Abstract
Background
The rebound of influenza A (H1N1) infection in post-COVID-19 era recently attracted enormous attention due the rapidly increased number of pediatric hospitalizations and the changed characteristics compared to classical H1N1 infection in pre-COVID-19 era. This study aimed to evaluate the clinical characteristics and severity of children hospitalized with H1N1 infection during post-COVID-19 period, and to construct a novel prediction model for severe H1N1 infection.
Methods
A total of 757 pediatric H1N1 inpatients from nine tertiary public hospitals in Yunnan and Shanghai, China, were retrospectively included, of which 431 patients diagnosed between February 2023 and July 2023 were divided into post-COVID-19 group, while the remaining 326 patients diagnosed between November 2018 and April 2019 were divided into pre-COVID-19 group. A 1:1 propensity-score matching (PSM) was adopted to balance demographic differences between pre- and post-COVID-19 groups, and then compared the severity across these two groups based on clinical and laboratory indicators. Additionally, a subgroup analysis in the original post-COVID-19 group (without PSM) was performed to investigate the independent risk factors for severe H1N1 infection in post-COIVD-19 era. Specifically, Least Absolute Shrinkage and Selection Operator (LASSO) regression was applied to select candidate predictors, and logistic regression was used to further identify independent risk factors, thus establishing a prediction model. Receiver operating characteristic (ROC) curve and calibration curve were utilized to assess discriminative capability and accuracy of the model, while decision curve analysis (DCA) was used to determine the clinical usefulness of the model.
Results
After PSM, the post-COVID-19 group showed longer fever duration, higher fever peak, more frequent cough and seizures, as well as higher levels of C-reactive protein (CRP), interleukin 6 (IL-6), IL-10, creatine kinase-MB (CK-MB) and fibrinogen, higher mechanical ventilation rate, longer length of hospital stay (LOS), as well as higher proportion of severe H1N1 infection (all P < 0.05), compared to the pre-COVID-19 group. Moreover, age, BMI, fever duration, leucocyte count, lymphocyte proportion, proportion of CD3+ T cells, tumor necrosis factor α (TNF-α), and IL-10 were confirmed to be independently associated with severe H1N1 infection in post-COVID-19 era. A prediction model integrating these above eight variables was established, and this model had good discrimination, accuracy, and clinical practicability.
Conclusions
Pediatric H1N1 infection during post-COVID-19 era showed a higher overall disease severity than the classical H1N1 infection in pre-COVID-19 period. Meanwhile, cough and seizures were more prominent in children with H1N1 infection during post-COVID-19 era. Clinicians should be aware of these changes in such patients in clinical work. Furthermore, a simple and practical prediction model was constructed and internally validated here, which showed a good performance for predicting severe H1N1 infection in post-COVID-19 era.
Graphical Abstract

Similar content being viewed by others
Introduction
Influenza has been one of the major concerns encountered in the public health domain. Populations of all ages are susceptible to infection with influenza viruses, especially children due to their underdeveloped immune defense mechanisms [1]. According to statistics, approximately 109.5 million children under 5 years of age were infected with influenza viruses in 2018. Of these, 870,000 children were hospitalized with influenza-related acute lower respiratory infection (ALRI) and up to 34,800 deaths, accounting for 4% of all ALRI-related deaths in this age group [2]. However, it is noteworthy that during the COVID-19 pandemic, both Northern and Southern Hemispheres showed little records of influenza activity. This phenomenon was primarily attributed to the implementation of non-pharmaceutical interventions (NPIs), including use of face masks, social distancing, etc., which not only limited the transmission of SARS-CoV-2 but also influenza viruses [3,4,5]. Despite this positive collateral effect on preventing additional overload of the healthcare system in the short term, the lack of immune stimulation due to the declined circulation of pathogens induced an “immunity debt” which may result in negative consequences when the COVID-19 pandemic is controlled and NPIs are lifted [6, 7]. In fact, in the post- COVID-19 era with the lifting of strict NPIs, many countries and regions have reported significant resurgence of influenza circulation [8, 9]. Influenza rebound following three seasons of inactivity was also observed in China after gradually easing NPIs. According to the data from Chinese Center for Disease Control and Prevention (CDC) (https://www.chinacdc.cn/), a rapid increase in the number of pediatric patients hospitalized with influenza A (H1N1) infection was observed in February 2023, and the positive rate of H1N1 infection peaked (53.2%) in 10th week of 2023 (February 6, 2023- February 12, 2023). Newly diagnosed cases were still being reported every day as of July 2023 in various regions of China, including Yunnan.
