and other races, consistent with the conclusions of previous studies [31, 32].
This study explored the risk factors for CSS and OS in elderly patients with localized PC, where we developed nomograms to assist clinicians and patients in assisted decision-making. However, studies based on the SEER database have limitations, starting with the need for more active surveillance and ADT-related data. These two are the preferred measures for treating many PC patients. Active monitoring can achieve a better prognosis, especially for many patients with localized PC. Second, this study was retrospective, and it is challenging to avoid selection bias. Finally, our study lacks critical information such as specific chemotherapy regimen, dose and course of treatment. However, this study still included many key clinicopathological factors and underwent internal and temporal external validation so the results would not be too biased.
Conclusions
We explored the influencing factors of CSS and OS in elderly patients with localized PC, and we found that surgery, radiotherapy, T stage, GS, PSA, age, race, and marriage were independent risk factors for CSS; however, T stage was not an independent risk factor for OS. We developed new nomograms to predict CSS and OS in elderly localized PC patients. With internal and external validation, models showed good accuracy and reliability. DCA showed that our nomogram could guide clinicians and patients to make better decisions due to the T staging and D’Amico risk stratification systems.
Availability of data and materials
The SEER data analyzed in this study is available at https://seer.Cancer.gov/.
References
Nguyen-Nielsen M, Borre M. Diagnostic and therapeutic strategies for prostate Cancer. Semin Nucl Med. 2016;46(6):484–90. https://doi.org/10.1053/j.semnuclmed.2016.07.002.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. https://doi.org/10.3322/caac.21708.
Arnold M, Karim-Kos HE, Coebergh JW, Byrnes G, Antilla A, Ferlay J, Renehan AG, Forman D, Soerjomataram I. Recent trends in incidence of five common cancers in 26 European countries since 1988: analysis of the European Cancer observatory. Eur J Cancer. 2015;51(9):1164–87. https://doi.org/10.1016/j.ejca.2013.09.002.
Meltzer D, Egleston B, Abdalla I. Patterns of prostate cancer treatment by clinical stage and age. Am J Public Health. 2001;91(1):126–8. https://doi.org/10.2105/ajph.91.1.126.
Narita S, Hatakeyama S, Sakamoto S, Kato T, Inokuchi J, Matsui Y, Kitamura H, Nishiyama H, Habuchi T. Management of prostate cancer in older patients. Jpn J Clin Oncol. 2022;52(6):513–25. https://doi.org/10.1093/jjco/hyac016.
Zincke H, Oesterling JE, Blute ML, Bergstralh EJ, Myers RP, Barrett DM. Long-term (15 years) results after radical prostatectomy for clinically localized (stage T2c or lower) prostate cancer. J Urol. 1994;152(5 Pt 2):1850–7. https://doi.org/10.1016/s0022-5347(17)32399-6.
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, Alteri R, Robbins AS, Jemal A. Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin. 2014;64(4):252–71. https://doi.org/10.3322/caac.21235.
Mohan R, Schellhammer PF. Treatment options for localized prostate cancer. Am Fam Physician. 2011;84(4):413–20.
Paladini A, Cochetti G, Felici G, Russo M, Saqer E, Cari L, Bordini S, Mearini E. Complications of extraperitoneal robot-assisted radical prostatectomy in high-risk prostate cancer: a single high-volume center experience. Front Surg. 2023;30(10):1157528. https://doi.org/10.3389/fsurg.2023.1157528.
Wu K, Tang Y, Shao Y, Li X. Nomogram predicting survival to assist decision-making of radical prostatectomy in patients with metastatic prostate cancer. Transl Androl Urol. 2021;10(2):879–87. https://doi.org/10.21037/tau-20-1166.
Miyoshi Y, Noguchi K, Yanagisawa M, Taguri M, Morita S, Ikeda I, Fu**ami K, Miura T, Kobayashi K, Uemura H. Nomogram for overall survival of Japanese patients with bone-metastatic prostate cancer. BMC Cancer. 2015;1(15):338. https://doi.org/10.1186/s12885-015-1330-x.
Qi F, Zhu K, Cheng Y, Hua L, Cheng G. How to pick out the "unreal" Gleason 3 + 3 patients: a nomogram for more precise active surveillance protocol in low-risk prostate Cancer in a Chinese population. J Investig Surg. 2021;34(6):583–9. https://doi.org/10.1080/08941939.2019.1669745.
