Abstract
Background
To identify the malignant potential and prognostic indicators of renal epithelioid angiomyolipoma (eAML), clinicopathological and molecular features as well as the drug efficacy of 67 eAML cases were analyzed.
Materials and methods
Sixty-seven renal eAML patients were enrolled and the immunohistochemical features of these patients were examined. FFPE slides of all patients were re-examined. 21 patients with metastasis received Everolimus 10 mg orally once daily. Responses were evaluated with RECIST criteria by three authors. A risk stratification model was constructed using the following factors: pT3 and pT4, presence of necrosis, mitotic count ≥ 2; the presence of atypical mitoses; severe nuclear atypia, SMA negative, Ki-67 ≥ 10%.
Results
The average percentage of the epithelioid component was 85.6% (range 80–95%). Immunohistochemically, Ki-67 ≥ 10% and negative SMA staining were significantly correlated with malignant characteristics (Ki-67: p < 0.001; SMA: p = 0.001). Survival analysis suggested that pT3-pT4 stage, presence of necrosis, severe nuclear atypia, presence of atypical mitoses, mitotic count ≥ 2, Ki-67 ≥ 10% and negative SMA expression were significantly associated with poorer PFS and OS (p < 0.05). The risk model sufficiently discriminated recurrence/metastasis (AUC = 0.897) and cancer-specific mortality (AUC = 0.932) of renal eAML patients in different risk groups. 21 patients had received Everolimus targeted therapy after recurrence/metastasis. The best response for Everolimus treatment was 8/21 (38.1%) partial responses (PR), 9/21 (42.9%) stable disease (SD) and 4/21 (19.0%) progressive disease (PD).
Conclusion
The risk stratification model could well distinguish eAML patients at high risk of recurrence/metastasis. Everolimus targeted treatment showed good efficacy in patients with recurrence/metastasis.
Similar content being viewed by others
Introduction
Renal angiomyolipoma (AML) is a relatively rare mesenchymal neoplasm. According to the World Health Organization (WHO) tumor classification, there are two types of renal AML: classic AML and epithelioid AML. Renal epithelioid angiomyolipoma (eAML) is a potentially malignant variant of renal AML [1, 2], accounting for less than 1% of all renal neoplasm [3] and approximately 7.7% of renal AML cases [4]. Unlike classic renal AML, which is composed of various proportions of dysmorphic blood vessels, smooth muscle components, and fat cells, renal eAML consists of at least 80% of epithelioid cells as well [5]. Tumor cells can be polygonal with varying degrees of nuclear atypia, round to oval nuclei, atypical mitoses, and transparent to eosinophilic cytoplasm [6]. Immunohistochemically, typical renal eAML is positive for Human Melanoma Black (HMB-45), MART-1/Melan-A, smooth muscle actin (SMA) and muscle-specific actin myoid markers [7]. Although classic renal AML is considered to be a benign mesenchymal tumor, several studies have demonstrated that renal eAML exhibits aggressive clinical characteristics such as local recurrence and distant metastasis [6, 6,8,9,10,11]. Therefore, renal eAML can be an atypical variant of renal AML or a distinct malignant tumor element [6, 12].
Nevertheless, because of the rarity of renal eAML, there is insufficient data to clarify its clinicopathological characteristics and pathological prognostic predictors. Several case reports and small series studies have investigated renal eAML 13,14,15], but our understanding of the features and prognosis of renal eAML remain limited. Brimo et al. established a predictive model of renal eAML and reported that four atypical features of renal eAML could accurately categorize 78% of renal eAML cases with malignant characteristics in their series [16]. Subsequently, Nese et al. analyzed 41 cases of pure renal eAML and published risk factors for disease progression. They identified five adverse prognostic parameters and stratified patients into three risk categories [17]. However, the clinicopathological features and risk factors that can predict the prognosis of renal eAML patients need further investigation and validation.
To clarify the clinicopathological characteristics and immunohistochemical (IHC) features of renal eAML and investigate the potential prognostic predictors of renal eAML, we analyzed the clinicopathological data and IHC indexes of a large series of renal eAML cases. Although there are some recognized risk factors for predicting the potential malignancy of renal eAML, for more comprehensive analyses, we attempted to establish a prognostic model to distinguish patients at risk of recurrence or metastasis. Our findings may help identify the malignant potential of renal eAML and its prognostic indicators.
