Abstract
Background
A complication of elective cesarean section (CS) delivery is its interference with the normal intestinal colonization of the infant, affecting the immune and metabolic signaling in early life— a process that has been associated with long-term morbidity, such as allergy and diabetes. We evaluate, in CS-delivered infants, whether the normal intestinal microbiome and its early life development can be restored by immediate postnatal transfer of maternal fecal microbiota (FMT) to the newborn, and how this procedure influences the maturation of the immune system.
Methods
Sixty healthy mothers with planned elective CS are recruited and screened thoroughly for infections. A maternal fecal sample is taken prior to delivery and processed according to a transplantation protocol. After double blinded randomization, half of the newborns will receive a diluted aliquot of their own mother’s stool orally administered in breast milk during the first feeding while the other half will be similarly treated with a placebo. The infants are clinically followed, and fecal samples are gathered weekly until the age of 4 weeks, then at the ages of 8 weeks, 3, 6, 12 and 24 months. The parents fill in questionnaires until the age of 24 months. Blood samples are taken at the age of 2–3 days and 3, 6, 12 and 24 months to assess development of major immune cell populations and plasma proteins throughout the first years of life.
Discussion
This is the first study to assess long-time effects on the intestinal microbiome and the development of immune system of a maternal fecal transplant given to term infants born by CS.
Trial registration
ClinicalTrials.gov NCT04173208, registration date 21.11.2019.
Similar content being viewed by others
Background
Microbes colonizing newborn infants at birth and during the first weeks of life are considered important, and perturbation to this process of colonization is associated with disruption of the stereotypic immune system development early in life [1, 2]. Early disturbances in gut microbiome have been associated with a multitude of inflammatory diseases, such as the development of autoimmune diseases [3], allergic diseases and atopy [4, 5], asthma, type I diabetes [6], and inflammatory bowel diseases [7, 8]. A recently published population cohort study also showed that compared with vaginally-delivered (VD) infants, the risk of infection-related hospitalization was greater among those born by cesarean section (CS) [9]. The difference of the early colonizing microbiome was thought to be one of the associating factors [9, 10].
The first stools of the newborns, the meconium, contain very low amounts of bacterial DNA and their composition differs greatly from that of later stool samples. The stool microbial communities develop along similar and time-dependent trajectories, in the absence of treatment with antibiotics [11, 12]. During the postnatal period the gut microbiome of VD and by CS-delivered infants differs markedly from each other [12,13,14,15,16] and this difference persists throughout the first years of life [17]. The disturbed transmission of the maternal gastrointestinal bacteria (particularly pioneering Bacteroides and Bifidobacterium species) through delivery by CS and maternal intrapartum antibiotic prophylaxis predispose newborn infants to colonization by potentially clinically important opportunistic pathogens that circulate in the hospital environment [16]. Infants born by CS have a less diverse intestinal microbiome and lower Th1 response than those born by vaginal delivery [18].
Various studies show that the intestinal microbiome influences vaccine responses, especially early in life [19,20,21]. Pneumococcal vaccine response can be studied for example by measuring serotype specific IgG antibodies. Finnish children are vaccinated with the pneumococcal conjugate vaccine at the age of 3, 5 and 12 months.
Due to the anticipated impact of disturbed microbial development on the develo** immune system associated with delivery by CS, many researchers have tried to alleviate the effect of CS delivery on child microbiota. Treating the mother and breastfed child with a multispecies probiotic supplement may correct undesired changes in microbiota composition and function caused by cesarean birth [22]. Breastfeeding has a significant role in sha** the microbiota for example because of its oligosaccharides. Fucosylated oligosaccharides in mother's milk may also alleviate the effects of cesarean birth on infant gut microbiota [23]. A recent study reported that the microbial composition of breast milk was associated with the birth mode and exposure to intrapartum antibiotics [24].
Maternal probiotic supplementation has been shown to decrease the development of atopic dermatitis in the offspring [25]. In a 5-year and later on 13-year follow-up, probiotic intervention protected CS-delivered children from allergic disease and eczema [26, 27]. However, the topic is controversial and there is lack of evidence that probiotics prevent other chronic immune-mediated diseases.
