Abstract
Background
The Basic Public Health Service (BPHS), a recently announced free healthcare program, aims to combat the most prevalent Noncommunicable Disease-“Hypertension” (HTN)-and its risk factors on a nationwide scale. In China, there is a rife that HTN less impacts women during their lifetime. We, therefore, aimed to evaluate the sex disparity in hypertension patients with comorbidities among south-west Chinese and the contribution of BPHS to address that concern.
Methods
We have opted for a multistage stratified random sampling method to enroll hypertensive patients of 35 years and older, divided them into BPHS and non-BPHS groups. We assessed the sex disparity in HTN patients with four major comorbidities- Dyslipidemia, Diabetes Mellitus (DM), Cardiovascular Disease (CVD), and Chronic Kidney Disease (CKD), and descriptive data were compiled. Odds ratios from logistic regression models estimated the effectiveness of BPHS in the management of HTN with comorbidities.
Results
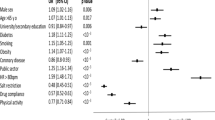
Among 1521 hypertensive patients,1011(66.5%) were managed in the BPHS group. The proportion of patients who had at least one comorbidity was 70.7% (95% confidence interval [CI]: 66.3-76.8%), patients aged 65 years and older were more likely to have coexisting comorbidities. Participants who received the BPHS showed significant blood pressure (BP) control with two comorbidities (odds ratio [OR] = 2.414, 95% CI: 1.276–4.570), three or more (OR = 5.500, 95%CI: 1.174–25.756). Patients with dyslipidemia and DM also benefited from BPHS in controlling BP (OR = 2.169, 95% CI: 1.430–3.289) and (OR = 2.785, 95%CI: 1.242–6.246), respectively. In certain high-income urban survey centers, there was sex differences in the HTN management provided by BPHS, with men having better BP control rates than women.
Conclusions
Perhaps this is the first study in China to succinctly show the effectiveness and sex disparity regarding “management of hypertensive comorbidities”. This supports that the BPHS program plays a pivotal role in controlling BP, therefore should recommend the national healthcare system to give women a foremost priority in BPHS, especially to those from low-socioeconomic and low-scientific literacy regions.
Similar content being viewed by others
Introduction
Hypertension (HTN) is a major modifiable risk factor and a leading cause of mortality and premature deaths among the NCD’S [1–2]. It is reported that more than 1 billion people are affected globally [3]. Managing HTN is a significant public health concern [4]. The prevalence of HTN is increasing in low and middle-income countries (LMICs) than in high-income countries [3,4,5].
China has approximately 245 million HTN patients, with treatment and control rates of only 40.7% and 15.3%, respectively [6]. HTN is not only a risk factor for many unfavorable clinical outcomes but also has an adverse effect on other conditions like diabetes mellitus (DM), chronic kidney disease (CKD), cardiovascular diseases (CVD), stroke, and loss of cognitive function [7,8,9,10]. Therefore, even modest improvements in the management of raised BP might have a significant long-term positive impact, especially in patients with underlying comorbid conditions [7]. It is reported that two-thirds of hypertensive patients had underlying comorbidities such as DM, CKD, CVD, and dyslipidemia [11].
BP is not only diurnal [12–13] but also a dimorphic variable that can change at different rates in males and females throughout their life span [13–14]. These variations are caused by a combination of genetically (sex-related) and psychosocially (gender-related) determined variables [15–16], but overall, men are more likely to have other coexisting conditions in China [17]. The prevalence of HTN differs between males and females with comorbidities, as does their awareness of the condition [6, 18,19,20,21]. Sex disparities in the treatment of HTN with comorbidities, however, have not received enough consideration [22–23]. Sex disparities in HTN care, which have been overlooked, would hinder the Sustainable Development Goal (SDGs) of reducing non-communicable diseases (NCDs) mortality by one-third [24–25]. It would be challenging to reach SDG’s goal of 3.0 in Yunnan Province (a low-income region in south-west China) [26].
