Abstract
Background
The possibility of adverse effects of medical treatment (AEMT) is increasing worldwide, but little is known about AEMT in China. This study analyzed the health burden of AEMT in China in recent years through the Global Burden of Disease Study (GBD) 2019 and compared it with the worldwide average level and those in different sociodemographic index (SDI) regions.
Methods
We calculated the age-standardized rate (ASR) of deaths, disability-adjusted life years (DALYs), years of life lost (YLLs), years lived with disability (YLDs), incidence and prevalence attributed to AEMT in China, worldwide and countries with different sociodemographic indices during 1990–2019 using the latest data and methods from the GBD 2019.
Results
From 1990 to 2019, the global age-standardized death rate (ASDR), DALYs, and YLLs for AEMT showed a significant downward trend and were negatively associated with the SDI. By 2040, the ASDR is expected to reach approximately 1.58 (95% UI: 1.33–1.80). From 1990 to 2019, there was no significant change in the global incidence of AEMT. The occurrence of AEMT was related to sex, and the incidence of AEMT was greater among females. In addition, the incidence of AEMT-related injuries and burdens, such as ASR of DALYs, ASR of YLLs and ASR of YLDs, was greater among women than among men. Very old and very young people were more likely to be exposed to AEMT.
Conclusions
From 1990 to 2019, progress was made worldwide in reducing the harm caused by AEMT. However, the incidence and prevalence of AEMT did not change significantly overall during this period. Therefore, the health sector should pay more attention to AEMT and take effective measures to reduce AEMT.
Similar content being viewed by others
Introduction
The adverse effects of medical treatment (AEMT) are commonly defined as “unintentional injuries during medical activities that affect a patient’s diagnosis, increase the patient’s pain and burden, and cause serious long-term irreversible consequences or death” [1]. AEMT are a result of a medical condition occurring widely in health care settings rather than the patient’s underlying disease [2]. In 1984, the Harvard Medical Practice Study was the first to provide an estimate of medical injuries in U.S. hospitals, and medical errors were estimated to be the third leading cause of death in the United States [1, 3]. In the 1980s, adverse reaction monitoring began in China, and currently, there are three main medical adverse event reporting systems. The adverse drug reaction monitoring system, gross medical negligence and medical malpractice reporting system, and patient safety (adverse event) reporting system are used [4]. Progress was made in reducing deaths from AEMT in the UK between 1990 and 2013, but unfortunately, the incidence of AEMT has not changed [5]. The occurrence of AEMT is common worldwide; fortunately, most adverse events are preventable [6]. Therefore, an increasing number of countries and regions have begun to attach importance to AEMT, which led to a key strategy developed by the World Health Organization (WHO) on AEMT that aims to halve the global incidence of AEMT by 2022 [7]. However, in light of physicians’ fears of negative consequences and lack of knowledge about AEMT, little is known about the levels, trends, and patterns of AEMT in hospital settings in China over time [8].
AEMT are a global health problem. Although the detection methods and reporting systems for AEMT have improved in recent years, there are still many worries and challenges [9]. The Global Burden of Disease Study (GBD) quantifies the global health losses caused by different diseases, injuries and risk factors. In addition, the GBD can use time, geographic location, age and sex to calculate the course of health loss caused by different causes [10]. Based on the GBD 2019, this study described the changing trend of the ASR of the incidence, prevalence, deaths, DALYs, YLDs and YLLs due to AEMT in China from 1990 to 2019, as well as forecasts of possible trends in the future. Although GBD data are estimated, this study is conducive to strengthening the public’s understanding of AEMT.
Methods
GBD 2019
The Global Study on Diseases, Injuries and Risk Factors is a systematic and collaborative global database (https://vizhub.healthdata.org/gbd-results/) that was established to quantify the health losses caused by hundreds of diseases from 1990 to 2019 according to age, sex and geographic location [11]. The GBD is based on multiple data sources (epidemiological studies, health registries, official statistics, hospital data, etc.) and applies highly sophisticated models to fill in data gaps to make the most informed estimates. Cause-specific death rates and cause fractions were calculated using the cause of death ensemble model and spatiotemporal Gaussian process regression. Cause-specific deaths were adjusted for to match the total all-cause deaths calculated as part of the GBD population, fertility, and mortality estimates [12, 13]. The list of causes in the GBD is detailed and regular due to the International Classification of Diseases (ICD) codes used for statistics [13]. We used the ICD-10 to define AEMT and then retrieved and analyzed epidemiological data attributed to AEMT from the latest GBD 2019. The forecast data for the ASDR and ASR of YLLs were obtained from the following website: https://vizhub.healthdata.org/gbd-foresight/.