On the other hand, the history of SARS-CoV-2 infection may exert a detrimental clinical influence on H1N1 infection in the post-COVID-19 era. During the latest Omicron wave between December 2022 and February 2023 in China, over 82% of the Chinese population contracted SARS-CoV-2 Omicron infection between December 2022 and February 2023 [10]. One or more persistent COVID-19-related symptoms with hypothesised pathophysiologic mechanisms involving residual virus in a variety of tissues, immune dysregulation, and autoimmunity resulting from cross reactivity of SARS-CoV-2-specific antibodies with host proteins, etc. have been reported in a significant proportion of individuals who recovered from COVID-19 for months or even longer [11,12,13,14]. Therefore, the prior infection of SARS-CoV-2 is a non-negligible factor that may further exacerbate the clinical severity and manifestations of children with H1N1 infection in the post-COVID-19 era.
Until now, most studies about influenza infection in post-COIVD-19 era focused on the epidemiological investigations but limited studies concentrated on the changes in clinical severity and presentation of influenza infection in children. In this study, we retrospectively collected demographic and clinical data from children hospitalized with H1N1 during November 2018- April 2019 (influenza season in Northern Hemisphere before COVID-19 pandemic) and February 2023- July 2023 (post-COVID-19 era) in nine hospitals in Yunnan and Shanghai, investigating the changes in clinical severity and characteristics of pediatric H1N1 infection from pre- to post-COVID-19 era and constructing a predictive model for severe H1N1 cases in the post-COVID-19 era.
Methods
Participants
This multicenter retrospective study was performed at nine hospitals in Yunnan and Shanghai, all of which are large, public tertiary hospitals. Children who were hospitalized with H1N1 infection in any of the participating hospitals during November 2018- April 2019 and February 2023- July 2023 were retrospectively included in our study. The inclusion criteria were as follows: (1) children who met the diagnostic criteria of influenza A (H1N1) infection [15, 16]; (2) children aged ≤ 14 years at initial diagnosis; and (3) the interval from symptom onset to admission was within 48 h. All subjects eventually included were divided into two groups, including pre-COVID-19 group (November 2018- April 2019) and post-COVID-19 group (February 2023- July 2023), based on the date of admission.
According to the World Health Organization (WHO) guidelines for influenza A (H1N1) virus [17], severe H1N1 infection were defined as patients presenting with one or more of the following manifestations: (1) dyspnea, tachypnea, or hypoxia; (2) radiological signs of lower respiratory tract disease (e.g. pneumonia); (3) severe central nervous system (CNS) involvement (e.g., encephalopathy, encephalitis); (4) severe dehydration; (5) multiorgan failure; (6) septic shock; (7) exacerbation of underlying chronic disease, including asthma, chronic obstructive pulmonary disease, chronic hepatic or renal insufficiency, diabetes mellitus, or other cardiovascular conditions; and (8) any other influenza-related condition or clinical manifestation requiring hospital admission. The remaining cases were defined as the general H1N1 infection.
This study was performed under the Declaration of Helsinki and was approved by the Ethics Committees of Kunming Children’s Hospital Affiliated to Kunming Medical University (the lead institution of this study) (approval number: 2023-04-129-K01), who also waived the informed consent due to the retrospective design of the study.
Data extraction
A retrospective review of subjects’ medical records at admission from the participating hospitals was conducted to gather the demographic information [age, gender, body mass index (BMI)], clinical features (fever, fever duration, fever peak, cough, rhinorrhea, wheezing, sore throat, headache, myalgia, seizures, drowsiness, diarrhea, vomiting, abdominal pain), laboratory characteristics [leucocyte count, neutrophil proportion, lymphocyte proportion, proportions of CD3+ T cells, CD3+8+ T cells, CD3+4+ T cells, NK cells and B cells, C-reactive protein (CRP), interleukin 6 (IL-6), IL-10, tumor necrosis factor α (TNF-α), creatine kinase-MB (CK-MB), high-sensitivity troponin T (hs-TnT), alanine transaminase (ALT), aspartate transaminase (AST), fibrinogen], co-infection with SARS-CoV-2, mechanical ventilation rate, length of hospital stay (LOS), as well as rate of severe H1N1 infection. The vaccination information including data on H1N1 vaccination and COVID-19 vaccination status was also collected and patients who received at least one dose were considered as vaccinated. All data were reviewed and checked by a trained team of clinicians.