Methods and materials
Patients
This study was a retrospective cohort study of 67 renal eAML patients, which were diagnosed from June 2013 to December 2019 at the Department of Urology. According to the WHO definition, all eAML cases enrolled in our cohort consisted of at least 80% of epithelioid cells. The number of cases during the study period determined the sample size. Among them, 4 patients were diagnosed as distant metastasis at the time of diagnosis, so they were excluded from the training cohort but still included in the analysis of treatment response. The study was approved by the institutional review board of our insitution. All cases were independently re-reviewed by two experienced genitourinary pathologists toexclude the misdiagnosed cases and maintain consistency of pathological parameters.
Clinicopathological data
The clinicopathological parameters of all patients were obtained from electronic medical records or by re-assessed the slides. Tumor size was recorded using the largest tumor diameter. The stage was assessed by combining the clinical and pathological TNM staging according to the American Joint Committee on Cancer (AJCC) TNM staging, 8th edition, 2017. Tumor necrosis was defined as microscopic coagulative necrosis. Epithelioid cells were defined as polygonal cells with clear to deeply eosinophilic cytoplasm, vesicular nuclei, and prominent nucleoli. The degree of nuclear atypia was graded as mild, moderate, or severe. Mild nuclear atypia: Conspicuous nucleoli, nuclear membrane irregularities, and slight variation in nuclear size. Moderate nuclear atypia: Cells are intermediate in size and show enlarged nuclei with moderate pleomorphism and prominent nucleoli. Severe nuclear atypia: Cells are large with abundant eosinophilic cytoplasm, extensive nuclear pleomorphism, and prominent nucleoli [16].The percentage of epithelioid cells and the degree of nuclear atypia were estimated visually in relation to the total tumor areas in the available slides. Atypical mitoses and multinucleated giant cells were assessed in 10 high-power fields (HPFs).
Immunohistochemical evaluation
All the slides were sectioned using the primary tumor tissue. The IHC profiles of 57 renal eAML patients were assessed using a broad panel of targets: HMB-45, Melan-A, SMA, PNL-2, desmin, CD34, AE1/AE3, CK7, vimentin, TFE3-OPT, PAX8, CD10, S-100, and Ki-67. Positive or negative staining of a target on one FFPE slide and all haematoxylin and eosin (H&E)-stained slides were independently assessed by two experienced genitourinary pathologists. The immunohistochemistry (IHC) staining degree score was graded from 0 to 4, based on the coverage percentage of tumor cells (0%, 1–25%, 26–50%, 51–75%, 76–100%). Staining intensity degrees was ranging from 0 to 3, representing samples with no staining, weak, median and strong, respectively. The overall IHC score (from 0 to 12) was calculated according to the multiply of staining degree score and staining intensity, and 0–2 was defined as negative staining and 3–12 as positive staining.
Survival assessment
The primary endpoint was overall survival (OS), which was assessed from the date of surgical treatment or needle biopsy to the date of death or last follow-up. Progression-free survival (PFS) was the secondary endpoint and was defined as the length of time from the date of surgery or needle biopsy to the date of progression, second-line treatment, or death, whichever occurred first. Survival curves were established using the Kaplan–Meier method and analyzed by the log-rank test with 95% confidence intervals (95% CIs). To identify independent predictors, hazard ratio (HR) estimates and 95% CIs were calculated using univariate and multivariate Cox logistic regression models.
Treatment
According to patients’ tolerance, 21 patients have treated with Everolimus 10 mg orally once daily with continues until disease progression, the occurrence of unacceptable toxicity, or death. The inclusion criteria for patients treated with Everolimus are as follows: (1) Age ≥ 18 years; (2) Patients had a histological or cytological diagnosis of at least one metastatic site; (3) patients had a radiologically measurable metastatic disease; 4. Receiving Everolimus as first-line treatment. Dose modification or discontinuation was administered according to the patients’ tolerance. Responses were evaluated with Response Evaluation Criteria In Solid Tumors (RECIST) by three authors. Timing of assessments is at the discretion of the treating physician, usually once every 3 months. Follow-up information was obtained during clinical visits or by telephone.
Statistical analysis
To maximize the statistical analysis and minimize any bias caused by the missing data, multiple imputation with chained equations was performed using R language to assign missing values.
Correlations between the clinicopathological and IHC parameters of the experimental groups were determined by chi-squared test and independent sample t-test. Continuous variables were reported as means ± SD; categorical variables were reported as the number and percentage of the total population. Evaluations were based on point estimates and 95% CIs. All hypothetical tests were two-sided and p-values less than 0.05 were considered significant in all tests.