Incidence and prevalence
The incidence was defined as the number of new cases of AEMT in a given region or country at a given time (one year) divided by the population of that region or country. The main distinction between prevalence and incidence is that the incidence emphasizes the frequency of new cases in a given population within a given period of time. The prevalence is a better indicator of the long-term occurrence of certain diseases and their impact on public health.
Years of Life Lost (YLLs), Years Lived with Disability (YLDs) and Disability-Adjusted Life Years (DALYs)
The guiding principle of the GBD is a comprehensive assessment of health loss due to death and disability, with disability defined as any deviation from full health. The Global Health Data Exchange (GHDx, http://ghdx.healthdata.org/) is the world’s largest health data repository. DisMod-MR 2.1 is a Bayesian meta-regression tool that was our primary method for analyzing nonmortality data [14]. YLLs are equal to the difference in standard life expectancy minus age at death, and YLDs are the number of years lived with disability. DisMod-MR 2.1 or meta-analysis is used to summarize the proportion of patients with each sequela or from patient series analysis. The YLD estimates are obtained by multiplying the prevalence of sequelae for each disease by an appropriate disability weight factor. YLLs are estimated by multiplying the number of deaths by the standard ideal remaining life expectancy at the time of death [15]. DALYs, a sum of YLLs and YLDs, use the total health loss of the population as a variable to estimate the total burden of AEMT.
Death rates
The death rate is the proportion of AEMT deaths per 100,000 people and is determined by the number of deaths caused by AEMT per year. Age-standardized death rates (ASDRs) can be used to effectively address the differences in mortality rates caused by population size and age structure in different regions. The WHO has modeled cause-of-death clusters for ASDRs under various conditions. The GBD model is used as a standardized tool for mortality causation analysis to obtain the ASDR across age, sex, geography, and year [16].
Sociodemographic index
The sociodemographic index (SDI) is a comprehensive indicator of the development status of countries in terms of overall national wealth. The SDI is a comprehensive evaluation of the average education level of the population aged 15 years and older, the average per capita income under a lagged distribution, and the total fertility rate of the population under 25 years old. The SDI classifies 195 countries and regions into five grades: low SDI, low middle SDI, middle SDI, high middle SDI and high SDI. Integrated analysis of the disease burden and SDI can better reveal the link between a specific disease and the development status of a country [17].
Statistical analysis
The GBD 2019 was used not only to calculate the ASR of various indicators for different ages, sexes and years but also to estimate the 95% uncertainty interval (UI) to quantify the total burden of adverse medical events between 1990 and 2019. The annual rate of change (ARC) can more directly display the temporal change trend of various data. The age group and the sex ratio can make the trend more visible. All the data were analyzed using GraphPad Prism 8.0.
Results
ASDRs of AEMT in China, worldwide and in other countries and regions with different SDI levels, 1990–2019
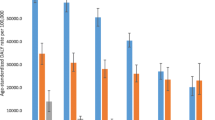
As shown in Table 1, there was a clear negative correlation between the ASDRs due to AEMT and the SDI levels from 1990 to 2019. From 1990 to 2019, the global ASDRs caused by AEMT showed a downward trend; China had an ARC of -0.76 (95% UI: -0.82 to -0.61) (Fig. 1A). The ratio of males to females in AEMT-related ASDRs was correlated with the SDI. In low-SDI areas, the ASDRs of AEMT were approximately the same for males and females. However, in low-middle-SDI regions, women had higher ASDRs than men did, and in other SDI areas, the ASDRs were greater for men than for women. From a sex perspective, the female-to-male ratio of ASDRs caused by AEMT in China has shown a significant downward trend in the past decade, and the ratio dropped to 0.64 in 2019.In 2019, the global ratio of males to females in ASDR due to AEMT was approximately 0.95 (Fig. 1B). Figure 1C shows the age distribution of the death rate due to AEMT in China, middle SDI regions and worldwide, and all of them showed similar trends. Mortality from AEMT showed a slightly higher in the early years of life, with a low death rate in the 10–60 age group, while the death rate of elderly individuals (over 60 years old) increased with age. China’s death rate attributed to AEMT was lower than that worldwide in any age group. The ASDR due to AEMT is expected to decline steadily in all regions by 2040. The global ASDRs for AEMT are predicted to be 1.67 (95% UI: 1.43–1.86) in 2030 and 1.58 (95% UI: 1.33–1.80) in 2040, and they are estimated to be 0.36 (95% UI: 0.31–0.48) in 2030 and 0.31 (95% UI: 0.26–0.41) in 2040 in China. Notably, countries in the low-SDI and middle-SDI regions still had high ASDRs (Fig. 1D).