Statistical analysis
The whole study was divided into two parts: (1) comparison of clinical severity across the pre- and post-COVID-19 groups and (2) construction of prediction model for severe pediatric H1N1 infection.
In the part 1, to minimize the influence of potential demographic confounders, propensity-score matching (PSM) using 1:1 nearest neighbor matching with a caliper of 0.02 was adopted to balance age, gender, and BMI between these two groups, and then clinical severity was compared between groups based on a series of clinical and laboratory characteristics.
In the part 2, a subgroup analysis in the original post-COVID-19 group (without PSM) was performed to construct a model for predicting the risk of severe pediatric H1N1 infection during the post-COVID-19 era. Specifically, during this process, to avoid omitting important predictive variable, all variables (except for mechanical ventilation rate and LOS) were included into Least Absolute Shrinkage and Selection Operator (LASSO) regression, which was utilized to minimize potential multicollinearity and overfitting, thus selecting most useful candidate predictors based on the value of lambada. To ensure the accuracy and conciseness of the model at the same time, a lambda within one standard error of the minimum criteria (lambda.1se) was chosen as the optimal lambda by a 10-fold cross-validation using the built-in function cv.glmnet from R package glmnet. Logistic regression analysis was used to further identify independent risk factors, establishing the prediction model. Patients in the post-COVID-19 group were randomly divided into training and internal validation sets at a ratio of 7:3 using the R package caret, then the receiver operating characteristic (ROC) curve (R package pROC), calibration curve (R package rms), and decision curve analysis (DCA) (R package rmda) were used in both training and internal validation sets for assessing the discriminatory ability, accuracy, and clinical benefit of this model, respectively.
In addition, general descriptive statistics were calculated as follows. Distribution of variables was checked using the Shapiro-Wilk test. Categorical variables were presented as percentages (%) and compared using Pearson’s chi-square or Fisher’s exact test, while continuous variables with skewed distribution were expressed as medians (interquartile range, IQR) and compared using Mann-Whitney U test. All statistical analyses were conducted using R software version 3.5.1 (R Foundation, Vienna, Austria) with a two-side significance level of P value < 0.05.
Results
Comparison of patients’ characteristics and severity between the pre- and post-COVID-19 groups after PSM
During the entire study period, a total of 757 children with H1N1 infection were included. Among these, 431 and 326 patients were classified into the post- and pre-COVID-19 groups, respectively (Fig. 1). As shown in Table 1, prior to PSM, the post-COVID-19 group showed an older median age at infection (5.4 vs. 4.6 years, P = 0.001), a slighter male predominance (58.0% vs. 66.0%, P = 0.026), as well as a higher BMI (18.0 vs. 17.1 kg/m2, P < 0.001), compared to the pre-COVID-19 group. After PSM, 291 subjects were retained in each group with no significant differences in distribution of age, gender, and BMI (all P > 0.05).
According to the analysis results of the matched data, notable differences in several clinical characteristics and laboratory indicators were identified between these two groups. Specifically, compared to the pre-COVID-19 group, the post-COVID-19 group revealed markedly longer duration of fever (4.0 vs. 3.0 days, P < 0.001), higher fever peak (39.0 vs. 38.8 °C, P < 0.001), more frequent cough (90.7% vs. 82.5%, P = 0.003) and seizures (18.2% vs. 7.6%, P < 0.001), as well as higher levels of CRP (14.9 vs. 11.7 mg/L, P < 0.001), IL-6 (20.5 vs. 11.0 pg/mL, P < 0.001), IL-10 (16.5 vs. 14.9 pg/mL, P = 0.03), CK-MB (44.9 vs. 36.0 U/L, P < 0.001) and fibrinogen (3.9 vs. 3.7 g/L, P = 0.046). Furthermore, more patients requiring mechanical ventilation (4.1% vs. 1.4%, P = 0.043), longer LOS (8.0 vs. 6.0 days, P < 0.001), as well as a higher proportion of severe H1N1 infection (20.6% vs. 14.1%, P = 0.038) were found in the post-COVID-19 group than those in the pre-COVID-19 group. These findings suggested a greater severity of H1N1 infection in the post-COVID-19 group than the pre-COVID-19 group.
