Abstract
Background
Neutropenia is a noteworthy side effect of clozapine, which might warrant this drugs’ discontinuance for safety. Studies have revealed that the risk of neutropenia increases with concurrent administration of valproate, but the evidence was limited. Conversely, lithium may have an ameliorating effect on clozapine-induced neutropenia. This study explored the effects of valproate and lithium on white blood cell counts in patients treated with clozapine.
Methods
We retrospectively investigated the electronic medical records from one tertiary psychiatric hospital in Taiwan and enrolled patients discharged between January 1, 2006, and December 31, 2017, with clozapine prescriptions. We scrutinized their demographic data, medications, and hematological results at discharge and during follow-up outpatient clinic visits over the subsequent 3 years. Patients were classified into four groups: clozapine only (CLO), clozapine and valproate (CLO + VAL), clozapine and lithium (CLO + Li), and clozapine, valproate, and lithium (CLO + VAL + Li). We also identified hematological events (neutropenia or leukocytosis) of these patients during outpatient follow-ups.
Results
Of the included 1084 patients, 55(5.1%) developed neutropenia. Concurrent valproate use (odds ratio [OR] = 3.49) and older age (p = .007) were identified as risk factors. Moreover, 453 (41.79%) patients developed leukocytosis. Younger age; male sex; and concurrent use of lithium (OR = 3.39, p < .001), clozapine daily dosage, and benzodiazepines were the risk factors for leukocytosis.
Conclusion
Concurrent valproate use and older age are associated with the development of neutropenia in patients treated with clozapine. Concurrent lithium usage, younger age, male sex, and concurrent benzodiazepine use might be related to leukocytosis.
Similar content being viewed by others
Introduction
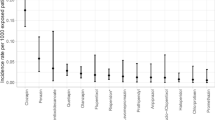
Clozapine, a second-generation antipsychotic (SGA), is the most effective antipsychotic for treatment-refractory schizophrenia (TRS) [1, 2], especially in reducing positive psychotic symptoms [1]. Approximately 30% of patients with schizophrenia respond poorly to antipsychotics and are thus clinically categorized as TRS [3]. Clozapine is well-known for its neutropenic side effects. Among the clozapine-induced adverse drug reactions, neutropenia is particularly dangerous because it may eventually develop into agranulocytosis, a potentially life-threatening condition due to high risk of infection [4]. The prevalence of neutropenia (absolute neutrophil count [ANC] < 1500/mL or white blood count [WBC] < 3000) and agranulocytosis (ANC < 500/mL) caused by clozapine was determined to be 2–3% and 0.4%-0.7%, respectively [5, A total of 1084 patients were included in our analysis. Among them, 796 (73.4%) patients were diagnosed with schizophrenia, 149 (13.7%) with schizoaffective disorder, 78 (7.2%) with bipolar disorder, and the remaining 61 (5.7%) with other psychiatric disorders (Table 1). Table 2 reveals the patients’ demographic characteristics and medications at discharge. Among the included patients, 539 (49.7%) were men. The average age was 41.06 ± 12.81 (mean ± standard deviation) years and average daily clozapine dosage was 242.08 ± 148.86 mg. Concomitant antipsychotics were prescribed to 325 (30.0%) patients, with 245 (22.6%) receiving FGAs and 86 (7.9%) of them receiving SGAs. Antidepressants were prescribed to 164 (15.1%) patients. Ten (0.9%) patients were prescribed with mood stabilizers other than sodium valproate and lithium. Regarding other concurrent medications, 376 (34.7%) patients in the cohort were taking anticholinergics, 559 (51.6%) were taking benzodiazepine, 378 (34.9%) were taking antihypertensives, 29 (2.7%) were taking antidiabetics, 23 (2.1%) were taking antihyperlipidemics, and 22 (2.0%) were taking antiepileptics (Table 2). A total of 501 events of neutropenia and leukocytosis occurred among all participants during the follow-up period. Specifically, 2.9% of patients in the CLO group and 8.8% of patients in the CLO + VAL group developed neutropenia, whereas 39.6% of patients in the CLO group, 42% of patients in the CLO + VAL group, 71.1% of patients in the CLO + Li group, and 50% of patients the CLO + VAL + Li group developed leukocytosis. Concerning neutropenia, Fisher’s exact test demonstrated that the CLO + VAL group had a significantly higher ratio of neutropenia (p < .001; Table 3). There was no significant difference in the incidence of neutropenia between the group receiving CLO + VAL and the group receiving CLO + Li. In this study, we did not observe any neutropenia event in the CLO + Li group or in the CLO + VAL + Li group. As for leukocytosis, concomitant lithium administration was associated with a higher ratio of leukocytosis event (p < .001; Table 3). We also found seven cases (five in the CLO group and two in the CLO + VAL group) who had developed both neutropenia and leukocytosis during the 3-year follow-up. However, the ratios