Vaginal microbial transfer has been suggested to partially restore the intestinal microbiome of CS-delivered infants [28]. However, the vaginal microbiome is limited to mainly Lactobacillus spp. and does not contain the microbes that are abundant in the gut microbiota of the infant or the mother [14]. In addition, vaginal lactobacilli do not colonize the gastrointestinal tract of neonates but only pass it transiently, and their relevance for long-term health remains unclear [14, 29]. Hence, we recently reported that a fecal transfer from the infant’s own mother could restore rapidly and significantly the microbiome of CS-delivered infants towards that of those born vaginally [30]. Among the 17 mothers recruited, seven were selected after careful screening. Their infants received a diluted fecal sample from their own mothers, taken prior to delivery. Following a 3-month follow-up, all seven infants presented an uneventful clinical course without any adverse effects. The temporal development of the fecal microbiota composition of FMT-treated CS-delivered infants no longer resembled that of untreated CS-delivered infants but showed significant similarity to that of VD infants.
The implication of this study is that maternal fecal microbiota transplantation (FMT) mimics the natural transfer of microbiota from mother to VD infants.
Here, we present a protocol for randomized, double-blinded placebo-controlled clinical trial of orally delivered FMT from mothers to their CS-delivered infants, with a two-year follow-up period. The aim of the trial is to study the differences in microbiota between infants born by CS that received maternal fecal microbiota or a placebo transplantation, and to gain insight into the mechanisms involved in immune development and its association with early microbiota composition.
Significance
Study purpose
To the best of our knowledge, this is the first randomized study to assess whether maternal fecal transplant can be used as a method to close the gap in the heterogeneity of the intestinal microbiota of CS-delivered infants compared with the VD infants. In addition, it gives a unique possibility to study the interaction of gastrointestinal microbiome with the development of immunity during infancy.
Study design
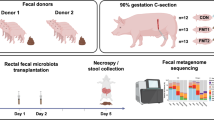
One hundred healthy pregnant women scheduled for elective CS at term, are recruited at 35–37 weeks of gestation during a visit for the assessment of mode of delivery (Fig. 1) at Women’s Hospital, Helsinki and Jorvi Hospital, Espoo, Finland. Maternal exclusion criteria are age below 18 years, gestational diabetes that requires medication, use of regular medication, known or suspected fetal congenital abnormality, travelling abroad within the last three months and antibiotic treatment within 3 months of delivery (excluding the prophylactic cefuroxime (or other in case of allergy) given prior to the elective CS). Non-elective CS is an exclusion criterion.
The midwifes and doctors inform potential mothers of the study at the visit and those who are interested to participate are contacted by the study nurse.
After informed consent, the pregnant woman is tested for potential contagious diseases as explained below (Table 1). Resulting from the screening process, a 40% exclusion rate is expected because of group B streptococci (GBS) carrier state (24% of pregnant women in our region) [31] and other positive findings in the screening samples.
The eligible women are randomized into placebo (GP, 30 women), and intervention group (GI, 30 women). The randomization 1:1 is done in blocks of 4 mothers. The study is double blinded. The laboratory technicians who prepare the FMT product also perform the computer-generated randomization.
For promoting the study, we have set up posters and informed the staff at the maternity clinics, and used social media.
A fecal sample of 100 g and a blood sample of 15 mL are collected from the mother approximately two weeks prior to scheduled CS for screening of contagious diseases (Fig. 1). The mother divides the feces into the administered sample tubes according to written instructions. Feces for the transplant is collected into an empty tube using a spoon in the cap. The mother informs the research nurse, who delivers the tubes taken for screening to the laboratory as soon as possible, where the transplant is prepared from the fresh sample – this process is completed with a 6 h time frame.
The fresh fecal sample is screened for the presence of parasites and pathogenic viruses and bacteria (Fig. 1, Table 1). An aliquot (0.125 g) of the fresh fecal sample is used to determine the bacterial composition of the sample. Another part of this fresh sample is used as the transplant and for that purpose 1 g of feces is dissolved in 15 mL of isotonic saline and 10% glycerol, homogenized, and the 0.5 mL aliquots of the transplant are immediately frozen and stored at -80 °C [32].
