Abstract
Introduction
Only a few case reports regarding pediatric posterior cruciate ligament (PCL) ruptures without bone avulsion exist in the literature. The present study aims to share our experience in the diagnosis, treatment, and prognosis of a child with a proximal PCL tear.
Materials and methods
This article reports a 5-year-old female diagnosed with a proximal PCL tear. The ruptured PCL was repaired with an all-epiphyseal suture tape augmentation (STA) without evidence of growth plate violation.
Results
The suture tape was removed under arthroscopy and revealed the PCL was re-attached at 12 months after the first surgery. And at the time of this report, 36 months after surgery, she was doing well without any problems and with negative posterior drawer test.
Conclusions
Pediatric PCL tear without bone avulsion is rare. However, the torn PCL was noticed healed based on an arthroscopic second-look.
Similar content being viewed by others
Background
Posterior cruciate ligament (PCL) ruptures are uncommon, largely due to the high relative strength of the fibers [1], and PCL injuries are even more rare in the skeletally immature. There are some studies [2,3,4] regarding pediatric proximal PCL ruptures without bone avulsion, but the paucity of published data makes clinical decision more difficult and prognostic report especially an arthroscopic second-look rarer. Similar to pediatric ACL injuries, the presence of open epiphyseal growth plates complicates the use of traditional reconstruction techniques. Several recent studies [5,6,7,8] in adults reported that suture tape augmentation (STA) may protect and optimize healing in a repaired PCL, eliminating the need to reconstruct a new PCL with an autograft. However, no studies have reported the use of STA in the skeletally immature patients when repairing a ruptured PCL [9]. We present the case of a young child with a proximal PCL rupture that was successfully arthroscopically repaired with STA and without growth plate injury.
Case presentation
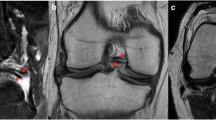
A 5-year-old girl injured her right knee while playing with her mother. It occurred when the mother hugged the girl’s neck from behind and leaned on the girl’s shoulders with her body weight. The mother’s weight was transferred through the girl’s extended right knee, as she was standing on that one leg. Since this event, the girl complained of right knee pain and the inability to bear weight on the right lower extremity. An adjustable splint was applied in her first visit clinic at the time of the injury and was worn until the patient was seen in our clinic 20 days later. Examination of her knee revealed clinical signs of effusion, no limitation of the range of motion, a positive sagging sign of the right tibia, and a posterior drawer test with over 10 mm displacement (Supplement Video 1). A negative right hip exam was observed. X-Ray did not reveal osseous lesions. Magnetic resonance imaging (MRI) showed a complete proximal tear of the PCL with an intact anterior cruciate ligament (ACL) and intact menisci (Fig. 1). A clinical diagnosis of a grade III PCL tear was made, and the girl was scheduled to be treated with surgery as non-operative management might fail to restore the normal kinematics of the knee and predispose to early degeneration. Written informed consent of the operation was obtained from the patient’s parents.
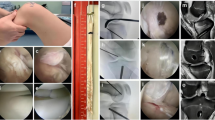
The patient was placed under general anesthesia and positioned supine with a thigh tourniquet and image intensifier set to allow for intra-operative images. Under standard sterile precautions, a standard 30° arthroscope 4 mm in diameter was introduced into the knee for initial assessment. The menisci and ACL were intact. The PCL was found to be ruptured proximally, and without bone avulsion (Fig. 2A-B). Two No. 0 braided absorbable sutures (Coated VICRYL™ Plus, Ethicon) were placed through the tibial PCL stump with a suture passer (Labral scorpion, Arthrex) (Fig. 2C-D). The ends of the sutures were pulled out of the joint through the all-epiphyseal femoral tunnel (Fig. 3), which was drilled using a 2 mm K-wire and a PCL femoral tunnel guide positioned in the PCL femoral footprint (Smith & Nephew) using fluoroscopy. The STA (internal brace, Arthrex) was folded at the eyelets of the cortex-fixation button (Endo-button, Smith & Nephew), and the repair sutures were passed through the eyelets as well (Fig. 4). The end of the STA was extracted out of the joint through an all-epiphyseal tibial tunnel (Fig. 5), which was drilled using a 2 mm K-wire (Fig. 2E-F) and a PCL tibial tunnel guide (Smith & Nephew) manually using fluoroscopy. To tension the PCL, the PCL repair sutures were tied at the surface of the cortex-fixation button on the femur, followed by tibial epiphyseal fixation of the STA. Platelet-rich plasma (PRP) was injected into the PCL femoral footprint (Fig. 2G), and a reduction of the PCL could be seen (Fig. 2H) when the sutures were tensioned in 90° of knee flexion with an anterior drawer force applied to reduce any posterior tibial sag.