Bill-Axelson A, Holmberg L, Filén F, Ruutu M, Garmo H, Busch C, Nordling S, Häggman M, Andersson SO, Bratell S, Spångberg A, Palmgren J, Adami HO, Johansson JE. Scandinavian prostate Cancer group study number 4. Radical prostatectomy versus watchful waiting in localized prostate cancer: the Scandinavian prostate cancer group-4 randomized trial. J Natl Cancer Inst. 2008;100(16):1144–54. https://doi.org/10.1093/jnci/djn255.
Bill-Axelson A, Holmberg L, Garmo H, Rider JR, Taari K, Busch C, Nordling S, Häggman M, Andersson SO, Spångberg A, Andrén O, Palmgren J, Steineck G, Adami HO, Johansson JE. Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med. 2014;370(10):932–42. https://doi.org/10.1056/NEJMoa1311593.
Eastham JA, Kattan MW, Fearn P, Fisher G, Berney DM, Oliver T, Foster CS, Møller H, Reuter V, Cuzick J, Scardino P. Transatlantic Prostate Group. Local progression among men with conservatively treated localized prostate cancer: results from the Transatlantic Prostate Group. Eur Urol. 2008;53(2):347–54. https://doi.org/10.1016/j.eururo.2007.05.015.
Holmes JA, Wang AZ, Hoffman KE, Hendrix LH, Rosenman JG, Carpenter WR, Godley PA, Chen RC. Is primary prostate cancer treatment influenced by likelihood of extraprostatic disease? A surveillance, epidemiology and end results patterns of care study. Int J Radiat Oncol Biol Phys. 2012;84(1):88–94. https://doi.org/10.1016/j.ijrobp.2011.10.076.
Samson N, Khanolkar RA, Quirk S, Quon H, Roumeliotis M, Balogh A, Sia M, Thind K, Husain S, Martell K. Clinical outcomes from dose-reduced radiotherapy to the prostate in elderly patients with localized prostate Cancer. Curr Oncol. 2021;28(5):3729–37. https://doi.org/10.3390/curroncol28050318.
Ishiyama H, Kamitani N, Kawamura H, Kato S, Aoki M, Kariya S, Matsumura T, Kaidu M, Yoshida K, Hashimoto Y, Noda Y, Lim KHC, Kawase T, Takahashi T, Inaba K, Kumano M, Yoshikawa N, Yoshioka Y, Nakamura K, Hiratsuka J, Itami J, Hayakawa K. Nationwide multi-institutional retrospective analysis of high-dose-rate brachytherapy combined with external beam radiotherapy for localized prostate cancer: an Asian prostate HDR-BT consortium. Brachytherapy. 2017;16(3):503–10. https://doi.org/10.1016/j.brachy.2017.01.006.
Evans AJ. Treatment effects in prostate cancer. Mod Pathol. 2018;31(S1):S110–21. https://doi.org/10.1038/modpathol.2017.158.
Thomsen FB, Westerberg M, Garmo H, Robinson D, Holmberg L, Ulmert HD, Stattin P. Prediction of metastatic prostate cancer by prostate-specific antigen in combination with T stage and Gleason grade: Nationwide, population-based register study. PLoS One. 2020;15(1):e0228447. https://doi.org/10.1371/journal.pone.0228447.
D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA, Kaplan I, Beard CJ, Wein A. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280(11):969–74. https://doi.org/10.1001/jama.280.11.969.
Swanson GP, Trevathan S, Hammonds KAP, Speights VO, Hermans MR. Gleason score evolution and the effect on prostate Cancer outcomes. Am J Clin Pathol. 2021;155(5):711–7. https://doi.org/10.1093/ajcp/aqaa130.
Cooperberg MR, Konety BR. Management of localized prostate cancer in men over 65 years. Curr Opin Urol. 2009;19(3):309–14. https://doi.org/10.1097/MOU.0b013e328329a303.
Zhu X, Gou X, Zhou M. Nomograms predict survival advantages of Gleason score 3+4 over 4+3 for prostate Cancer: a SEER-based study. Front Oncol. 2019;16(9):646. https://doi.org/10.3389/fonc.2019.00646.
Tang P, Chen H, Uhlman M, Lin YR, Deng XR, Wang B, Yang WJ, **e KJ. A nomogram based on age, prostate-specific antigen level, prostate volume and digital rectal examination for predicting risk of prostate cancer. Asian J Androl. 2013;15(1):129–33. https://doi.org/10.1038/aja.2012.111.