Trends in ASDRs due to AEMT in China, in different SDI regions and globally, disaggregated by sex and age, 1990–2019. (A) ASDRs due to AEMT in China, SDI regions and globally in 1990, 2010 and 2019. (B) The difference and change trend of the sex ratio (female to male) of ASDRs due to AEMT in China from 1990 to 2019. (C) The age difference in the ASDR due to AEMT between China and the SDI regions. (D) The projected trend based on the change in the ASDR due to AEMT from 1990 to 2019, projected to 2040. ASDR, age-standardized death rate; AEMT, adverse effects of medical treatment; SDI, sociodemographic index
DALY rates due to AEMT in China, worldwide and in other countries and regions with different SDI levels, 1990–2019
The ASR of DALYs caused by AEMT exhibited a significant downward trend worldwide during 1990–2019. During the study period, the ASR of DALYs for AEMT in China decreased most significantly, from 67.65 (95% UI: 44.17–81.67) in 1990 to 12.33 (95% UI: 10.42–15.77) in 2019, with an ARC of -0.82 (95% UI: -0.86 to -0.70). Although most countries showed a downward trend for AEMT-related ASRs of DALYs, both Japan and Russia presented a trend of initial growth and then a decline but an overall rise. In addition, the SDI strongly influenced the ASRs of DALYs (Table 2; Fig. 2A).
Trends in ASR-DALYs caused by AEMT in China and other regions with different SDIs disaggregated by sex and age, 1990–2019. (A) ASR-DALYs due to AEMT in China, the SDI region, and globally in 1990, 2010 and 2019. (B) Sex differences and trends in ASR-DALYs induced by AEMT in China during 1990–2019. (C) Age difference in ASR-DALYs caused by AEMT between China and regions with SDI levels worldwide. ASR, age-standardized rate; DALYs, disability-adjusted life years; AEMT, adverse effects of medical treatment; SDI, sociodemographic index
In 2019, the global ASR of DALYs due to AEMT was estimated to be slightly greater for women than for men. In China, the ASR of DALYs caused by AEMT changed significantly in terms of sex from 1990 to 2019. Specifically, the female-to-male ratio of the ASR of DALYs in China showed an upward then downward trend, 1998 as the inflection point. Since 2002, there have been more ASRs of DALYs caused by AEMT among Chinese men than among women, and the sex-specific gap has gradually widened (Fig. 2B). In addition, the change trends of DALY rates in China, middle SDI regions and worldwide were roughly the same. Overall, the DALY rate of AEMT was particularly high at early ages and gradually increased for older people (over 65 years of age) after a trough from 10 to 60 years of age (Fig. 2C).
Rates of YLLs and YLDs due to AEMT in China, worldwide and in other countries and regions with different SDI levels, 1990–2019
As shown in Tables 3 and 4; Fig. 3A, from 1990 to 2019, the global ASR-YLLs due to AEMT showed a significant downward trend, and the global ASR-YLDs was almost unchanged. The ASR-YLLs attributed to AEMT was also correlated with the SDI. In general, the higher the SDI was, the lower the ASR-YLLs. Most countries presented a clear downward trend in AEMT related ASR-YLLs; of those, China topped the list with an ARC of -0.83 (95% UI: -0.87 to -0.72).