Based on the American College of Cardiology (ACC)/American Heart Association (AHA) hypertension guidelines [27] and the Chinese guidelines [6).
Supplementary file 7 shows the BP control rate in men and women with coexisting comorbidities in all eight study centers. Both male and female participants with dyslipidemia, CVD, CKD, and DM experienced a higher rate of BP control in the BPHS group than in the non-BPHS group. Despite having four comorbidities, men from the urban areas of “Guandu” (Fig. 1G in Supplementary file 7) and “Mengzi” (Fig. 1D in Supplementary file 7) in the BPHS group had a higher control rate than female patients.
Discussion
This study explored the effectiveness of BPHS policy in reducing HTN among those with pre-existing long-term comorbidities. Also, it revealed whether women and men benefited equally from BPHS policy. We presented the findings of a survey associated with the BPHS program to analyze BP control in hypertensive patients with comorbidities. We found that 70.7% (1076/1521) of HTN patients had at least one coexisting comorbidity, which was higher than the percentage found in studies from Hong Kong (47.4%) [57] and the UK (51.0%) [58].
Dyslipidemia was the primary comorbidity for the majority of the participants (43.7%), followed by CKD (35.5%), which is consistent with the fact that dyslipidemia was the most prevalent comorbidity in the Chinese hypertensive population (about 41.3%) [59–60]. HTN combined with hypercholesterolemia has become the most important risk factor for ischemic heart disease mortality among Chinese residents [61]. HTN has resulted in 32.75 million disability-adjusted life years in entire China [62]; hypertensive patients with low socioeconomic status, low health literacy, and having lower access to medical services [63] require considerable health resource input, especially in south-west China, where the population is aging in a higher rate. Attention was deemed necessary in the interim since China has the highest proportion of CKD patients in Asia (up to 159.8 million) [64].
ISH [7] and ACC guidelines [27] recommend lifestyle intervention for CVD prevention and non-pharmacological treatment of hypertensive comorbidities as an effective means to lower BP. Consistent with ISH and ACC guidelines, the Chinese national standards for BPHS (the third edition) [31] recommend primary healthcare providers to create personalized models of lifestyle modification for hypertensive patients, to supervise and track constantly, to provide patient counseling, and to encourage patients to follow the recommended lifestyle changes consistently. Thus, lifestyle modification was included as an essential component of managing hypertensive patients [28, 31, 65]. This study found that a higher percentage of male hypertensive patients with comorbidities in the BPHS group received services related to salt reduction instruction (BPHS 89.6% vs. non-BPHS 82.6%), alcohol consumption reduction (87.8% vs.81.5%), and stress reduction guidance (81.8% vs. 73.7%). It is observed that the more the primary healthcare practitioners provided health education and lifestyle modifications to patients, the more it enhanced health awareness, helped in BP control, and encouraged people to adopt a better lifestyle [66–67].
This study also found that BPHS group patients with comorbidities had a higher proportion of taking a single drug (BPHS group 54.3% vs. non-BPHS group 37.2%) or combination of drugs (17.3% vs. 8.6%) than those in the non-BPHS group, which is in line with a report stating that HTN patients with comorbidities typically took more medications for a longer period of time to manage their blood pressure [7, 29]. ‘Consistency’ could be the key to effectively controlling BP in comorbid patients in the BPHS group. A patient-centered approach to clinical practice and the use of herbal medications were linked to optimum BP control in earlier studies, which may offer guidance for future BPHS policy amendments [68–69].
Moreover, our study observed lower DBP and SBP in the BPHS group, regardless of the different types of comorbidities or accumulated comorbidities. As hypertensive dyslipidemia or DM, patients were 2.169 times and 2.785 times more likely to receive BPHS management, respectively, and a similar trend was observed in patients with comorbidities clusters. The above findings further provided sufficient evidence that BPHS can effectively manage HTN with comorbidities in the low-income provinces of south-west China. However, the adjusted model from HTN patients with CKD was not statistically significant (p > 0.05), and the results imply that “anti-hypertensive medication” appears to be a substantial and important predictor of BP control, which detracts from/influences the potential association between the independent variable (BPHS management) and the dependent variable (BP control). It is evident that the BPHS management system should be a priority consideration for hypertensive patients with comorbid CKD. Unlike the current clinical practice recommendations, which primarily address managing HTN from a single comorbidity [70], our findings support the trend among primary healthcare providers to monitor BP and assess risks to manage the targeted BP better and provide high-quality services, as per international guidelines for the treatment of hypertensive patients with multiple and accumulated comorbidities.