At delivery, the transplant is thawed and 0.5 mL representing 3.5 mg of the mother’s fecal sample is dissolved in 5 mL of the mother’s own milk or when not available pasteurized bank milk. The sample is given orally to newborn infants born to GI (Intervention group) mothers within 2 h of delivery. The newborn infants born to GP (Placebo group) mothers are given 0.5 mL of isotonic saline dissolved in 5 mL of pasteurized bank milk or mother’s own milk as described earlier. The randomization is performed on the day of the scheduled CS and 0.5 mL of either transplant or placebo is delivered to the ward on ice in a black polypropylene tube for blinding purposes.
Infant exclusion criteria are Apgar score of less than 8 at 5 min of age, birth weight below 2500 g or above 4500 g, disturbances of neonatal adaptation (such as transient tachypnea of the newborn) and antibiotic treatment of the newborn before discharge. In case of a suspected infection of the newborn the randomization code can be opened.
After the first feeding the newborn is observed for potential reactions, such as increased peristalsis, diarrhea, vomiting, fever, and rash. Possible adverse events are reported to the electronic database. Before discharge, typically on postnatal day 2, a 3 mL blood sample is gathered from the newborn for the assessment of white cell count, C-Reactive Protein (CRP) and hemoglobin, and for detailed immunological analyses. The sample is taken at the routine sampling for metabolic screening.
During the hospital stay two fecal samples are collected from the newborn: on the day of birth and third day of life (Fig. 1).
From the first postnatal week on, the infant is followed in the well-baby clinic according to national protocols. As a part of the study, the parents can be in contact with the study nurse and pediatrician by telephone. Fecal samples of the infant are taken weekly for the first 4 weeks, and at 8 weeks and 3 months, by the parents. Fecal sample from the mother is taken 4 weeks postpartum. Samples are temporarily stored at − 20 °C in the home freezer before transfer in frozen form to − 80 °C. (Fig. 1).
Breastfeeding mothers give a breast milk sample at 2 and 8 weeks postpartum. Milk samples are temporarily stored at − 20 °C in the home freezer before transfer in frozen form to − 80 °C.
At 3 months postnatally, the study nurse visits the family homes. The visit is timed before the second orally given rota virus vaccination, if possible. Data from growth measurements performed at the well-baby clinic visits are gathered. Fecal samples of the infant and the mother (4 weeks post partum) stored in the home freezer are collected during the visit. A capillary blood sample of 1–1.5 mL is collected by the study nurse. The families have the possibility to meet with the study pediatrician (Fig. 1).
At 6 months of age fecal samples are collected from the mother and infant and a 3 mL blood sample is collected from the infant at a laboratory.
At 12 months of age, a follow-up visit to the study nurse takes place for all families for the assessment of growth (Fig. 1). Also, data from growth measurements performed at the well-baby clinic visits are gathered as well as vaccination status. A week prior to the visit, fecal samples of the infant and the mother are taken by the parents and stored at -20 °C in the home freezer and delivered at the visit. At the visit a 5 mL blood sample is collected. The families have the possibility to meet with a pediatrician. The families are also given a sealed envelope containing information of the allocation group.
At 24 months of age, a follow-up visit to the study nurse takes place (Fig. 1). The visit, including collecting fecal samples from mother and child, and a 5 mL blood sample from the child, is identical to the follow-up visit at the age of 12 months.
Methods
Fecal samples
The maternal transplant is prepared from a fresh fecal sample taken at least one week before elective CS and within 6 h of donation prepared as described [32], and frozen at -80C.
For the follow-up samples, a home sampling kit is provided for fecal samples of the mother and of the infant’s feces from diapers. The intestinal microbiota of mothers and infants is determined using 16S rRNA gene amplicon sequencing using the MiSeq sequencing [22, 23]. Fecal DNA is extracted by repeated bead beating from ca. 125 mg of fecal material [33] and processed for sequencing of the hypervariable V3-V4 region of the 16S rRNA gene using primers 341F 5′-CCTACGGGNGGCWGCAG-3′ and 785R 5’-GACTACHVGGGTATCTAATCC-3′ [15, 34] and barcoding primers from Kozich et al. [35] as explained in detail elsewhere [36]. The pooled libraries are sequenced with Illumina MiSeq platform using a MiSeq v3 reagent kit (MS-102–3003) with 5% PhiX as spike-in (Illumina).