Comparison of YLL and YLD values caused by AEMT in China and in different SDI regions from 1990 to 2019. (A) Comparison of the ASRs of YLLs and YLDs caused by AEMT in China and SDI regions and globally in 1990, 2010 and 2019. (B) Sex differences and trends in ASR-YLLs and ASR-YLDs caused by AEMT from 1990 to 2019. (C) Age differences in ASR-YLLs and ASR-YLDs caused by AEMT between China and the SDI region. (D) Projected trends based on changes in the global ASR of YLLs due to AEMT from 1990 to 2019, projected to 2040. ASR, age-standardized rate; YLLs, years of life lost; YLDs, years lived with disability; AEMT, adverse effects of medical treatment; SDI, social demographic index
The sex ratio (female:male) of ASR-YLDs due to AEMT remained relatively stable from 1990 to 2019 and was positively correlated with the SDI. Globally, women had higher ASR-YLDs for AEMT than men. This was especially true in China, where the female-to-male ratio of ASR-YLDs due to AEMT fluctuated around 1.20. The sex ratio (female:male) of ASR-YLLs for AEMT was more dispersed than that of ASR-YLDs, and the trend was more similar to that of ASR-DALYs due to AEMT. In 2019, the sex ratio (female:male) of ASR-YLLs in low-middle-SDI regions was 1.23, which was the highest among all the SDI regions, while the ratio in high-SDI regions was the lowest, at only 0.76 (Fig. 3B).
The YLD and YLL rates attributed to AEMT in China, middle-SDI regions and worldwide were relatively high in the 0- to 10-year-old age group, with a significant downward trend. Inconsistent with what was observed globally, the AEMT-related YLD rate in China stabilized and decreased among individuals older than 20 years. Moreover, the global AEMT-related YLL rate increased with age in China and among elderly individuals (over 60 years old) in middle-SDI regions and worldwide. The age distribution trend of the YLL rate attributed to AEMT in China was lower than that worldwide and in middle-SDI regions at any age (Fig. 3C).
It is predicted that the ASR-YLLs due to AEMT will continue to decrease worldwide until 2040. The global ASR-YLLs due to AEMT is predicted to reach 54.7 2 (95% UI: 45.24–63.18) by 2030 and 50.21 (95% UI: 40.71–59.29) by 2040. The ASR-YLLs due to AEMT in China will remain at the lower-middle level, estimated to be 13.43 (95% UI: 10.95–18.40) in 2030 and 10.61 (95% UI: 8.24–14.71) in 2040 (Fig. 3D).
Rates of prevalence and incidence due to AEMT in China, worldwide and in other countries and regions with different SDI levels, 1990–2019
The incidence of ASR due to AEMT showed an upward trend in high-SDI regions, with an ARC of 0.29 (95% UI: 0.24–0.35). During this period, the ASR-incidence attributed to AEMT in China decreased first, from 100.18 (95% UI: 75.53-129.64) in 1990 to 78.81 (95% UI: 57.33-103.66) in 2010, and then rebounded to 100.30 (95% UI: 72.66-133.22) in 2019 (Table 5; Fig. 4A). The female-to-male ratios of the ASR of prevalence and ASR of incidence due to AEMT did not change significantly between 1990 and 2019 across SDI regions. There was a positive correlation between the sex ratio of the ASR of the incidence (female:male) and the SDI. In China, the ASR of the incidence and ASR of the prevalence of AEMT among females were greater than those among males (Fig. 4B). As shown in Fig. 4C, the ASR of the incidence of AEMT in 2019 was high among people younger than 20 years, decreased with age, remained at a very low level between 20 and 50 years of age, and increased among those 50 years and older; moreover, the overall trend was not affected, although there was a slight decrease in the 80–90 age group.
Comparison of the ASR of the incidence and ASR of the prevalence caused by AEMT in China and in different SDI regions from 1990 to 2019. (A) Comparison of the incidence and prevalence of ASR in China and SDI regions and globally in 1990, 2010 and 2019. (B) Sex differences and trends in ASR incidence and ASR prevalence of AEMT from 1990 to 2019. (C) Age differences in ASR incidence and prevalence due to ASR caused by AEMT between China and the SDI region
Discussion
At present, the reporting and management of AEMT in China are still in their infancy. The findings show that the main categories of medical adverse events in China include errors in information delivery, medication administration, and program management. In addition, there are incidents related to care and equipment use [23]. Therefore, the change in ASR-YLDs in China was not obvious, which highlights the challenges in meeting the health needs of economically develo** countries in rapid economic transition.