Characteristics of patients in the post-COVID-19 group without PSM
There was a total of 431 patients in the post-COVID-19 group without PSM, of which 93 (21.6%) eventually developed severe H1N1 infection (severe H1N1 subgroup) and 338 (78.4%) were considered to be general type (general H1N1 subgroup). As described in Table 2, in comparison with general H1N1 cases, patients with severe H1N1 infection reported a younger age (4.0 vs. 5.5 years, P < 0.001), more clear male predominance (71.0% vs. 54.4%, P = 0.004), as well as a greater BMI (19.4 vs. 17.5 kg/m2, P < 0.001). Despite no marked between-group differences in total number of patients receiving the COVID-19 vaccine or H1N1 vaccine, the severe H1N1 subgroup indicated a lower proportion of three-dose COVID-19 vaccination than the general subgroup (17.2% vs. 27.8%, P = 0.038). Significant differences in clinical and laboratory characteristics were observed across these two subgroups, including longer fever duration (6.0 vs. 4.0 days, P < 0.001), higher fever peak (39.1 vs. 39.0 °C, P = 0.022), more frequent wheezing (55.9% vs. 23.4%, P < 0.001), seizures (44.1% vs. 10.9%, P < 0.001) and drowsiness (69.9% vs. 25.1%, P < 0.001), increased leucocyte count (9.5 vs. 5.7 × 109/L, P < 0.001) and neutrophil proportion (56.1% vs. 44.5%, P < 0.001), higher levels of CRP (23.5 vs. 14.6 mg/L, P < 0.001), IL-6 (28.7 vs. 19.3 pg/mL, P < 0.001), IL-10 (23.7 vs. 14.9 pg/mL, P < 0.001), TNF-α (13.2 vs. 7.3 pg/mL, P < 0.001), CK-MB (53.2 vs. 43.9 U/L, P < 0.001), hs-TnT (7.8 vs. 4.1 pg/mL, P < 0.001) and fibrinogen (4.1 vs. 3.8 g/L, P = 0.002), elevated rates of co-infection with SRAS-CoV-2 (19.4% vs. 10.9%, P = 0.031) and mechanical ventilation (21.5% vs. 0, P < 0.001), as well as longer LOS (9.0 vs. 7.0 days, P < 0.001) in the severe subgroup than those in the general subgroup. On the other hand, the severe subgroup indicated lower proportions of lymphocyte (28.8% vs. 44.0%, P < 0.001), CD3+ T cells (58.5% vs. 70.6%, P < 0.001), CD3+8+ T cells (22.3% vs. 26.9%, P < 0.001) and CD3+4+ T cells (28.7% vs. 37.7%, P < 0.001), compared to the general subgroup.
Identification of independent risk factors and construction of prediction model for severe H1N1 infection in the post-COVID-19 era
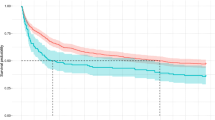
Fourteen candidate predictor variables, including age, BMI, fever duration, leucocyte count, lymphocyte proportion, proportion of CD3+ T cells, CRP, TNF-α, IL-10, wheezing, seizures, diarrhea, vomiting, and drowsiness, were selected by LASSO regression (Fig. 2a and b) and were further included into the logistic regression analysis. Eventually, age (OR: 0.660; 95% CI: 0.525–0.830), BMI (OR: 1.700; 95% CI:1.301–2.222), fever duration (OR: 1.860; 95% CI: 1.429–2.421), leucocyte count (OR: 1.198; 95% CI: 1.061–1.354), lymphocyte proportion (OR: 0.958; 95% CI: 0.931–0.986), proportion of CD3+ T cells (OR: 0.929; 95% CI: 0.898–0.962), TNF-α (OR: 1.057; 95% CI: 1.026–1.089), and IL-10 (OR: 1.049; 95% CI: 1.026–1.073) were confirmed to be the independent risk factors for severe H1N1 infection in the post-COVID-19 group (Fig. 3a). Based on the regression coefficient (β) values of intercept and these eight independent factors, the predicted probability equation was derived as follows:
Selection of candidate predictive variables using LASSO regression. A LASSO coefficient profiles of these all potential predictive variables. The coefficient profile plot was generated against the log lambda sequence. B Tuning parameter (lambda) selection in the LASSO model using 10-fold cross-validation via one standard error of the minimum criteria (lambda.1se). Based on lambda.1se, 14 variables with non-zero coefficients were selected. LASSO, Least Absolute Shrinkage and Selection Operator
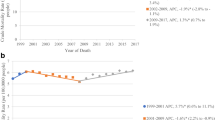
Construction and performance evaluation of the prediction model for severe pediatric H1N1 infection in post-COVID-19 era. A The result of logistic regression analysis. Age, BMI, fever duration, leucocyte count, lymphocyte proportion, proportion of CD3+ T cells, TNF-α, and IL-10 were independently associated with severe H1N1 infection in the post-COVID-19 group. B and C ROC curve analysis showed that the AUC for the training set was 0.973, with a sensitivity of 93.1% and a specificity of 93.6%, and the AUC was 0.949 for the validation set, with a sensitivity of 90.5% and a specificity of 88.6%. D and E Calibration curve analysis indicated favorable agreement between the predicted probability and the observed probability in both training and internal validation sets. F and G DCA identified good clinical utility of this prediction model in both training and internal validation sets. AUC, area under the curve; BMI, body mass index; DCA, decision curve analysis; IL-10, interleukin 10; ROC, receiver operating characteristic; TNF-α, tumor necrosis factor α
Evaluation of model performance