were not significantly different across the four groups (Table 2). After adjustment for covariates (i.e., age, sex, hematological events, daily dosage of clozapine, concomitant psychotropics, and other medications) through logistic regression, the CLO + VAL group (odds ratio [OR] = 3.49, p < .001, compared with the CLO group) and age (OR = 1.03, p = .007) were significantly associated with an increased risk of neutropenia. The CLO + Li group (OR = 3.39, p < .001, compared with the CLO group), younger age (OR = 0.97, p < .001), clozapine daily dosage (OR = 1.01, p = .025), and benzodiazepine use (OR = 1.64, p < .001) were significantly associated with leukocytosis development (Table 4). In addition, in the two formulas presented in Table 3, individual multicollinearity diagnostics revealed that all variables involved in the first step of logistic regression were nonsignificant due to multicollinearity, meaning that every variable had a variance inflation factor (VIF) < 1.5. To explore whether there was an increasing or decreasing trend of develo** neutropenia and leukocytosis according to age, dosage of valproate, and dosage of lithium, we conducted the Cochran–Armitage test, wherein, individuals were stratified by age (i.e., aged < 30, aged 30–39, aged 40–49, aged 50–59, aged ≥ 60 years). With the group of < 30 years as the reference, neutropenia development did not differ significantly among the subgroups. However, with an increase in age, a trend of increased neutropenic events was observed (p = .039; Fig. 1A). In addition, to examine the relationship between valproate daily dosage and neutropenia, we classified the valproate dosage into three subgroups (i.e., dosage ≤ 1000 mg, 1001–2000 mg, and > 2000 mg), with dosage ≤ 1000 mg serving as the reference group. We found no significant difference in each subgroup nor a trend of decreasing or increasing incidence of neutropenia with an increase in valproate dosage (p = .808; Fig. 1C). Regarding leukocytosis, compared with the reference group (< 30 years), those aged 40–49, 50–59, and ≥ 60 had significantly lower risks of develo** leukocytosis. Moreover, a decreasing trend of leukocytosis development was observed with increasing age (p < .001; Fig. 1B). Regarding lithium dosage, with a dosage of < 600 mg as the reference group, each of the other two subgroups (i.e., 601–1200 mg and > 1200 mg) demonstrated no significant difference in leukocytosis development; however, an increasing trend of leukocytosis incidence with an increase in lithium daily dosage was observed (p < .001; Fig. 1D). Adjusted variables include clozapine dosage, sex, antipsychotics use, antidepressants use, anticholinergics use, benzodiazepine use, antihypertensives use, antidiabetics use, antihyperlipidemics use, and antiepileptics use. The Spearman correlation matrix in Supplementary Fig. 2. reveals that the correlations between many covariates were nonsignificant, and a few covariates were significantly but weakly correlated, as evidenced by the correlation coefficients, which were all less than 0.3. Therefore, the correlation between the covariates in our analysis may not affect our main outcome. Our study found a significantly increased risk of valproate-related neutropenia and lithium-related leukocytosis in patients receiving clozapine. These findings were independent of other variables, such as age, sex, daily dose of clozapine, and other concomitant medications. Younger age, male sex, and concurrent benzodiazepine use might be linked to leukocytosis, and older age is a risk factor for neutropenia. Lithium dosage increase is related to an upward trend of leukocytosis development, but such a trend was not noted between valproate dosage increase and neutropenia development. On the basis of our literature review, we enrolled a relatively large number (N = 1084) of patients compared with other studies on valproate-related neutropenia and lithium-related leukocytosis. Our research data were from one large psychiatric institution, and the data were collected between 2006 and 2020. We observed that valproate coadministration is a significant risk factor (OR = 3.49) for the development of clozapine-associated neutropenia. This finding was consistent with those of other studies [16, 26, 27]. Clozapine by itself would induce neutropenia; however, the precise underlying mechanisms remain unclear. One popular hypothesis is that the bioactivation of clozapine produces a chemically reactive nitrenium ion, which causes apoptosis to neutrophils as well as toxicity to stromal cells, the precursors of neutrophils in bone marrow [28]. Clozapine is metabolized by CYP1A2 and CYP3A4, with CYP1A2 playing a major role [26,27,28]. Clozapine metabolism through CYP1A2 is competitively inhibited by valproate [29]. Additionally, valproate by itself may induce blood dyscrasias by affecting the differentiation of normal multipotent hematopoietic progenitors. The risk of blood dyscrasia is higher when valproate is used in combination with clozapine [30]. In