In addition, this study demonstrated that, compared to the non-BPHS group, the BPHS care group was beneficial in lowering SBP and DBP with multiple comorbidities in both sex. In some high-income urban survey centers, men appeared more likely to have their BP well under control. Previous studies from Denmark and the United States have reported differences in BP control rates depending on the presence of different diseases in men as compared to women [53, 71]. Current HTN recommendations give sex disparity relatively minimal consideration [23, 72]. Therefore, national health initiatives like BPHS must consider this inequality. This can be achieved by providing additional BPHS resources, particularly in areas with limited access to female patients with multiple comorbidities.
The study reveals that BPHS would significantly contribute to the ‘targeted BP control’ among patients with comorbidities and encourage them to adhere to BPHS-assisted lifestyle changes. Furthermore, by imparting the most recent information and experience, it would benefit prospective policies in LMIC regions.
Limitation
The results could have been impacted by the duration and occurrence of CKD, CVD, and DM, but we did not validate this interdependency in this study. The relationship between BPHS management and BP control should be evaluated cautiously due to the limitations imposed by the cross-sectional study methodology. Secondly, the efficiency of HTN management could have been unintentionally underestimated in hypertensive patients with comorbidities (1, 2, 3, or more comorbidities) owing to the short duration of BPHS services provided. Thirdly, this study identified four comorbidities as the most prevalent comorbidities (dyslipidemia, DM, CKD, CVD) in the Chinese populace, and thus only these four were considered in inclusion criteria, and minor comorbidities like Gout, rheumatic changes, dementia, and tumors were excluded from the study. Due to a very small sample size of patients in the group with four major comorbidities in some survey centers attributed to a lack of ‘scientific literacy’ in general, therefore both BPHS and non-BPHS enrollment trajectories declined significantly. This is inexorably shown on individual study center maps, which presents as extreme values of cases with control rates of “0 “or “100”, especially “Anning” study center (see Supplementary file 7).
Our recommendations to health policymakers are: (a) Future prospective cohort studies should consider enrolling a larger sample size, as doing so could help to better assess the effectiveness of BPHS in lowering BP, reducing related disability, and preserving medical and health resources in hypertension patients with complications. (b) NCD’s awareness camps should be conducted prior to study, as centers like “Anning” seems to lack ‘scientific literacy’ in general. (c) Furthermore, an emphasis on extensive research is necessary to comprehend the mechanisms by which sex influences the onset of HTN and vascular aging, as well as how this correlation can help in the early prevention of other comorbid conditions. (d) Due to the constant changes in the guidelines [73] for treating HTN, there should be an introduction of Chinese HTN education program recommendations for the management of hypertension, which should be taught to healthcare providers on a regular basis. (e) By collaborating with other Asian societies of HTN [74–75] and sharing knowledge with international committees working on HTN, it is essential to develop a HTN treatment specifically tailored to suit the Chinese race.
Conclusion
This study evaluated the community-based Chinese BPHS program for effectively managing male and female hypertensive patients with comorbidities and found that almost two-thirds of the hypertensive patients have comorbidity in Yunnan Province. The BPHS program also successfully encouraged healthy lifestyle changes, lowered DBP and SBP, and improved BP control in HTN patients with various comorbidities. However, we also observed that male patients with HTN seemed to benefit more from BPHS than women. For the first time in China, this study results call for better management strategies and allocation of health care resources for chronic diseases, especially to women in older age group.
Data Availability
The data supporting the findings of this study and its supplementary material are available on reasonable request from the project administrator/principal corresponding author (LD).
