Abstract
Background
Previous studies have found that increased intra-abdominal pressure helps to reduce spinal loading and improve spine stability. Non-extensible lumbar belts (NEBs) could elevate intra-abdominal pressure and augment spinal stability. NEBs have been used in the healthcare field to help reduce pain and improve spine function for people with low back pain. However, the effect of NEBs on static and dynamic postural stability is not clear.
Methods
This study aimed to investigate whether NEBs affect static and dynamic postural stability. Twenty-eight healthy male subjects were recruited to finish four static postural stability tasks and two dynamic postural stability tests. Center of pressure (COP) values during 30 s of quiet standing, dynamic postural stability index (DPSI) and Y balance test (YBT) score with and without NEBs were analyzed.
Results
NEBs had no significant effect in all COP variables in the static postural tasks. The results of a repeated measure two-way ANOVA indicated the NEBs significantly improved the dynamic postural stability in YBT score and DPSI (F (1,27) = 5.506, p = .027, \({{\eta }_{p}}^{2}=.169\) and F (1,27) = 83.94, p = .000, \({{\eta }_{p}}^{2}=.757\) respectively).
Conclusions
The study results indicate that non-extensible belts improve dynamic stability in healthy male participants, with potential implications for rehabilitation and performance enhancement programs.
Similar content being viewed by others
Background
Lumbar belts (LBs) have been applied to protect the lumbar and relieve low back pain (LBP) [1]. People with LBP exhibited impaired postural stability during standing and increased trunk muscle activity during dynamic activities [2,3,4]. LBs are regarded to reduce the lumbar range of motion and enhance lumbar stiffness during maximal trunk flexion–extension and manual material handling tasks [5]. Although there is a small decrease in muscle activation with LBs [1, 6], they do not decondition the muscle, decrease spinal function and induce muscle fatigue wearing for a certain period of time [7, 8]. LBs reduce pain and decrease functional impairment for people with LBP [1, 6, 9].
The possible mechanism of LBs for relieving LBP is to improve spine stability and reduce spinal loading by increasing intra-abdominal pressure (IAP) [9, 10]. Studies show that increased IAP can promote co-contraction of spinal flexor and extensor muscles to increase trunk stiffness [10, 11]. Besides, IAP generates a longitudinal moment acting on the pelvis and diaphragm, which helps reduce intervertebral pressure and enhance spine stability [12]. Furthermore, transversus abdominis (TrA), in which bundles run horizontally, can transfer tension from the abdominal muscles to the lumbar spine, thereby regulating the segmental motion of the lumbar spine [13]. Biomechanical models have shown that TrA successfully compensates for other abdominal muscle co-activities [14]. LBs increase IAP by tightening the abdominal cavity like TrA to stabilize the spine. Also, it was reported that an adequate IAP increase leads to an enhancement of hip extension maximum voluntary contraction torque [15], which may help to improve stability. Above all, LBs seem to be simple and effective in augmenting IAP and improving spine stability.
Static and dynamic postural stability (PS) are essential for controlling the center of mass and maintaining equilibrium [16]. Typically, static PS is assessed by collecting the center of pressure (COP) trajectories during quiet standing with different visual or somatosensory conditions [17]. In contrast, dynamic PS reflects the ability to coordinate locomotor and maintain PS in sports and daily life [16, 18]. Previous studies have shown that dynamic PS tasks, such as landing and stabilizing after a jump, involve additional components of the neuromuscular systems compared to static posture tasks [19, 20]. One of the most commonly used clinical assessments for dynamic postural PS is the Y balance test (YBT), which has high reliability and validity [21]. However, YBT cannot capture the PS variability during dynamic posture transition [22]. To address this limitation, the dynamic postural stability index (DPSI) has been developed to measure stability during sudden transitions from a dynamic to a static state [23]. Previous work has shown that DPSI is an accurate and sensitive method for measuring the variability in ground reaction forces on landing [24,25,26]. Combining YBT and DPSI provides a comprehensive assessment of dynamic PS.