From 1990 to 2019, the global ASR of the incidence of AEMT exhibited a fluctuating upward trend. Notably, areas with high SDIs had higher morbidity rates and lower mortality rates. This is related to many factors, such as countries and regions with high SDIs having better basic medical systems and more standardized adverse event reporting systems; additionally, medical staff are paying more attention to AEMT, and the public has a deeper understanding of AEMT. The presence of these factors enables high-SDI regions to accurately record the occurrence of AEMT in a timely manner and learn from them to avoid similar incidents.
In contrast to regions with high SDI levels, other SDI regions exhibited a downward then upward trend, as did China. Due to the lack of a complete reporting system in rural medical models, the statistics of the incidence of AEMT are overdependent on the personal behaviors of medical staff [24]. This further leads to large errors and uncertainties in the statistics of AEMT, which are possible reasons why the incidence rate of AEMT decreased dramatically between 1990 and 2010. From 2010 to 2019, the Chinese government paid more attention to national health issues and proposed a new reform plan for the medical and health system in 2009. Through this reform, a four-in-one basic medical and health security system covering the entire population was initially established; this system consists of a medical service system, a public health service system, a drug supply security system and a medical security system [25, 26]. Moreover, China has strengthened its relationships with the WHO to promote international medical cooperation. During this period, China gradually formed a reporting system for AEMT that combined a compulsory reporting system, voluntary reporting system and internal reporting system. In addition, big data play a nonnegligible role in medical adverse event reporting. For example, the use of electronic medical records and artificial intelligence (AI) has led to more complete statistics on adverse medical events among patients [27,28,29,30]. Second, China’s basic medical insurance system was implemented in the early 21st century and has developed rapidly since then. By 2012, China’s rural cooperative medical care coverage had reached 95%. Other medical security systems for urban workers are also making steady progress under the supervision of the government [31]. Finally, with the increase in national economic income and the strengthening of people’s understanding of commercial insurance, an increasing number of people recognize and purchase commercial medical insurance [32, 33]. These factors reduce the ASDR and ASR-DALYs of AEMT but increase the ASR of the incidence of AEMT.
In terms of sex, the ASR of the incidence and prevalence of AEMT among Chinese women were greater than those among men, while the ASDR of AEMT among women was lower than that among men. The female-to-male ratios of ASR-DALYs and ASR-YLLs changed greatly in China during 1990–2019. The high ASR of the incidence and ASR of the prevalence of AEMT among women was because women are more susceptible to adverse drug reactions than men are, and women have a greater probability of accidents during surgery [34]. Some women tend to fall into a negative state after illness. Because men and women are biologically different, women have a greater risk burden during pregnancy and childbirth [35]. Many men are engaged in heavy physical work, and their average life expectancy is shortened. Moreover, smoking, drinking and other unhealthy habits are associated with greater mortality among males than among females [36,37,38]. Since the beginning of the 21st century, the social status of Chinese women has gradually improved, and an increasing number of women have become economically independent. The impact of treatment and rehabilitation burden after accidental injury has also been reduced, which has a great impact on the follow-up treatment of patients. As a result, the ASR-DALYs of Chinese men increased during the observation period.
The incidence of AEMT was highest among children (0–10 years old) in China because their bodies are not mature enough to adapt to the outside world, and their resistance to disease is weak. Surgical and perioperative adverse events, drug dose effects and accidents are the main causes of high mortality [39]. In addition, patients older than 65 years have reduced physical function and a reduced ability to recover after surgery and are more prone to multiple complications, which greatly limits the effectiveness of medications and treatments for older patients [40, 41]. Multiple morbidities is a major challenge facing global health care systems, and the current GBD often fails to account for the co-occurrence of multiple diseases, thus increasing the uncertainty of AEMT data.
Our research has important implications for global health care delivery. This study can not only increase the public’s attention regarding AEMT but also help the government fully utilize its administrative functions, formulate relevant policies and laws, and promote the unified management of an AEMT reporting system. This approach is also conducive to training medical staff on AEMT so that they can respond to adverse events in hospitals in a timely and efficient manner. However, AEMT still faces many problems and challenges, such as how to effectively reduce the occurrence of AMET and how to reduce the harm caused by AEMT as soon as possible.