ROC curves and calibration curves were plotted to evaluate the predictive performance and accuracy of this model. The prediction model achieved an area under the ROC curve (AUC) of 0.973 in the training set, with a sensitivity of 93.1% and a specificity of 93.6% (Fig. 3b), while the AUC was 0.949 for the validation set, with a sensitivity of 90.5% and a specificity of 88.6% (Fig. 3c), suggesting favorable discriminatory capacity. Meanwhile, the calibration curves revealed that the model-predicted probability was well consistent with the observed probability, since the bias-corrected curves were very close to the 45-degree ideal lines in both training set (Hosmer-Lemeshow test P = 0.832) and validation set (Hosmer-Lemeshow test P = 0.659) (Fig. 3d and e). Moreover, to further assess the clinical value of the prediction model, DCA was employed here. The ordinate represented the net benefit, while the abscissa indicated the threshold probability. The results of DCA indicated that the net benefit derived from this model surpassed the “All” and “None” schemes when the threshold probability ranged from 0 to 0.93 in the training set (Fig. 3f) and from 0 to 0.95 in the validation set (Fig. 3g), respectively.
Discussion
In the present study, we analyzed changes in clinical characteristics and severity of children hospitalized with H1N1 infection in the post-COVID-19 era compared to the pre-COVID-19 era, and constructed a simple and practical risk model integrating eight common demographic, clinical and laboratory indicators for predicting severe H1N1 infection in the post-COVID-19 era.
After PSM for age, gender, and BMI between the pre- and post-COVID-19 groups, we found significant differences in clinical and laboratory indicators among the two groups, including longer fever duration, higher fever peak, more frequent cough and seizures, elevated levels of inflammatory markers and CK-MB, higher rates of severe cases and mechanical ventilation, as well as longer LOS in the post-COVID-19 group than those in the pre-COVID-19 group, suggesting a greater severity in the post-COVID-19 group. The difference of clinical severity of H1N1 infection between these two periods may be explained by the following three main reasons. The first one is the co-infection with SRAS-CoV-2. Although the critical stage of COVID-19 pandemic has ended, the transmission of SARS-CoV-2 is still ongoing at a low level with ‘mini-wave’ pattern [18]. Echoing this viewpoint, a small number of H1N1 patients co-infected SARS-CoV-2 were observed in post-COVID-19 group in our study. There has been evidence suggesting that co-infections will aggravate viral pathology and clinical severity of patients compared to the single infection of SARS-CoV-2 or influenza A virus by prolonging the virus infection period and impairing neutralizing antibody response [19]. The second one is immunity debt. The lack of exposure to pathogens due to strict NPIs during COVID-19 pandemic resulted in a reduced immune stimulation, thereby weakening the adaptive immunity to specific pathogens [20]. The longer the duration of “pathogens low-exposure” is, the greater the risk of future more severe pandemics due to an increasing susceptible population and decreased level of herd immunity [6]. This issue is particularly concerning in China given that China is one of the countries with the most restrictive and longest-duration NPIs. Thirdly, another non-negligible factor may be the medical history of acute SARS-CoV-2 infection due its ultra-high infection rate (more than 82%) between December 2022 and February 2023 in China [28, 29], both younger and overweight children are more prone to develop severe form of influenza infection. Second, as we know, during viral invasion, the brain orchestrates evolutionary conserved physiological symptoms, aiming to clear the pathogens and promote the survival of host [30]. Of which, fever is a cardinal symptom of viral infection and triggered by pathogen associated molecules that stimulate the secretion of inflammatory factors by immune cells [31]. This mechanism perhaps partially accounts for why TNF-α and IL-10 could play important roles in predicting occurrence of severe H1N1 infection in this study. There is already evidence suggesting that long fever duration and excessive release of inflammatory factors are closely linked with aggravated sickness behaviors and worse outcomes in patients with severe viral infection [32, 33]. Third, differences regarding leucocyte and its subsets among patients with viral infection also reflect the variance in the severity or progression of disease. Consistent with our find, previous studies have reported an increased leucocyte count and reduced lymphocyte count in patients with severe viral infection compared to non-severe cases, where the underlying mechanism primarily involves imbalance of immune system, including excessive activation of immune cells, hyperinflammation, and direct effects of the virus on lymphocyte recruitment [34,35,36]. The most crucial change in the decreased lymphocytes induced by viral infection is the decline in CD3+ T cells, which are regarded as key players in adaptive immunoreaction against influenza infection due to the potent cytotoxic function in activated CD3+8+ T cells, the function of producing a series of cytokines and facilitating synthesis and secretion of antibodies in CD3+4+ T cells, etc. [37]. Noteworthy, as we have mentioned earlier, degranulating virus-specific CD3+8+ T cells were demonstrated to be reduced in some patients who had overcome acute SARS-CoV-2 infection for over eight months [21]. Therefore, the proportion of CD3+ T cells will play a significant role for predicting severe H1N1 infecting during the post-COVID-19 era.