Several studies have revealed that LBs can improve PS by enhancing spine stability and supporting the lower back [1, 8, 27]. For instance, one study reported that the postural sway of people with LBP showed a 51% reduction during standing wearing a lumbar support [27]. In terms of the immediate effects of LBs on postural control, another study found that wearing LBs for 4 weeks improved static PS in anteroposterior and mediolateral directions among people with LBP [28]. Additionally, a systematic review revealed that external lumbar supports had positive effects on postural control in conditions where somatosensory interference was presented, such as LBP or standing on an unstable surface [29]. However, some studies did not reach the same conclusion. Some studies showed that LBs reduced posture sway in patients with LBP only when completing challenging postural tasks (i.e., single leg landing with closed eyes), while others indicated that lumbar supports mainly corrected posture mechanics and failed to affect postural control system [30,31,32]. These inconsistent findings highlight the need for more evidence regarding the effect of LBs on static PS. Despite the existing studies on LBs on static PS, the evaluation of dynamic PS changes is of great significance. To our knowledge, no study has yet examined the effect of LBs on dynamic PS by YBT or DPSI. Thus, in this study, we aim to use DPSI combined with YBT to investigate the impact of LBs on dynamic PS.
The effect of LBs for improving stability is closely related to the material and design of the LBs [9, 32]. Extensible and non-extensible belts (NEBs) are two common types of LBs. Extensible belts are elastic made of neoprene and lycra, while NEBs are made of polyester and nylon with fixed length [32, 33]. Besides, NEBs have a tensioning system with rigid anchors in the back and adjustable straps on both sides, which can increase intra-abdominal pressure [1]. While both types of LBs have been reported to enhance spinal stability in healthy adults, the materials and design of LBs may result in different outcomes in terms of their effects on spine stability [1, 33]. Several studies have found that NEBs increase trunk stiffness more significantly than extensible belts [7, 32, 34]. Moreover, a study that compared the effects of both types of belts on trunk stiffness with a pressure of 70 mmHg found that NEBs were more effective in restricting trunk motion following a perturbation [34]. Furthermore, wearing a NEB for two weeks significantly increased trunk extensor endurance for healthy participants who performed a modified Sorensen test, while wearing extensible belts for 21 days decreased trunk extensor endurance [7, 35]. Additionally, NEBs were found to lead to greater improvement in daily living function for LBP patients than extensible belts [32]. Therefore, it can be preliminarily considered that the NEB is a better lumbar belt option for enhancing IAP and spine stability.
Above all, the aim of this study is to investigate the effect of NEBs on static and dynamic PS in different static and dynamic postural tasks. As NEBs have been demonstrated to augment spine stability by inducing higher IAP, we hypothesized that NEBs contribute to improving static and dynamic PS in healthy subjects.
Methods
Participants
This study recruited 28 male subjects (age = 22 ± 2.07 years, height = 175.79 ± 5.82 cm, weight = 65.9 ± 7.84 kg). The dominant leg of all subjects was the right leg. The dominant leg was determined through a test to hit a soccer ball. The exclusion criteria were injuries of the lower extremity in the past six months and lower extremity surgery in the past two years and any musculoskeletal condition that might interfere with postural stability, such as lower extremity soreness or a neurological disorder. The sample size was calculated using G*Power software (Version 3.1 for Mac). The results indicated that a total of 24 participants were necessary with a significant level of 0.05, an effect size of 0.25 and a statistical power of 0.8 [36, 37].
Experimental procedures
The subjects completed the static and dynamic PS tests with and without the NEB, respectively, of which the static PS test was standing still for 30 s under different conditions [38]. Dynamic PS tests included YBT and jump landing. The test order was pseudo-randomized and counterbalanced. Half of the subjects completed the tests with NEB first, and the other half completed the tests without NEB first. The time interval between trials was 30 s. The NEB applied pressure was set to 70 mmHg measured by a force sensor inserted between the above anterior superior iliac crest and the NEB (applied pressure = 77.76 ± 11.18 mmHg) [34] (Fig. 1).
Static postural stability test
Static PS were tested using four paradigms: 1) Standing with eyes open on firm ground (EO); 2) Standing with eyes closed on firm ground (EC); 3) Standing with eyes open with a foam mat (EOMAT); 4) Standing with eyes closed with a foam mat (ECMAT) [39, 40]. The first task was chosen because it reflects the posture in natural state, and the latter ones were picked to disturb the visual and/or somatosensory systems. The foam mat used in this study was the Airex Balance Pad (Airex AG, Sins, Switzerland).
Subjects were requested to stand upright on a force platform (OR-6, 1000 Hz, AMTI, USA) with their arms at their sides, barefoot with feet together, remaining as stable as possible, and looking straight ahead at the black cross marked 1.5 m away on the wall.