Arthroscopic images of the operation. Only PCL was found ruptured proximally without bone avulsion after general inspection (a-b). Absorbable sutures were placed in the PCL stumps by suture passer (c-d). STA tibial tunnel was drilled using a 2 mm K-wire (e–f). The PRP was injected into the PCL femoral footprint (g), and a reduction of the PCL could be seen when the sutures were tensioned in 90° of flexion and anterior drawer (h). ACL (asterisk); PCL (arrow); Medial condyle (arrowhead)
Immediately post operation, the posterior drawer test was negative (Supplement Video 1). The ruptured PCL was repaired with an all-epiphyseal STA without evidence of growth plate violation (Figs. 6 and 7). The child was allowed to walk in an adjustable splint with the help of crutch and was sent to rehabilitation for quadriceps strengthening among the first 4 weeks after the operation. The splint could allow the knee with full range of motion. After 4 weeks post-operation, the crutch and the splint were not applied. At 12 weeks post-operative, she was able ambulate without pain and could take part in all pre-injury activities. (Supplement Video 1) The suture tape was removed under arthroscopy and revealed the PCL was re-attached (Fig. 8) at 12 months after the first surgery. And at the time of this report, 24 months after surgery, she was doing well without any problems and with negative posterior drawer test. Meanwhile, based on the physical examination, no varus or valgus deformity was noticed; and the length of the lower limbs were equal. However, the longer follow up result about the limbs related to growth plate is still unknown, which would be evaluated by annual clinical assessment.
Discussion and conclusion
To the best of our knowledge, this is the first reported case utilizing an all-epiphyseal repair with STA in a skeletally immature patient with a proximal PCL tear. In the present case, the mechanism of injury was hyperextension. This caused failure at the femoral attachment since the femoral chondro-osseous junction is the weakest point in children’s PCLs [1, 10]. A delay of more than 2–3 weeks after injury could result in a time-dependent decrease in tissue quality [11]. Therefore, primary repair combined with STA augmentation was applied in the present case.
The literature on the treatment of pediatric PCL lesions without bone avulsion (Table 1) is sparse. The youngest case report of arthroscopic PCL repair was reported by Lobenhoffer et al. [2], who reported encouraging results with a normal range-of-motion and firm anterior–posterior endpoint in a 3-year-old boy. Nevertheless, MacDonald et al. [12] reported anterior knee pain with nonoperative treatment in a 5-year-old girl. Moreover, a study of seven children [13] with femoral avulsion fractures of the PCL treated conservatively or surgically found that non-operatively treated children had poor functional results. Considering the lack of knowledge regarding the natural history of PCL injuries in children, the most logical strategy is to follow the protocol of adult PCL treatment, which may include repair of the PCL stump securely and without the injury of the growth plate.
Treatment of pediatric PCL injuries always poses a dilemma [14]. One main reason to consider arthroscopic PCL repair over reconstruction includes the potential preservation of the native fibers [15]. Additional benefits include the smaller diameter of the bone tunnels drilled and the absence of graft harvesting [16,17,18]. The decision to repair PCL is made intraoperatively upon verification that the remnant can be reapproximated to the femoral footprint. For that reason, an alternative plan, such as physis-sparing hamstring graft PCL reconstruction [19, 20], should always be presented and discussed with the child and parents. Furthermore, long-term data and consistent clinical evaluation are lacking for this specific technique. These issues must also be addressed during preoperative consultation regarding the risks and benefits of the procedure. Meanwhile, quadriceps strengthening during recovery and rehabilitation remains crucial in this case [21].
