Abstract
Background
Garden I femoral neck fractures are nondisplaced femoral neck fractures. Nonoperative treatment and in situ fixation are the preferred treatments. However, the postoperative outcome is not satisfactory and the incidence of complications remains high, which raises doubts about the accuracy of the diagnosis of nondisplaced Garden I fractures. Recently, three-dimensional (3D) reconstruction has been reported as a mature technology for reconstructing the bone structure of patients. We further extended this technique in the measurement of the fracture spatial displacement to verify the accuracy of Garden I femoral neck fractures.
Methods
This was a retrospective study of patients with Garden I femoral neck fractures from January 2013 to December 2018 at our institution, who were included according to specified criteria. A bilateral proximal femur model of each patient was established based on computed tomography (CT) data. The displacement of the deepest portion of the femoral head fovea, the displacement of the center of the femoral head and the rotation of the femoral head were measured in the bilateral model.
Results
A total of 102 patients diagnosed with Garden I fractures were included in this study. The cohort included 32 men and 70 women, with an average age of 55.88 ± 15.32 years. In these patients, the average displacement of the deepest portion of the femoral head fovea was 16.43 ± 7.69 mm. The minimum and maximum displacement was 3.58 and 44.32 mm, respectively. The average displacement of the center of the femoral head was 10.39 ± 5.47 mm and ranged from 2.16 to 34.42 mm. The rotational angle was 23.81 ± 10.15 ° and ranged from 3.71 ° to 61.19 °.
Conclusions
Garden I fractures have large spatial displacement and cannot be considered incomplete or nondisplaced fractures. Therefore, we suggest that anatomical reduction should be considered during treatment.
Similar content being viewed by others
Background
Patients with femoral neck fractures are at substantial risk for disability, death and reduced quality of life [1,2,3]. Garden I fractures are called nondisplaced fractures, accounting for 15–33% of all femoral neck fractures [4, 5]. Despite the high frequency of the injury [6], no consensus exists about the optimal management of Garden I femoral neck fractures. Options include nonsurgical treatment, which involves fixation with plaster after traction or manual reduction; surgical treatment, which involves treatment with in situ fixation using multiple parallel cannulated screws and arthroplasty. Advocates of nonsurgical treatment perceive benefits with regard to patients’ prognostic function and quality of life compared with surgical treatment for Garden I fractures [7]. There are concerns, however, that nonsurgical treatment has a higher complication rate than surgical treatment and may increase the risk of secondary displacement [8, 9]. Primary arthroplasty may be considered for Garden I and II femoral neck fractures with posterior tilt ≥ 20°, especially among older patients [10].
Surgical treatment was also reported to be optimal [11]. Meta-analyses of studies involving patients with nondisplaced femoral neck fractures have suggested that surgical treatment results in a higher cure rate and lower rate of femoral head necrosis than nonsurgical treatment [12]. In the surgical treatment of nondisplaced femoral neck fractures, in situ fixation using multiple parallel cannulated screws has been favored by orthopedic surgeons [13, 14]. However, many previous studies report a high incidence of femoral head necrosis after internal fixation using various parallel implants for the surgical treatment of Garden I or II fractures [15,16,17].
Necrosis is caused by displacement of the femoral head, which results in the femoral head being subjected to improper forces [18]. The high incidence of osteonecrosis of the femoral head raises doubts about the accuracy of the diagnosis of nondisplaced Garden I fractures. The purpose of the current study was to precisely measure the spatial displacement of the femoral head in Garden I femoral neck fractures by using three-dimensional (3D) reconstruction and digital technology. These data were used to reevaluate the deficiency of Garden I fractures and to improve the diagnosis and treatment of these fractures in clinical practice.
Materials and methods
Study population
This retrospective study collected patients with Garden I femoral neck fractures from January 2013 to December 2018 at our institution. The fractures were classified based on the original Garden classification using the original preoperative anteroposterior radiographs [19]. All patients were selected with a standard diagnostic code, exclusion rule, and inclusion rule.
Inclusion criteria were as follows: (1) simple unilateral femoral neck fracture, and (2) fresh fracture. The exclusion criteria were as follows: (1) ipsilateral femoral shaft fracture or bilateral femoral neck fractures, (2) pathological femoral neck fracture, (3) congenital malformation, (4) previous femoral neck fracture, and (5) lack of preoperative anteroposterior radiographs or CT data.
This study was approved by our institutional ethics committee, and patients provided informed consent.