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- BPHS:
-
Basic public health services
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CVD:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- HDL-C:
-
High-density lipoprotein cholesterol
- HTN:
-
Hypertension
- LDL-C:
-
Low-density lipoprotein cholesterol
- LMICs:
-
Low and middle-income countries
- NCD:
-
Non-communicable diseases
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1223–49.
Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2019;394(10204):1145–58.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in Hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–80.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and Hypertension. Nat Rev Cardiol. 2021;18(11):785–802.
Schutte AE, SrinivasapuraVenkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in low- and Middle-Income Countries. Circ Res. 2021;128(7):808–26.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of Hypertension in China: results from the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344–56.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334–57.
Alsaadon H, Afroz A, Karim A, Habib SH, Alramadan MJ, Billah B, et al. Hypertension and its related factors among patients with type 2 Diabetes Mellitus - a multi-hospital study in Bangladesh. BMC Public Health. 2022;22(1):198.
Shrestha PL, Shrestha PA, Vivo RP. Epidemiology of comorbidities in patients with Hypertension. Curr OpinCardiol. 2016;31(4):376–80.
Chen Y, Zhou ZF, Han JM, ** X, Dong ZF, Liu L, et al. Patients with comorbid coronary artery Disease and Hypertension: a cross-sectional study with data from the NHANES. Ann Transl Med. 2022;10(13):745.
Kennard L, O’Shaughnessy KM. Treating Hypertension in patients with medical comorbidities. BMJ. 2016;352:i101.
Narita K, Hoshide S, Kario K. Difference between morning and evening home blood pressure and cardiovascular events: the J-HOP study (Japan Morning Surge-Home blood pressure). Hypertens Res. 2021;44(12):1597–605.
Kario K, Ishikawa J, Pickering TG, Hoshide S, Eguchi K, Morinari M, et al. Morning Hypertension: the strongest Independent risk factor for Stroke in Elderly Hypertensive patients. Hypertens Res. 2006;29(8):581–7.
Hoshide S, Kubota K, Kario K. Difference between morning and evening blood pressure at home and nocturnal hypoxia in the general practitioner-based. J-HOP Study Hypertens Res. 2023;46(3):751–5.
Xu Y, Möller J, Wang R, Liang Y. Life-course blood pressure trajectories and Cardiovascular Diseases: a population-based cohort study in China. PLoS ONE. 2020;15(10):e0240804.
Connelly PJ, Currie G, Delles C. Sex differences in the prevalence, outcomes and Management of Hypertension. CurrHypertens Rep. 2022;24(6):185–92.
Wang J, Ma JJ, Liu J, Zeng DD, Song C, Cao Z. Prevalence and risk factors of comorbidities among hypertensive patients in China. Int J Med Sci. 2017;14(3):201–12.
Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart Disease and Stroke Statistics-2021 update: a Report from the American Heart Association. Circulation. 2021;143(8):e254–e743.
DeGuire J, Clarke J, Rouleau K, Roy J, Bushnik T. Blood pressure and Hypertension. Health Rep. 2019;30(2):14–21.
Neufcourt L, Deguen S, Bayat S, Paillard F, Zins M, Grimaud O. Geographical variations in the prevalence of hypertensionin France: cross-sectional analysis of the CONSTANCES cohort. Eur J PrevCardiol. 2019;26(12):1242–51.
Fenech G, Vallée A, Cherfan M, Kab S, Goldberg M, Zins M, et al. Poor awareness of Hypertension in France: the CONSTANCES Population-based study. Am J Hypertens. 2020;33(6):543–51.
Connelly PJ, Azizi Z, Alipour P, Delles C, Pilote L, Raparelli V. The importance of gender to Understand Sex differences in Cardiovascular Disease. Can J Cardiol. 2021;37(5):699–710.
Song J-J, Ma Z, Wang J, Chen L-X, Zhong J-C. Gender differences in Hypertension. J Cardiovasc Transl Res. 2020;13(1):47–54.