The present case featured somewhat unusual characteristics. First, the patient came to our clinic almost three weeks after the injury. Second, the parent refused any procedures that violated the growth plate. The present technique avoided the growth plate entirely and allowed for repair of the PCL in combination with STA [22,23,24] in the event of decreased tissue quality. Additionally, to potentially promote healing of the PCL at the site of the injury, PRP was applied to the femoral footprint [25]. However, the application of PRP is still controversial, especially in the graft healing. It was not recommended to routinely applied in all ligament surgeries. The updated systematic review [26] indicated reduced postoperative pain and improved knee function in the short and medium terms after the PRP injection, however, the long term is ineffective. PRP does not accelerate the healing of grafts. More studies would be required in the future.
In conclusion, proximal PCL tears in skeletally immature patients are rare. This is the first report of a pediatric PCL repair with STA using the physis-sparing technique as a possible method to restore knee function and stability.
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
Abbreviations
- PCL:
-
Posterior cruciate ligament
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- ACL:
-
Anterior cruciate ligament
- PRP:
-
Platelet-rich plasma
- STA:
-
Suture tape augmentation
References
Kannus P, Bergfeld J, Jarvinen M, et al. Injuries to the posterior cruciate ligament of the knee. Sports Med. 1991;12:110–31.
Lobenhoffer P, Wünsch L, Bosch U, Krettek C. Arthroscopic repair of the posterior cruciate ligament in a 3-year-old child. Arthroscopy. 1997;13:248–53. https://doi.org/10.1016/S0749-8063(97)90164-X.
Wheatley WB, Martinez AE, Sacks T, et al. Arthroscopic posterior cruciate ligament repair. Arthroscopy. 2002;18:695–702. https://doi.org/10.1053/jars.2002.32836.
Pisanu G, Moura JL, Saithna A, Sonnery-Cottet B. Arthroscopic repair of proximal posterior cruciate ligament injuries in pediatric patients. Arthrosc Tech. 2019;8:e691–5. https://doi.org/10.1016/j.eats.2019.03.003.
van der List JP, DiFelice GS. Arthroscopic primary posterior cruciate ligament repair with suture augmentation. Arthrosc Tech. 2017;6:e1685–90. https://doi.org/10.1016/j.eats.2017.06.024.
Hopper GP, Heusdens CHW, Dossche L, Mackay GM. Posterior cruciate ligament repair with suture tape augmentation. Arthrosc Tech. 2019;8:e7–10. https://doi.org/10.1016/j.eats.2018.08.022.
Achtnich A, Schmitt A, Forkel P, et al. Acute injury of the posterior cruciate ligament with femoral avulsion: arthroscopic ligament repair and bracing. Oper Orthop Traumatol. 2019;31:12–9. https://doi.org/10.1007/s00064-018-0578-0.
Shu HT, Rigor P, Panish BJ, et al. Posterior cruciate ligament repair with suture augmentation: a report of two cases with two-year follow-up. Cureus. 2021;13. https://doi.org/10.7759/cureus.12447
Vermeijden HD, Van Der List JP, DiFelice GS. Arthroscopic posterior cruciate ligament primary repair. Sports Med Arthrosc Rev. 2020;28:23–9. https://doi.org/10.1097/JSA.0000000000000250.
Janousek AT, Jones DG, Clatworthy M, et al. Posterior cruciate ligament injuries of the knee joint. Sports Med. 1999;28:429–41. https://doi.org/10.2165/00007256-199928060-00005.
DiFelice GS, Lissy M, Haynes P. When to arthroscopically repair the torn posterior cruciate ligament. Clin Orthop Relat Res. 2012;470:861–8. https://doi.org/10.1007/s11999-011-2034-4.
MacDonald PB, Black B, Old J, et al. Posterior cruciate ligament injury and posterolateral instability in a 6-year-old child: a case report. Am J Sports Med. 2003;31:135–6. https://doi.org/10.1177/03635465030310010701.
Zhao X, Kuang S da, Su C, et al. Arthroscopic treatment of femoral avulsion fracture of the posterior cruciate ligament in association with meniscus tear. Orthop Surg. 2020;692–697. https://doi.org/10.1111/os.12636
Scott CEH, Murray AW. Paediatric intrasubstance posterior cruciate ligament rupture. BMJ Case Rep. 2011;1–4. https://doi.org/10.1136/bcr.09.2011.4803
Rugg CM, Liu T, Zhang AL. Arthroscopic primary bundle-specific posterior cruciate ligament repair with transosseous fixation. Arthrosc Tech. 2019;8:e911–6. https://doi.org/10.1016/j.eats.2019.04.005.