contrast to the mentioned UK study [16], we did not find a dose-dependent effect of sodium valproate on neutropenia development. In the present study, another mood stabilizer, lithium, increased the risk of leukocytosis in patients treated with clozapine (OR = 3.39). The precise mechanism by which lithium increases WBC count remains unclear. Putative theories include an increase in granulocyte production, direct stem-cell stimulation, cytokine stimulation, redistribution of demarginated leukocytes, and increased cortisol production [31]. Lithium has been used to treat clozapine-induced neutropenia [21, 32] and to prevent neutropenia during clozapine rechallenge [33], with a minimum serum lithium level of 0.4 mmol/L required for such effects [34]. Nevertheless, prescribing clozapine to a patient already under lithium may result in leukocytosis [46, 47]. Future studies are warranted to confirm our findings. A slightly increased risk of leukocytosis was observed with higher clozapine doses (OR = 1.01, 95% confidence interval: 1.00–1.02). Leukocytosis, a generally asymptomatic and benign condition [33], appears to be a potential side effect of clozapine [36]. The mechanisms of clozapine-induced leukocytosis may be related to changes in plasma concentrations of the granulocyte colony-stimulating factor, tumor necrosis factor-α, interleukin (IL)-2 cytokines, and IL-6 cytokines [33]. Moreover, a downward dose titration results in normalization of WBC counts, suggesting a dose-dependent effect of clozapine [48] . Our study did not replicate a recent finding in the UK demonstrating a reduced risk of neutropenia in patients cotreated with SSRIs [16]. Although the study reported reduced risks of neutropenia in patients treated with SSRIs, a large drug surveillance study with 122,000 psychiatric inpatients [49], which had a similar finding as ours, did not support this finding. In addition, the use of concomitant antidepressants such as mirtazapine and imipramine was associated with neutropenia development. Evidence does not support SSRIs or serotonin–norepinephrine reuptake inhibitors causing neutropenia in patients treated with clozapine [50]. A recent study in Japan involving 3746 patients treated with clozapine reported that 4.9% of the patients developed neutropenia. In our study, the incidence of neutropenia was 2.9%, which was consistent with the 2–3% prevalence described in the literature [5]. Additionally, a recent systematic review reported significantly lower clearance of clozapine in East Asian patients compared with Caucasians [51]. Poor metabolism of clozapine was noted in approximately 10% of Asians; therefore, they needed lower doses to reach therapeutic concentrations [52]. Because of this, Asian patients may be more sensitive to blood dyscrasia (neutropenia or leukocytosis). Data on the concomitant use of clozapine with valproate and lithium in Asian patients are limited. Therefore, a strength of our study is the identification of incidences of neutropenia and leukocytosis between patients treated with clozapine monotherapy alone and subgroups of patients on clozapine cotreated with mood stabilizers. Our study has some limitations. Because this was a retrospective cohort study, some important predictive factors may have been underestimated. Moreover, because the groups were not randomly assigned, some threats to internal validity may have occurred. Although we analyzed participants’ basic demographic data and common concurrent medications, other factors such as smoking [11], oral contraceptive use [29], obesity [53], and inflammation [54] may have affected the WBC counts. Currently, no clinical registry comprises data on physical conditions and treatments from both psychiatric and general hospitals. Furthermore, because the included patients may have irregular outpatient clinic visits, routine hematologic examination may not be regularly performed. We also did not include the serum levels of both valproate and lithium for our patients at discharge. Additionally, clozapine adherence was not objectively confirmed because monitoring clozapine levels is not the standard practice in Taiwan. Our study demonstrated that concomitant administration of valproate with clozapine was significantly associated with the neutropenia three-fold risk increase. Concomitant use of clozapine with lithium was associated with three-fold higher risks of leukocytosis. Therefore, regular follow-up hematology profiles are warranted in patients who received combined treatment with clozapine and valproate/lithium.Results
Demographic and clinical data
Prevalence of neutropenia, leukocytosis, and related factors
Result of logistic regression
Trend for neutropenia and leukocytosis according to age, dosage of valproate, and dosage of lithium
Relationship between the covariates
Discussion
Conclusion
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the ethical restrictions from the Institutional Review Board, but are available from the corresponding author on reasonable request.