The DNA sequences are processed and analyzed using the R-package mare [37, 38], which uses USEARCH and ASVs for read processing, and taxonomic annotation [39]. DNA extractions and MiSeq runs are processed in a time frame of 12 months and include internal reference samples and, if requested, a mock community [40, 41]. Metagenomic analysis is conducted essentially as previously demonstrated [42]. In brief, Nextera XT libraries are sequenced with Illumina Novaseq with the target of 7 Gbp of sequence per sample at the sequencing laboratory of the Institute for Molecular Medicine Finland FIMM Technology Centre, University of Helsinki. Filtered reads are assembled with Metaspades and Megahit and ORFs are predicted with Prodigal. Species level community profiling based on marker genes are done using Metaxa2. Resistance genes are characterized by map** metagenomic reads with Bowtie2 against the CARD and Resfinder databases to search for acquired antibiotic resistance genes [42].
Blood samples
We collect 1.5–5 mL of blood from the children depending on their age. For mass cytometry analysis, 100 μL whole blood is mixed with Whole Blood Cell Stabilizer (Cytodelics AB, Stockholm, Sweden) at a ratio of 1:1, incubated at room temperature for 10 min and transferred to a − 80 °C freezer for storage (6–9 months as per the manufacturer’s recommendation) until further processing for mass cytometry experimentation [2].
For fix/lysis of stabilized and cryopreserved whole blood sample, 100 μL sample is thawed at 37 °C followed by addition of Fix/Lyse buffer (Cytodelics AB, Stockholm, Sweden) at a blood:buffer concentration of 1:10 and incubated at room temperature for 10 min. The sample is then diluted 1:4 with Wash buffer #1 (Cytodelics AB,Stockholm, Sweden) and left to lyse for 15 min at ambient temperature. Cells are then washed twice with Wash buffer #2 (Cytodelics AB, Stockholm, Sweden), filtered through a 35 μm mesh and counted using a Bio-Rad TC20 cell counter [2].
Peripheral blood mononuclear cells (PBMC) are isolated using density gradient-based separation. 300–500 µL of blood is put in a BD Vacutainer CPT tube and centrifuged at 1600xg for 15 min followed by collection of buffy coat. Cells are frozen in freezing medium containing 50% RPMI, 30% FBS and 20% DMSO and processed as described previously [2] and transferred to a − 80 °C freezer for long-term storage awaiting analysis.
Plasma samples are obtained by centrifugation of blood samples at 2000xg for 10 min at 8–12 °C and supernatant collected and processed as described previously [2]. The samples are frozen at -80 °C post collection. Plasma protein analyses are done using Olink’s PEA assay (Olink, Uppsala, Sweden).
Humoral vaccine responses are measured at the age of 12 and 24 months as follows: concentrations of serum IgG to pneumococcal capsule polysaccharides included in the 10-valent PCV (1, 4, 5, 6B, 7F, 9 V, 14, 18C, 19F and 23F) and Haemophilus influenzae type b capsule polysaccharide are measured from serum samples with a fluorescent bead-based multiplex immunoassay (Luminex) as described previously [43].
Assessment of allergen-specific IgEs are analyzed with Immuno-CAP (Phadia, Uppsala, Sweden) in blood samples collected at the 12 and 24 months visits at the Laboratory of Helsinki University Hospital as described earlier [44].
Breast milk
The samples are collected 2 and 8 weeks post-partum from breast feeding mothers. FUT2 dependent milk oligosaccharides are analyzed as described earlier [23]. In essence, skimmed breast milk samples are analyzed using MALDI-TOF (matrix assisted laser desorption/ionization—time of flight) mass spectrometry (MS) profiling and liquid chromatography to quantify 2′fucosyllactose (2′FL) and by high performance anion exchange chromatography (HPAEC) with a CarboPac PA1 analytical column coupled to a pulsed amperometry detector (ICS3000, Thermo Fischer Dionex, Sunnyvale, USA).