Dynamic postural stability test
Two dynamic PS tests were conducted, including YBT and jump landing. For YBT, subjects were asked to put their hands on their hips and place the most distal end of the longest toe of the stance leg barefoot at the red line on the platform on the test kit while the other leg gently pushed the baffle to the limit in anterior, posteromedial, and posterolateral directions [22]. In the whole process, the subjects need to maintain balance. If there were phenomena such as the swing leg falling and the stance leg moving off the platform, the attempts would not count. The assessment was conducted on both the non-dominant (N-Dominant) and dominant (Dom) legs. To obtain accurate measurements, three consecutive attempts were performed in each direction with both legs, and the maximum value was selected for data analysis [41]. All subjects were familiarized with the test after completing 4 to 6 practices trials.
For jump landing, participants were required to take off on both feet from a specific distance and jump over a hurdle and the dominant leg landing on the force platform and standing with hands-on-hips for 10 s, including anterior–posterior (AP) jump and medial–lateral (ML) jump. The force platform is flush with the surrounding ground. The jump distance equals 40% and 33% of the subjects' height in the AP and ML jump, respectively. The height of hurdles in the AP and ML jump is 30 cm and 15 cm, respectively [42]. If the non-stance leg of the subject touched the stance leg or force platform and the stance leg was moving, trials were discarded and retested. Two successful trials were required in each direction, and the mean value was used for analysis [43].
Data processing
All data from the force platform were processed offline using customized MATLAB programs (R2021a, MathWorks, USA) and filtered using low-pass Butterworth filters with a cut-off frequency of 20 Hz. COP trajectories were calculated by Eq. (1) and Eq. (2), in which d (0.038 m) represents the height of the force platform itself [44]. Considering the influence of oral instructions by the investigator at the start and the end of the static PS test on COP trajectory, the first and the last 5 s of raw data were discarded. COP sway area (EA) was calculated with a 95% confidence ellipse area. COP path length (PL), COP velocity in the mediolateral (ML velocity) and anteroposterior (AP velocity) directions were also calculated. DPSI values of 3 s were calculated for the filtered GRF data according to Eq. (3) [24]. Data were cropped from the time of initial contact with the force platform, defined by a threshold of greater than 5.0% of body weight [45]. YBT data was calculated for the composite score using Eq. (4) [41].
Statistical analysis
SPSS software (version 20.0, IBM. USA) analyzed the processed data statistically. Data distribution was examined for normality using Shapiro–Wilk test (< 50 samples). T-tests and non-parametric alternatives Wilcoxon signed-rank test were used to analyze differences between without NEB and NEB conditions resulting from different static postural stability tasks. A repeated-measure two-way analysis of variance (ANOVA) design was used to assess the effect of NEB on YBT composite score (NEB × stance leg), and DPSI (NEB × jump direction). Bonferroni was used for post hoc. The statistical significance level was set as p < 0.05.
Results
Twenty-eight male subjects finished four static PS tasks and two types of dynamic PS tasks. The data of static PS tasks were shown in Table 1. The static PS parameters related to the COP sway, i.e., EA and PL did not differ for without NEB conditions or NEB conditions either in eyes open nor eyes closed condition. Similarly, the stability parameters related to the COP velocity did not differ for without NEB conditions or NEB conditions.
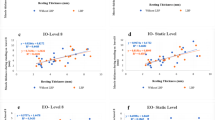
The analysis results of DPSI are shown in Fig. 2. The main effect of NEB was significant (F (1,27) = 83.94, p = 0.000, \({{\eta }_{p}}^{2}=.757\)), but the main effect of the jump direction was not significant (F (1,27) = 83.94, p = 0.850, \({{\eta }_{p}}^{2}=.001\)), and the interaction effect of NEB and jump direction was not significant (F (1,27) = 83.94, p = 0.783, \({{\eta }_{p}}^{2}=.077\)).
The analysis results of YBT are shown in Fig. 3. The composite score showed a significant main effect of NEB (F (1,27) = 5.506, p = 0.027, \({{\eta }_{p}}^{2}=.169\)), and the main effect of the stance leg was not significant (F (1,27) = 1.309, p = 0.263, \({{\eta }_{p}}^{2}=.046\)), and the interaction effect of NEB and the stance leg was not significant (F (1,27) = 1.867, p = 0.183, \({{\eta }_{p}}^{2}=.065\)).