Ross G, Driscoll J, McDevitt E, Scheller A. Arthroscopic posterior cruciate ligament repair for acute femoral “peel off” tears. Arthroscopy. 2003;19:431–5. https://doi.org/10.1053/jars.2003.50134.
Rosso F, Bisicchia S, Amendola A. Arthroscopic repair of “peel-off” lesion of the posterior cruciate ligament at the femoral condyle. Arthrosc Tech. 2014;3:e149–54. https://doi.org/10.1016/j.eats.2013.09.014.
Murakami R, Honda E, Fukai A, et al. Single-stage arthroscopic anterior and posterior cruciate ligament repairs and open medial collateral ligament repair for acute knee dislocation. Case Rep Orthop. 2020;2020:1–7. https://doi.org/10.1155/2020/7348201.
Sørensen OG, Faunø P, Christiansen SE, Lind M. Posterior cruciate ligament reconstruction in skeletal immature children. Knee Surg Sports Traumatol Arthrosc. 2017;25:3901–5. https://doi.org/10.1007/s00167-016-4416-3.
Khakha RS, Yasen SK, Wilson AJ. Paediatric physeal sparing posterior cruciate ligament (PCL) reconstruction with parental donation allograft: Rationale and operative approach. Knee. 2018;25:203–9. https://doi.org/10.1016/j.knee.2017.10.003.
Beecher M, Garrison JC, Wyland D. Rehabilitation following a minimally invasive procedure for the repair of a combined anterior cruciate and posterior cruciate ligament partial rupture in a 15-year-old athlete. J Orthop Sports Phys Ther. 2010;40:297–309. https://doi.org/10.2519/jospt.2010.3162.
Richter M, Kiefer H, Hehl G, Kinzl L. Primary repair for posterior cruciate ligament injuries: an eight-year followup of fifty-three patients. Am J Sports Med. 1996;24:298–305.
Lombardo-Torre M, Espejo-Reina A, García-Gutiérrez G, et al. Arthroscopic treatment of concurrent avulsion fracture of anterior and posterior cruciate ligament with suspension device. J Orthop case reports. 2018;8:81–85. https://doi.org/10.13107/jocr.2250-0685.1062
Heitmann M, Akoto R, Krause M, et al. Management of acute knee dislocations: anatomic repair and ligament bracing as a new treatment option—results of a multicentre study. Knee Surg Sports Traumatol Arthrosc. 2019;27:2710–8. https://doi.org/10.1007/s00167-018-5317-4.
Rodkey WG, Arnoczky SP, Steadman JR. Healing of a surgically created partial detachment of the posterior cruciate ligament using marrow stimulation: an experimental study in dogs. J Knee Surg. 2006;19:14–8. https://doi.org/10.1055/s-0030-1248071.
Zhu T, Zhou J, Hwang J, Xu X. Effects of platelet-rich plasma on clinical outcomes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Orthop J Sports Med. 2022;10:23259671211061536. https://doi.org/10.1177/23259671211061535.
Acknowledgements
Not applicable.
Funding
The National Natural Science Foundation of China (81802208) funds this study. The fund was used for platelet-rich plasma and intra-articular injections.
Author information
Authors and Affiliations
Contributions
All listed authors contributed to the manuscript: JH, KB, JL, AL, SW participated in diagnosing and treating the patient, acquisition of data. JH wrote the case report including performing the literature review. SW provided guidance for the literature search and guaranteed the integrity of the work. KB revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors declare that all investigations were conducted in conformity with ethical standards.
Consent for publication
Written informed consent was obtained from the patient and her parents for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplement Video 1. Captured steps of PCL repair.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, J., Byrne, K., Liang, J. et al. Posterior cruciate ligament rupture and all-epiphyseal repair with suture tape augmentation in a 5-year-old girl: a case report and review of the literature. BMC Pediatr 23, 331 (2023). https://doi.org/10.1186/s12887-023-04146-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-023-04146-3