Results
Clinicopathological characteristics
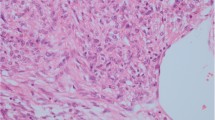
Sixty-seven renal eAML patients from our institution were analyzed. The clinicopathological characteristics of patients were shown in Table 1. Over the entire duration of follow-up (median follow-up, 49.5 months, range 8.9–102.5 months), 46 renal eAML patients had no recurrence/metastasis (73.0%) and 17 cases had recurrence/metastasis (27.0%).. The mean age of the study cohort was 40.8 ± 13.7 years and there were 31 men (49.2%) and 32 women (50.8%). The tumor size of recurrence/metastasis cases was significantly larger than that of no recurrence/metastasis patients (6.2 ± 3.5 vs. 11.4 ± 4.9, p < 0.001). In addition, patients with recurrence/metastasis were significantly correlated with advanced T (p = 0.003) stages. Fifteen cases presented necrosis (Fig. 1A), and the presence of tumor necrosis was significant in the recurrence/metastasis group (7/17, 41.2%) compared with the no recurrence/metastasis group (8/46, 17.4%) (p = 0.049). Moreover, four cases presented perinephric fat invasion and one case showed microvascular invasion. Three cases were associated with multiple tumors: a single eAML tumor on the left kidney coexisting with a single eAML tumor on the right lobe of the liver in one case; multiple eAML tumors on the right kidney in one case; and a single eAML tumor on both kidneys in one case.
Histopathological features of renal eAML. Haematoxylin and eosin staining. A The arrowhead indicates the necrosis in a renal eAML sample. Magnification 100 × . B In renal eAML cases, tumors were composed of epithelioid endothelial cells. The arrowhead indicates hyaline degeneration of the vascular wall. Magnification 100 × . As shown by Arrowhead, compared with cells displaying mild nuclear atypia C, cells with severe nuclear atypia (D) are characterized by their larger size, abundant eosinophilic cytoplasm, and nuclear polymorphism. Magnification 400 × . E Renal eAML also displayed atypical mitotic figures (arrows). The higher atypical mitotic figure may associate with malignant behaviors. Magnification 400 × . F Arrowhead indicates the Multinucleated giant cell. Magnification 200 ×
The average percentage of the epithelioid component was 85.6% (range 80–95%) (Fig. 1B). A total of 22.2% (14/63) cases revealed mild nuclear atypia, while 63.5% (40/63) exhibited moderate nuclear atypia and 14.3% (9/63) showed severe nuclear atypia. Importantly, elevated nuclear atypia was significantly correlated with malignancy (p = 0.005). Compared with cells displaying mild and moderate nuclear atypia, cells with severe nuclear atypia were characterized by their larger size and abundant eosinophilic cytoplasm, and nuclear polymorphism (Fig. 1C, D). Moreover, the mitotic count was 0–2 per 10 HPFs in the no recurrence/metastasis cohort, with an average mitotic count of 0.7, and 1–7 per 10 HPFs in the recurrence/metastasis cohort, with an average mitotic count of 3.6 (p < 0.001). In addition, 25.4% (16/63) cases displayed atypical mitotic figures (Fig. 1E), and the presence of atypical mitoses was significantly related to malignant behavior (p < 0.001). Multinucleated giant cells were observed in 46.0% (29/63) of cases (Fig. 1F), but the presence of multinucleated giant cells was not significantly correlated with malignancy (p = 0.071).
Immunohistochemical features
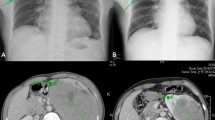
The IHC staining was available for 57 renal eAML patients in the study cohort. All the cases exhibited positive staining of at least one melanocytic marker (HMB-45 or Melan-A). Negative SMA staining (IHC score 0–2) was significantly correlated with tumor recurrence/metastasis (p = 0.001), and the malignant cases displayed weak staining of SMA compared with cases with good outcomes. (Fig. 2A–D). In addition, patients with Ki-67 ≥ 10% were also significantly associated with recurrence/metastasis (p < 0.001), and malignant cases tended to show strong nuclear staining of Ki-67 relative to the cases with favorable prognoses (Fig. 2E–H). The chi-squared test revealed that other indexes were balanced in the distribution of categorical data, including HMB-45, Melan-A, PNL-2, desmin, CD34, AE1/AE3, CK7, vimentin, TFE3-OPT, PAX8, CD10, and S-100, as shown in Table 2.