Cao B, Bray F, Ilbawi A, Soerjomataram I. Effect on longevity of one-third reduction in premature mortality from non-communicable Diseases by 2030: a global analysis of the sustainable development goal health target. Lancet Glob Health. 2018;6(12):e1288–96.
Redfern A, Peters SAE, Luo R, Cheng Y, Li C, Wang J, et al. Sex differences in the awareness, treatment, and control of hypertensionin China: a systematic review with meta-analyses. Hypertens Res. 2019;42(2):273–83.
Chen S, Guo L, Wang Z, Mao W, Ge Y, Ying X, et al. Current situation and progress toward the 2030 health-related Sustainable Development Goals in China: a systematic analysis. PLoS Med. 2019;16(11):e1002975.
Whelton PK, Carey RM, Aronow WS, Casey DEJr, Collins KJ, Dennison Himmelfarb C, ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH et al. /ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248.
Bureau of Disease Prevention and Control. National Health Commission of people’s Republic of China. National guideline for Hypertension management in China. Zhonghua **n xue guan bing za zhi. 2020;48:10–46.
Joint Committee for Guideline R. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16(3):182–241.
Li X, Lu J, Hu S, Cheng KK, De Maeseneer J, Meng Q, et al. The primary healthcare system in China. The Lancet. 2017;390(10112):2584–94.
Ministry of Health. National guideline of basic public health services (Third Edition). 2017. http://wjw.bei**g.gov.cn/wjwh/ztzl/ggwsfw/201912/P020191217743891499573.pdf. Accessed 25 Mar 2023.
Hao G, Chen Z, Wang X, Zhang L, Kang Y, Zheng C, et al. Evaluation of the community-based Hypertension Management Programs in China. Front Public Health. 2022;10:896603.
Pang L, Kottu L, Guo Z, Shi Y, Ferdous M, Zhao Y, et al. Dawning public health services dogma: an indigenous South-West Chinese perspective in managing hypertension-with or without the BPHS? Front Public Health. 2022;10:1017795.
Liang X, Chen J, Liu Y, He C, Li T. The effect of Hypertension and Diabetes management in South-West China: a before- and after-intervention study. PLoS ONE. 2014;9(3):e91801.
Yan C, Yuan Y, Zhao D, Li J, Fu P, Chen Y, et al. Family Doctor Contract services and awareness of blood pressure measurement among Hypertension patients: a cross-sectional study in rural Shandong, China. Front Public Health. 2022;10:757481.
Zheng X, **ao F, Li R, Yin D, **n Q, Yang H, et al. The effectiveness of Hypertension management in China: a community-based intervention study. Prim Health Care Res Dev. 2019;20:e111.
Fang G, Yang D, Wang L, Wang Z, Liang Y, Yang J. Experiences and Challenges of Implementing Universal Health Coverage with China’s National Basic Public Health Service Program: Literature Review, Regression Analysis, and Insider interviews. JMIR Public Health Surveill. 2022;8(7):e31289.
Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2021;1(1):Cd006560.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, et al. The association between Smoking and blood pressure in men: a cross-sectional study. BMC Public Health. 2017;17(1):797.
Li Z, Yu S, Han X, Liu J, Yao H. Changes to cardiovascular risk factors over 7 years: a prospective cohort study of in situ urbanised residents in the Chaoyang District of Bei**g. BMJ Open. 2020;10(3):e033548.
Zhou BF. Predictive values of body mass index and waist circumference for risk factors of certain related Diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic Kidney Disease. J Am Soc Nephrol. 2006;17(10):2937–44.
Hoshide S, Mogi M, Kario K. The next stage of Hypertension management in Asia. Hypertens Res. 2022;45(10):1552.
Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. Management of Hypertension: summary of NICE guidance. BMJ. 2011;343:d4891.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial Hypertension: the Task Force for the management of arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31:1281–357.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of Hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3–15.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of High Blood Pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Ghazi L, Oparil S. Impact of the SPRINT Trial on Hypertension Management. Annu Rev Med. 2018;69:81–95.