Questionnaires
Data are collected on the families’ lifestyle, environmental exposures and the health of the study infants and their parents using online questionnaires, enabling monitoring and data query during data collection. Questionnaires are filled by the parents before the birth of the infant and subsequently. Parents are requested to fill in questionnaires on child’s nutrition, gastrointestinal function, and care practices weekly for the first 3 months, then monthly until 12 months of age and then at 18 months and 24 months of age. The questions change as the child grows. Illnesses, medication and use of probiotics and other dietary supplements are reported in the questionnaires. The questionnaires related to nutrition, health and background are mainly similar as in the ongoing HELMi study [45]. To enhance compliance of response rates to the questionnaire, parents receive automatic reminders via email and SMS-messages.
Outcome
Microbiome
The primary outcome of the study is the difference in composition of the intestinal microbiome, specifically diversity and relative abundances of Bacteroides spp., Bifidobacterium spp. as well as known pathobionts between the two groups at 3 months of age. We use beta-diversity between the microbiota profiles of the two groups calculated by PERMANOVA as described previously [46]. The analysis of the gut microbiome is performed at 12 months (including previous sequential samples) and at 24 months. Unblinding for the parents is done at 12 months and for the research group at 24 months.
Markers of immunodevelopment
Early life immune system development follows a standardized trajectory recently described in human infants [2]. By analyzing ~ 50 markers per immune cell we are able to assess all white blood cell populations and their phenotypic and activation state. By map** the immune development in this proposed study, we can directly compare immune developmental trajectories between children with different microbiomes.
Markers of allergens and vaccine responses
The secondary outcomes are the differences in markers of allergy and vaccine responses at 12 and 24 months of age.
Power analysis
The trial is designed with a planned sample of 100 mothers, allowing the final number of the subjects with an estimated 40% drop-out rate due to screening positivity to be 60 (30 in each intervention group) taking into consideration that it is likely to have drop-outs during the follow-up period.
Heterogeneity of microbiota is calculated as an index and used as the primary outcome at 3 months of age. The Standard Benjamini–Hochberg corrections for multiple testing are applied when testing multiple taxa. FDR-corrected p-values < 0.15 are considered statistically significant, but if needed uncorrected p-values are reported for clarity. 15 infants per CS group would be sufficient to detect a moderate effect size of 0.25 standard deviations for our primary outcome (power calculation for balanced one-way ANOVA test, 85% power, α = 0.05).
Availability of data and materials
Findings from this study will be communicated with the scientific community and participants. Scientific communication will be through presentations at relevant international and domestic conferences and meetings, as well as publications in peer-reviewed journals.
Abbreviations
- CRP:
-
C-reactive Protein
- CS:
-
Cesarean section
- FMT:
-
Fecal microbiota transplant
- FUT2:
-
Fucosyltransferase 2
- GBS:
-
Group B streptococci
- GI:
-
Intervention group
- GP:
-
Placebo group
- VD:
-
Vaginally-delivered
References
Olszak T, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science. 2012;336(6080):489–93.
Olin A, et al. Stereotypic immune system development in newborn children. Cell. 2018;174(5):1277-1292.e14.
Collado MC, et al. Gut microbiota: a source of novel tools to reduce the risk of human disease? Pediatr Res. 2015;77(1–2):182–8.
Kalliomäki M, et al. Distinct patterns of neonatal gut microflora in infants in whom atopy was and was not develo**. J Allergy Clin Immunol. 2001;107(1):129–34.
Abrahamsson TR, et al. Low diversity of the gut microbiota in infants with atopic eczema. J Allergy Clin Immunol. 2012;129(2):434-40-440.e1-2.
Vatanen T, et al. Variation in microbiome LPS immunogenicity contributes to autoimmunity in humans. Cell. 2016;165(6):1551.
Sevelsted A, et al. Cesarean section and chronic immune disorders. Pediatrics. 2015;135(1):e92–8.