Immunohistochemical features of renal eAML. Immunoperoxidase staining. The overall immunohistochemistry (IHC) score of 0–3 was defined as negative staining and 4–12 as positive staining. A, B Metastatic renal eAML with negative SMA staining. C, D Non-metastatic renal eAML with diffuse positive SMA staining. E, F Non-metastatic renal eAML with less than 10% of cells showing nuclear staining with Ki-67. G, H Malignant renal eAML shows strong nuclear staining with Ki-67
Prognostic factors for PFS and OS
The median PFS and OS of the total cohort were not reached during the follow-up period (Additional file 1: Fig. S1A, B). Patients with tumor size > 7 cm were significantly correlated with shorter PFS (p = 0.0061), but not significantly correlated with OS (p = 0.053) (Additional file 1: Fig. S1C, D). Besides, patients with pT3-pT4 also significantly correlated with poor PFS (p = 0.0044) and OS (p = 0.0022) (Additional file 1: Fig. S1E, F). In addition, presence of atypical mitoses (PFS: p < 0.0001, OS: p = 0.0085), presence of necrosis (PFS: p = 0.0428, OS: p = 0.0293), severe nuclear atypia (PFS: p < 0.0001, OS: p < 0.0001) and mitotic count > = 2 (PFS: p < 0.0001, OS: p = 0.0174) were significantly correlated with both shorter PFS and OS (Additional file 1: Fig. S3G-N). Survival curves also demonstrated that patients with Ki-67 ≥ 10% were significantly correlated with poorer PFS (HR = 13.38, p < 0.0001) and OS (HR = 15.15, p = 0.0005) (Additional file 1: Fig. S1O, P). Besides, the survival analysis also indicated that patients with negative SMA staining (IHC score 0–2) had shorter PFS (HR = 4.59, p = 0.0002) and shorter OS (HR = 16.96, p < 0.0001) (Additional file 1: Fig. S1Q, R).
Univariate and multivariate Cox regression analyses were performed on 57 eAML patients from the our insititution. The median follow-up was 49.5 months (range 8.9–102.5 months), and during the entire follow-up duration, 16 patients exhibited desease progression and seven patients died. As shown in Fig. 3A–D, in univariate Cox regression analysis, traditional prognostic factors, especially the pT stage were significantly correlated with PFS (p < 0.0001) and OS (p = 0.0084), but the pN stage was only significant for PFS (p = 0.0100). In addition, mitotic count (PFS: p < 0.0001; OS: p = 0.0161), atypical mitoses (PFS: p < 0.0001; OS: p = 0.0059), nuclear atypia (PFS: p = 0.0009; OS: p = 0.0007) were also significantly correlated with poor PFS and OS. Tumor size (p < 0.001) and necrosis were only significant for PFS. Importantly, SMA and Ki-67 were markedly associated with poor PFS (SMA: p = 0.0006; Ki-67: p < 0.0001) and OS (SMA: p = 0.0002; Ki-67: p = 0.0098). In the multivariate Cox regression analysis, pT stage (p = 0.042), necrosis (p = 0.027), mitotic count (p = 0.004) and Ki-67 (p = 0.013) were significantly correlated with poor PFS, and nuclear atypia (p = 0.028) and SMA (p = 0.045) were significantly correlated with OS.