Discussion
This study aimed to determine the effect of NEBs on static and dynamic PS in healthy participants. The main findings of this study were as follows: 1) the NEBs had no significant effect on the static PS in healthy male participants; 2). the NEBs were beneficial for healthy male subjects to improving dynamic PS.
No significant difference of COP values was revealed between NEB wearing and not wearing tasks, including in visual deprivation and somatosensory interference conditions. Previous studies about the effect of lumbar belts and orthosis rarely measured the COP of postural stability [27, 46]. Several relevant studies involving COP values showed that wearing orthosis contributed to reducing the postural sway [31, 47]. One study reported no significant changes in COP values (i.e., AP velocity and ML velocity) of the NEB group compared to the control group under open or closed eyes conditions, which is consistent with our findings [31]. Another study found that a lumbar orthosis reduced COP mean displacement by 51% for LBP patients during quiet standing with eyes closed [27]. However, the authors suggested that the degree of displacement was insufficient to explain the effects of the lumbar orthosis. Additionally, another study found that the lumbar orthoses improved static stability when standing on a foam mat [47]. A systematic review also showed the positive effects of LBs on static PS were observed in the case of somatosensory feedback impaired (i.e. LBP) or deprivation (i.e. standing on an unstable surface with eyes closed) [29]. In line with the results above, a study concluded that the effect of LBs is associated with the challenging of the postural tasks and the type of subjects [30]. In our study, quiet standing was a simple task for healthy participants, which made the NEB not show the effect of enhancing static PS. Furthermore, as previously described, the somatosensory acuity of the spine affects trunk muscle control and altered postural control [48, 49]. It was noted that the somatosensory function in the low back region of patients with LBP is compromised [50]. LBs were thought to could partly provide somatosensory information for the lumbar of LBP [51]. However, another study presented that LBs had no somatosensory benefits to healthy subjects [52], which might explain why the NEB did not improve static PS in our study. Future research should examine the effect of the NEB on elderly and LBP patients with balance disorders and somatosensory impairment.
In addition to static PS testing, more studies about postural control have begun to pay attention to dynamic PS. Nevertheless, to the best of our understanding, there hasn't been any prior research assessing the impact of the NEB on dynamic PS. Our study initially discovered that the utilization of NEB led to an improvement in dynamic PS among healthy male participants. The dynamic PS was assessed through two standardized tests that measured balance and stability, including YBT and DPSI. The results showed a statistically significant improvement in dynamic PS among participants who wore the NEB compared to those who did not. On average, the improvement of DPSI was 9.3% and 1.5% of YBT score higher in the NEB condition. These results suggest that utilizing NEBs may be a slightly effective intervention for improving dynamic PS in healthy males.
Our investigation found that the utilization of NEBs led to an average elevation of IAP to 70 mmHg. Previous research has demonstrated that IAP impacts body movement, which aligns with the decrease in DPSI observed in our study [53]. Additionally, a 30 mmHg increase in IAP has been shown to improve spinal stability by 25% [53], and targeted trunk muscle strengthening exercises have also been demonstrated to enhance spinal stability and postural control in individuals with LBP [54]. Similarly, heightened IAP has been shown to enhancing spinal stability [55]. These findings support our conclusion that the use of NEBs improve dynamic postural stability by enhancing spinal stability. Furthermore, one study reported a significant improvement in walking efficacy for LBP patients without causing erector spinae muscle fatigue after walking a NEB for a month, suggesting that NEBs may contribute to enhancing dynamic performance [8]. However, the effect of NEBs on dynamic postural stability is not yet fully understood and requires further investigation. Future research should aim to explore the long-term effects of NEBs on dynamic postural stability and the underlying mechanisms.
The Jump landing test presents a reliable and challenging evaluation of dynamic PS [45], which was initially designed to assess the dynamic balance of athletes. DPSI has been found to reflect not only the adjustment phase of the center of mass during impact, but also the kinetic energy absorption during the landing process [56], making it a comprehensive indicator of joint energy absorption and PS during jum** movements. Previous studies, as well as our own, have consistently demonstrated that there is no significant difference in DPSI between AP and ML jumps. This is likely due to the fact that DPSI primarily reflects the body's ability to absorb kinetic energy from the vertical peak force and is not strongly influenced by the direction of the jump [26, 57]. Therefore, while our findings and those of previous studies suggest that there may be no significant difference in DPSI between AP and ML jumps, further research is needed to confirm and expand upon these results. Addtionally, the correlation between spinal stability and dynamic PS has yet to be thoroughly investigated, despite studies indicating that ankle and knee flexion and extension strength predict dynamic PS [25]. Our findings suggest that improving spinal stability through the use of NEBs enhance dynamic postural stability, though further research is needed to fully understand the underlying mechanism of this relationship.