Establishment of Model
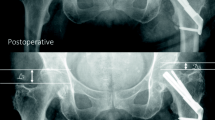
The CT data of the patients were imported into Mimics 22.0 (Materialize, Leuven, Belgium) in DICOM format, which generated 3D models of the bilateral proximal femurs. Using the mirror function in Mimics, a mirror 3D model of the normal femur was established. Then, the mirror model of the normal femur was superimposed on the model of the fractured femur. Registration of two 3D models was completed according to the overlap of the greater and lesser trochanter and the direction of the femoral shaft.
Three-dimensional measurement
To measure the displacement and rotation of the femoral neck fracture, two distinct and constant anatomical landmarks were selected: the femoral head fovea and the femoral head center. The lowermost point was marked in the femoral head fovea. The femoral head center was calculated and marked automatically by selecting four points on the edge of the femoral head using a 3-matic module. The distance between the lowermost points of the bilateral femoral head fovea (d1) and the distance between the centers of the bilateral femoral heads (d2) were selected to describe the displacement of the femoral neck fracture. In addition, the angle between lines drawn between two feature points (α) was used to measure the rotation of the femoral neck fracture (Fig. 1).
Statistical method
All data were analyzed using SPSS version 21 (IBM, USA). Means and standard deviations for the variables were obtained.
Results
A total of 267 patients with femoral neck fractures in the Tian** Hospital database during our study dates were diagnosed with Garden I fracture. Of these, 102 patients met our selection criteria. This cohort included 32 men and 70 women, with an average age of 55.88 ± 15.32.
In these patients, the average displacement of the deepest portion of the femoral head fovea was 16.43 ± 7.69 mm, the average displacement of the center of the femoral head was 10.39 ± 5.47 mm, and the rotational angle was 23.81 ± 10.15° (Table 1).
Discussion
Accurate diagnosis of fracture displacement is helpful in choosing the treatment method. Garden classification is commonly used in the clinic and is superior to other classification methods [20]. However, an increasing number of scholars have recently questioned the Garden classification. Chen [21]found that incomplete femoral neck fractures observed on radiographs are complete fractures on CT. Du’s three-dimensional reconstruction revealed a spatial displacement angle of 17.17 ± 10.40° for the inserted fracture, indicating the limitations of the Garden classification [22]. The results (Table 1) showed that the distance of the bilateral femoral head foveae was 3.58–44.32 mm, the distance of the bilateral femoral heads was 2.16–34.42 mm, and the rotation of the femoral head was 3.71–61.19°, which further confirms that the Garden classification is inaccurate in diagnosing fracture displacement.
Studies have found that the rate of femoral head necrosis, fracture redisplacement rate, and fracture nonunion rate are higher after nonsurgical treatment of Garden I fracture [23]. Based on the results of this study, we believe that patients with Garden I fractures cannot achieve effective reduction of fractures either conservatively or with in situ fixation surgery [24, 25]. However, it easily leads to fracture deformity and healing, increasing the risk of osteonecrosis of the femoral head. Therefore, we suggest that anatomic reduction is recommended for X-ray diagnosis of Garden I femoral neck fracture.
This study follows the measurement method proposed by Ma’s team [22]. Displacement measurement is based on bilateral limb symmetry and high reliability [18]. The feature points selected in the measurement are easy to identify on the femur and have a low error rate. Zhang [26]believes that this method has certain advantages in assessing fracture displacement. The limitation of this study is that the sample size is small. The next step is to continue the study using big data from multiple centers.
Conclusions
Garden I femoral neck fractures have large spatial displacement and cannot be considered incomplete or nondisplaced fractures. Therefore, we suggest that CT and 3D reconstruction should be used in the diagnosis of femoral neck fractures to improve the accuracy of diagnosis and treatment, especially before selecting surgical options.
Data Availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 3D:
-
Three-dimensional
- CT:
-
Computed tomography
References
Cooper C, Campion G, Melton LR. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–9.
Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377:2053–62.
Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87:2122–30.
Aufranc OE, Jones WN, Harris WH. Undisplaced femoral neck fracture. JAMA. 1964;189:314–7.
Editorial Board of Osteoporosis Prevention and Treatment. (China White Paper), China Health Promotion Foundation. White paper on osteoporosis. Chin J Health Manage. 2009;3:148–54.
Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011;45:15–22.
Amsellem D, Parratte S, Flecher X, Argenson JN, Ollivier M. Non-operative treatment is a reliable option in over two thirds of patients with Garden I hip fractures. Rates and risk factors for failure in 298 patients. Orthop Traumatol Surg Res. 2019;105:985–90.
Taha ME, Audigé L, Siegel G, Renner N. Factors predicting secondary displacement after non-operative treatment of undisplaced femoral neck fractures. Arch Orthop Trauma Surg. 2015;135:243–9.
Buord JM, Flecher X, Parratte S, Boyer L, Aubaniac JM, Argenson JN. Garden I femoral neck fractures in patients 65 years old and older: is conservative functional treatment a viable option? Orthop Traumatol Surg Res. 2010;96:228–34.