Univariate and multivariate Cox regression analysis. Univariate Cox regression analysis showed that tumor size (p < 0.0001), pT stage (p < 0.0001), pN stage (p = 0.0100), mitotic count (p < 0.0001), atypical mitoses (p < 0.0001), nuclear atypia (p = 0.0009), SMA expression (p = 0.0006) and percentage of Ki-67 (p < 0.0001) were significantly correlated with PFS (A), and pT stage (p = 0.0084), mitotic count (p = 0.0161), atypical mitoses (p = 0.0059), nuclear atypia (p = 0.0007), SMA expression (p = 0.0002) and percentage of Ki-67 (p = 0.0098) were significantly correlated with OS (C). In multivariate Cox regression analysis, pT stage (p = 0.0419), necrosis (p = 0.0273), mitotic count (p = 0.0037) and percentage of Ki-67 (p = 0.0127) were still significantly correlated with PFS (B), and nuclear atypia (p = 0.0283), SMA expression (p = 0.0449) were significantly correlated with OS (D)
Construction of prognostic prediction model
We selected significant indicators to establish a prognostic prediction model of renal eAML. After assessment of the prognostic markers of renal eAML, pT3-pT4, presence of necrosis, mitotic count ≥ 2; presence of atypical mitoses; severe nuclear atypia, SMA negative, Ki-67 ≥ 10% were considered to be risk factors for desease progression of renal eAML. Patients who had 0–1 risk factor were included in the low-risk group, patients with 2–3 of the risk factors were included in the intermediate-risk group, and patients with 4–7 risk factors were included in the high-risk group (Additional file 2: Table S1). Survival curves also indicated that the PFS and OS of the three prognostic groups differed significantly (p < 0.0001). The median PFS and OS of the low and intermediate-risk groups were not reached, which were much better than the high-risk group (median PFS:18.3; median OS: 61.9) (Fig. 4A, B). Overall, the stratification model sufficiently discriminated recurrence/metastasis (AUC = 0.897) and cancer-specific mortality (AUC = 0.932) of renal eAML patients in different risk groups. (Fig. 4C, D).
Construction of FUSCC cohort and drug efficacy. Patients in high risk group shows both poor PFS (A) and OS (B) than patients in low and intermediate risk group (p < 0.0001). C, D ROC curves indicates that the FUSCC model has high sensitivity and specificity to predict the recurrence/metastasis risk (AUC = 0.897) and cancer specific mortality (AUC = 0.932) of renal eAML patients. E The waterfall plot shows the best efficacy and reduction of the target lesion after Everolimus targeted treatment in 21 renal eAML patients with recurrence/metastasis, of which, the best response for Everolimus targeted treatment was 8/21 (38.1%) PR, 9/21 (42.9%) SD and 4/21 (19.0%) PD. F The representative imaging figures from one PR case (left: baseline CT imaging; right: 6 months after treatment) and one case of SD (right: baseline MRI imaging; right: 4 months after treatment
Treatment
In the recurrence/metastasis group, four (6.0%) cases had confirmed distant metastasis through preoperative systemic imaging and confirmed by biopsy of the primary tumor at the time of diagnosis. Partial nephrectomy was performed in 27 (42.9%) cases and radical nephrectomy in 36 (57.1%) cases. Among patients undergoing protocol surgery, recurrence/metastasis occurred in 17 (27.0%) patients in the follow-up period with a mean time to recurrence/metastasis of 22.2 months. Imaging examination and puncture biopsy confirmed that the most frequent metastatic site was lung 12 (57.1%), as well as 8 (38.1%) cases with recurrence. All patients who occurred recurrence/metastasis during follow-up period (N = 17), as well as patients who ouccered metastasis at the time of initial diagnosis (N = 4) had received Everolimus (10 mg qd) targeted therapy. Based on radiology review, the best response for Everolimus treatment was 8/21 (38.1%) partial responses (PR), 9/21 (42.9%) stable disease (SD) and 4/21 (19.0%) progressive disease (PD) (Fig. 4E). Figure 4F is the representative imaging figures from one case of PR and one case of SD. Four PD cases were switched to second-line targeted therapy, of which two patients were treated with Axitinib, one patient was treated with Pazopanib, and one patient was treated with Sorafenib. One patient who received nephron sparing surgery had an operation area recurrence that was treated successfully with radical nephrectomy after partial response to Everolimus targeted therapy. One patient with lung metastasis received wedge resection of pulmonary metastasis after partial response. One patient received abdominal wall metastatic site resection after partial response to Everolimus targeted therapy. Treatment details were summarized in Table 3.
Discussion
To clarify the potential malignancy of eAML and investigate prognostic predictors for this disease, we studied the pathological characteristics and clinical outcomes of 67 eAML patients. More importantly, we established a risk model for eAML patients and accurately predicted the recurrence/metastasis risk. Our model provides a novel approach for the diagnosis and early intervention of eAML, a potentially malignant disease.