Andersen V, et al. Caesarean delivery and risk of chronic inflammatory diseases (inflammatory bowel disease, rheumatoid arthritis, coeliac disease, and diabetes mellitus): a population based registry study of 2,699,479 births in denmark during 1973–2016. Clin Epidemiol. 2020;12:287–93.
Miller JE, et al. Mode of birth and risk of infection-related hospitalisation in childhood: a population cohort study of 7.17 million births from 4 high-income countries. PLoS Med. 2020;17(11):e1003429.
Reyman M, et al. Impact of delivery mode-associated gut microbiota dynamics on health in the first year of life. Nat Commun. 2019;10(1):4997.
de Weerth C, et al. Intestinal microbiota of infants with colic: development and specific signatures. Pediatrics. 2013;131(2):e550–8.
Korpela K, de Vos WM. Early life colonization of the human gut: microbes matter everywhere. Curr Opin Microbiol. 2018;44:70–8.
Bäckhed F, et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe. 2015;17(5):690–703.
Ferretti P, et al. Mother-to-infant microbial transmission from different body sites shapes the develo** infant gut microbiome. Cell Host Microbe. 2018;24(1):133-145.e5.
Korpela K, et al. Selective maternal seeding and environment shape the human gut microbiome. Genome Res. 2018;28(4):561–8.
Shao Y, et al. Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature. 2019;574(7776):117–21.
Salminen S, et al. Influence of mode of delivery on gut microbiota composition in seven year old children. Gut. 2004;53(9):1388–9.
Jakobsson HE, et al. Decreased gut microbiota diversity, delayed Bacteroidetes colonisation and reduced Th1 responses in infants delivered by caesarean section. Gut. 2014;63(4):559–66.
Zimmermann P, Curtis N. The influence of the intestinal microbiome on vaccine responses. Vaccine. 2018;36(30):4433–9.
Harris VC, et al. significant correlation between the infant gut microbiome and rotavirus vaccine response in Rural Ghana. J Infect Dis. 2017;215(1):34–41.
Harris V, et al. Rotavirus vaccine response correlates with the infant gut microbiota composition in Pakistan. Gut Microbes. 2018;9(2):93–101.
Korpela K, et al. Probiotic supplementation restores normal microbiota composition and function in antibiotic-treated and in caesarean-born infants. Microbiome. 2018;6(1):182–182.
Korpela K, et al. Fucosylated oligosaccharides in mother’s milk alleviate the effects of caesarean birth on infant gut microbiota. Sci Rep. 2018;8(1):13757.
Hermansson H, et al. Breast milk microbiota is shaped by mode of delivery and intrapartum antibiotic exposure. Front Nutr. 2019;6:4.
Pelucchi C, et al. Probiotics supplementation during pregnancy or infancy for the prevention of atopic dermatitis: a meta-analysis. Epidemiology. 2012;23(3):402–14.
Kuitunen M, et al. Probiotics prevent IgE-associated allergy until age 5 years in cesarean-delivered children but not in the total cohort. J Allergy Clin Immunol. 2009;123(2):335–41.
Kallio S, et al. Perinatal probiotic intervention prevented allergic disease in a Caesarean-delivered subgroup at 13-year follow-up. Clin Exp Allergy. 2019;49(4):506–15.
Dominguez-Bello MG, et al. Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med. 2016;22(3):250–3.
Kervinen K, et al. Vaginal microbiota in pregnancy: Role in induction of labor and seeding the neonate’’s microbiota? J Biosci. 2019;44(5):116.
Korpela K, et al. Maternal fecal microbiota transplantation in cesarean-born infants rapidly restores normal gut microbial development: a proof-of-concept study. Cell. 2020;183(2):324-334.e5.
Place K, et al. Vaginal streptococcus B colonization is not associated with increased infectious morbidity in labor induction. Acta Obstet Gynecol Scand. 2021;100(8):1501–10.
Helve O, et al. Protocol for oral transplantation of maternal fecal microbiota to newborn infants born by cesarean section. STAR Protoc. 2021;2(1):100271.
Korpela K, et al. Gut microbiota develop towards an adult profile in a sex-specific manner during puberty. Sci Rep. 2021;11(1):23297.
van Nood E, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–15.