Nilsson P. What is the optimal blood pressure in patients with Diabetes Mellitus? Am J Cardiovasc Drugs. 2001;1(3):173–7.
Herberth J, Soliman KM, Fülöp T, Basile JN. How we got where we are in blood pressure targets. Curr Hypertens Rep. 2021;23(6):33.
Chen L, Tonkin AM, Moon L, Mitchell P, Dobson A, Giles G, et al. Recalibration and validation of the SCORE risk chart in the Australian population: the AusSCORE chart. Eur J Cardiovasc Prev Rehabil. 2009;16(5):562–70.
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal Cardiovascular Disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003.
Paulsen MS, Andersen M, Thomsen JL, Schroll H, Larsen PV, Lykkegaard J, et al. Multimorbidity and blood pressure control in 37 651 hypertensive patients from Danish general practice. J Am Heart Assoc. 2012;2(1):e004531.
Joint committee for guideline r. 2016 Chinese guidelines for the management of dyslipidemia in adults. J GeriatrCardiol. 2018;15(1):1–29.
Chinese Diabetes Society. National guidelines for the prevention and control of Diabetes in primary care. ZhonghuaNeiKe Za Zhi. 2018;57:885–93.
Kidney Disease. Improving global outcomes (KDIGO) Diabetes Work Group.KDIGO 2022 Clinical Practice Guideline for Diabetes Management in chronic Kidney Disease. Kidney Int. 2022;102(5s):1–s127.
Li YT, Wang HHX, Liu KQL, Lee GKY, Chan WM, Griffiths SM, et al. Medication adherence and blood pressure control among hypertensive patients with coexisting long-term conditions in primary care settings: a cross-sectional analysis. Med (Baltim). 2016;95(20):e3572.
Sarkar C, Dodhia H, Crompton J, Schofield P, White P, Millett C, et al. Hypertension: a cross-sectional study of the role of multimorbidity in blood pressure control. BMC Fam Pract. 2015;16:98.
Hypertensive Group of Chinese Society of Cardiology of Chinese Medical Association. Editorial Board of Chinese Journal of Cardiology.Expert consensus on the comprehensive management of blood pressure and dyslipidemia in Chinese hypertensive patients. Zhonghua **n xue guan bing za zhi. 2021;49:554–63.
**ng L, **g L, Tian Y, Yan H, Zhang B, Sun Q, et al. Epidemiology of dyslipidemia and associated cardiovascular risk factors in northeast China: a cross-sectional study. NutrMetab Cardiovasc Dis. 2020;30(12):2262–70.
Zhang G, Yu C, Zhou M, Wang L, Zhang Y, Luo L. Burden of ischaemic Heart Disease and attributable risk factors in China from 1990 to 2015: findings from the global burden of Disease 2015 study. BMC Cardiovasc Disord. 2018;18(1):18.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global Burden of Hypertension and systolic blood pressure of at least 110 to 115 mm hg, 1990–2015. JAMA. 2017;317(2):165–82.
Li X, Cai L, Cui WL, Wang XM, Li HF, He JH, et al. Association of socioeconomic and lifestyle factors with chronic non-communicable Diseases and multimorbidity among the elderly in rural south-west China. J Public Health (Oxf). 2020;42(2):239–46.
Liyanage T, Toyama T, Hockham C, Ninomiya T, Perkovic V, Woodward M et al. Prevalence of chronic Kidney Disease in Asia: a systematic review and analysis. BMJ Glob Health. 2022;7(1).
Ministry of Health, Treasury Department, State Administration of Traditional Chinese Medicine. Announcement on the national basic public health service project in 2016. http://www.nhfpc.gov.cn/jws/s3577/201606/f29a4659c7f4455ca6f62f8d14eb4b02.shtml.Accessed 25 Mar 2023.
Zhang R, Chen Y, Liu S, Liang S, Wang G, Li L, et al. Progress of equalizing basic public health services in South-West China— health education delivery in primary healthcare sectors. BMC Health Serv Res. 2020;20(1):247.