References
Siskind D, McCartney L, Goldschlager R, Kisely S. Clozapine v. first-and second-generation antipsychotics in treatment-refractory schizophrenia: systematic review and meta-analysis. Br J Psychiatry. 2016;209(5):385–92.
Masuda T, Misawa F, Takase M, Kane JM, Correll CU. Association with hospitalization and all-cause discontinuation among patients with schizophrenia on clozapine vs other oral second-generation antipsychotics: a systematic review and meta-analysis of cohort studies. JAMA psychiatry. 2019;76(10):1052–62.
Elkis H, Buckley PF. Treatment-resistant schizophrenia. Psychiatric Clin. 2016;39(2):239–65.
De Berardis D, Rapini G, Olivieri L, Di Nicola D, Tomasetti C, Valchera A, et al. Safety of antipsychotics for the treatment of schizophrenia: a focus on the adverse effects of clozapine. Therapeutic Adv drug Saf. 2018;9(5):237–56.
Wiciński M, Węclewicz MM. Clozapine-induced agranulocytosis/granulocytopenia: mechanisms and monitoring. Curr Opin Hematol. 2018;25(1):22–8.
Myles N, Myles H, **a S, Large M, Kisely S, Galletly C, et al. Meta-analysis examining the epidemiology of clozapine‐associated neutropenia. Acta psychiatrica Scandinavica. 2018;138(2):101–9.
Li X-H, Zhong X-M, Lu L, Zheng W, Wang S-b, Rao W-w, et al. The prevalence of agranulocytosis and related death in clozapine-treated patients: a comprehensive meta-analysis of observational studies. Psychol Med. 2020;50(4):583–94.
Taylor D, Vallianatou K, Whiskey E, Dzahini O, MacCabe J. Distinctive pattern of neutrophil count change in clozapine-associated, life-threatening agranulocytosis. Schizophrenia. 2022;8(1):21.
Honigfield G. Effects of the clozapine national registry system on incidence of deaths related to agranulocytosis.Psychiatric Services. 1996.
Miller DD. Review and management of clozapine side effects. J Clin Psychiatry. 2000;61(suppl 8):18308.
Paribello P, Manchia M, Zedda M, Pinna F, Carpiniello B. Leukocytosis associated with clozapine treatment: a case series and systematic review of the literature. Medicina. 2021;57(8):816.
Siskind DJ, Lee M, Ravindran A, Zhang Q, Ma E, Motamarri B, et al. Augmentation strategies for clozapine refractory schizophrenia: a systematic review and meta-analysis. Australian & New Zealand Journal of Psychiatry. 2018;52(8):751–67.
Kelly DL, Conley RR, Feldman S, Yu Y, McMahon RP, Richardson CM. Adjunct divalproex or lithium to clozapine in treatment-resistant schizophrenia. Psychiatr Q. 2006;77(1):81–95.
Bender S, Linka T, Wolstein J, Gehendges S, Paulus H-J, Schall U, et al. Safety and efficacy of combined clozapine–lithium pharmacotherapy. Int J Neuropsychopharmacol. 2004;7(1):59–63.
Imbarlina MJ, Sarkar S, Marwah S, Parepally H, Johnston PR, Brar JS, et al. Leukopenia in clozapine treated patients may be induced by other drugs: a case series. Eur psychiatry. 2004;19(8):506–9.
Malik S, Lally J, Ajnakina O, Pritchard M, Krivoy A, Gaughran F, et al. Sodium valproate and clozapine induced neutropenia: a case control study using register data. Schizophr Res. 2018;195:267–73.
Rahman A, Mican LM, Fischer C, Campbell AH. Evaluating the incidence of leukopenia and neutropenia with valproate, quetiapine, or the combination in children and adolescents. Ann Pharmacother. 2009;43(5):822–30.