Based on GBD data and China’s actual development experience, we summarize the concerns and challenges of addressing the AEMT burden in China from 1990 to 2019. This research has certain limitations. First, the data relied on secondary information obtained from the GBD study rather than from the clinical setting. Second, each country and region have different criteria for classifying adverse events, and these factors may fundamentally affect our results. Third, the basic public facilities in some economically underdeveloped areas are not perfect, and the reporting consciousness of medical staff is not sound, resulting in large errors in the statistical data. Finally, the cause classification system of the GBD study classifies each death as a single root cause, which can lead to some events related to AEMT that may be classified elsewhere.
Conclusions
From 1990 to 2019, the world experienced rapid social and economic changes, medical conditions in countries and regions greatly improved, and medical systems gradually improved. Much progress has been made globally in reducing the ASDRs and ASR-DALYs caused by AEMT, but some countries with rapidly changing economies have yet to achieve effective results in reducing the incidence of AEMT. The same is true of China. This requires countries to continuously strengthen the reform of the AEMT reporting system and governments and relevant personnel to pay more attention to AEMT and take effective measures to reduce the occurrence of AEMT.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AEMT:
-
adverse effects of medical treatment
- ARC:
-
annual rate of change
- ASDR:
-
age-standardized death rate
- ASR:
-
age-standardized rate
- DALYs:
-
disability-adjusted life years
- YLDs:
-
years lived with disability
- YLLs:
-
years of life lost
- GBD:
-
Global Burden of Disease
- ICD:
-
International Classification of Diseases
- SDI:
-
sociodemographic index
- UI:
-
uncertainty interval
- WHO:
-
World Health Organization
References
Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med. 1991;324(6):370–6.
de Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA. The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care. 2008;17(3):216–23.
Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016;353:i2139.
MA Xudong. The classification of adverse events on Medical Quality and Safety in China. Chin Health Qual Manage 2021, 28(06).
Lunevicius R, Haagsma JA. Incidence and mortality from adverse effects of medical treatment in the UK, 1990–2013: levels, trends, patterns and comparisons. Int J Qual Health Care. 2018;30(7):558–64.
Wilson RM, Michel P, Olsen S, Gibberd RW, Vincent C, El-Assady R, Rasslan O, Qsous S, Macharia WM, Sahel A, et al. Patient safety in develo** countries: retrospective estimation of scale and nature of harm to patients in hospital. BMJ. 2012;344:e832.
Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: WHO’s Third Global Patient Safety Challenge. Lancet. 2017;389(10080):1680–1.
Xue Y, Yang J, Zhang J, Luo M, Zhang Z, Liang H. Motivating Physicians to report adverse medical events in China: Stick or Carrot? J Patient Saf. 2021;17(5):e455–61.
Schwendimann R, Blatter C, Dhaini S, Simon M, Ausserhofer D. The occurrence, types, consequences and preventability of in-hospital adverse events - a sco** review. BMC Health Serv Res. 2018;18(1):521.
Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T, et al. GBD 2010: design, definitions, and metrics. Lancet. 2012;380(9859):2063–6.
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 Diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88.
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49.
Li Y, Zhang J. Disease burden and risk factors of Ischemic Heart Disease in China during 1990–2019 based on the global burden of Disease 2019 report: a systematic analysis. Front Public Health. 2022;10:973317.
Foreman KJ, Lozano R, Lopez AD, Murray CJ. Modeling causes of death: an integrated approach using CODEm. Popul Health Metr. 2012;10:1.
Haagsma JA, James SL, Castle CD, Dingels ZV, Fox JT, Hamilton EB, Liu Z, Lucchesi LR, Roberts NLS, Sylte DO, et al. Burden of injury along the development spectrum: associations between the socio-demographic index and disability-adjusted life year estimates from the global burden of Disease Study 2017. Inj Prev. 2020;26(Supp 1):i12–i26.
**ong R, Bi XY. Analysis and countermeasures of 1, 117 medical adverse events in a certain General Hospital. Jiangsu Healthc Adm 2022, 05.
Wang L, Wang Z, Ma Q, Fang G, Yang J. The development and reform of public health in China from 1949 to 2019. Global Health. 2019;15(1):45.
Zhang D, Unschuld PU. China’s barefoot doctor: past, present, and future. Lancet. 2008;372(9653):1865–7.