Zhou T, Wang Y, Zhang H, Wu C, Tian N, Cui J, et al. Primary care institutional characteristics associated with Hypertension awareness, treatment, and control in the China PEACE-Million persons Project and primary healthcare survey: a cross-sectional study. Lancet Glob Health. 2023;11(1):e83–e94.
Buawangpong N, Pinyopornpanish K, Jiraporncharoen W, Dejkriengkraikul N, Sagulkoo P, Pateekhum C, Angkurawaranon C. Incorporating the patient-centered approach into clinical practice helps improve quality of care in cases of Hypertension: a retrospective cohort study. BMC Fam Pract. 2020;21(1):108.
Thangsuk P, Pinyopornpanish K, Jiraporncharoen W, Buawangpong N, Angkurawaranon C. Is the Association between Herbal Use and blood-pressure control mediated by Medication Adherence? A cross-sectional study in primary care. Int J Environ Res Public Health 2021, 18(24).
Skou ST, Mair FS, Fortin M, Guthrie B, Nunes BP, Miranda JJ, et al. Multimorbidity Nat Rev Dis Primers. 2022;8(1):48.
Gu Q, Burt VL, Paulose-Ram R, Dillon CF. Gender differences in Hypertension treatment, drug utilization patterns, and blood pressure control among US adults with Hypertension: data from the National Health and Nutrition Examination Survey 1999–2004. Am J Hypertens. 2008;21(7):789–98.
Griffin BL, Bolch CA, Bourjeily G, Madsen TE, Hasnain M, McGregor AJ, et al. Hypertension: are current guidelines inclusive of sex and gender? J Womens Health (Larchmt). 2022;31(10):1391–6.
Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH, Kenerson JG, et al. Clinical practice guidelines for the management of Hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;16(1):14–26.
Hoshide S, Mogi M, Kario K. Current status of Hypertension and treatment in Asia. Hypertens Res. 2022;45(7):1095–6.
Kario K, Mogi M, Hoshide S. Latest Hypertension research to inform clinical practice in Asia. Hypertens Res. 2022;45(4):555–72.
Acknowledgements
The authors thank the National Center for Cardiovascular Diseases for providing the overall program design and planning. The authors also thank the Yunnan Provincial Health Commission for the electronic Basic Public Health Service program data and the coordination of multiple departments at each surveillance site. We also thank Bei**g Woodpecker Cloud Health Technology Co., Ltd for their technical support during data collection. We also thank all the health workers, nurses, paramedics, volunteers, caregivers, supporters, and researchers who took part in this project.
Funding
This study was funded by building a joint laboratory for important chronic and epidemic diseases in South and Southeast Asia (Grant No. 202103AF140002); Yunnan Provincial Clinical Research Center for Cardiovascular Diseases-New Technology Research and Development Project for Diagnosis and Treatment of Major Cardiovascular Diseases (Grant No. 202102AA310002); Research and Application of Epidemiology, Pathogenesis, Diagnosis and Treatment of Cardiovascular Diseases in High Altitude of Yunnan Province Project (Grant No.202103AC100004).
Author information
Authors and Affiliations
Contributions
LP and LK were co-first authors and drafted the manuscript. MF, ZG and LH initiated, conceived, and supervised the study. LD, DM, WL and YZ guided the analysis and modified the article. LP, MM and HW were involved in data curation and analysis. MT, YS and XW completed field execution and coordinated all divisions. JS and MS checked the integrity of the data. LK and DM reviewed and edited the manuscript. LD conceptualized, and supervised this project. All authors have read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the Ethics Review Boards of National Center for Cardiovascular Disease (approval number: 2020 − 1360, approval date: August 11, 2020), and informed consent and electronic signatures were obtained on-site for all participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pang, L., Kottu, L., Guo, Z. et al. A tryst of ‘blood pressure control- sex- comorbidities’: the odyssey of basic public health services in Yunnan in quest for truth. BMC Public Health 24, 490 (2024). https://doi.org/10.1186/s12889-023-17157-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17157-7