Fehsel K, Loeffler S, Krieger K, Henning U, Agelink M, Kolb-Bachofen V, et al. Clozapine induces oxidative stress and proapoptotic gene expression in neutrophils of schizophrenic patients. J Clin Psychopharmacol. 2005;25(5):419–26.
Shopsin B, Friedmann R, Gershon S. Lithium and leukocytosis. Clin Pharmacol Ther. 1971;12(6):923–8.
Ozdemir MA, Sofuoğlu S, Tanrikulu G, Aldanmaz F, Eşel E, Dündar S. Lithium-induced hematologic changes in patients with bipolar affective disorder. Biol Psychiatry. 1994;35(3):210–3.
Suraweera C, Hanwella R, de Silva V. Use of lithium in clozapine-induced neutropenia: a case report. BMC Res Notes. 2014;7(1):1–3.
Focosi D, Azzarà A, Kast RE, Carulli G, Petrini M. Lithium and hematology: established and proposed uses. J Leukoc Biol. 2009;85(1):20–8.
Parente J. Diagnostics for White Blood Cell Abnormalities: leukocytosis and Leukopenia. Physician Assistant Clinics. 2019;4(3):625–35.
Organization WH. ATC/DDD Index 2019 https://www.whocc.no/atc_ddd_index.Accessed; 2018.
Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts E, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–45.
Ghaznavi S, Nakic M, Rao P, Hu J, Brewer JA, Hannestad J, et al. Rechallenging with clozapine following neutropenia: treatment options for refractory schizophrenia. Am J Psychiatry. 2008;165(7):813–8.
Pantelis C. Increased risk of neutropaenia and agranulocytosis with sodium valproate used adjunctively with clozapine. Aust N Z J Psychiatry. 2001;35(4):544–5.
Pessina A, Turlizzi E, Bonomi A, Guizzardi F, Cavicchini L, Croera C, et al. In vitro toxicity of clozapine, olanzapine, and quetiapine on granulocyte-macrophage progenitors (GM-CFU). Pharmacopsychiatry. 2006;39(01):20–2.
de Leon J. Future studies on the interaction between clozapine and valproic acid should aspire to include longitudinal designs and free valproate concentrations, and should consider that inducer and/or inhibitory effects may vary with time, the individual, and the auto-induction of valproic acid. Ther Drug Monit. 2020;42(1):159–61.
Bartels M, van Solinge WW, den Breeijen HJ, Bierings MB, Coffer PJ, Egberts TC. Valproic acid treatment is associated with altered leukocyte subset development. J Clin Psychopharmacol. 2012;32(6):832–4.
Whiskey E, Taylor D. Restarting clozapine after neutropenia. CNS Drugs. 2007;21(1):25–35.
Aydin M, Ilhan BC, Calisir S, Yildirim S, Eren I. Continuing clozapine treatment with lithium in schizophrenic patients with neutropenia or leukopenia: brief review of literature with case reports. Therapeutic Adv Psychopharmacol. 2016;6(1):33–8.
Kanaan RA, Kerwin RW. Lithium and clozapine rechallenge: a retrospective case analysis. J Clin Psychiatry. 2006;67(5):756–60.
Paton C, Esop R. Managing clozapine-induced neutropenia with lithium. Psychiatr Bull. 2005;29(5):186–8.
Palominao A, Kukoyi O, **ong GL. Leukocytosis after lithium and clozapine combination therapy. Annals of clinical psychiatry: official journal of the American Academy of Clinical Psychiatrists. 2010;22(3):205–6.
Volz H-P, Möller H-J. Antidepressant drug therapy in the elderly-a critical review of the controlled clinical trials conducted since 1980. Pharmacopsychiatry. 1994;27(03):93–100.
Gareri P, De Fazio P, Stilo M, Ferreri G, De Sarro G. Conventional and atypical antipsychotics in the elderly. Clin Drug Investig. 2003;23(5):287–322.
Greenblatt DJ, Sellers EM, Shader RI. Drug disposition in old age. N Engl J Med. 1982;306(18):1081–8.
Gareri P, Stilo G, Bevacqua I, Mattace R, Ferreri G, De Sarro G. Antidepressant drugs in the elderly. Gen Pharmacology: Vascular Syst. 1998;30(4):465–75.
Uchida H, Mamo DC, Mulsant BH, Pollock BG, Kapur S. Increased antipsychotic sensitivity in elderly patients: evidence and mechanisms. J Clin Psychiatry. 2009;70(3):397.