The improvement in dynamic PS with the use of NEBs has potential clinical applications, especially for individuals who are prone to falls or have difficulty with balance, such as athletes with lower extremity injuries, older athletes and patients with balance disorders. Besides, the results of our study suggest that the NEB may be a useful tool for enhancing dynamic PS. It can be applied in several areas of health, including sports rehabilitation, physical therapy and so on, to enhance the effectiveness of treatment and promoting positive outcomes for individuals.
This study had two limitations. First, the participants were only healthy male individuals and not include females or other special populations. Therefore, the results may not be generalizable to other groups. Secondly, the EMG data of muscles were not collected in static and dynamic standing posture tests, therefore this study failed to explore the physiological and neural control mechanism of NEB on static and dynamic PS. Future research should include both genders to increase the generalizability of the findings, as well as investigate the effectiveness of NEBs in populations with LBP or musculoskeletal injuries. These results suggest that NEBs may be a useful component of rehabilitation programs for improving balance instability.
Conclusions
The results of our study showed that using non-extensible belts improved dynamic postural stability in healthy male participants, while static stability remained unchanged. These findings have implications for understanding the impact of non-extensible belts on postural stability and for the design and implementation of effective rehabilitation and performance enhancement programs. Further research is necessary to confirm these findings in other populations, including those with LBP, and to gain a better understanding of the mechanisms behind the improvement in dynamic stability.
Availability of data and materials
The dataset supporting the conclusions of this article is available from the corresponding author Jian Wang on reasonable request.
Abbreviations
- AP:
-
Anterior-posterior
- COP:
-
Center of pressure
- Dom:
-
Dominant leg
- DPSI:
-
Dynamic postural stability index
- EA:
-
Elliptical area
- EC:
-
Eyes closed on firm ground
- EO:
-
Eyes open on firm ground
- ECMAT:
-
Eyes closed with a foam mat
- EOMAT:
-
Eyes open with a foam mat
- IAP:
-
Intra-abdominal pressure
- LBP:
-
Low back pain
- LBs:
-
Lumbar belts
- NEBs:
-
Non-extensible lumbar belts
- NDom:
-
Non-Dominant leg
- ML:
-
Medial-lateral
- PL:
-
Path length
- PS:
-
Postural stability
- TrA:
-
Transversus abdominis
- YBT:
-
Y balance test
References
Ludvig D, Preuss R, Larivière C. The effect of extensible and non-extensible lumbar belts on trunk muscle activity and lumbar stiffness in subjects with and without low-back pain. Clin Biomech. 2019;67:45–51. https://doi.org/10.1016/j.clinbiomech.2019.04.019.
Koch C, Hänsel F. Non-specific low back pain and postural control during quiet standing—a systematic review. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.00586.
Hemming R, Sheeran L, van Deursen R, Sparkes V. Investigating differences in trunk muscle activity in non-specific chronic low back pain subgroups and no-low back pain controls during functional tasks: a case-control study. BMC Musculoskelet Disord. 2019;20:459. https://doi.org/10.1186/s12891-019-2843-2.
Li X, Lo WLA, Lu S, Liu H, Lin K, Lai J, et al. Trunk muscle activity during pressure feedback monitoring among individuals with and without chronic low Back pain. BMC Musculoskelet Disord. 2020;21:569. https://doi.org/10.1186/s12891-020-03565-y.
Shahvarpour A, Preuss R, Sullivan MJL, Negrini A, Larivière C. The effect of wearing a lumbar belt on biomechanical and psychological outcomes related to maximal flexion-extension motion and manual material handling. Appl Ergon. 2018;69:17–24. https://doi.org/10.1016/j.apergo.2018.01.001.
Cholewicki J, Peter Reeves N, Everding VQ, Morrisette DC. Lumbosacral orthoses reduce trunk muscle activity in a postural control task. J Biomech. 2007;40:1731–6. https://doi.org/10.1016/j.jbiomech.2006.08.005.
Kawchuk GN, Edgecombe TL, Wong AYL, Cojocaru A, Prasad N. A non-randomized clinical trial to assess the impact of nonrigid, inelastic corsets on spine function in low back pain participants and asymptomatic controls. Spine J. 2015;15:2222–7. https://doi.org/10.1016/j.spinee.2015.06.047.