Shi L. Health care in China: a rural-urban comparison after the socioeconomic reforms. Bull World Health Organ. 1993;71(6):723–36.
Lee K. Health policy in Asia and the Pacific: navigating local needs and global challenges. Asia Pac Policy Stud. 2014;1(1):45–57.
Mor N. Lessons for develo** Countries from Outlier Country Health systems. Front Public Health. 2022;10:870210.
Li X, Zhang S, Chen R, Gu D. Hospital climate and peer report intention on adverse medical events: role of attribution and rewards. Int J Environ Res Public Health 2021, 18(5).
Yip WC, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379(9818):833–42.
Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R, Pan J, Hu M, Zhou Z, Chen Q, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–204.
Williams F, Boren SA. The role of the electronic medical record (EMR) in care delivery development in develo** countries: a systematic review. Inf Prim Care. 2008;16(2):139–45.
Ahuja AS. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ. 2019;7:e7702.
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, Wang Y, Dong Q, Shen H, Wang Y. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43.
Uslu A, Stausberg J. Value of the Electronic Medical Record for Hospital Care: Update from the literature. J Med Internet Res. 2021;23(12):e26323.
Yi H, Zhang L, Singer K, Rozelle S, Atlas S. Health insurance and catastrophic Illness: a report on the New Cooperative Medical System in rural China. Health Econ. 2009;18(Suppl 2):119–27.
Choi WI, Shi H, Bian Y, Hu H. Development of Commercial Health Insurance in China: a systematic literature review. Biomed Res Int. 2018;2018:3163746.
Xu BC, Li XJ, Gao MY. Influence of Commercial Insurance Purchase on the Health Status of Chinese residents. Front Public Health. 2021;9:752530.
Zopf Y, Rabe C, Neubert A, Janson C, Brune K, Hahn EG, Dormann H. Gender-based differences in drug prescription: relation to adverse drug reactions. Pharmacology. 2009;84(6):333–9.
McCauley M, Zafar S, van den Broek N. Maternal multimorbidity during pregnancy and after Childbirth in women in low- and middle-income countries: a systematic literature review. BMC Pregnancy Childbirth. 2020;20(1):637.
Chen Z, Peto R, Zhou M, Iona A, Smith M, Yang L, Guo Y, Chen Y, Bian Z, Lancaster G, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386(10002):1447–56.
Hesselbrock MN, Hesselbrock VM, Chan G, Del Boca F, Chartier K. Subtypes of Alcohol Dependence and 36-Year mortality. Alcohol Clin Exp Res. 2020;44(8):1658–65.
Wilsnack RW, Wilsnack SC, Gmel G, Kantor LW. Gender differences in binge drinking. Alcohol Res. 2018;39(1):57–76.
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–20.
Szlejf C, Farfel JM, Curiati JA, Couto Ede B Jr., Jacob-Filho W, Azevedo RS. Medical adverse events in elderly hospitalized patients: a prospective study. Clin (Sao Paulo). 2012;67(11):1247–52.
Leape LL, Brennan TA, Laird N, Lawthers AG, Localio AR, Barnes BA, Hebert L, Newhouse JP, Weiler PC, Hiatt H. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–84.
Acknowledgements
We appreciate the great work of the Global Burden of Disease Study 2019 collaborators.
Funding
This study was supported by research projects established by the Chinese Pharmaceutical Association Hospital Pharmacy Department (No. CPA-Z05-ZC-2022-002), the Liaoning Provincial Department of Science and Technology Applied Basic Research Program Project (No. 2023JH2/101300101) and the Science and Technology Talent Innovation Foundation of Dalian (No. 2022RY16).
Author information
Authors and Affiliations
Contributions
X.K., X.T., and D.D. designed the study and wrote the manuscript. X.K., L.L., and Y.L. collected and analyzed the data. X.Z., J.R., and S.Y. performed the statistical analysis. X.K., X.C., H.X., G.W., and D.D. edited the manuscript and provided valuable suggestions for study design and data analysis. All authors have approved the final version of this paper.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, X., Tao, X., Li, L. et al. Global trends and partial forecast of adverse effects of medical treatment from 1990 to 2019: an epidemiological analysis based on the global burden of disease study 2019. BMC Public Health 24, 295 (2024). https://doi.org/10.1186/s12889-023-17560-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17560-0