Via integrating these above eight variables, we constructed a simple and practical prediction model, which showed good accuracy and discrimination. Meanwhile, net benefit of using this model was determined by DCA method, which suggested the good clinical practicability. This prediction model may be a very suitable tool for early clinical identification of severe cases among children hospitalized with H1N1 infection during the post-COVID-19 era, aiding clinicians in decision-making. Another important and attracted point is that these eight predictive variables used in our model are very common in clinic and are readily available even in a primary hospital without additional financial cost to patients. During the post-COVID-19 era, this model could hold significant value for the clinical management of pediatric H1N1 patients, especially given the greater severity and increased number of hospitalizations of such patients compared to classical influenza individuals in the pre-COVID-19 era.
This study is subject to several limitations. Due to the retrospective nature of the study, the existence of selection bias and residual confounding variables cannot be excluded despite the application of PSM. Despite the multicenter design, there is a relative limitation in the source and distribution of participants due to the study being conducted solely in Yunnan Province, which may cause an excessively high AUC value of the prediction model here. Besides, this prediction model should be validated by external cohorts, which are absent in our study. Future studies should include larger, multicenter cohorts in a prospective multicenter design.
Conclusions
Pediatric H1N1 infection during the post-COVID-19 era showed a higher overall disease severity compared to classical H1N1 infection in the pre-COVID-19 period. Meanwhile, cough and seizures were more prominent in children with H1N1 infection during the post-pandemic era. Clinicians should be aware of these changes in H1N1 infection in the post-pandemic era and more attention to such patients is needed in clinical work. Besides, a prediction model based on age, BMI, fever duration, leucocyte count, lymphocyte proportion, proportion of CD3+ T cells, TNF-α, and IL-10 was constructed and internally validated here, which showed a good performance for predicting severe H1N1 infection in the post-COVID-19 era.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate transaminase
- BMI:
-
Body mass index
- CK-MB:
-
Creatine kinase-MB
- CRP:
-
C-reactive protein
- DCA:
-
Decision curve analysis
- hs-TnT:
-
High-sensitivity troponin T
- IL-6:
-
Interleukin 6
- IL-10:
-
Interleukin 10
- IQR:
-
Interquartile range
- LASSO:
-
Least Absolute Shrinkage and Selection Operator
- LOS:
-
Length of hospital stay
- NPIs:
-
Non-pharmaceutical interventions
- PSM:
-
Propensity-score matching
- ROC:
-
Receiver operating characteristic
- TNF-α:
-
Tumor necrosis factor α
References
Somes MP, Turner RM, Dwyer LJ, Newall AT. Estimating the annual attack rate of seasonal influenza among unvaccinated individuals: a systematic review and meta-analysis. Vaccine. 2018;36(23):3199–207.
Wang X, Li Y, O’Brien KL, Madhi SA, Widdowson MA, Byass P, Omer SB, Abbas Q, Ali A, Amu A, et al. Global burden of respiratory infections associated with seasonal influenza in children under 5 years in 2018: a systematic review and modelling study. Lancet Glob Health. 2020;8(4):e497–510.
ÓhAiseadha C, Quinn GA, Connolly R, Wilson A, Connolly M, Soon W, Hynds P. Unintended consequences of COVID-19 non-pharmaceutical interventions (NPIs) for population health and health inequalities. Int J Env Res Pub Health. 2023;20(7):5223.