Renal eAML was once considered a hamartoma [18]. However, in subsequent years, several studies reported the malignant behavior of renal eAML, including local recurrence, distant metastasis, and death from the disease, as described in small case reports 19,20,21]. Nevertheless, because of the rarity of renal eAML cases, the clinicopathological characteristics, diagnosis, and clinical outcomes should be further investigated for better treatment. To evaluate the potential malignancy of this rare disease, Brimo et al. studied a series of 40 renal eAML cases and demonstrated that the presence of at least 70% atypical epithelioid cells, a mitotic count of ≥ 2 per 10 HPFs, atypical mitotic figures, and necrosis were prognostic factors for renal eAML [16]. Nese et al. also performed a similar study of 41 renal eAML cases and indicated that necrosis, tuberous sclerosis complex and/or concurrent AML, carcinoma-like growth, extrarenal extension and/or the involvement of the renal vein, and tumor size > 7 cm were prognostic factors for renal eAML [17]. In previous studies, many predictors of poor clinical outcomes were investigated but not unified.
Studies have shown that eAML is a potentially malignant neoplasm, with approximately 30% of cases exhibiting distant metastasis to lymph nodes, liver, lungs, and spine [22]. Similarly, there were 17 (25.6%) patients with metastasis in our cohort. Notably, Antonio et al. first reported a case of primary eAML of the adrenal gland in patients without evidence of tuberous sclerosis [23]. Therefore, because of its similarity upon imaging, eAML is easily misdiagnosed as renal cell carcinoma or sarcoma [24]. Furthermore, abnormal blood vessels and mature adipocytes are not obvious in eAML, and thus it is difficult to diagnose eAML using radiographic devices [25]. Hence, the diagnosis of eAML should be mainly based on the different proportions of epithelioid components as well as positive staining of HMB-45 or Melan-A. In our eAML study cohort, all patients were diagnosed with the pathological characteristics described above, and 57 of these patients were examined to investigate the potential value of IHC indexes.
Ki-67 was first identified as an antigen by Gerdes et al. in Hodgkin lymphoma cell nuclei [26]. Previous studies based on cell cycle analyses have illustrated that among the identified cell cycle markers, only Ki-67 is downregulated in the quiescent G0 phase while being highly expressed in the G1, S, and G2 phases [27]. In recent years, similar investigations have been undertaken in renal eAML, but the results were inconclusive. Ooi et al. demonstrated that Ki-67 was strongly positive in two eAML cases but negative in four classic AMLs [28]. Moreover, Xu et al. evaluated the use of Ki-67 as a prognostic predictor in six eAML patients and found that patients with positive expression of Ki-67 had a poorer prognosis [29]. Conversely, no significant difference in Ki-67 was identified between classic AML and eAML cases [30]. However, all these studies were based on small sample sizes, and hence it is necessary to further verify the role of Ki-67 as a prognostic indicator in eAML patients.
The advantage of our study is that we systemically analyzed clinicopathological and IHC features and clinical outcomes in an unprecedented number of renal eAML cases. Through this, we demonstrated that renal eAML patients with malignancy exhibited larger tumor size, advanced T/N stage, and necrosis. Immunohistochemically, we also revealed that negative SMA expression and Ki-67 ≥ 10% were significantly correlated with malignancy. Based on these features, we attempted to investigate the prognostic factors of renal eAML patients and found that Ki-67 ≥ 10% and negative SMA expression were correlated with poor PFS and OS in eAML patients. Next, we established a risk model for renal eAML, which incorporated the most common, representative and accurate pathological parameters as risk factors.
This study has some limitations. First, due to the nature of the retrospective study and the missing data of some patients, we cannot but accept all the biases of our study. Second, our study did not examine the underlying mechanism of Ki-67 and SMA in the tumor metabolism of renal eAML. Third, our risk model should be verified in other renal eAML cases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
**zaki M, Silverman SG, Akita H, et al. Diagnosis of renal angiomyolipomas: classic, fat-poor, and epithelioid types. Semin Ultrasound CT MR. 2017;38(1):37–46.
Lopez-Beltran A, Scarpelli M, Montironi R, et al. 2004 WHO classification of the renal tumors of the adults. Eur Urol. 2006;49(5):798–805.
Faraji H, Nguyen BN, Mai KT. Renal epithelioid angiomyolipoma: a study of six cases and a meta-analytic study: development of criteria for screening the entity with prognostic significance. Histopathology. 2009;55(5):525–34.
Aydin H, Magi-Galluzzi C, Lane BR, et al. Renal angiomyolipoma: clinicopathologic study of 194 cases with emphasis on the epithelioid histology and tuberous sclerosis association. Am J Surg Pathol. 2009;33(2):289–97.
Moch H, Cubilla AL, Humphrey PA, et al. The 2016 WHO classification of tumours of the urinary system and male genital organs-part a: renal, penile, and testicular tumours. Eur Urol. 2016;70(1):93–105.