Lee A, Lim J, Gao X, Liu L, Chia SJ. A nomogram for prediction of prostate cancer on multi-core biopsy using age, serum prostate-specific antigen, prostate volume and digital rectal examination in Singapore. Asia Pac J Clin Oncol. 2017;13(5):e348–55. https://doi.org/10.1111/ajco.12596.
Kimura T, Onozawa M, Miyazaki J, Kawai K, Nishiyama H, Hinotsu S, Akaza H. Validation of the prognostic grou** of the seventh edition of the tumor-nodes-metastasis classification using a large-scale prospective cohort study database of prostate cancer treated with primary androgen deprivation therapy. Int J Urol. 2013;20(9):880–8. https://doi.org/10.1111/iju.12064.
Schwartz KL, Alibhai SM, Tomlinson G, Naglie G, Krahn MD. Continued undertreatment of older men with localized prostate cancer. Urology. 2003;62(5):860–5. https://doi.org/10.1016/s0090-4295(03)00690-3.
Copeland LA, Elshaikh MA, Jackson J, Penner LA, Underwood W 3rd. Impact of brachytherapy on regional, racial, marital status, and age-related patterns of definitive treatment for clinically localized prostate carcinoma. Cancer. 2005;104(7):1372–80. https://doi.org/10.1002/cncr.21341.
Knipper S, Preisser F, Mazzone E, Mistretta FA, Palumbo C, Tian Z, Briganti A, Shariat SF, Saad F, Tilki D, Graefen M, Karakiewicz PI. Contemporary analysis of the effect of marital status on survival of prostate cancer patients across all stages: a population-based study. Urol Oncol. 2019;37(10):702–10. https://doi.org/10.1016/j.urolonc.2019.04.023.
Siegel DA, O'Neil ME, Richards TB, Dowling NF, Weir HK. Prostate Cancer incidence and survival, by stage and race/ethnicity - United States, 2001-2017. MMWR Morb Mortal Wkly Rep. 2020;69(41):1473–80. https://doi.org/10.15585/mmwr.mm6941a1.
Thorpe RJ Jr, Bruce MA, Howard DL, LaVeist TA. Race differences in mobility status among prostate cancer survivors: the role of socioeconomic status. Adv Cancer Res. 2020;146:103–14. https://doi.org/10.1016/bs.acr.2020.01.006.
Acknowledgements
Not applicable.
Methods
The methods used in this study comply with the regulations and guidelines of the SEER database.
Funding
This study was supported by Yunnan Education Department of Science Research Fund (No. 2020 J0228, 2023 J0295), Kunming City Health Science and Technology Talent “1000” training Project (No. 2020- SW (R)-112), Kunming Health and Health Commission Health Research Project (No. 2020–0201-001), Open Research Fund of Clinical Research Center for Children’s Health and Diseases of Yunnan Province (No.2022-ETYY-YJ-03), Department of Science and Technology of Yunnan Province Kunming Medicine Joint Special Program-General Program (No. 202001AY070001-271, 202301AY070001-108), and Kunming Health Personnel Training Project Technology Center Construction Project (No. 2020-SW (T) -15). The funding bodies played no role in the study’s design and collection, analysis and interpretation of data, and writing the manuscript.
Author information
Authors and Affiliations
Contributions
CHZH designed the study; CHZH, JKW, LL, YCX, FMJ and HYT collected and analyzed the data; CHZH drafted the initial manuscript; CHZH, JJZ, YL, JM, ZY and BY revised the article critically; CHZH, JJZ, YL, ZGY and CCW reviewed and edited the article. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The data of this study is obtained from the SEER database. The patients’ data is public and anonymous, so this study does not require ethical approval and informed consent.
Consent for publication
None.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Calibration curve in the external verification of CSS and OS in elderly patients with localized prostate cancer. Figure S2. The AUC in the external verification of CSS and OS in elderly patients with localized prostate cancer.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhanghuang, C., Zhu, J., Li, Y. et al. Prognostic significance of surgery and radiotherapy in elderly patients with localized prostate cancer: establishing and time-based external validation a nomogram from SEER-based study. BMC Urol 24, 12 (2024). https://doi.org/10.1186/s12894-023-01384-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-023-01384-6