Chan CP, Wong NS, Leung CC, Lee SS. Positive impact of measures against COVID-19 on reducing influenza in the Northern Hemisphere. J Travel Med. 2020;27:27(8).
Lee SS, Viboud C, Petersen E. Understanding the rebound of influenza in the post COVID-19 pandemic period holds important clues for epidemiology and control. Int J Infect Dis. 2022;122:1002–4.
Cohen R, Levy C, Rybak A, Angoulvant F, Ouldali N, Grimprel E. Immune debt: recrudescence of disease and confirmation of a contested concept. Infect Dis Now. 2023;53(2):104638.
Rybak A, Levy C, Angoulvant F, Auvrignon A, Gembara P, Danis K, Vaux S, Levy-Bruhl D, van der Werf S, Béchet S, et al. Association of nonpharmaceutical interventions during the COVID-19 pandemic with invasive pneumococcal disease, pneumococcal carriage, and respiratory viral infections among children in France. Jama Netw Open. 2022;5(6):e2218959.
Kandeel A, Fahim M, Deghedy O, Roshdy WH, Khalifa MK, Shesheny RE, Kandeil A, Naguib A, Afifi S, Mohsen A, et al. Resurgence of influenza and respiratory syncytial virus in Egypt following two years of decline during the COVID-19 pandemic: outpatient clinic survey of infants and children, October 2022. BMC Public Health. 2023;23(1):1067.
Hoy G, Maier HE, Kuan G, Sánchez N, López R, Meyers A, Plazaola M, Ojeda S, Balmaseda A, Gordon A. Increased influenza severity in children in the wake of SARS-CoV-2. Influenza Other Resp. 2023;17(7):e13178.
Fu D, He G, Li H, Tan H, Ji X, Lin Z, Hu J, Liu T, **ao J, Liang X, et al. Effectiveness of COVID-19 vaccination against SARS-CoV-2 Omicron variant infection and symptoms - China, December 2022-February 2023. China CDC Wkly. 2023;5(17):369–73.
Global Burden of Disease Long COVID Collaborators, Wulf HS, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, Blyuss O, Bobkova P, Bonsel G, et al. Estimated global proportions of individuals with persistent fatigue, cognitive, and respiratory symptom clusters following symptomatic COVID-19 in 2020 and 2021. JAMA. 2022;328(16):1604–15.
Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–5.
Gu X, Wang S, Zhang W, Li C, Guo L, Wang Z, Li H, Zhang H, Zhou Y, Liang W, et al. Probing long COVID through a proteomic lens: a comprehensive two-year longitudinal cohort study of hospitalised survivors. EBioMedicine. 2023;98:104851.
Yao XH, He ZC, Li TY, Zhang HR, Wang Y, Mou H, Guo Q, Yu SC, Ding Y, Liu X, et al. Pathological evidence for residual SARS-CoV-2 in pulmonary tissues of a ready-for-discharge patient. Cell Res. 2020;30(6):541–3.
Kumar V. Influenza in children. Indian J Pediatr. 2017;84(2):139–43.
Gaitonde DY, Moore FC, Morgan MK. Influenza: diagnosis and treatment. Am Fam Physician. 2019;100(12):751–8.
World Health Organization. WHO Guidelines for Pharmacological Management of Pandemic Influenza A(H1N1) 2009 and Other Influenza Viruses. Geneva: World Health Organization; 2010.
Callaway E. COVID’s future: mini-waves rather than seasonal surges. Nature. 2023;617(7960):229–30.
Kim EH, Nguyen TQ, Casel MAB, Rollon R, Kim SM, Kim YI, Yu KM, Jang SG, Yang J, Poo H, et al. Coinfection with SARS-CoV-2 and influenza A virus increases disease severity and impairs neutralizing antibody and CD4+ T cell responses. J Virol. 2022;96(6):e0187321.
Munro AP, Jones CE. Immunity debt and unseasonal childhood respiratory viruses. Brit J Hosp Med. 2022;83(9):1–3.
Peluso MJ, Deitchman AN, Torres L, Iyer NS, Munter SE, Nixon CC, Donatelli J, Thanh C, Takahashi S, Hakim J, et al. Long-term SARS-CoV-2-specific immune and inflammatory responses in individuals recovering from COVID-19 with and without post-acute symptoms. Cell Rep. 2021;36(6):109518.
Lai CC, Hsu CK, Yen MY, Lee PI, Ko WC, Hsueh PR. Long COVID: an inevitable sequela of SARS-CoV-2 infection. J Microbiol Immunol. 2023;56(1):1–9.