Saito H, Sekiguchi M, Yamada H, Kubota T, Shigihara T, Iwasaki T, et al. Comparison of postural changes and muscle fatigue between two types of lumbar support: a prospective longitudinal study. Fukushima J Med Sci. 2014;60:141–8. https://doi.org/10.5387/fms.2014-17.
Anders C, Hübner A. Influence of elastic lumbar support belts on trunk muscle function in patients with non-specific acute lumbar back pain. PLOS ONE. 2019;14:e0211042. https://doi.org/10.1371/journal.pone.0211042.
Cholewicki J, Juluru K, Radebold A, Panjabi MM, McGill SM. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J. 1999;8:388–95. https://doi.org/10.1007/s005860050192.
Cholewicki J, Ivancic PC, Radebold A. Can increased intra-abdominal pressure in humans be decoupled from trunk muscle co-contraction during steady state isometric exertions? Eur J Appl Physiol. 2002;87:127–33. https://doi.org/10.1007/s00421-002-0598-0.
Stokes IAF, Gardner-Morse MG, Henry SM. Intra-abdominal pressure and abdominal wall muscular function: Spinal unloading mechanism. Clin Biomech. 2010;25:859–66. https://doi.org/10.1016/j.clinbiomech.2010.06.018.
Barker PJ, Urquhart DM, Story IH, Fahrer M, Briggs CA. The middle layer of lumbar fascia and attachments to lumbar transverse processes: implications for segmental control and fracture. Eur Spine J. 2007;16:2232–7. https://doi.org/10.1007/s00586-007-0502-z.
Guo J, Guo W, Ren G. Embodiment of intra-abdominal pressure in a flexible multibody model of the trunk and the spinal unloading effects during static lifting tasks. Biomech Model Mechanobiol. 2021;20:1599–626. https://doi.org/10.1007/s10237-021-01465-1.
Tayashiki K, Mizuno F, Kanehisa H, Miyamoto N. Causal effect of intra-abdominal pressure on maximal voluntary isometric hip extension torque. Eur J Appl Physiol. 2018;118:93–9. https://doi.org/10.1007/s00421-017-3748-0.
Marinkovic D, Belic A, Marijanac A, Martin-Wylie E, Madic D, Obradovic B. Static and dynamic postural stability of children girls engaged in modern dance. Eur J Sport Sci. 2022;22:354–9. https://doi.org/10.1080/17461391.2021.1922503.
Wright WG, Handy JD, Haskell A, Servatius L, Servatius R. History of mild traumatic brain injury affects static balance under complex multisensory manipulations. J Neurotrauma 2022:neu.2020.7600. https://doi.org/10.1089/neu.2020.7600.
Pau M, Mereu F, Melis M, Leban B, Corona F, Ibba G. Dynamic balance is impaired after a match in young elite soccer players. Phys Ther Sport. 2016;22:11–5. https://doi.org/10.1016/j.ptsp.2016.05.008.
Dallinga JM, van der Does HTD, Benjaminse A, Lemmink KAPM. Dynamic postural stability differences between male and female players with and without ankle sprain. Phys Ther Sport. 2016;17:69–75. https://doi.org/10.1016/j.ptsp.2015.05.002.
Godzik J, Frames CW, Smith Hussain V, Olson MC, Kakarla UK, Uribe JS, et al. Postural stability and dynamic balance in adult spinal deformity: prospective pilot study. World Neurosurg. 2020;141:e783–91. https://doi.org/10.1016/j.wneu.2020.06.010.
Gribble PA, Hertel J, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47:339–57. https://doi.org/10.4085/1062-6050-47.3.08.
Smith CA, Chimera NJ, Warren M. Association of Y balance test reach asymmetry and injury in division I athletes. Med Sci Sports Exerc. 2015;47:136–41. https://doi.org/10.1249/MSS.0000000000000380.
Wikstrom EA, Tillman MD, Schenker SM, Borsa PA. Jump-landing direction influences dynamic postural stability scores. J Sci Med Sport. 2008;11:106–11. https://doi.org/10.1016/j.jsams.2007.02.014.
Wikstrom EA, Tillman MD, Smith AN, Borsa PA. A new force-plate technology measure of dynamic postural stability: the dynamic postural stability index. 2005. p. 305–9.