Kozich JJ, et al. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl Environ Microbiol. 2013;79(17):5112–20.
Virtanen S, et al. Vaginal Microbiota Composition Correlates Between Pap Smear Microscopy and Next Generation Sequencing and Associates to Socioeconomic Status. Sci Rep. 2019;9(1):7750.
Korpela K, et al. Intestinal microbiome is related to lifetime antibiotic use in Finnish pre-school children. Nat Commun. 2016;7:10410.
Korpela K. mare: Microbiota Analysis in R Easily. R package version 1.0. 2016 [cited 2016]. https://github.com/katrikorpela/mare.
Edgar RC. Search and clustering orders of magnitude faster than BLAST. Bioinformatics. 2010;26(19):2460–1.
Ramiro-Garcia J, et al. NG-Tax, a highly accurate and validated pipeline for analysis of 16S rRNA amplicons from complex biomes. F1000Res. 2016;5:1791.
Salonen A, et al. Comparative analysis of fecal DNA extraction methods with phylogenetic microarray: effective recovery of bacterial and archaeal DNA using mechanical cell lysis. J Microbiol Methods. 2010;81(2):127–34.
Pärnänen K, et al. Maternal gut and breast milk microbiota affect infant gut antibiotic resistome and mobile genetic elements. Nat Commun. 2018;9(1):3891.
Nurk S, et al. metaSPAdes: a new versatile metagenomic assembler. Genome Res. 2017;27(5):824–34.
Rosendahl J, et al. High-dose vitamin D supplementation does not prevent allergic sensitization of infants. J Pediatr. 2019;209:139-145.e1.
Korpela K, et al. Cohort profile: finnish Health and Early Life Microbiota (HELMi) longitudinal birth cohort. BMJ Open. 2019;9(6):e028500.
Wilson BC, et al. Oral administration of maternal vaginal microbes at birth to restore gut microbiome development in infants born by caesarean section: A pilot randomised placebo-controlled trial. EBioMedicine. 2021;69:103443.
Acknowledgements
We wish to thank all the families who have already participated in this study. We also thank the personnel of Helsinki Women’s Hospital, Espoo Hospital and Jorvi Hospital. We are grateful to our research nurse, midwife Sirpa Nolvi and technicians Sari Lindén and Evgenia Dikareva.
Confidentiality
Any information collected from potential and consented participants is stored securely and can only be accessed by the research team and monitor. Copies of consent forms are stored in a locked filing cabinet with access limited to research team members. Questionnaires are in an online database only accessible for the research team and the monitor. Data from hard copies are subsequently entered into password-protected web-based platforms, only accessible by the research team. Participants’ study information is not released outside of the research team (except to a study monitor provided by Helsinki and Uusimaa Hospital District), with the exception of positive screening results for mothers. All data and samples are de-identified prior to analyses.
Funding
This research is supported by grants by Suomen Lääketieteen Säätiö, a Governmental Subsidy for Clinical Research, Biocodex Microbiota Foundation, Foundation for Pediatric Research in Finland, Päivikki and Sakari Sohlberg Foundation, Finska Läkaresällskapet and Academy of Finland.
The supporters have had no role in study design, data collection, analysis, or interpretation, or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
SA, OH and WMdV conceptualized and designed the study, and obtained funding; KLK, PB, NC contributed to study design. NC drafted the initial manuscript, which was critically revised for important intellectual content by OH, AS, SA, PB, KLK, WMdV, all authors approved the final version of the protocol and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Committee of the Hospital District of Helsinki and Uusimaa has approved the study (HUS/3233/2017) and it is registered into ClinicalTrials.com (NCT04173208). An informed written consent is obtained from the parents at recruitment by the study nurse.
The study protocol adheres to the ethical guidelines outlined in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
No competing interest to be declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Carpén, N., Brodin, P., de Vos, W.M. et al. Transplantation of maternal intestinal flora to the newborn after elective cesarean section (SECFLOR): study protocol for a double blinded randomized controlled trial. BMC Pediatr 22, 565 (2022). https://doi.org/10.1186/s12887-022-03609-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-022-03609-3