Liu HF, Lu R, Yang J, **ang M, Ban D, Yang JW, Guo ZH, Yuan TY, Fu HM. Evaluation of febrile seizures in children infected with SARS-CoV-2 Omicron variant in Yunnan, China: a multi-center, retrospective observational study. Front Pediatr. 2023;11:1223521.
Davis HE, McCorkell L, Vogel JM, Topol EJ. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21(3):133–46.
Stein SR, Ramelli SC, Grazioli A, Chung JY, Singh M, Yinda CK, Winkler CW, Sun J, Dickey JM, Ylaya K, et al. SARS-CoV-2 infection and persistence in the human body and brain at autopsy. Nature. 2022;612(7941):758–63.
Cárdenas G, Soto-Hernández JL, Díaz-Alba A, Ugalde Y, Mérida-Puga J, Rosetti M, Sciutto E. Neurological events related to influenza A (H1N1) pdm09. Influenza Other Resp. 2014;8(3):339–46.
Zuin M, Rigatelli G, Bilato C, Porcari A, Merlo M, Roncon L, Sinagra G. One-year risk of myocarditis after COVID-19 infection: a systematic review and meta-analysis. Can J Cardiol. 2023;39(6):839–44.
Principi N, Esposito S. Severe influenza in children: incidence and risk factors. Expert Rev Anti Infect Ther. 2016;14(10):961–8.
Vitoratou DI, Milas GP, Korovessi P, Kostaridou S, Koletsi P. Obesity as a risk factor for severe influenza infection in children and adolescents: a systematic review and meta-analysis. Eur J Pediatr. 2023;182(1):363–74.
Osterhout JA, Kapoor V, Eichhorn SW, Vaughn E, Moore JD, Liu D, Lee D, DeNardo LA, Luo L, Zhuang X, et al. A preoptic neuronal population controls fever and appetite during sickness. Nature. 2022;606(7916):937–44.
Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol. 2015;15(6):335–49.
Launey Y, Nesseler N, Mallédant Y, Seguin P. Clinical review: fever in septic ICU patients–friend or foe? Crit Care. 2011;15(3):222.
Welliver RC. Immunology of respiratory syncytial virus infection: eosinophils, cytokines, chemokines and asthma. Pediatr Infect Dis J. 2000;19(8):780–3.
Yamada T, Wakabayashi M, Yamaji T, Chopra N, Mikami T, Miyashita H, Miyashita S. Value of leukocytosis and elevated C-reactive protein in predicting severe coronavirus 2019 (COVID-19): a systematic review and meta-analysis. Clin Chim Acta. 2020;509:235–43.
Tan L, Wang Q, Zhang D, Ding J, Huang Q, Tang YQ, Wang Q, Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Tar. 2020;5(1):33.
Yu J, Li H, Jia J, Huang Z, Liu S, Zheng Y, Mu S, Deng X, Zou X, Wang Y, et al. Pandemic influenza A (H1N1) virus causes abortive infection of primary human T cells. Emerg Microbes Infec. 2022;11(1):1191–204.
Tsang TK, Lam KT, Liu Y, Fang VJ, Mu X, Leung N, Peiris J, Leung GM, Cowling BJ, Tu W. Investigation of CD4 and CD8 T cell-mediated protection against influenza a virus in a cohort study. BMC Med. 2022;20(1):230.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers: 81660017 and 81960021) and the Yunnan Provincial Department of Education Science Research Fund Project (grant number: 2023Y0790).
Author information
Authors and Affiliations
Contributions
H.F.L. involved in study design, data analysis, data interpretation, literature search, generation of figures, and writing of the manuscript. X.Z.H. involved in study design, data collection, data analysis, generation of figures. R.W.H., Z.H.G., J.R.G., M.X., R.L., D.B., C.Y.L., Y.Y.W., W.L., Y.L. and Y.J.G. involved in data collection, data analysis, and literature search. Q.L. and H.M.F. contributed to conceptualization, study design, project supervision, and writing of the manuscript. All authors reviewed and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committees of Kunming Children’s Hospital Affiliated to Kunming Medical University (the lead institution of this study) (approval number: 2023-04-129-K01), who also waived the informed consent due to the retrospective design of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, HF., Hu, XZ., Huang, RW. et al. Evaluation of disease severity and prediction of severe cases in children hospitalized with influenza A (H1N1) infection during the post-COVID-19 era: a multicenter retrospective study. BMC Pediatr 24, 234 (2024). https://doi.org/10.1186/s12887-024-04645-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-024-04645-x