Mete O, van der Kwast TH. Epithelioid angiomyolipoma: a morphologically distinct variant that mimics a variety of intra-abdominal neoplasms. Arch Pathol Lab Med. 2011;135(5):665–70.
Armah HB, Parwani AV. Perivascular epithelioid cell tumor. Arch Pathol Lab Med. 2009;133(4):648–54.
He W, Cheville JC, Sadow PM, et al. Epithelioid angiomyolipoma of the kidney: pathological features and clinical outcome in a series of consecutively resected tumors. Modern Pathol Off J USA Can Acad Pathol. 2013;26(10):1355–64.
Pea M, Bonetti F, Martignoni G, et al. Apparent renal cell carcinomas in tuberous sclerosis are heterogeneous: the identification of malignant epithelioid angiomyolipoma. Am J Surg Pathol. 1998;22(2):180–7.
Martignoni G, Pea M, Rigaud G, et al. Renal angiomyolipoma with epithelioid sarcomatous transformation and metastases: demonstration of the same genetic defects in the primary and metastatic lesions. Am J Surg Pathol. 2000;24(6):889–94.
Svec A, Velenská Z. Renal epithelioid angiomyolipoma—a close mimic of renal cell carcinoma: report of a case and review of the literature. Pathol Res Pract. 2005;200:851–6.
Lei JH, Liu LR, Wei Q, et al. A four-year follow-up study of renal epithelioid angiomyolipoma: a multi-center experience and literature review. Sci Rep. 2015;5:10030.
Gamé X, Soulié M, Moussouni S, et al. Renal angiomyolipoma associated with rapid enlargement [correction of enlargment] and inferior vena caval tumor thrombus. J Urol. 2003;170(3):918–9.
Yamamoto T, Ito K, Suzuki K, et al. Rapidly progressive malignant epithelioid angiomyolipoma of the kidney. J Urol. 2002;168(1):190–1.
Inoue C, Saito R, Nakanishi W, et al. Renal epithelioid angiomyolipoma undergoing aggressive clinical outcome: the MDM2 expression in tumor cells of two cases. Tohoku J Exp Med. 2019;247(2):119–27.
Brimo F, Robinson B, Guo C, et al. Renal epithelioid angiomyolipoma with atypia: a series of 40 cases with emphasis on clinicopathologic prognostic indicators of malignancy. Am J Surg Pathol. 2010;34(5):715–22.
Nese N, Martignoni G, Fletcher CD, et al. Pure epithelioid PEComas (so-called epithelioid angiomyolipoma) of the kidney: A clinicopathologic study of 41 cases: detailed assessment of morphology and risk stratification. Am J Surg Pathol. 2011;35(2):161–76.
Musella A, De Felice F, Kyriacou AK, et al. Perivascular epithelioid cell neoplasm (PEComa) of the uterus: a systematic review. Int J Surg (Lond, Engl). 2015;19:1–5.
Zheng S, Bi XG, Song QK, et al. A suggestion for pathological grossing and reporting based on prognostic indicators of malignancies from a pooled analysis of renal epithelioid angiomyolipoma. Int Urol Nephrol. 2015;47(10):1643–51.
Yang L, Feng XL, Shen S, et al. Clinicopathological analysis of 156 patients with angiomyolipoma originating from different organs. Oncol Lett. 2012;3(3):586–90.
Cho NH, Shim HS, Choi YD, et al. Estrogen receptor is significantly associated with the epithelioid variants of renal angiomyolipoma: a clinicopathological and immunohistochemical study of 67 cases. Pathol Int. 2004;54(7):510–5.
Luo D, Gou J, Yang L, et al. Epithelioid angiomyolipoma with involvement of inferior vena cava as a tumor thrombus: a case report. Kaohsiung J Med Sci. 2011;27(2):72–5.
D’Antonio A, Caleo A, Caleo O, et al. Monotypic epithelioid angiomyolipoma of the adrenal gland: an unusual site for a rare extrarenal tumor. Ann Diagn Pathol. 2009;13(5):347–50.
**zaki M, Tanimoto A, Narimatsu Y, et al. Angiomyolipoma: imaging findings in lesions with minimal fat. Radiology. 1997;205(2):497–502.