Williams VJ, Nagai T, Sell TC, Abt JP, Rowe RS, McGrail MA, et al. Prediction of dynamic postural stability during single-leg jump landings by ankle and knee flexibility and strength. J Sport Rehabil. 2016;25:266–72. https://doi.org/10.1123/jsr.2015-0001.
Head PL, Kasser R, Appling S, Cappaert T, Singhal K, Zucker-Levin A. Anterior cruciate ligament reconstruction and dynamic stability at time of release for return to sport. Phys Ther Sport. 2019;38:80–6. https://doi.org/10.1016/j.ptsp.2019.04.016.
Munoz F. Low back pain sufferers: Is standing postural balance facilitated by a lordotic lumbar brace? Orthop Traumatol Surg Res. 2010;96:362–6.
Kang J-I, Kwon H-M, Jeong D-K, Choi H, Moon Y-J, Park J-S. The effects on postural control and low back pain according to the types of orthoses in chronic low back pain patients. J Phys Ther Sci. 2016;28:3074–7.
Azadinia F, Kingma I, Mazaheri M. Effect of external lumbar supports on joint position sense, postural control, and postural adjustment: a systematic review. Disabil Rehabil 2022:1–19. https://doi.org/10.1080/09638288.2022.2043464.
Ghofrani M, Olyaei G, Talebian S, Bagheri H, Malmir K, Mousavi S. Research Paper: Immediate effects of lumbosacral belt on postural control during challenging tasks in patients with chronic low back pain. J Mod Rehabil. 2017;11:119–26.
Azadinia F, Ebrahimi-Takamjani I, Kamyab M, Parnianpour M, Asgari M. A RCT comparing lumbosacral orthosis to routine physical therapy on postural stability in patients with chronic low back pain. Med J Islam Repub Iran. 2017;31:26. https://doi.org/10.18869/mjiri.31.26.
Morrisette DC, Cholewicki J, Logan S, Seif G, McGowan S. A randomized clinical trial comparing extensible and inextensible lumbosacral orthoses and standard care alone in the management of lower back pain. Spine. 2014;39:1733–42. https://doi.org/10.1097/BRS.0000000000000521.
Shahvarpour A, Preuss R, Larivière C. The effect of extensible and non-extensible lumbar belts on trunk postural balance in subjects with low back pain and healthy controls. Gait Posture. 2019;72:211–6. https://doi.org/10.1016/j.gaitpost.2019.06.013.
Cholewicki J, Lee AS, Peter Reeves N, Morrisette DC. Comparison of trunk stiffness provided by different design characteristics of lumbosacral orthoses. Clin Biomech. 2010;25:110–4. https://doi.org/10.1016/j.clinbiomech.2009.10.010.
Fayolle-Minon I, Calmels P. Effect of wearing a lumbar orthosis on trunk muscles: Study of the muscle strength after 21days of use on healthy subjects. Joint Bone Spine. 2008;75:58–63. https://doi.org/10.1016/j.jbspin.2007.04.018.
Prajapati B, Dunne M, Armstrong R. Sample size estimation and statistical power analyses. Optom Today. 2010;16:10–8.
Costantini G. A Practical Primer To Power Analysis for Simple Experimental Designs. Int Rev Soc Psychol. 2018;31:20. https://doi.org/10.5334/irsp.181.
Janura M. Standing balance of professional ballet dancers and non-dancers under different conditions. PLoS ONE. 2019;14:e0224145.
Wrisley DM, Whitney SL. The effect of foot position on the modified clinical test of sensory interaction and balance11No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated. Arch Phys Med Rehabil. 2004;85:335–8. https://doi.org/10.1016/j.apmr.2003.03.005.
Harringe ML, Halvorsen K, Renström P, Werner S. Postural control measured as the center of pressure excursion in young female gymnasts with low back pain or lower extremity injury. Gait Posture. 2008;28:38–45. https://doi.org/10.1016/j.gaitpost.2007.09.011.
González-Fernández FT, Martínez-Aranda LM, Falces-Prieto M, Nobari H, Clemente FM. Exploring the Y-Balance-Test scores and inter-limb asymmetry in soccer players: differences between competitive level and field positions. BMC Sports Sci Med Rehabil. 2022;14:45. https://doi.org/10.1186/s13102-022-00438-w.
Sell TC. An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Phys Ther Sport. 2012;13:80–6. https://doi.org/10.1016/j.ptsp.2011.06.006.