Gareri P, De Fazio P, Russo E, Marigliano N, De Fazio S, De Sarro G. The safety of clozapine in the elderly. Exp Opin Drug Saf. 2008;7(5):525–38.
Fabrazzo M, Prisco V, Sampogna G, Perris F, Catapano F, Monteleone AM, et al. Clozapine versus other antipsychotics during the first 18 weeks of treatment: a retrospective study on risk factor increase of blood dyscrasias. Psychiatry Res. 2017;256:275–82.
Möhler H, Fritschy J, Rudolph U. A new benzodiazepine pharmacology. J Pharmacol Exp Ther. 2002;300(1):2–8.
Carmen J, Okafor K, Ike E. The effects of lithium therapy on leukocytes: a 1-year follow-up study. J Natl Med Assoc. 1993;85(4):301.
Madhusoodanan S, Cuni L, Brenner R, Sajatovic M, Palekar N, Amanbekova D. Chronic leukocytosis associated with clozapine: a case series. J Clin Psychiatry. 2007;68(3):2637.
Aminzadeh Z, Parsa E. Relationship between age and peripheral white blood cell count in patients with sepsis. Int J Prev Med. 2011;2(4):238.
Beerman I, Maloney WJ, Weissmann IL, Rossi DJ. Stem cells and the aging hematopoietic system. Curr Opin Immunol. 2010;22(4):500–6.
Liu F, Mahgoub N, Ferrando S. Leukocytosis associated with clozapine treatment: a case report. Psychosomatics. 2011;52(5):488–91.
Stübner S, Grohmann R, Engel R, Bandelow B, Ludwig W-D, Wagner G, et al. Blood dyscrasias induced by psychotropic drugs. Pharmacopsychiatry. 2004;37(S 1):70–8.
Demler TL, Trigoboff E. Are clozapine blood dyscrasias associated with concomitant medications? Innovations in Clinical Neuroscience. 2011;8(4):35.
Ruan C-J, Zang Y-N, Wang C-Y, Cheng Y-H, Sun C, Spina E, et al. Clozapine metabolism in East Asians and Caucasians: a pilot exploration of the prevalence of poor metabolizers and a systematic review. J Clin Psychopharmacol. 2019;39(2):135–44.
Ruan C-J, Wang C-Y, Tang Y-L, Lin S-K, Lee S-T, Hong KS, et al. Exploring the prevalence of clozapine phenotypic poor metabolizers in 4 asian samples: they ranged between 2% and 13%. J Clin Psychopharmacol. 2019;39(6):644–8.
Kuzin M, Haen E, Hiemke C, Bochon B, Bochon K, Gründer G, et al. Body mass index as a determinant of clozapine plasma concentrations: a pharmacokinetic-based hypothesis. J Psychopharmacol. 2021;35(3):273–8.
De Leon J, Schoretsanitis G, Smith RL, Molden E, Solismaa A, Seppälä N, et al. An international adult guideline for making clozapine titration safer by using six ancestry-based personalized dosing titrations, CRP, and clozapine levels. Pharmacopsychiatry. 2022;55(02):73–86.
Acknowledgements
The authors wish to acknowledge the help of Dr. Hung-Yu Chan in commenting on an early draft of this work.
Funding
This work was supported by Hospital and Social Welfare Organizations Administration Commission, Taiwan [program number: 11058].
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: Chia-Chun Yang, **-Yu Wang; data collection: **-Yu Wang, Chia-Chun Yang; analysis and interpretation of results: **-Yu Wang; draft manuscript preparation: Chia-Chun Yang, **-Yu Wang; review & editing: Po-Han Chou, Ching- Hua Lin, **-Yu Wang. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study protocol was approved by the Taoyuan Psychiatric Center Institutional Review Boards and was conducted in accordance with both the Human Subjects Research Act of Taiwan and the Declaration of Helsinki (2013). The need for Informed Consent was waived by the Taoyuan Psychiatric Center Institutional Review Boards due to the retrospective nature of the study.
Conflict of interest
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, CC., Wang, XY., Chou, PH. et al. Valproate-related neutropenia and lithium-related leukocytosis in patients treated with clozapine: a retrospective cohort study. BMC Psychiatry 23, 170 (2023). https://doi.org/10.1186/s12888-023-04659-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04659-2