Adanur S, Keskin E, Ziypak T, et al. Renal epithelioid angiomyolipoma mimicking urothelial carcinoma of the upper urinary tract. Archivio italiano di urologia, andrologia : organo ufficiale [di] Societa italiana di ecografia urologica e nefrologica. 2014;86(3):235–6.
Gerdes J, Schwab U, Lemke H, et al. Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int J Cancer. 1983;31(1):13–20.
Urruticoechea A, Smith IE, Dowsett M. Proliferation marker Ki-67 in early breast cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2005;23(28):7212–20.
Ooi SM, Vivian JB, Cohen RJ. The use of the Ki-67 marker in the pathological diagnosis of the epithelioid variant of renal angiomyolipoma. Int Urol Nephrol. 2009;41(3):559–65.
Xu C, Jiang XZ, Zhao HF, et al. The applicability of Ki-67 marker for renal epithelioid angiomyolipoma: experience of ten cases from a single center. Neoplasma. 2013;60(2):209–14.
Li W, Guo L, Bi X, et al. Immunohistochemistry of p53 and Ki-67 and p53 mutation analysis in renal epithelioid angiomyolipoma. Int J Clin Exp Pathol. 2015;8(8):9446–51.
Acknowledgements
We thank H. Nikki March, Ph.D., from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (Nos. 81772706, 81802525, and 821172817) and the National Key Research and Development Program of China Project (no. 2019YFC1316005).
Author information
Authors and Affiliations
Contributions
AA: protocol/project development; data collection or management; data analysis; manuscript writing/editing. WHX: protocol/project development; data analysis; manuscript writing/editing. XT: data analysis; manuscript writing/editing. TD: protocol/project development; data analysis; manuscript writing/editing. JQS: data collection or management; manuscript writing/editing. YW: data analysis; manuscript writing/editing. YYQ: protocol/project development; data collection or management; manuscript writing/editing. HLZ: protocol/project development; data analysis; manuscript writing/editing. DWY: protocol/project development; data analysis; manuscript writing/editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All of the study designs and test procedures were performed in accordance with the Helsinki Declaration II. The Ethics approval and participation consent of this study was approved and agreed by the ethics committee of Fudan University Shanghai Cancer Center (Ethical IRB number:050432-4-1911D). All patients participating in this study signed informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Supplementary Figure 1.
Correlation between clinical parameters and prognosis. Survival curves indicated the PFS (A) and OS (B) of total cohort. Patients with tumour size>7cm were significantly correlated with PFS (C) (HR=4.47, p=0.0061), but not significant in OS (D) (HR=4.61, p=0.053). Patients with pT3-pT4 stage were correlated with both shorter PFS (E) (HR=3.74, p=0.0044) and OS (F) (HR=10.27, p=0.0022). Patients with presence of atypical mitosis (G, H), presence of necrosis (I, J), severe nuclear atypia (K, L), and mitotic count >=2 (M, N) were significantly correlated with poor PFS (presence of atypical mitoses: HR=5.41, p<0.0001; necrosis: HR=3.01, p=0.0428; severe nuclear atypia: p<0.0001; mitotic count>=2: HR=7.56, p<0.0001) and OS (presence of atypical mitoses: HR=5.30, p=0.0085; necrosis: HR=3.85, p=0.0293; nuclear atypia: p<0.0001; mitotic count: HR=4.40, p=0.0174). (O, P) Patients with Ki-67 ≥10% were significantly correlated with poor PFS (HR=13.38; p<0.0001 and OS (HR=15.15; p=0.0005). (Q, R) Patients with negative SMA staining (IHC score 0-2) also exhibited shorter PFS (HR=4.59; p=0.0002) and OS (HR=16.96; p<0.0001).
Additional file 2. Supplementary Table 1.
Distribution of prognostic risk factors in 57 renal eAML patient. Risk factors included: pT3 and pT4, presence of necrosis, mitotic count≥2; the presence of atypical mitoses; severe nuclear atypia, SMA negative, Ki-67≥10%. Low-risk group: including 0-1 risk factor, Intermediate-risk group: including 2-3 risk factors, High-risk group: including 4-7 risk factors. *p value less than 0.05 was considered as statistically significant and marked in bold.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Anwaier, A., Xu, WH., Tian, X. et al. ♣Evaluation of clinicopathological profiles and development of a risk model in renal epithelioid angiomyolipoma patients: a large-scale retrospective cohort study. BMC Urol 22, 148 (2022). https://doi.org/10.1186/s12894-022-01101-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-022-01101-9