Okike K, Udogwu UN, Isaac M, Sprague S, Swiontkowski MF, Bhandari M, et al. Not all Garden-I and II femoral neck fractures in the elderly should be fixed: effect of posterior tilt on rates of subsequent arthroplasty. J Bone Joint Surg Am. 2019;101:1852–9.
Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the american board of orthopaedic surgery database. J Bone Joint Surg Am. 2014;96:e149.
Xu DF, Bi FG, Ma CY, Wen ZF, Cai XZ. A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis. J Orthop Surg Res. 2017;12:28–40.
Rodríguez-Merchán EC. In situ fixation of nondisplaced intracapsular fractures of the proximal femur. Clin Orthop Relat Res. 2002;399:42–51.
Shin WC, Moon NH, Jang JH, Jeong JY, Suh KT. Three-dimensional analyses to predict surgical outcomes in non-displaced or valgus impaction fractures of the femoral neck: a multicenter retrospective study. Orthop Traumatol Surg Res. 2019;105:991–8.
Rodríguez-Merchán EC. Displaced intracapsular hip fractures: hemiarthroplasty or total arthroplasty? Clin Orthop Relat Res. 2002;399:72–7.
Bjørgul K, Reikerås O. Outcome of undisplaced and moderately displaced femoral neck fractures. Acta Orthop. 2007;78:498–504.
Phillips JE, Christie J. Undisplaced fracture of the neck of the femur: results of treatment of 100 patients treated by single Watson-Jones nail fixation. Injury. 1988;19:93–6.
Wang Y, Ma JX, Yin T, Han Z, Cui SS, Liu ZP, et al. Correlation between reduction quality of femoral Neck fracture and femoral Head Necrosis based on Biomechanics. Orthop Surg. 2019;11:318–24.
Garden RS. Stability and union in subcapital fractures of the femur. J Bone Joint Surg Br. 1964;46:630–47.
Wang MY, Wei J. Some problems and new concepts in clinical research on femoral neck fractures. Chin J Orthop Trauma. 2003;5:5–9.
Chen W, Li Z, Su Y, Hou Z, Zhang Q, Zhang Y. Garden type I fractures myth or reality? A prospective study comparing CT scans with X-ray findings in Garden type I femoral neck fractures. Bone. 2012;51:929–32.
Du CL, Ma XL, Zhang T, Zhang HF, Wang CG, Zhao F, et al. Reunderstanding of garden type I femoral neck fractures by 3-dimensional reconstruction. Orthopedics. 2013;36:820–5.
Hardy J, Collin C, Mathieu PA, Vergnenègre G, Charissoux JL, Marcheix PS. Is non-operative treatment still relevant for Garden Type I fractures in elderly patients? The femoral neck impaction angle as a new CT parameter for determining the indications of non-operative treatment. Orthop Traumatol Surg Res. 2019;105:479–83.
Koval KJ, Zuckerman JD. Hip fractures. A practical guide to management. New York: Springer; 2000.
Swart E, Roulette P, Leas D, Bozic KJ, Karunakar M. ORIF or arthroplasty for displaced femoral Neck Fractures in patients younger Than 65 Years Old: an economic decision analysis. J Bone Joint Surg Am. 2017;99:65–75.
Zhang LP, Zhang GL, Xu W, Wang D, Wang WL. Correlation between reduction quality of femoral neck fracture and femoral head necrosis evaluated by three-dimensional measurement method. Chin J Tissue Eng Res. 2016;20:3287–93.
Acknowledgements
The authors gratefully acknowledged all collaborating researchers and participants during this study.
Funding
This work was supported by Tian** Science and Technology planning Project [No. 21JCQNJC01060]; Key project of Tian** Natural Science Foundation [No. 22JCZDJC00340]; National Key Research and Development Project of China [No. 2022YFC3601904].
Author information
Authors and Affiliations
Contributions
Ying Wang, Jianxiong Ma and **nlong Ma conceived the theme of study and drafted the manuscript. Ying Wang and Hongqi Zhan collected cases and conducted data analysis. Bin Lu, Lei Sun and **ngwen Zhao conducted three-dimensional model modeling. Jiahui Chen, Yanfei Wu made measurements of the three-dimensional model. Haohao Bai and **nlong Ma revised this manuscript and all the author read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval statement
All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki) and all experimental protocols were approved by Tian** hospital ethics committee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, Y., Ma, J., Bai, H. et al. A three-dimensional measurement study of fracture displacement in Garden I femoral neck fracture: a retrospective study. BMC Musculoskelet Disord 24, 623 (2023). https://doi.org/10.1186/s12891-023-06737-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06737-8