Huurnink A, Fransz DP, Kingma I, de Boode VA, van Dieën JH. The assessment of single-leg drop jump landing performance by means of ground reaction forces: a methodological study. Gait Posture. 2019;73:80–5. https://doi.org/10.1016/j.gaitpost.2019.06.015.
Winter A, Frank JS, Zabjek F. Unified theory regarding A/P and M/L balance in quiet stance. J Neurophysiol. 1996;75:2334–43.
Heebner NR, Akins JS, Lephart SM, Sell TC. Reliability and validity of an accelerometry based measure of static and dynamic postural stability in healthy and active individuals. Gait Posture. 2015;41:535–9. https://doi.org/10.1016/j.gaitpost.2014.12.009.
Azadinia F, Ebrahimi-Takamjani I, Kamyab M, Asgari M, Parnianpour M. Immediate effects of lumbosacral orthosis on postural stability in patients with low back pain: a preliminary study. Arch Bone Jt Surg. 2019;7:360–6.
Mi J, Ye J, Zhao X, Zhao J. Effects of lumbosacral orthoses on postural control in individuals with or without non-specific low back pain. Eur Spine J. 2018;27:180–6. https://doi.org/10.1007/s00586-017-5355-5.
Brumagne S, Janssens L, Knapen S, Claeys K, Suuden-Johanson E. Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J. 2008;17:1177–84. https://doi.org/10.1007/s00586-008-0709-7.
van Duijvenbode I, Jellema P, van Poppel M, van Tulder MW. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev. 2008. https://doi.org/10.1002/14651858.CD001823.pub3.
O’Sullivan PB, Burnett A, Floyd AN, Gadsdon K, Logiudice J, Miller D, et al. Lumbar Repositioning Deficit in a Specific Low Back Pain Population. Spine. 2003;28:1074–9. https://doi.org/10.1097/01.BRS.0000061990.56113.6F.
Newcomer K, Laskowski ER, Yu B, Johnson JC, An K-N. The effects of a lumbar support on repositioning error in subjects with low back pain. Arch Phys Med Rehabil. 2001;82:906–10. https://doi.org/10.1053/apmr.2001.23281.
Cholewicki J, Shah KR, McGill KC. The Effects of a 3-Week Use of Lumbosacral Orthoses on Proprioception in the Lumbar Spine. J Orthop Sports Phys Ther. 2006;36:225–31. https://doi.org/10.2519/jospt.2006.36.4.225.
Bojairami IE, Driscoll M. Coordination between trunk muscles, thoracolumbar fascia, and intra-abdominal pressure toward static spine stability. Spine. 2021. https://doi.org/10.1097/BRS.0000000000004223.
van Dieën JH, Selen LPJ, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol. 2003;13:333–51. https://doi.org/10.1016/S1050-6411(03)00041-5.
Cholewicki J, Juluru K, McGill SM. Intra-abdominal pressure mechanism for stabilizing the lumbar spine. J Biomech. 1999;32:13–7. https://doi.org/10.1016/S0021-9290(98)00129-8.
Fransz DP, Huurnink A, de Boode VA, Kingma I, van Dieën JH. Time series of ground reaction forces following a single leg drop jump landing in elite youth soccer players consist of four distinct phases. Gait Posture. 2016;50:137–44. https://doi.org/10.1016/j.gaitpost.2016.09.002.
Zhang Q, Hautier CA. Influence of jump-landing direction on dynamic postural stability and hamstring-to-quadriceps co-activation ratio. Res Sports Med 2021:1–11. https://doi.org/10.1080/15438627.2021.1975117.
Acknowledgements
The authors thank the participants for their contribution to the study.
Funding
This work was supported by the National Defense Foundation Strengthening Program Technology Field Fund Project [grant number 2022-JCJQ-JJ-0864].
Author information
Authors and Affiliations
Contributions
JW conceptualized the study and provided project supervision and administration. JB developed the study methodology and conducted formal analysis, as well as contributing to data curation and writing the original draft. AH and NW contributed to revising the manuscript. DW was involved in data collection and data curation. All authors have reviewed and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Research Ethics Board of Center for Psychological Sciences at Zhejiang University (issued no. 2020–003). All participants provided informed written consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bai, J., Hua, A., Weng, D. et al. Effects of non-extensible lumbar belts on static and dynamic postural stability. BMC Musculoskelet Disord 24, 362 (2023). https://doi.org/10.1186/s12891-023-06476-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06476-w